Abstract
This study described discharge prescription medication errors written for emergency department patients. This study used content analysis in a cross-sectional design to systematically categorize prescription errors found in a report of 1000 discharge prescriptions submitted in the electronic medical record in February 2015. Two pharmacy team members reviewed the discharge prescription list for errors. Open-ended data were coded by an additional rater for agreement on coding categories. Coding was based upon majority rule. Descriptive statistics were used to address the study objective. Categories evaluated were patient age, provider type, drug class, and type and time of error. The discharge prescription error rate out of 1000 prescriptions was 13.4%, with “incomplete or inadequate prescription” being the most commonly detected error (58.2%). The adult and pediatric error rates were 11.7% and 22.7%, respectively. The antibiotics reviewed had the highest number of errors. The highest within-class error rates were with antianginal medications, antiparasitic medications, antacids, appetite stimulants, and probiotics. Emergency medicine residents wrote the highest percentage of prescriptions (46.7%) and had an error rate of 9.2%. Residents of other specialties wrote 340 prescriptions and had an error rate of 20.9%. Errors occurred most often between 10:00 am and 6:00 pm.
According to the Food and Drug Administration, there have been over 95,000 reports of medication errors to MedWatch since 2000, with the number of actual errors estimated as even higher (1). The National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance project showed that nearly 17% of 700,000 US patients treated annually for adverse drug events in the emergency department (ED) require hospitalization (2, 3). The ED's increasing patient volumes, pressure to see more patients in shorter amounts of time, lack of continuity of care, and unfamiliar patients all play a role in the development of medication errors (4, 5). Despite computerized provider order entry and decision support tools in place to prevent prescribing errors in the ED, high error rates of 10% to 21% persist (5–9). Cesarz et al found that out of 674 ED discharge prescriptions reviewed, 68 prescriptions required intervention to prevent errors and optimize therapy (54% and 46%, respectively) (6). This study provided evidence to support pharmacist prescription review in the ED, but it lacked the description of what prescriptions required interventions most often and for what reason, the time of day the interventions occurred most frequently, and what providers were most likely to need intervention. The current study aimed to describe those specifics regarding discharge prescription errors in an academic medical center ED.
METHODS
This study was approved by the study site's institutional review board. This study was a retrospective chart review that used content analysis in a cross-sectional design to systematically categorize prescription errors found in a report capturing a convenience sample of the first 1000 discharge prescriptions written and submitted in the electronic medical record (Meditech 6.8) in February 2015. Providers for these visits included emergency medicine (EM) attending physicians, EM residents, attending physicians from other specialties, and resident physicians from other specialties. All prescriptions written during this timeframe were included in the analysis.
The study site is an urban academic medical center with an annual ED volume of approximately 48,000 patients. The ED has 48 hours of EM faculty physician coverage daily (four 12-hour shifts: 7:00 am–7:00 pm, 9:00 am–9:00 pm, 1:00 pm–1:00 am, and 7:00 pm–7:00 am). An EM clinical pharmacist is available on site from 8:00 am to 4:30 pm and is physically present in the ED from 11:00 am to 4:30 pm focusing on drug information questions, drug dosing, and medication reconciliation. Numerous EM, off-service, and pharmacy residents also are present in the department.
The primary objective of this study was to identify the percentage of prescription errors in a sample of discharge prescriptions from an academic medical ED. The secondary objectives were to describe errors based on 1) patient age, 2) type of error that occurred, 3) medication class, 4) prescriber type, and 5) time of day the prescription was written.
Data collected from the electronic medical record included a list of discharge prescriptions (drug name, strength, dose, route, frequency, dispense quantity, number of refills), sex of the patient, patient age, weight (in kg), time of day the prescription was printed, and provider type. Prescribing errors were categorized into three broad categories (with subcategories also listed): incomplete/inadequate prescription (directions missing/“as directed,” directions unclear, quantity calculated in error, quantity missing, quantity sufficient with number of days' supply not indicated), dosing outside recommended range (below recommended dose, duration outside recommended range, over recommended dose, frequency outside recommended range), and drug selection error (direction/dosage mismatch, dosage form not available, not recommended for age, wrong dosage form).
One pharmacy intern and one clinical pharmacist reviewed the discharge prescription list for errors following training in error identification. Open-ended data were viewed by an additional clinical pharmacist for agreement on categories. The final prescription data set evaluated was compiled based on the majority's decision of whether a prescription error occurred. The errors were then evaluated based on the primary and secondary outcomes listed above. Excel was used to evaluate data and formulate results.
RESULTS
Out of 1000 discharge prescriptions, prescribing errors were present in 134 (13.4%). The number of prescriptions written for adults and pediatric patients were 846 and 154, respectively. Of the 134 total prescription errors, 35 (26.1%) were for pediatric patients, which is an age group error rate of 22.7%. The adult prescription error rate was 11.7% (99 prescriptions with errors out of 846). The most common prescription error type was “incomplete/inadequate prescription,” with “directions missing/as directed” the most common subcategory error. The most frequently prescribed medications that fell into this category of error were prednisone, albuterol, and azithromycin. Table 1 shows the subtypes of errors detected, including frequencies.
Table 1.
Types of prescription errors detected
| Type | Errors |
|
|---|---|---|
| N | % | |
| Incomplete/inadequate prescription | 78 | 58.2% |
| Directions missing/noting only “take as directed” | 25 | 18.7% |
| Directions unclear | 13 | 9.7% |
| Quantity calculated in error | 19 | 14.2% |
| Quantity missing | 12 | 9.0% |
| Quantity sufficient but no indication of number of days | 9 | 6.7% |
| Dosing outside recommended range | 27 | 20.1% |
| Below recommended dose | 7 | 5.2% |
| Duration outside recommended range | 1 | 0.7% |
| Higher than recommended dose | 12 | 9.0% |
| Frequency outside recommended range | 5 | 3.7% |
| Other (unable to find indication for nonprocedural use) | 2 | 1.5% |
| Drug selection errors | 29 | 21.6% |
| Direction/dosage mismatch | 17 | 12.7% |
| Dosage form not available | 6 | 4.5% |
| Not recommended for age | 1 | 0.7% |
| Wrong dosage form | 5 | 3.7% |
Fifty-two classes of medications were prescribed. The drug class with the highest number of prescription errors was antibiotics, resulting in a within-class error rate of 14.9%. Within this category, errors were found most frequently in prescriptions written for azithromycin and amoxicillin. Azithromycin errors found were “directions missing/as directed,” “quantity calculated in error,” “directions unclear,” or “duration outside recommended range.” Amoxicillin errors found were either “quantity missing” or “quantity sufficient but with number of days' supply not indicated.” Eleven of the 23 antibiotic prescription errors were for pediatric patients. The medication classes with 50% or higher within-class error rates included antianginal medications, antiparasitic medications, antacids, appetite stimulants, probiotics, nebulized medications, and insulin. Table 2 lists the frequencies of error rates by drug class.
Table 2.
Prescription errors organized by medication class
| Class | Prescriptions | Errors | Errors in class (%) | Class's % of total errors |
|---|---|---|---|---|
| Antibiotic | 154 | 23 | 14.9% | 17.2% |
| Analgesic | 141 | 5 | 3.5% | 3.7% |
| Antiemetic | 106 | 9 | 8.5% | 6.7% |
| Inhaler | 77 | 5 | 6.5% | 3.7% |
| Corticosteroid | 54 | 16 | 29.6% | 11.9% |
| Antihypertensive | 42 | 7 | 16.7% | 5.2% |
| Topical | 30 | 13 | 43.3% | 9.7% |
| Proton pump inhibitor | 26 | 11 | 42.3% | 8.2% |
| Muscle relaxer | 24 | 1 | 4.2% | 0.7% |
| Nebulized medication | 22 | 14 | 63.6% | 10.4% |
| Antiplatelet | 19 | 1 | 5.3% | 0.7% |
| Antiepileptic | 18 | 1 | 5.6% | 0.7% |
| Supplement | 15 | 4 | 26.7% | 3.0% |
| Diuretic | 15 | 1 | 6.7% | 0.7% |
| Ophthalmic | 12 | 3 | 25.0% | 2.2% |
| Antiviral | 10 | 2 | 20.0% | 1.5% |
| Benzodiazepine | 10 | 1 | 10.0% | 0.7% |
| Laxative | 7 | 1 | 14.3% | 0.7% |
| Insulin | 5 | 3 | 60.0% | 2.2% |
| Antipsychotic | 5 | 2 | 40.0% | 1.5% |
| Anticoagulant | 5 | 1 | 20.0% | 0.7% |
| Nasal | 5 | 1 | 20.0% | 0.7% |
| Anticholinergic | 3 | 1 | 33.3% | 0.7% |
| Otic | 3 | 1 | 33.3% | 0.7% |
| Antianginal | 2 | 2 | 100.0% | 1.5% |
| Antiparasitic | 2 | 2 | 100.0% | 1.5% |
| Antacid | 1 | 1 | 100.0% | 0.7% |
| Appetite stimulant | 1 | 1 | 100.0% | 0.7% |
| Probiotic | 1 | 1 | 100.0% | 0.7% |
Forty-four individual physicians wrote ED discharge prescriptions. EM attending physicians and residents were responsible for 40.3% of the total errors that were identified. The error rate was 6.1% for EM attending physicians, 9.2% for EM residents, 69.2% for non-EM attending physicians, and 20.9% for non-EM residents (Table 3).
Table 3.
Prescription errors organized by provider type
| Physician type | Rx written | Percentage of total Rx written | Errors | Percentage of total errors | Percentage of Rx with errors |
|---|---|---|---|---|---|
| EM attending | 180 | 18% | 11 | 8.2% | 6.1% |
| EM resident | 467 | 46.7% | 43 | 32.1% | 9.2% |
| Non-EM attending | 13 | 1.3% | 9 | 6.7% | 69.2% |
| Non-EM resident | 340 | 34% | 71 | 53.0% | 20.9% |
EM indicates emergency medicine; Rx, prescriptions.
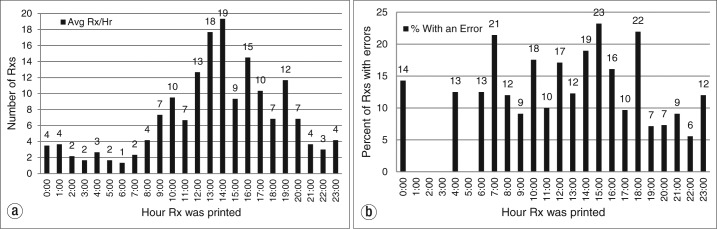
The average rate of prescriptions written per hour over the study period was 6.9, with rates increasing around 10:00 am, peaking at 2:00 pm, and decreasing around 8:00 pm (Figure 1a). Most prescription errors occurred between 10:00 am and 6:00 pm (104 errors, 77.6%), and particularly between 2:00 pm and 3:00 pm (22 errors, or 19% of all prescriptions written) (Figure 1b).
Figure 1.
(a) Average number of prescriptions (Rx) written per hour. (b) Percentage of prescription errors per hour.
DISCUSSION
This study shows that nearly 14% of discharge prescriptions written in the ED contain medication errors. The finding that nearly half of the errors in antibiotic prescriptions were for children is concerning. The potential for underdose or overdose is present and can impact the patient response and recovery for the condition for which the antibiotics were prescribed. Reasons for incorrect dosing of an antibiotic may be due to incorrect weight-based dosing or simply not being able to visualize the label comments or handwritten edits on “take as directed” antibiotics.
The type of error that occurred most frequently was missing directions or simply noting “take as directed”—which was also found in a study conducted by the Institute for Safe Medication Practices (10). Many patients may be unable to remember specific administration directions given by a practitioner without written instruction as a backup. Similar to the study by Bizovi et al (11), medication prescriptions with fill-in prepopulated information were prone to errors. If a specific medication regimen was incorrect in a prepopulated “favorite prescriptions” list, then it may have been incorrect for all of the prescriptions printed for that medication by that physician. Also, the lack of directly available dosage calculators and decision support aids may have contributed to a greater chance for inaccurate dosing, especially for weight-based medications. Errors were also observed when the dose and frequency of liquid solutions or suspensions were included but the quantity to be dispensed was “1 bottle” instead of the specific bottle size needed. Also seen were prescriptions where the package size was left in the dose category, such as a 30 g tube of hydrocortisone 1% cream printed as “Hydrocortisone 1% cream 30 g, 30 applications TP daily #1 tube.” Dose and package size interchange may lead to patient confusion, supratherapeutic doses, and adverse events.
In the ED, analgesics, muscle relaxers, antiepileptics, and inhalers are often prescribed in acute care patient visits, supporting the low within-class error rate seen in this study. Seventeen percent of all prescription errors were written for antibiotics, paralleling other medication error identification studies (8, 12). Other classes of drugs that demonstrated high levels of prescription errors were nebulized, topical, and steroid medications. These are all medications that require special instructions, and counseling should be given both verbally and via the prescription label to maximize patient understanding. Medications less frequently prescribed, such as antiparasitics, antianginals, nebulized medications, and appetite stimulants, may be less familiar to physicians, and therefore may be more prone to errors. Knowing the classes of medications that have high within-class error rates as well as high total error rates may help determine appropriate educational and quality improvement interventions.
The error rate for EM residents was higher than that for EM attending physicians. The prescription error rates were highest for off-service resident and attending physicians. Medication regimens used by off-service disciplines can be significantly different from those prescribed in the ED setting. This suggests a potential need for better orientation of these residents to the types of prescriptions written in the ED and potentially more oversight and input from attending physicians, pharmacists, and nurses.
Unsurprisingly, the greatest amount of prescription errors occurred during the busiest time of day for an ED, from 10:00 am to 6:00 pm. There were 641 prescriptions written during this time frame, 104 of which contained an error. This result is proportional to the number of patients roomed in the ED at the time of prescription printing, increasing the demand on providers and expectedly dividing their focus.
Dedicating more ED pharmacist, pharmacy resident, or student time to prescription review during peak hours of patient care could help minimize errors. EM pharmacists have the advanced knowledge and skill set to help reduce patient harm through minimization of prescription medication errors. The data showing that pharmacists improve the error rates for medications is robust, showing a positive impact on medication errors (12), decreasing unintended medications being continued from medication reconciliation (13), reducing pediatric adverse drug events (14, 15), reducing pediatric prescription errors (16), and reducing ED prescription errors (6). A dedicated discharge prescription reviewing policy may be prudent; however, implementation could have an impact on ED metrics such as total length of stay in the ED for those being discharged. Pharmacists could also conduct in-service training regarding the importance of electronically correcting prescriptions in lieu of hand-correcting the already printed version.
This study is not without its limitations. The prescriptions reviewed spanned a 6-day period and represented a small subset of physicians. Also, any handwritten prescription corrections or handwritten prescriptions that may have been distributed during these 6 days were not included in the analysis. Additionally, the potential for harm or delay of patient receipt was not assessable. Finally, interobserver variability was not formally assessed, and classification bias cannot be ruled out.
This pilot study can help researchers springboard into more robust research, including confirmation of error rate with a larger sample size, design of interventions to help reduce error rates, improvement of error rates after the educational intervention in this particular academic medical center ED, and further solidification of the positive impact an ED pharmacist can have on discharge prescription error rates.
References
- 1.Food and Drug Administration. Avoiding medication mistakes (updated 8/31/15) Available at http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048644.htm; accessed November 20, 2015.
- 2.Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296(15):1858–1866. doi: 10.1001/jama.296.15.1858. [DOI] [PubMed] [Google Scholar]
- 3.Budnitz DS, Shehab N, Kegler SR, Richards CL. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med. 2007;147(11):755–765. doi: 10.7326/0003-4819-147-11-200712040-00006. [DOI] [PubMed] [Google Scholar]
- 4.Lifshitz AE, Goldstein LH, Sharist M, Strugo R, Asulin E, Haim SB, Feigenberg Z, Berkovitch M, Kozer E. Medication prescribing errors in the prehospital setting and in the ED. Am J Emerg Med. 2012;30(5):726–731. doi: 10.1016/j.ajem.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 5.Sard BE, Walsh KE, Doros G, Hannon M, Moschetti W, Bauchner H. Retrospective evaluation of a computerized physician order entry adaptation to prevent prescribing errors in a pediatric emergency department. Pediatrics. 2008;122(4):782–787. doi: 10.1542/peds.2007-3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cesarz JL, Steffenhagen AL, Svenson J, Hamedani AG. Emergency department discharge prescription interventions by emergency medicine pharmacists. Ann Emerg Med. 2013;61(2):209–214. doi: 10.1016/j.annemergmed.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terrell KM, Perkins AJ, Dexter PR, Hui SL, Callahan CM, Miller DK. Computerized decision support to reduce potentially inappropriate prescribing to older emergency department patients: a randomized controlled trial. J Am Geriatr Soc. 2009;57(8):1388–1394. doi: 10.1111/j.1532-5415.2009.02352.x. [DOI] [PubMed] [Google Scholar]
- 8.Condren M, Studebaker IJ, John BM. Prescribing errors in a pediatric clinic. Clin Pediatr. 2009;49(1):49–53. doi: 10.1177/0009922809342459. [DOI] [PubMed] [Google Scholar]
- 9.Taylor BL, Selbst SM, Shah AEC. Prescription writing errors in the pediatric emergency department. Pediatr Emerg Care. 2005;21(12):822–827. doi: 10.1097/01.pec.0000190239.04094.72. [DOI] [PubMed] [Google Scholar]
- 10.Acute Care IMSP Safety Alert. “Use as directed” can cause confusion for both patients and practitioners Horsham, PA: Institute for Safe Medication Practices, August 2016. Available at http://www.ismp.org/newsletters/acutecare/showarticle.aspx?id=1146; accessed January 25, 2017. [Google Scholar]
- 11.Bizovi KE, Beckley BE, McDade MC, Adams AL, Lowe RA, Zechnich AD, Hedges JR. The effect of computer-assisted prescription writing on emergency department prescription errors. Acad Emerg Med. 2002;9(11):1168–1175. doi: 10.1111/j.1553-2712.2002.tb01572.x. [DOI] [PubMed] [Google Scholar]
- 12.Kuo GM, Touchette DR, Marinac JS. Drug errors and related interventions reported by United States clinical pharmacists: the American College of Clinical Pharmacy Practice-Based Research Network medication error detection amelioration and prevention study. Pharmacotherapy. 2013;33(3):253–265. doi: 10.1002/phar.1195. [DOI] [PubMed] [Google Scholar]
- 13.Leguelinel-Blache G, Arnaud F, Bouvet S, Dubois F, Castelli C, Roux-Marson C, Ray V, Sotto A, Kinowski JM. Impact of admission medication reconciliation performed by clinical pharmacists on medication safety. Eur J Intern Med. 2014;25(9):808–814. doi: 10.1016/j.ejim.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, Goldmann DA. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 15.Condren M, Honey BL, Carter SM, Ngo N, Landsaw J, Bryant C, Gillaspy S. Influence of a systems-based approach to prescribing errors in a pediatric resident clinic. Acad Pediatr. 2014;14(5):485–490. doi: 10.1016/j.acap.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 16.Winder MB, Johnson JL, Planas LG, Crosby KM, Gildon BL, Oberst-Walsh LA. Pharmacist-led educational and error notification interventions on prescribing errors in family medicine clinic. J Am Pharm Assoc. 2015;55(3):238–245. doi: 10.1331/JAPhA.2015.14130. [DOI] [PubMed] [Google Scholar]