Abstract
Background:
The incidence of permanent pacemaker implantation after orthotopic heart transplantation has been reported to be 2%-24%. Transplanted hearts usually exhibit sinus rhythm in the operating room following reperfusion, and most patients do not exhibit significant arrhythmias during the postoperative period. However, among the patients who do exhibit abnormalities, pacemakers may be implanted for early sinus node dysfunction but are rarely used after 6 months. Permanent pacing is often required for atrioventricular block. A different cohort of transplant patients presents later with bradycardia requiring pacemaker implantation, reported to occur in approximately 1.5% of patients. The objectives of this study were to investigate the indications for pacemaker implantation, compare the need for pacemakers following bicaval vs biatrial anastomosis, and examine the long-term outcomes of heart transplant patients who received pacemakers.
Methods:
For this retrospective, case-cohort, single-institution study, patients were identified from clinical research and administrative transplant databases. Information was supplemented with review of the medical records. Standard statistical techniques were used, with chi-square testing for categorical variables and the 2-tailed t test for continuous variables. Survival was compared with the use of log-rank methods.
Results:
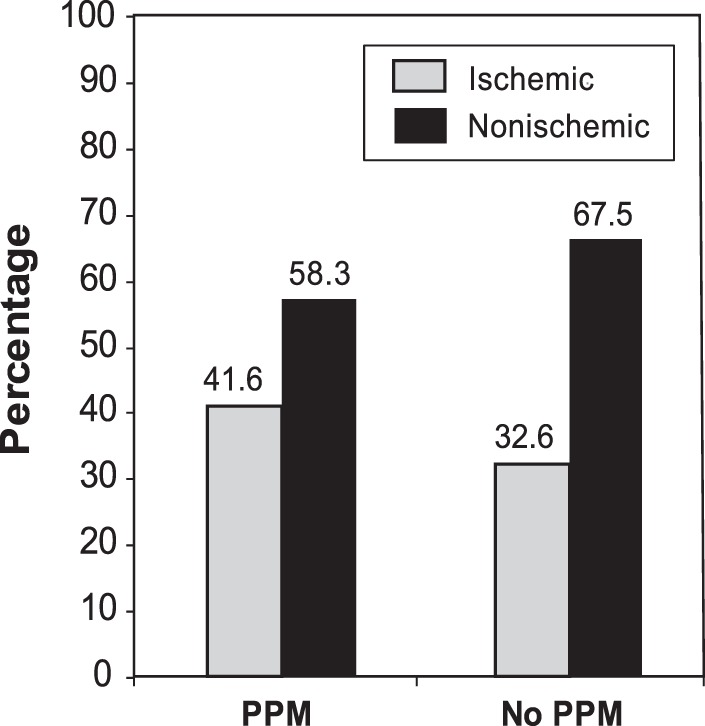
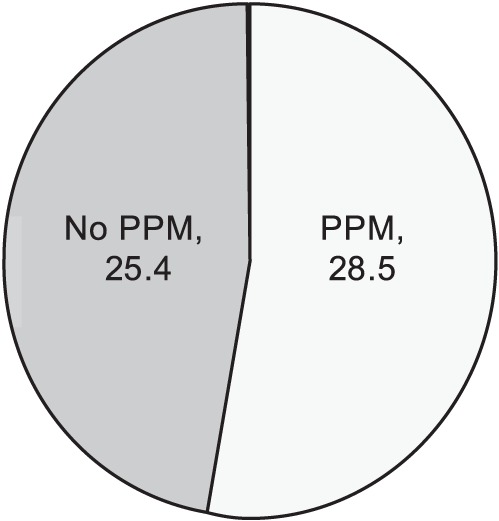
Between January 1968 and February 2008, 1,450 heart transplants were performed at Stanford University. Eighty-four patients (5.8%) were identified as having had a pacemaker implanted. Of these patients, 65.5% (55) had the device implanted within 30 days of transplantation, and 34.5% (29) had late implantation. The mean survival of patients who had an early pacemaker implant was 6.4 years compared to 7.7 years for those with a late pacemaker implant (P<0.05). Sinus node dysfunction and heart block were the most common indications for pacemaker implantation. Starting in 1997, a bicaval technique was used for implantation. The incidence of pacemaker implantation by technique was 2.0% for bicaval and 9.1% for biatrial (P=0.001). Significantly more rejection episodes occurred in the pacemaker group (2.67 ± 2.18) compared with the no-pacemaker group (2.01 ± 2.05) (P<0.05).
Conclusion:
Our results show a decreased pacemaker need after bicaval anastomosis and that more patients who needed a pacemaker after transplantation had a pretransplant diagnosis of ischemic cardiomyopathy. In our cohort, the need for a permanent pacemaker was also associated with older donor grafts and an increase in the number of treated rejection episodes.
Keywords: Heart transplantation, pacemaker-artificial, surgery
INTRODUCTION
The surgical procedure for orthotopic heart transplantation has undergone very few perturbations during the past 50 years. The early experiments by Lower and Shumway developed the standard biatrial technique of orthotopic heart transplantation.1,2 Use of the bicaval technique did not enter clinical practice until 1991.3,4 As the postoperative care of these patients became refined and standardized, the incidence of rejection and other complications was reduced. These factors resulted in increased overall survival. As a consequence of these improvements, the use of permanent pacemakers has declined.
The incidence of permanent pacemaker implantation after orthotopic heart transplantation has been reported to be 2%-24%.5,6,7 Transplanted hearts usually exhibit sinus rhythm in the operating room following reperfusion. The majority of patients experience no significant arrhythmias during the postoperative period. The most common abnormality encountered early after transplantation is sinus node dysfunction. This abnormality may be detectable only on electrophysiologic studies, or it can be clinically significant sinus or junctional bradycardia requiring pharmacologic support or pacemaker implantation. Sinus node dysfunction has been shown not to be predictive of an adverse outcome, and the majority of patients have complete resolution within the first few months to 1 year after transplantation.8 Pacemaker use is generally indicated for symptomatic bradycardia or junctional escape rhythms.9
Pacemakers implanted for early sinus node dysfunction are rarely used after 6 months; however, permanent pacing is often required for atrioventricular block. A different cohort of transplant patients presents later with bradycardia requiring pacemaker implantation, reported to occur in approximately 1.5% of patients.10 The presence of late bradycardia is an ominous sign and portends a poor outcome.
This study presents a retrospective investigation of a single-center experience that spans the first 40 years of cardiac transplantation. The goals of this study were to explore the indications for pacemaker implantation and the long-term outcomes and to directly compare pacemaker use between the biatrial and bicaval techniques. We also reviewed recipient and donor characteristics to elucidate any possible risk factors that would predispose patients to need a pacemaker following transplantation.
METHODS
This retrospective, case-cohort, single-institution study was approved by the institutional review board. Patients were identified from clinical research and transplant administrative databases. Information was supplemented with medical records review. Standard statistical techniques were used, with chi-square testing for categorical variables and the 2-tailed t test for continuous variables. Survival was compared with the use of log-rank methods, and statistical significance was defined by P<0.05.
RESULTS
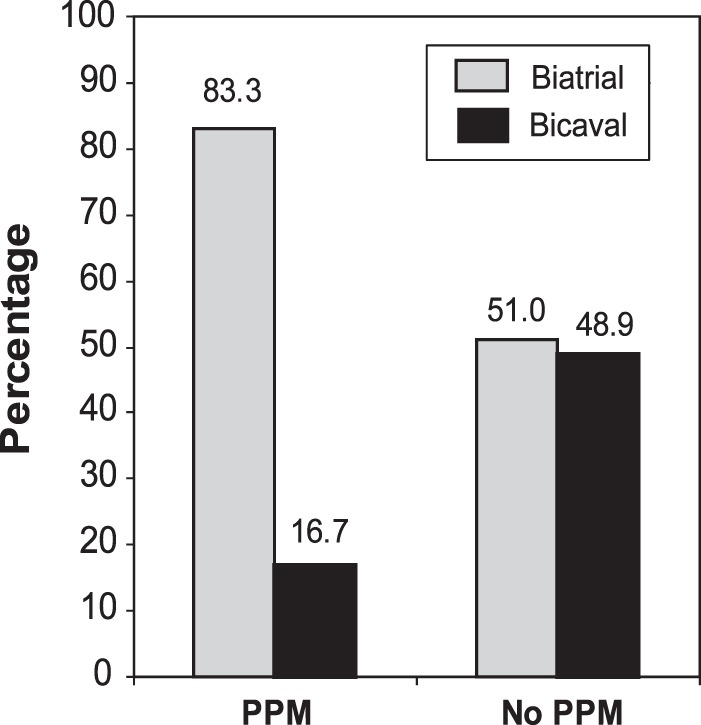
Between January 1968 and February 2008, 1,450 heart transplants were performed at Stanford University. Patient and donor demographics are presented in the Table. The bicaval technique for implantation of the donor heart was begun in 1997 at Stanford. The biatrial technique was used in 767 cases, and the bicaval implant was employed in 683. Eighty-four patients (5.8%) were identified as having had a pacemaker implanted following heart transplantation. Of these patients, 65.5% (55) had the device implanted within 30 days (early) of transplantation, and 34.5% (29) had the device implanted more than 30 days (late) after transplantation. No patients were excluded from the study. The mean survival of patients who had an early pacemaker implanted was 6.4 years compared to 7.7 years for those with late pacemaker implant (P<0.05). Sinus node dysfunction and heart block were the most common indications for pacemaker implantation. The pretransplant diagnosis of ischemic cardiomyopathy in the recipient had an increased rate of pacemaker requirement (Figure 1) (P<0.05). The incidence for pacemaker use in the bicaval group was 2.0% (14/683) compared with 9.1% (70/767) in the biatrial group (P=0.001). Of the 84 patients who received a permanent pacemaker, 83.3% had a biatrial technique and 16.7% had a bicaval technique (Figure 2). The average donor age was 28.5 years for the recipients requiring a pacemaker compared with 25.4 years for the recipients who did not (Figure 3) (P<0.05). An increased incidence of rejection episodes occurred in the pacemaker group. The mean number of rejection episodes in the pacemaker group was 2.67 ± 2.18 compared to a mean of 2.01 ± 2.05 in the cohort that did not require a pacemaker (P<0.05).
Table.
Patient and Donor Demographics
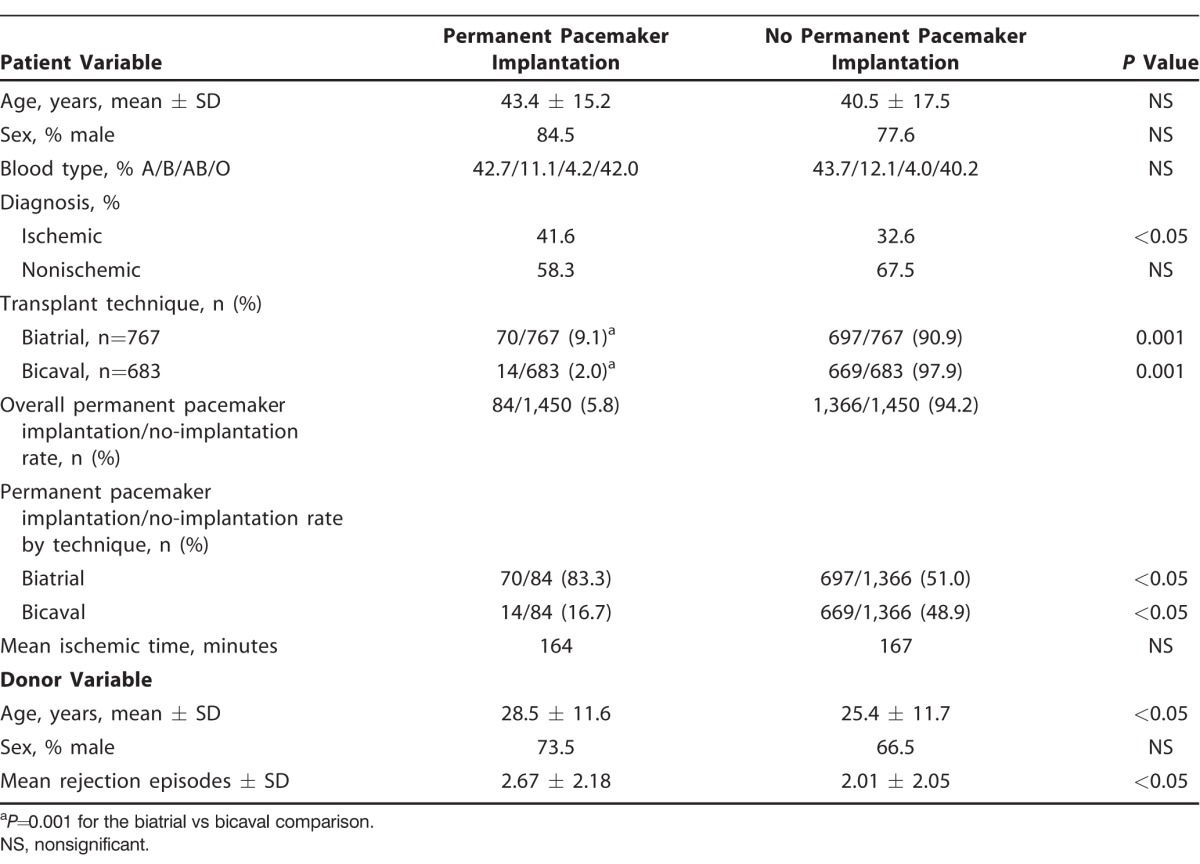
Figure 1.
Pretransplant recipient diagnosis and permanent pacemaker (PPM) rate.
Figure 2.
Surgical technique and permanent pacemaker (PPM) rate.
Figure 3.
Donor age and percentage of patients requiring permanent pacemaker (PPM).
DISCUSSION
Pacemaker use following heart transplantation falls into a bimodal distribution of early and late implantation. The early implants for bradyarrhythmias occur in the perioperative period, usually before discharge from the hospital. The recovery of the sinus node within the first 6 months usually obviates the need for permanent pacing in this cohort. The late implantation of pacemakers because of bradyarrhythmias or heart block is usually the result of an acute rejection episode or transplant vasculopathy.
The majority of transplanted hearts leave the operating room in a sinus rhythm. However, after heart transplantation, arrhythmias are a common occurrence, with ventricular arrhythmias occurring in 65% and atrial arrhythmias in 25% of patients.11 Ventricular arrhythmias usually take the form of premature ventricular complexes followed by nonsustained ventricular tachycardia. Ventricular arrhythmias are rarely malignant, usually respond to medical management, and are not associated with rejection episodes. They may be the result of metabolic disturbances or ischemia/reperfusion injuries of the allograft.11 Atrial arrhythmias are most commonly premature atrial complexes, with flutter, fibrillation, and tachycardia occurring rarely. Atrial arrhythmias have been associated with acute rejection episodes and respond to treatment of acute rejection. Outside the setting of acute rejection, they respond to rapid atrial pacing, beta blockers, or cardioversion.11 None of these arrhythmias is an indication for implanting a permanent pacemaker.
Sinus node dysfunction occurs with great frequency after heart transplantation but is usually managed without a permanent pacemaker. Up to half of transplanted hearts exhibit sinus node dysfunction based on electrophysiologic studies in the immediate posttransplant period.12 Surgical trauma, surgical technique, myocardial preservation and reperfusion, cardiac denervation, and underlying donor characteristics may all play a role in posttransplant sinus node dysfunction. A previous study from Stanford demonstrated an increased incidence of abnormal sinoatrial node artery in patients requiring pacemakers and suggested that disruption of the sinoatrial nodal blood supply may be an important factor in the development of bradycardia after transplant.5 In the early postoperative period, clinically relevant sinus bradycardia with a heart rate <80 bpm should be managed with atrial pacing or the administration of medications such as isoproterenol or theophylline. Adenosine released from the ischemic myocardium possibly contributes to early sinus node dysfunction.10,12,13 The use of theophylline, an adenosine receptor antagonist, can reverse bradycardia after heart transplantation, allow the withdrawal of chronotropic support, and reduce the need for permanent pacemaker implantation.14 Rate augmentation with isoproterenol has been used at Stanford since the early era of cardiac transplantation to augment graft function.15
Because of the benign and transient nature of early sinus node dysfunction, the indications for pacemaker implantation are difficult to standardize. Many patients with early sinus node dysfunction and bradycardia are not pacemaker dependent at 3 months; however, those with early atrioventricular block require long-term pacing.16,17 Patients with symptomatic bradycardia, those with impaired cardiac output, and individuals with atrioventricular block and a junctional rhythm should probably have a dual-chamber pacemaker implanted. Whenever possible, pacing the atria is advisable to maximize the atrial contribution to ventricular function.18
As stated earlier, late pacemaker implantation following heart transplantation is often a presenting sign of a rejection episode or severe transplant vasculopathy. Late bradycardia has been defined from 30 days to more than 5 or 6 months after transplantation and occurs in approximately 1.5% of patients.6,10,19 In this study, late need for pacemaker was defined at 30 days. When bradycardia is associated with a rejection episode, it usually responds to antirejection therapy. Bradycardia presenting late after heart transplantation has been associated with an increased incidence of transplant coronary artery disease that may be the result of the ischemia involving the sinoatrial node.20 The patient presenting with bradycardia or heart block late after transplantation should be aggressively worked up for rejection and vasculopathy with echocardiography, endomyocardial biopsy, and coronary angiography. Despite pacemaker implantation, many of these patients succumb to the underlying disease process—often with a precipitous decline—and retransplantation should be considered.21
The overall pacemaker rate reported in this study is lower than that reported in 2 other large studies. In this series, the overall rate for permanent pacemaker implantation was 5.8% compared with 8.1%19 in a prospective study at the Cleveland Clinic and 10.9% in a review of the United Network for Organ Sharing database.22 While many factors may account for this difference, it may be attributable to variation in the institutional use of permanent pacemakers following heart transplantation. Bradyarrhythmias can be managed through a range of therapies, including temporary pacing, pharmacology, and permanent pacemaker implantation. The thresholds for placing a permanent pacemaker after heart transplantation likely vary widely among individual programs.
Even though the surgical technique for heart transplantation has changed little during the years, much debate continues about the merits of biatrial vs bicaval anastomosis. The perceived advantages of performing the biatrial anastomosis are that it is technically easier than the bicaval technique and reduces the donor ischemic time. The theoretical advantages of performing the bicaval technique are that the intact donor right atrium can contribute to right ventricular function, the incidence of tricuspid valve insufficiency may be lower compared to the biatrial technique, and the rate of permanent pacemaker implantation also appears to be lower.
Several studies have demonstrated a decreased need for permanent pacemaker implantation in the bicaval group compared to the biatrial group.6,7,19,22-24 Although the incidence of pacing appears to be lower with the bicaval technique, this advantage was not evident in our study as the donor age increased. The average donor age was 28.5 years in the recipients requiring a pacemaker compared with 25.4 years among patients who did not (P<0.05). Pacing requirements are similar between techniques when using older donors. Increasing donor age is accompanied by an increased risk of needing a pacemaker, and the benefit of the bicaval technique is not seen in this patient population.19,22,25,26 The use of the bicaval anastomosis has been shown to decrease the incidence of atrial arrhythmias that occur late after cardiac transplantation, perhaps because of the integrity of the donor right atrium in the bicaval group.19,22,27
CONCLUSION
A permanent pacemaker after heart transplantation may be required in the early postoperative period or much later after the transplant event. Our study and others show a decreased rate of pacemaker use with the bicaval technique when compared with the biatrial method. In our cohort, more patients who needed a pacemaker after transplantation had a pretransplant diagnosis of ischemic cardiomyopathy. Increasing donor age and an increase in the number of treated rejection episodes both resulted in a higher percentage of patients requiring permanent pacemaker insertion regardless of the technique employed.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, and Practice-Based Learning and Improvement.
REFERENCES
- 1. Lower RR, Shumway NE. . Studies on orthotopic homotransplantation of the canine heart. Surg Forum. 1960; 11: 18- 19. [PubMed] [Google Scholar]
- 2. Shumway NE, Lower RR, Stofer RC. . Transplantation of the heart. Adv Surg. 1966; 2: 265- 284. [PubMed] [Google Scholar]
- 3. Dreyfus G, Jebara V, Mihaileanu S, Carpentier AF. . Total orthotopic heart transplantation: an alternative to the standard technique. Ann Thorac Surg. 1991. November; 52 5: 1181- 1184. [DOI] [PubMed] [Google Scholar]
- 4. Trento A, Takkenberg JM, Czer LS, et al. Clinical experience with one hundred consecutive patients undergoing orthotopic heart transplantation with bicaval and pulmonary venous anastomoses. J Thorac Cardiovasc Surg. 1996. December; 112 6: 1496- 1502; discussion 1502-1503. [DOI] [PubMed] [Google Scholar]
- 5. DiBiase A, Tse TM, Schnittger I, Wexler L, Stinson EB, Valantine HA. . Frequency and mechanism of bradycardia in cardiac transplant recipients and need for pacemakers. Am J Cardiol. 1991. June 15; 67 16: 1385- 1389. [DOI] [PubMed] [Google Scholar]
- 6. Woo GW, Schofield RS, Pauly DF, et al. Incidence, predictors, and outcomes of cardiac pacing after cardiac transplantation: an 11-year retrospective analysis. Transplantation. 2008. April 27; 85 8: 1216- 1218. 10.1097/TP.0b013e31816b677c. [DOI] [PubMed] [Google Scholar]
- 7. Weiss ES, Nwakanma LU, Russell SB, Conte JV, Shah AS. . Outcomes in bicaval versus biatrial techniques in heart transplantation: an analysis of the UNOS database. J Heart Lung Transplant. 2008. February; 27 2: 178- 183. 10.1016/j.healun.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 8. Heinz G, Kratochwill C, Koller-Strametz J, et al. Benign prognosis of early sinus node dysfunction after orthotopic cardiac transplantation. Pacing Clin Electrophysiol. 1998. February; 21 2: 422- 429. [DOI] [PubMed] [Google Scholar]
- 9. Scott CD, Dark JH, McComb JM. . Sinus node function after cardiac transplantation. J Am Coll Cardiol. 1994. November 1; 24 5: 1334- 1341. [DOI] [PubMed] [Google Scholar]
- 10. Miyamoto Y, Curtiss EI, Kormos RL, Armitage JM, Hardesty RL, Griffith BP. . Bradyarrhythmia after heart transplantation. Incidence, time course, and outcome. Circulation. 1990. November; 82 5 Suppl: IV313- IV317. [PubMed] [Google Scholar]
- 11. Little RE, Kay GN, Epstein AE, et al. Arrhythmias after orthotopic cardiac transplantation. Prevalence and determinants during initial hospitalization and late follow-up. Circulation. 1989. November; 80 5 Pt 2: III140- III146. [PubMed] [Google Scholar]
- 12. Jacquet L, Ziady G, Stein K, et al. Cardiac rhythm disturbances early after orthotopic heart transplantation: prevalence and clinical importance of the observed abnormalities. J Am Coll Cardiol. 1990. October; 16 4: 832- 837. [DOI] [PubMed] [Google Scholar]
- 13. Heinz G, Ohner T, Laufer G, Gössinger H, Gasic S, Laczkovics A. . Demographic and perioperative factors associated with initial and prolonged sinus node dysfunction after orthotopic heart transplantation. The impact of ischemic time. Transplantation. 1991. Jun:51(6);1217-1224. [DOI] [PubMed] [Google Scholar]
- 14. Bertolet BD, Eagle DA, Conti JB, Mills RM, Belardinelli L. . Bradycardia after heart transplantation: reversal with theophylline. J Am Coll Cardiol. 1996. August; 28 2: 396- 399. [DOI] [PubMed] [Google Scholar]
- 15. Stinson EB, Caves PK, Griepp RB, Oyer PE, Rider AK, Shumway NE. . Hemodynamic observations in the early period after human heart transplantation. J Thorac Cardiovasc Surg. 1975. February; 69 2: 264- 270. [PubMed] [Google Scholar]
- 16. Raghavan C, Maloney JD, Nitta J, et al. Long-term follow-up of heart transplant recipients requiring permanent pacemakers. J Heart Lung Transplant. 1995. Nov-Dec; 14 6 Pt 1: 1081- 1089. [PubMed] [Google Scholar]
- 17. Scott CD, McComb JM, Dark JH, Bexton RS. . Permanent pacing after cardiac transplantation. Br Heart J. 1993. May; 69 5: 399- 403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chartrand C, Angell WW, Dong E Jr, Shumway NE. . Atrial pacing in the postoperative management of cardiac homotransplantations. Ann Thorac Surg. 1969. August; 8 2: 152- 160. [DOI] [PubMed] [Google Scholar]
- 19. Cantillon DJ, Gorodeski EZ, Caccamo M, et al. Long-term outcomes and clinical predictors for pacing after cardiac transplantation. J Heart Lung Transplant. 2009. August; 28 8: 791- 798. 10.1016/j.healun.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 20. Gullestad L, Ross H, Myers J, et al. Importance of decreased heart rate in predicting transplant coronary artery disease. Clin Transplant. 1997. December; 11 6: 628- 632. [PubMed] [Google Scholar]
- 21. Blanche C, Czer LS, Fishbein MC, Takkenberg JJ, Trento A. . Permanent pacemaker for rejection episodes after heart transplantation: a poor prognostic sign. Ann Thorac Surg. 1995. November; 60 5: 1263- 1266. [DOI] [PubMed] [Google Scholar]
- 22. Cantillon DJ, Tarakji KG, Hu T, et al. Long-term outcomes and clinical predictors for pacemaker-requiring bradyarrhythmias after cardiac transplantation: analysis of the UNOS/OPTN cardiac transplant database. Heart Rhythm. 2010. November; 7 11: 1567- 1571. 10.1016/j.hrthm.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 23. Meyer SR, Modry DL, Bainey K, et al. Declining need for permanent pacemaker insertion with the bicaval technique of orthotopic heart transplantation. Can J Cardiol. 2005. February; 21 2: 159- 163. [PubMed] [Google Scholar]
- 24. Herre JM, Barnhart GR, Llano A. . Cardiac pacemakers in the transplanted heart: short term with the biatrial anastomosis and unnecessary with the bicaval anastomosis. Curr Opin Cardiol. 2000. March; 15 2: 115- 120. [DOI] [PubMed] [Google Scholar]
- 25. Zieroth S, Ross H, Rao V, et al. Permanent pacing after cardiac transplantation in the era of extended donors. J Heart Lung Transplant. 2006. Sep: 25 9: 1142-1147. [DOI] [PubMed] [Google Scholar]
- 26. Chau EM, McGregor CG, Rodeheffer RJ, et al. Increased incidence of chronotropic incompetence in older donor hearts. J Heart Lung Transplant. 1995. Jul-Aug; 14 4: 743- 748. [PubMed] [Google Scholar]
- 27. Brandt M, Harringer W, Hirt SW, et al. Influence of bicaval anastomoses on late occurrence of atrial arrhythmia after heart transplantation. Ann Thorac Surg. 1997. July; 64 1: 70- 72. [DOI] [PubMed] [Google Scholar]


