Abstract
Background:
We describe the role of primary care reengineering in the Ochsner Health System (OHS) patient portal implementation strategy and compare subsequent trends in service utilization and disease control among portal users vs nonusers within this context.
Methods:
This retrospective cohort study includes 101,019 patients with hypertension or diabetes who saw an OHS primary care provider (PCP) between 2012 and 2014. Inverse probability treatment weighting was used to reduce case-mix differences between study groups. We used generalized estimating equation modeling to compare changes in encounter rates (PCP, telephone, specialty services, emergency department [ED], inpatient hospitalization), blood pressure (BP), and hemoglobin A1c (HbA1c).
Results:
Age, sex, race, comorbidities, insurance, preindex utilization, and portal use were associated with changes in utilization, BP, and HbA1C; however, the strength and direction of these differences varied. An adjusted analysis comparing portal users to nonusers showed an increase in PCP (rate ratio per patient per year of 1.18, 95% confidence interval [CI] 1.14-1.22) and telephone encounter rates (1.15, 95% CI 1.08-1.22; both P<0.001) but no significant differences in specialty, ED, or inpatient hospitalization encounters. Among patients with preindex systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg, portal users compared to nonusers had a greater decline in their BP, although the between-group difference was small (mmHg [SE], –1.1 [0.42] and –1.2 [0.34], respectively; both P<0.01). Portal users with diabetes compared to nonusers with diabetes also had greater decreases in HbA1c (all patients, % [SE], –0.13 [0.06]; patients with a preindex HbA1c ≥8, –0.43 [0.13], both P<0.05).
Conclusion:
Our findings may reflect patient factors and system-level portal implementation strategies that focused heavily on accessibility to care.
Keywords: Diabetes mellitus; health care quality, access, and evaluation; hypertension; patient portals; primary health care; utilization
INTRODUCTION
Technology applications that support patient-centered care positively affect healthcare processes, clinical outcomes, patient-provider communication and satisfaction, and access to medical information.1 Patient portal technology is an example of such an application. Common features of patient portal websites include access to the patient's personal health information (eg, medical problems, medications, allergies, immunizations, laboratory results, and summaries of clinic and hospital visits); administrative functions that allow patients to schedule nonurgent appointments, update contact information, and make payments; secure messaging with healthcare teams (eg, email and medication refill requests); and access to medical tools (eg, educational materials and health tracking tools). Use of portal technology among patients remains low, and the impact of portal use on healthcare service utilization, outcomes, and cost remains unclear.2 Randomized controlled trials and observational studies have yielded mixed results regarding the association between portal use and rates of in-person clinic visits, telephone encounters, emergency department (ED) visits, and inpatient hospitalizations.2-7 Studies examining the associations between portal use and disease control among patients with chronic conditions such as hypertension and diabetes have also yielded mixed results.7-11 The extent to which organizational contexts and the processes for implementing portals in different settings contribute to these mixed results is uncertain.
In this article, we describe the quality improvement context in which an electronic medical record (EMR)-tethered patient portal was implemented in a large, integrated-delivery health system. Within this context, we examine the direction and strength of associations between portal use among primary care patients with hypertension and/or diabetes and population trends in healthcare service utilization, blood pressure (BP), and hemoglobin A1c (HbA1c) levels during a 2.5-year observation period. We explore how system-, practice-, and patient-level factors may be associated with the study results.
METHODS
Study Setting and Organizational Context
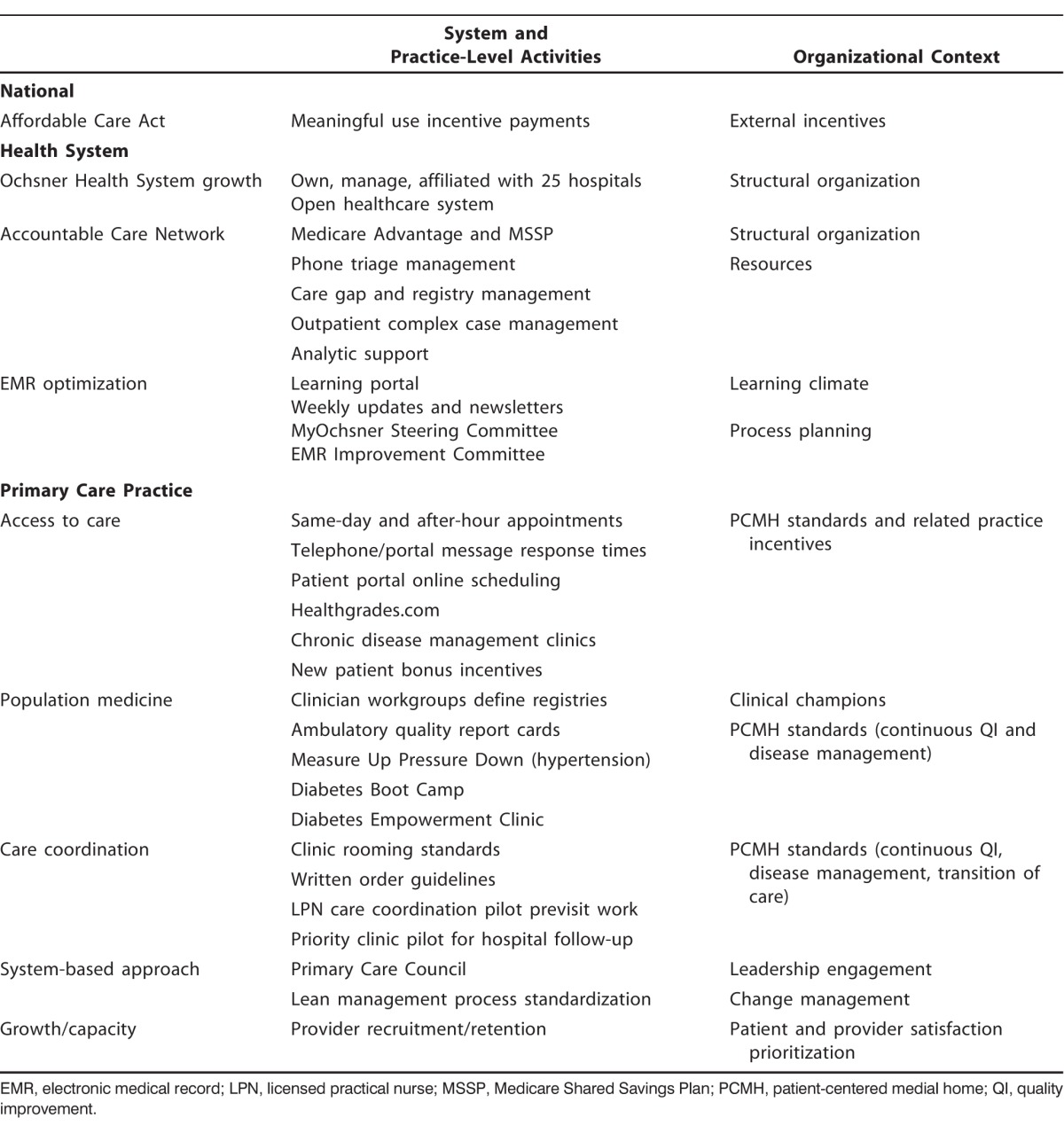
This study was conducted at Ochsner Health System (OHS), southeast Louisiana's largest nonprofit, academic, multispecialty healthcare delivery system that serves approximately 1 million unique patients through local, national, and international programming. OHS owns, manages, or is affiliated with 25 hospitals and 50 health centers. Table 1 summarizes the organizational context in which this study was conducted.
Table 1.
Organizational Context of Systemwide Factors and Primary Care Practice-Level Interventions in the Ochsner Health System from 2012 to 2014
Patient Portal Implementation.
In July 2012, OHS switched from a home-grown EMR system to Epic Systems which includes an online portal feature. OHS launched the portal, MyOchsner, to give patients the ability to review and manage their health information. MyOchsner allows patients to securely schedule/cancel nonurgent appointments, request medication refills, send and receive secure messages, view/download their health records, and access medical tools (eg, wireless or patient-entered flowsheet data). Between 2013 and 2014, the MyOchsner steering committee, which oversees strategic planning for portal service expansion, launched a campaign to encourage patients to activate their MyOchsner accounts through a variety of mechanisms, including notices posted in clinics, staff dissemination of information at check-in, after-visit instructions, patient mailings, and marketing via the OHS website.
The MyOchsner steering committee's major focus is enhancing accessibility to care. To date, 306,305 patients have activated their MyOchsner accounts, but only 8% of appointments are scheduled through the portal. Most of these appointments are with adult primary care and obstetrics/gynecology. Adult primary care has been the system leader for incorporating MyOchsner into the department's workflow and is frequently employed as the use case for expansion of portal features (eg, scheduling, previsit questionnaires, open notes) before the services are launched through other departments.
Primary Care Practice Reengineering.
OHS primary care practice reengineering is driven primarily by organizational changes occurring with regional service expansion across Louisiana, growth of the Ochsner Accountable Care Network, and financial incentives to achieve a quadruple aim: improve quality, reduce cost, and improve patient and healthcare worker experiences. The OHS medical home transformation focuses on strategies to make care accessible, patient-centered, comprehensive, and coordinated (Table 1). Equally important is a systems-based approach to quality and safety, leadership engagement through the Primary Care Council, and practice-level quality improvement to enhance the patient's experience of care. Primary care providers (PCPs) have led the health system in promoting the use of MyOchsner among their patients by incorporating recommendations for portal activation in the workflow procedures for placing patients in examination rooms (eg, rooming standards), being early adopters of online scheduling, and developing lean management strategies to improve care team response times to portal/telephone messages (eg, portal email is directed to the nursing pool first for triage).
Study Design
We conducted a retrospective observational study of adult patients (age ≥18 years) who had at least 2 primary care visits between July 2012 and December 2014 and a diagnosis of hypertension and/or diabetes. We focused on this subpopulation of Ochsner patients because of primary care's system leadership in adopting patient portal workflows; the high prevalence of hypertension and diabetes within our system and the larger Louisiana population; and our health system's launch of a number of chronic disease management programs for optimizing care of patients with hypertension or diabetes. This study compares health service utilization and health outcomes among MyOchsner portal users vs nonusers. Portal users were defined as having portal activity documented, whereas nonusers did not have any portal activity documented. This study was approved by the OHS Institutional Review Board.
Study Variables
We abstracted data from the EMR for patients ≥18 years old who had a diagnosis of hypertension (International Classification of Diseases, Ninth Revision [ICD-9] code range 401.xx-405.xx) or diabetes (ICD-9 codes 250.xx, 648.0x, 775.1x). We collected data for healthcare utilization documented in the EMR 1 year prior to and after the index date. We defined the index date for MyOchsner users as the date on which they first logged into the patient portal. For nonusers, we defined the index date as the midpoint between their first and last contact with a PCP, similar to the definition used in a previous study.6 Measures of healthcare utilization included the number of (1) PCP clinic encounters; (2) telephone encounters with primary care, endocrinology, cardiovascular service, nutritionist/dietician, or pharmacy; (3) specialty clinic encounters with endocrinology or cardiovascular services (including care management programs); (4) ED encounters; and (5) inpatient hospitalizations. We also collected data for age, sex, race, insurance type, diagnosis codes, BP, Charlson comorbidity index score,12 and HbA1c.
Data Analysis
We employed inverse probability treatment weighting (IPTW) to balance the case-mix between users and nonusers.13 We first calculated the propensity score “p” based on a logistic regression in which the predictors are age, sex, race, health conditions (hypertension and/or diabetes), and number of primary care office visits before the index date. The weights are defined as 1/p for users and 1/(1-p) for nonusers. The weights were then scaled so that the sum of weights in each group was equal to the group sample size. The subsequent weighted analysis was based on the above calculated weights.
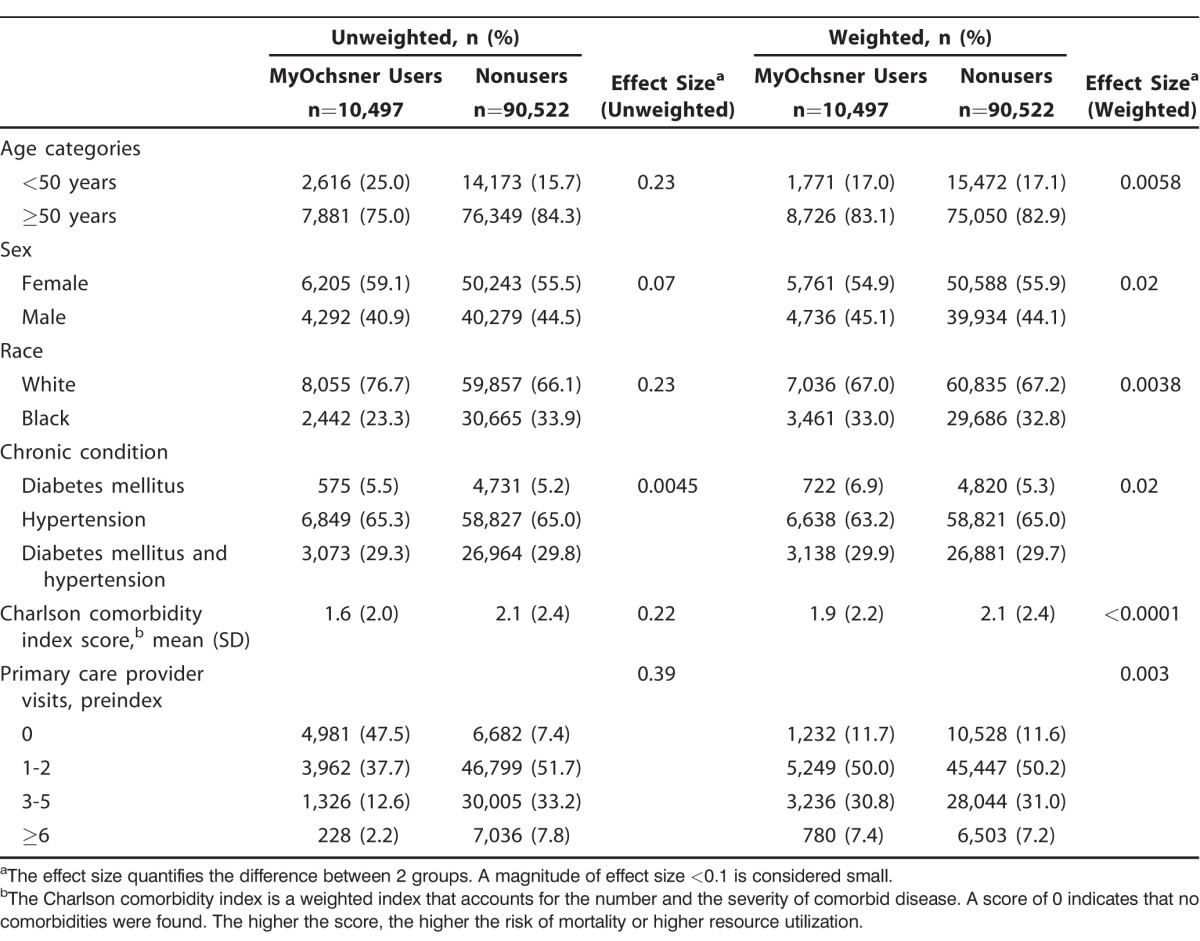
We compared patient characteristics of portal users vs nonusers using descriptive statistics (Table 2). We assessed the effect size of case-mix differences between the study groups. The effect size quantifies the difference between 2 groups regardless of sample size. We used unweighted and weighted standardized tests of differences in means for continuous variables (Charlson comorbidity index score) and in proportions for binary variables (age, sex, race) to measure effect size.12 For categorical variables (chronic condition, PCP visits), effect size was measured with the phi coefficient. The phi coefficient assesses the intercorrelation between 2 discrete variables. An effect size <0.1 is considered small and a successful application of IPTW.
Table 2.
Characteristics of MyOchsner User and Nonuser Primary Care Patients Seen Between 2012 and 2014
In the IPTW analysis of service utilization, we conducted both an unadjusted difference-in-difference analysis and an adjusted generalized estimating equation (GEE) model analysis. Our analysis focused on 5 types of healthcare encounters (PCP office visit, telephone, specialty, ED, and inpatient hospitalization) that occurred during 2 time periods: preindex (within 12 months prior to the index date) and postindex (within 12 months after the index date). The unadjusted difference-in-difference analysis of service utilization displayed in Table 3 was defined as (postindex rate for users – preindex rate for users) – (postindex rate for nonusers – preindex rate for nonusers) using a weighted t test. In the GEE analysis displayed in Table 4, we compared the encounter rates between users and nonusers (rate ratio) while adjusting for other covariates of interest. We assumed the encounter rate follows a Poisson distribution, and because all rates are yearly rates, no offsets were needed. In the GEE model, we used a log link function for the rate and the exchangeable correlation matrix as the correlation structure for each patient. The principal predictors in the model are the time indictor (preindex vs postindex), the portal user status, and the interaction term between the time indicator and the user status. Other covariates in the model are age, sex, race, baseline PCP visits, insurance type, hypertension/diabetes status, and Charlson comorbidity index score. For both the unadjusted difference-in-difference analysis and the GEE analysis (Tables 3 and 4), we report the mean yearly visit rate during the preindex and postindex periods. Because the encounter rates for specialty, ED, and inpatient hospitalization were small compared to PCP and telephone encounters, we report specialty, ED, and inpatient hospitalization encounter rates per 1,000 patients per year.
Table 3.
Unadjusted Inverse Probability Treatment Weighted Analysis of Annual Rates of Healthcare Utilization of Primary Care Patients at Baseline and After the Index Date
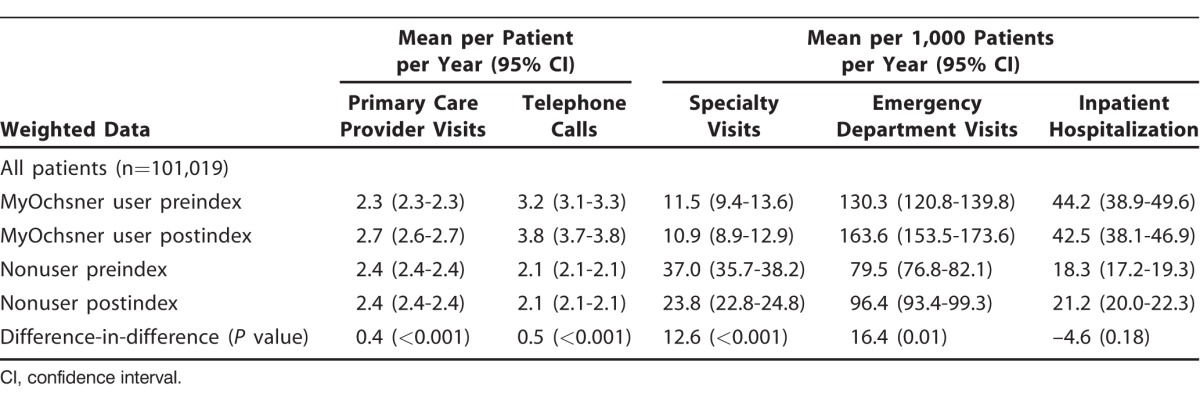
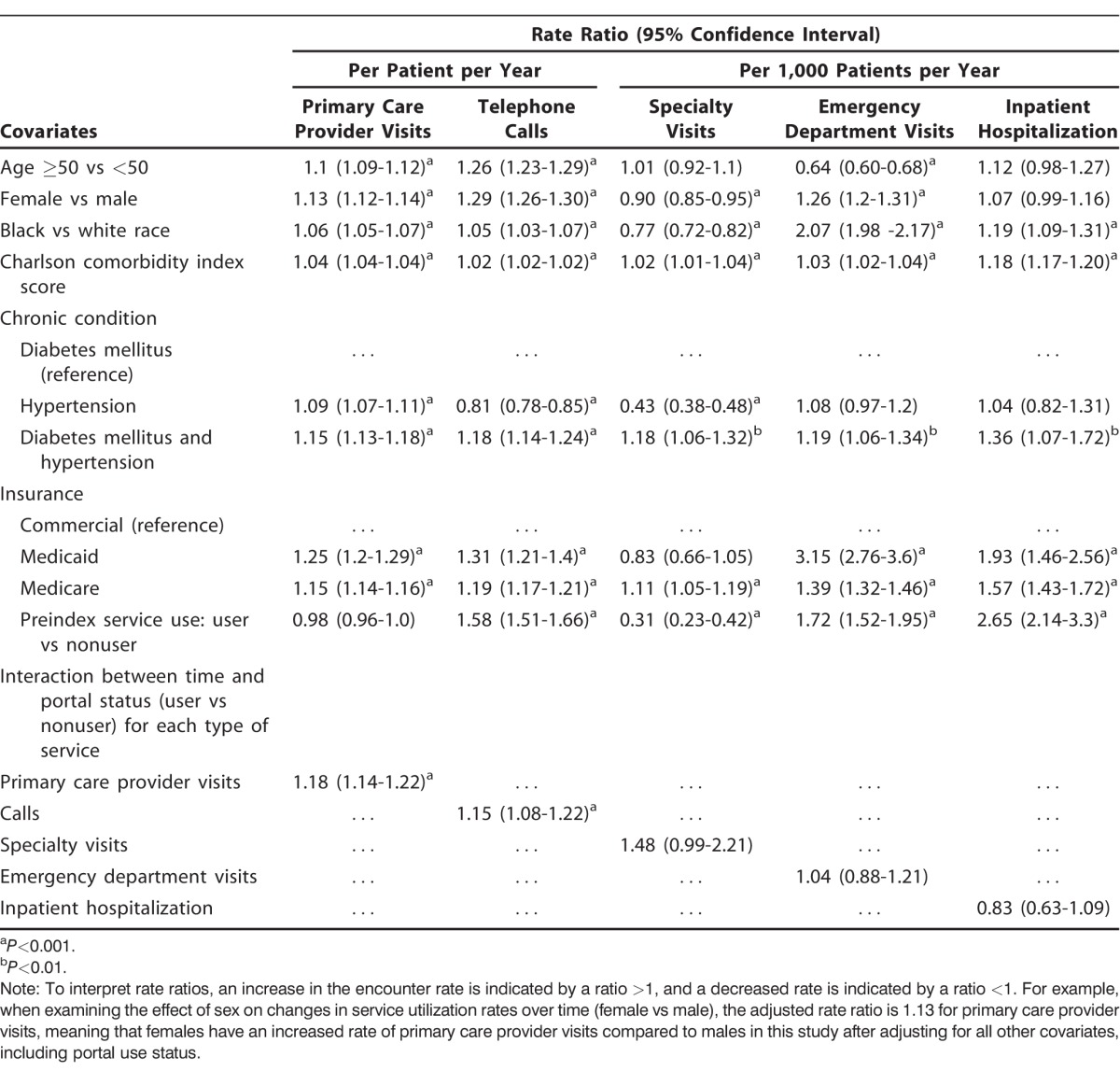
Table 4.
Generalized Estimating Equation Modeling to Compare Postindex to Preindex Service Utilization Rates Among All Patients (n=101,019)
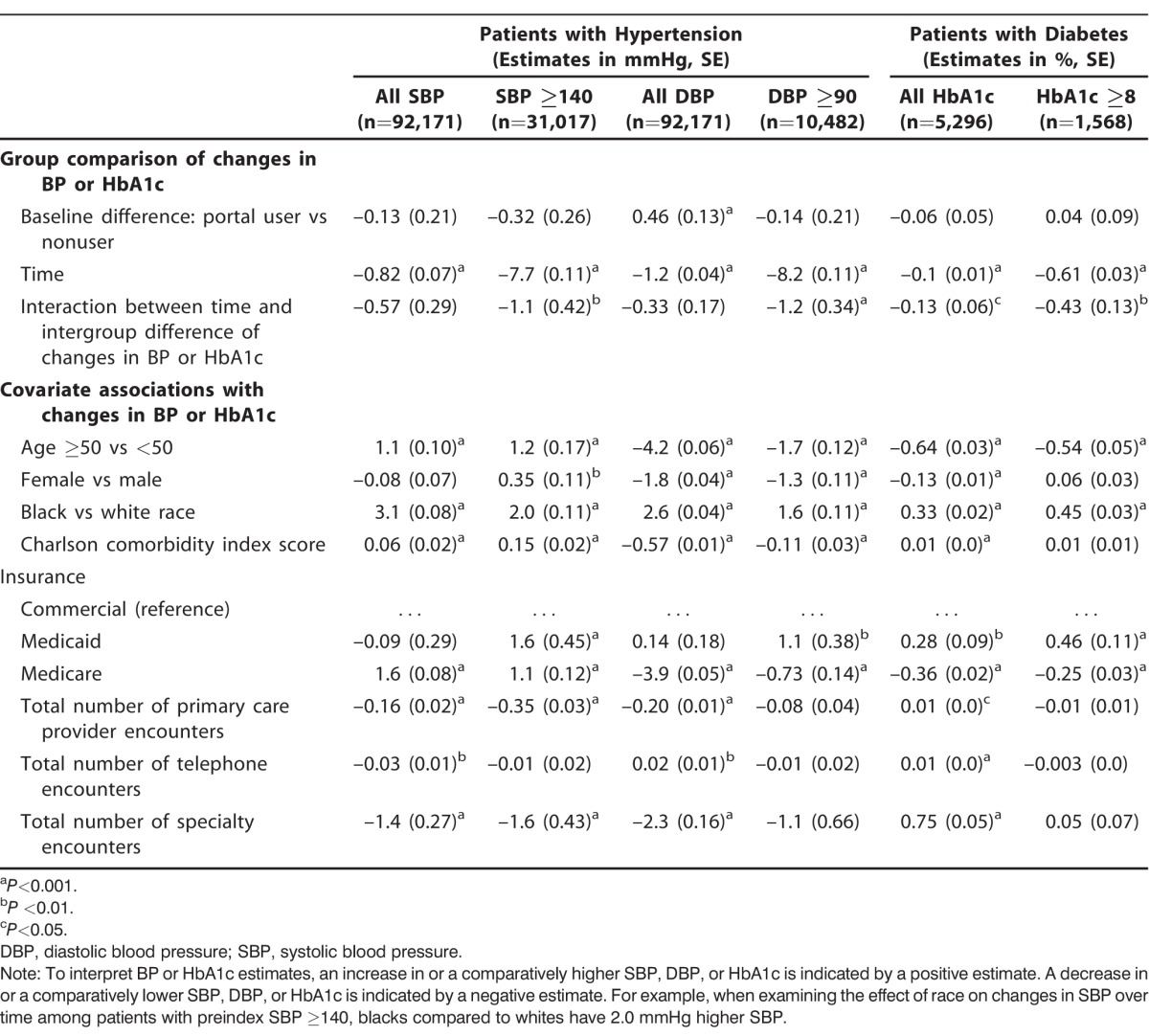
We examined the strength and direction of the association of portal use with time trends in BP and HbA1c levels using the adjusted GEE analysis. We examined changes in BP or HbA1c among patients who had at least one measurement documented in the preindex period and one measurement in the postindex period. In the GEE model, we used the identity link function. The primary predictors in the model are the time indictor (preindex vs postindex), portal user status, and the interaction term between the time indicator and user status. Other covariates in the model are age, sex, race, insurance type, Charlson comorbidity index score, annual PCP visit rate, annual telephone rate, and annual specialty encounter rate. We examined changes in BP for all patients with hypertension and stratified the analysis into patients with or without disease control in the preindex period. We repeated the analysis for all patients with diabetes and stratified the analysis by disease control status in the preindex period. The adjusted GEE analysis detailed in Table 5 was stratified to address concerns that changes in BP and HbA1c in the portal user group may represent the tendency for outliers to regress toward the mean rather than the effects of using technology. All statistical analyses were performed using SAS v.9.4 (SAS Inc.).
Table 5.
Generalized Estimating Equation Modeling to Compare Postindex to Preindex Blood Pressure (BP) and Hemoglobin A1c (HbA1c) Levels
RESULTS
Patient Characteristics
Among primary care patients seen during the study period, 101,019 patients were eligible for inclusion in the data analysis (Table 2). Most patients were age ≥50 years, female, and white, with a history of hypertension and 1 to 2 visits with their PCP in the preindex period. Approximately 90% were identified as nonusers of MyOchsner. In the unweighted analysis, the effect size of differences in patient characteristics between users and nonusers was >0.1 on all factors except for sex and chronic conditions. Additionally, in the unweighted analysis, a higher proportion of users (47.5%) compared to nonusers (7.4%) were new to Ochsner primary care during the preindex period. In the weighted data analysis, the effect size difference was <0.1 for all characteristics, indicating that IPTW reduced case-mix differences between the study groups.
Changes in Annual Rates of Service Utilization
In the unadjusted difference-in-difference analysis comparing portal users to nonusers (Table 3), the rate of PCP visits increased at a rate of 0.4 per patient per year, which among 100,000 patients translates into 40,000 visits per year (P<0.001). The rate of telephone encounters also increased among portal users compared to nonusers by 0.5 per patient per year, or 50,000 calls annually per 100,000 (P<0.001). Specialty visits increased at a rate of 12.6 per 1,000 patients per year, or 1,260 per 100,000 patients (P<0.001). ED visits increased at a rate of 16.4 per 1,000 patients per year, or 1,640 visits per 100,000 patients (P<0.01). Finally, we observed a decrease in the rate of inpatient hospitalization (–4.6 per 1,000 patients per year); however, this difference was not statistically significant.
In the adjusted GEE analysis (Table 4), multiple factors were associated with service utilization rates. Older age was associated with increased rates of PCP and telephone encounters (rate ratio >1.0) but with lower rates of ED visits (rate ratio <1.0). Females compared to males had significantly higher service utilization rates for PCP, telephone, and ED encounters but a lower rate of subspecialty visits. A similar trend was observed for black patients compared to whites except that black patients also had a significantly higher rate of inpatient hospitalization. An increased number of comorbidities (Charlson comorbidity index score) and Medicare insurance were associated with increases in utilization for all service types. Patients with Medicaid had significantly higher utilization for all service types except specialty care. Preindex rates of service utilization differed among study groups, whereby portal users compared to nonusers had significantly higher rates of telephone, ED, and inpatient hospitalization encounters and a lower rate of specialty encounters. Over time, portal users compared to nonusers had significantly higher rates of PCP and telephone encounters; however, the differences in all other encounter types were not significant.
Time Trends in Blood Pressure and Glucose
Table 5 displays the adjusted GEE analysis comparing postindex to preindex trends in BP and HbA1c. Among patients with preindex systolic BP (SBP) ≥140 mmHg or diastolic BP (DBP) ≥90 mmHg, portal users compared to nonusers had a greater decline in BP, although the between-group difference was small (mmHg [SE], –1.1 [0.42] and –1.2 [0.34], respectively; both P<0.01). Further, among patients with preindex SBP ≥140 mmHg, older age, female sex, black race, Charlson comorbidity index score, and Medicaid/Medicare insurance were significantly associated with increases in SBP, while PCP and specialty encounters were associated with decreases in SBP. In contrast, among patients with preindex DBP ≥90 mmHg, only black race and Medicaid insurance were significantly associated with increases in DBP, while older age, female sex, Charlson comorbidity index score, and Medicare were associated with decreases in DBP.
Compared to nonusers with diabetes, portal users with diabetes had greater decreases in HbA1c (all patients, % [SE], –0.13 [0.06]; patients with a preindex HbA1c ≥8, –0.43 [0.13]; both P<0.05). Among patients with a preindex HbA1c ≥8, black race and Medicaid insurance were associated with increases in HbA1c, while older age and Medicare insurance were associated with decreases in HbA1c. The relationship between HbA1c and other patient characteristics was not statistically significant.
DISCUSSION
Among patients with hypertension or diabetes, we found that portal users had higher rates of in-person PCP visits and telephone encounters; however, differences in the rates of encounters with specialty services, ED, and inpatient hospitalization were not significant. We also observed that portal use was associated with mild decreases in BP and HbA1c levels among our population. Because of the health service delivery redesign efforts that occurred concurrently with portal implementation, our findings likely reflect a combination of patient-, practice-, and system-level factors that are associated with portal use, service utilization, and clinical outcomes.
Multiple patient-level factors may explain our study findings. For example, during the study period, patients who were new to Ochsner primary care were more likely to be portal users compared to established patients. In fact, in the unweighted data, we observed a higher proportion of 0 PCP visits in the preindex period among portal users compared to nonusers. This pattern may reflect the differential impact of marketing enrollment to patients who have already established effective ways of navigating services and communicating with providers vs new patients who may readily accept portal use as the expected norm when accessing a new provider. We therefore employed IPTW to reduce case-mix differences between portal users and nonusers in our examination of the relationship between portal user status and service utilization. Notably, patients who are proactive in interacting with the health system are probably more likely to adopt portal use as another means of accessing services. Among patients with chronic illnesses, care received prior to accessing patient portals, the demand for different types of health services, and patient preferences for how to access services may contribute to patient choice about using patient portals.14 Patient race and ethnicity, education level, health literacy, degree of comorbid conditions, attitudes/preference for using technology, portal usability, and provider endorsement may also influence use.2,15 In our study, we adjusted the multivariate analysis for comorbid conditions, preindex service use patterns, and patient demographics.
Portal technology alone does not explain utilization patterns within our health system. The adult primary care services at OHS actively endorsed portal use as a practice- and system-level intervention. The portal was implemented within the context of primary care, with leadership employing lean management principles to redesign care team workflows, using nonphysician staff to reduce response times to patient portal and telephone messages, promoting same-day appointments, and increasing after-hour appointments as part of the practice reengineering strategy. There was no evidence that nonphysician contact resulted in higher utilization because of less-sophisticated care management patterns.
We observed slightly greater improvements in BP and HbA1c levels among portal users compared to nonusers. Portal use, however, may be a vehicle for and a surrogate measure of patient engagement and self-management. Our study findings contrast with Wagner et al who found that having access to personal health records had no impact on BP control, patient activation, perceptions of quality or medical utilization.11 Tenforde et al reported in an observational study that portal usage was associated with improvements in diabetes quality measures.10 Some studies have suggested that use of secure messaging may play a role in successfully achieving quality metrics for chronic disease management.7-9 Portal use in conjunction with case management appears to be the most effective strategy for engaging patients in using the technology and improving chronic disease management.2 Nonetheless, even after accounting for portal use status, our study demonstrates that a complex array of patient demographic factors may still affect clinical outcomes.
Our study has several limitations. This study reflects the experience of one organization and may have limited external generalizability. We restricted our analysis to patients with hypertension or diabetes and only examined the most common specialty services accessed by this population. We cannot draw conclusions about other populations. Nonetheless, we describe the organizational context for portal implementation to provide insights into concurrent healthcare delivery redesign strategies that may be associated with portal usage in settings utilizing similar approaches. We do not know why some patients opted to use the portal while others did not. We did not have access to measures of patient activation, health behaviors (eg, diet and exercise), health literacy, education, income/poverty level, or other social determinants of health in our sample population. We also did not have access to information about provider practice patterns (eg, medication intensification) that may influence BP and glucose control. Selection bias whereby any of these factors may have influenced portal use, utilization, or clinical outcomes remains a concern. Although randomization of patients to portal use or nonuse during systemwide implementation would have eliminated selection bias, doing so would not have been practical given the health system's priority for expanding the use of portal technology. We therefore employed IPTW, a widely accepted statistical methodology for reducing selection bias in retrospective observational studies. Because this study is retrospective, data interpretation is limited by missing or incomplete data. OHS is an open health system, and like most provider organizations, we did not have access to claims data for all payers. We do not know whether the ED encounters and inpatient hospitalization data accurately reflect patient use of these services. Estimates of the association between portal use and service utilization may be inaccurate if patients received care elsewhere. In any large study, one may find statistical differences that are not clinically significant. In contrast to the relatively small between-group differences in observed time trends for BP and HbA1c, an increase of 40,000 in-person visits and 50,000 calls represents a substantial increase in staff workload for which provider organizations must have effective workflow strategies.
CONCLUSION
In our health system, patient portal implementation emphasized improving accessibility through online scheduling and timely response to secure messaging. Chronic disease management was not a major focus in the early phases. As such, we observed clinically relevant increases in PCP and telephone encounters and smaller changes in BP and HbA1c levels (albeit trending in the desired direction). Our study was not designed to capture whether staff or providers perceived that work productivity was positively or negatively impacted by the incorporation of the patient portal into workflow redesign or whether the quality of care achieved was worth the effort. Therefore, future research must not only examine the role of specific healthcare delivery redesign strategies and portal features in mediating the relationship between portal use, service utilization, outcomes, and cost of care but simultaneously incorporate assessments of staff/provider perceptions of their work environment.
ACKNOWLEDGMENTS
The authors thank Timothy Hilbun (Research Department information analyst) and Jewel Harden-Barrios (clinical research coordinator) for their contributions to data management and Dr Pedro Cazabon (System Medical Director for Primary Care) for his critical review of the manuscript.
The authors have no financial or proprietary interest in the subject matter of this article.
This work was presented as an oral abstract at the Southern Regional Meeting for Southern Society of Clinical Investigations in February 2016.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Systems-Based Practice, and Practice-Based Learning and Improvement.
REFERENCES
- 1. Finkelstein J, Knight A, Marinopoulos S, et al. Enabling patient-centered care through health information technology. Evid Rep Technol Assess (Full Rep). 2012. June; (206):1-1531. [PMC free article] [PubMed] [Google Scholar]
- 2. Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013. November 19; 159 10: 677- 687. 10.7326/0003-4819-159-10-201311190-00006. [DOI] [PubMed] [Google Scholar]
- 3. Liss DT, Reid RJ, Grembowski D, Rutter CM, Ross TR, Fishman PA. . Changes in office visit use associated with electronic messaging and telephone encounters among patients with diabetes in the PCMH. Ann Fam Med. 2014. July; 12 4: 338- 343. 10.1370/afm.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Meng D, Palen TE, Tsai J, McLeod M, Garrido T, Qian H. . Association between secure patient-clinician email and clinical services utilisation in a US integrated health system: a retrospective cohort study. BMJ Open. 2015. November 9; 5 11: e009557 10.1136/bmjopen-2015-009557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. North F, Crane SJ, Chaudhry R, et al. Impact of patient portal secure messages and electronic visits on adult primary care office visits. Telemed J E Health. 2014. March; 20 3: 192- 198. 10.1089/tmj.2013.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Palen TE, Ross C, Powers JD, Xu S. . Association of online patient access to clinicians and medical records with use of clinical services. JAMA. 2012. November 21; 308 19: 2012- 2019. 10.1001/jama.2012.14126. [DOI] [PubMed] [Google Scholar]
- 7. Zhou YY, Kanter MH, Wang JJ, Garrido T. . Improved quality at Kaiser Permanente through e-mail between physicians and patients. Health Aff (Millwood). 2010. July; 29 7: 1370- 1375. 10.1377/hlthaff.2010.0048. [DOI] [PubMed] [Google Scholar]
- 8. Devkota B, Salas J, Sayavong S, Scherrer JF. . Use of an online patient portal and glucose control in primary care patients with diabetes. Popul Health Manag. 2016. April; 19 2: 125- 131. 10.1089/pop.2015.0034. [DOI] [PubMed] [Google Scholar]
- 9. Harris LT, Haneuse SJ, Martin DP, Ralston JD. . Diabetes quality of care and outpatient utilization associated with electronic patient-provider messaging: a cross-sectional analysis. Diabetes Care. 2009. July; 32 7: 1182- 1187. 10.2337/dc08-1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tenforde M, Nowacki A, Jain A, Hickner J. . The association between personal health record use and diabetes quality measures. J Gen Intern Med. 2012. April; 27 4: 420- 424. 10.1007/s11606-011-1889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wagner PJ, Dias J, Howard S, et al. Personal health records and hypertension control: a randomized trial. J Am Med Inform Assoc. 2012. Jul-Aug; 19 4: 626- 634. 10.1136/amiajnl-2011-000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40 5: 373- 383. [DOI] [PubMed] [Google Scholar]
- 13. Austin PC, Stuart EA. . Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015. December; 34 28: 3661- 3679. 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Riippa I, Linna M, Rönkkö I, Kröger V. . Use of an electronic patient portal among the chronically ill: an observational study. J Med Internet Res. 2014. December 8; 16 12: e275 10.2196/jmir.3722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Irizarry T, . DeVito Dabbs A, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015. June 23; 17 6: e148 10.2196/jmir.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]


