Abstract
Objective
Case volume-outcome associations bolster arguments to regionalize severe sepsis care, an approach that may necessitate inter-hospital patient transfers. Although transferred patients may most closely reflect care processes involved with regionalization, associations between sepsis case volume and outcomes among transferred patients are unclear. We investigated case volume-outcome associations among patients with severe sepsis transferred from another hospital.
Design
Serial cross-sectional study using the Nationwide Inpatient Sample
Setting
United States non-federal hospitals, years 2003 to 2011.
Patients
141,707 patients (weighted national estimate of 717, 732) with severe sepsis transferred from another acute care hospital.
Interventions
None
Measurements and Main Results
We examined associations between quintiles of annual hospital severe sepsis case volume for the receiving hospital and in-hospital mortality among transferred patients with severe sepsis. Secondary outcomes included hospital length of stay (LOS) and total charges. Transferred patients accounted for 13.2% of hospitalized severe sepsis cases. In-hospital mortality was 33.2%, with median LOS 11 days (interquartile range 5 – 22), and median total charge $70,722 (interquartile range, $30,591–$159,013). Patients transferred to highest volume hospitals had higher predicted mortality risk, greater number of acutely dysfunctional organs and lower adjusted in-hospital mortality as compared to the lowest volume hospitals (OR 0.80; 95% CI, 0.67–0.90). In stratified analysis, (P<0.001 for interaction of case volume by organ failure) mortality benefit associated with case volume was limited to patients with single organ dysfunction (N = 48,607, 34.3% of transfers) (OR 0.66; 95% CI, 0.55–0.80). Treatment at highest volume hospitals was significantly associated with shorter adjusted LOS (incidence rate ratio 0.86; 95% CI 0.75–0.98), but not costs (% charge difference, 95% CI: (−)18.8, (−)37.9 – (+) 0.3).
Conclusions
Hospital mortality was lowest among patients with severe sepsis who were transferred to high volume hospitals, however case volume benefits for transferred patients may be limited to patients with lower illness severity.
Keywords: severe sepsis, septic shock, case volume, mortality, outcomes
INTRODUCTION
The incidence of severe sepsis is increasing in the United States.(1–3) Despite a trend towards improved in-hospital mortality over the past decade, (4–6) severe sepsis is associated with greater than 50% of hospital deaths,(7) remains a leading cause of death in the United States(8) and costs the U.S. health care system about $24 billion annually.(9) Early recognition and timely treatment of severe sepsis remains a principal determinant of outcome.(10–14) Similar to patients with stroke,(15–17) trauma,(18) myocardial infarction(19, 20) and cardiac arrest,(21) multiple studies have observed better outcomes for patients with severe sepsis treated at high-volume centers.(22–25)
Case volume-outcome associations for severe sepsis may argue for efforts to regionalize care.(26, 27) Approaches that leverage case volume-outcome relationships through regionalization of care will likely necessitate inter-hospital transfer of patients. However, previous studies of volume-outcome associations in severe sepsis have systematically excluded patients who are most likely to be representative of those most affected by regionalization of care: patients transferred into another acute care hospital. Given the time-sensitive nature of severe sepsis treatment, a system of regionalization of care may paradoxically worsen outcomes if the gains in care processes at high volume hospitals are lost in care delays due to extra travel time and transfers. In order to better characterize the impact of regionalization of severe sepsis care, we sought to characterize the case volume-outcome associations among patients transferred into another acute care hospital with severe sepsis. We hypothesized that patients with severe sepsis who were transferred to higher volume hospitals would have lower in-hospital mortality than patients transferred to lower volume hospitals.
MATERIALS AND METHODS
We performed a serial cross sectional study of severe sepsis hospitalizations using the Nationwide Inpatient Samples (NIS) data from 2003 to 2011.The NIS is a 20% stratified sample of U.S. acute care hospitals, and contains approximately 8 million hospital stays annually, broadly representing admissions to regular hospital wards as well as intensive care units (ICU). The characteristics of the NIS, developed as part of the Healthcare Cost and Utilization Project (HCUP) by the Agency for Healthcare Research and Quality (AHRQ), has been previously described.(24) The Institutional Review Board at Geisinger Medical Center, Danville, PA deemed this study exempt due to its use of de-identified administrative data.
Case Identification
Sepsis definitions that were in place prior to the third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)(28) were utilized for case identification. In accordance with these pre-existing definitions by the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference,(29, 30) severe sepsis was classified as sepsis complicated by organ dysfunction (Martin et al(2)) or patients assigned International Classification of Diseases, Ninth Revision (ICD-9) codes for severe sepsis [995.92] and septic shock [785.52], a previously-validated approach with high positive predictive values of greater than 95%.(31, 32) We excluded patients who were less than 18 years of age. The specifics of ICD-9 coding for organ dysfunction and septicemia are outlined in Supplemental Table 1. ICD-9 codes for transferred patients in the NIS relate to the destination hospital stay.
Patient and Hospital Characteristics
The primary exposure variable was annual hospital severe sepsis case volume. We classified hospitals into case volume quintiles (Q1 – Q5) based on the total annual number of severe sepsis hospitalizations (including transferred and non-transferred patients). Quintile cut-off points were chosen to ensure approximately even distribution of hospital-year observations across the quintile categories in the final sample. Transferred patients were defined as those hospitalizations in the NIS data set whose admission source was designated as being from another acute care hospital. Non-transferred patients were defined as those who presented directly to the receiving hospital either through the emergency department or directly from home or a long term care facility. The primary outcome variable was in-hospital mortality. We also determined length of stay (LOS) and hospital charges as secondary outcomes. Co-morbidities were identified based on ICD-9 codes using previously published methods for comorbidity identification and adjustments in administrative datasets.(33) Patient severity of illness was captured using the All Patient Refined Diagnosis Related Groups (APR-DRG).(34) Patient demographic information included age, gender, race, median household income of patient’s zip code, primary insurance payer (Medicare, Medicaid, private), discharge disposition (home, transfer to another short-term hospital, skilled nursing facility and intermediate care facility and death). Hospital characteristics included geographic region, urban versus rural location, ownership, teaching status and bed size.
Statistical Analysis
Descriptive statistics for categorical variables were presented as frequencies and percentages, with comparisons across case volume quintile groups made using ANOVA test of independence. Comparisons of characteristics of transferred patients in relation to non-transferred patients was done using Pearson chi-square test for categorical characteristics and independent t test for continuous variables. A set of multivariable regression models were estimated for the relationship between case volume category and each of the three outcome variables of interest. We used logistic regression models to investigate mortality outcomes, Poisson regression for LOS(35) and log-linked gamma distribution generalized linear model to evaluate hospital charges. In all models, robust standard errors were calculated to account for hospital clustering.
For each of the three dependent variables of interest (mortality, LOS, and total charge), the regression model adjusted for the number of organ dysfunction variables, interaction terms between volume and organ dysfunction, patient gender, age, APR-DRG Mortality Risk category and 29 Elixhauser comorbid conditions, payor type, patient’s median zip code income level (to serve as a proxy for patient’s income level), and a set of hospital characteristics, such as teaching status, geographical region, number of beds, and control/ownership status. In addition, NIS data year indicator variables were included to capture secular trends over time during the study period. Due to a significant interaction of case volume by organ failure (P<0.001), we further explored the relationship between hospital volume of severe sepsis and mortality in subgroups of transferred patients stratified by number of organ dysfunction.
Unadjusted and adjusted odds ratios (OR) and incidence rate ratios (IRR) with 95 % confidence intervals (CI), and corresponding p-values were reported for in-hospital mortality and LOS respectively. For total charges, we reported percentage changes in dollar amount relative to the reference group, with corresponding 95% CI. All hypothesis tests were 2-sided with a significance alpha level of 0.05. All analyses were performed with SAS PROC SURVEY methodology using SAS version 9.1 for Windows (SAS Institute Inc. Cary, NC) and Stata version 13.0 (StataCorp LP. College Station, TX).
Sensitivity Analysis
Processes of care can differ markedly for patients admitted with severe sepsis as opposed to those who develop nosocomial sepsis.(25) Because the NIS lacks ‘present on admission’ modifiers to ICD-9 codes and is therefore limited in its ability to distinguish between patients with severe sepsis on admission and those that did not, we performed sensitivity analysis on transferred patients in the NIS with principal diagnosis (DX1) ICD-9 codes of 038 (septicemia), 785 (shock), or 995 (including systemic inflammatory response syndrome, sepsis and severe sepsis) who most likely represented patients admitted with severe sepsis.
Exploratory Analyses
We performed an exploratory stratified analysis investigating the relationship between case volume and hospital mortality according to surgical vs. non-surgical hospitalization status. Surgical hospitalizations were identified from the HCUP Surgical Software using the “narrow” definition of major therapeutic operating room procedure based upon ICD9 procedure codes.(36)
We also performed exploratory analysis for the primary outcome to investigate whether the need for organ-replacement or organ-support therapy might be associated with greater benefit of high case volume hospitals.(37) For this analysis, we utilized a surrogate for early organ dysfunction by examining procedure day in the NIS to identify patients with dialysis or mechanical ventilation on hospital days 0, 1 or 2. For dialysis, we captured patients with new dialysis for acute renal failure by identifying patients with ICD-9-CM acute failure code (584) plus a dialysis procedure code (39.95).(38) For mechanical ventilation procedures, we identified patients with ICD-9-CM code 96.7×(39) (where × can be 0,1, or 2).
RESULTS
Severe Sepsis Case Characteristics
Over a 9-year study period, we identified 141,707 (weighted population estimate: 717, 732) transferred patients with severe sepsis representing 13.2% of all hospitalized severe sepsis cases (Figure 1). Hospitals with higher total severe sepsis case volume had correspondingly higher volumes of transferred patients with severe sepsis (correlation coefficient 0.67, P<0.001). Characteristics of transferred severe sepsis hospitalizations by quintiles of total severe sepsis case volume are shown in Table 1. Severe sepsis patients who were transferred to the highest quintile hospitals were younger, had higher proportions of surgical hospitalizations, higher predicted mortality risks, more acute organ dysfunctions and were more likely to be discharged to home than patients transferred to the lowest case volume hospitals.
Figure 1.

Flow Chart of Severe Sepsis Case Identification and Selection
Table 1.
Characteristics of Transferred Patients with Severe Sepsis
| Annual Case Volumea | ||||||
|---|---|---|---|---|---|---|
| Variable | Total | Quintile 1 (≤ 40) |
Quintile 2 (41 – 101) |
Quintile 3 (102 – 193) |
Quintile 4 (194 – 358) |
Quintile 5 (>358) |
| Cases of Severe Sepsis na | 1,076,385 | 46,658 | 93,604 | 156,589 | 262,109 | 517,425 |
| Cases of Severe Sepsis Transferred nb | 141,707 | 5,629 | 12,648 | 14,797 | 30,596 | 78,037 |
| Hospital-Year Observations nb | 4,383 | 889 | 869 | 872 | 885 | 868 |
| Transferred Patients Onlyb | ||||||
| Age, years, mean (SD) | 68.3 (16.1) | 70.7 (14.3) | 70.4 (14.8) | 69.9 (15.6) | 68.8 (15.9) | 67.4 (16.6) |
| Female (%)c | 48.9 | 49.1 | 49.2 | 49.2 | 49.4 | 48.6 |
| Race (%) | ||||||
| White | 57.9 | 61.6 | 54.3 | 57.2 | 57.9 | 58.3 |
| Black | 13.0 | 10.9 | 12.4 | 9.7 | 12.8 | 13.9 |
| Hispanic | 5.9 | 5.4 | 7.7 | 5.6 | 6.4 | 5.5 |
| Asian/Pacific Islander | 2.0 | 1.2 | 2.1 | 1.8 | 2.4 | 1.9 |
| Native American | 0.7 | 0.8 | 1.3 | 0.6 | 0.6 | 0.8 |
| Severe Sepsis Code 995.92 (%) | 54.4 | 31.4 | 37.2 | 49.2 | 55 | 59.7 |
| Surgical Intervention (%)d | 26.0 | 16.4 | 17.3 | 23.3 | 26.4 | 28.4 |
| Comorbid conditions (%) | ||||||
| Metastatic Cancer | 4.0 | 2.7 | 2.9 | 3.4 | 4.2 | 4.3 |
| Congestive heart failure | 27.7 | 29.7 | 28.1 | 28.8 | 28.5 | 26.9 |
| Chronic pulmonary disease | 21.2 | 25.1 | 24.2 | 23.3 | 22.7 | 19.5 |
| Coagulopathy | 14.9 | 10.4 | 10.3 | 12.2 | 14.3 | 16.7 |
| Liver disease | 5.2 | 3.3 | 3.3 | 4 | 5.3 | 5.9 |
| Renal failure | 24.4 | 24.5 | 25.9 | 23.8 | 24.5 | 24.3 |
| APR-DRG Mortality Risk (%) | ||||||
| Extreme likelihood of dying | 82.5 | 70.4 | 76.8 | 80.6 | 82.3 | 84.8 |
| Major likelihood of dying | 15.9 | 26.5 | 21.5 | 17.7 | 15.8 | 13.9 |
| Moderate likelihood of dying | 1.3 | 2.3 | 1.5 | 1.6 | 1.3 | 1.2 |
| Minor likelihood | 0.2 | 0.8 | 0.2 | 0.2 | 0.6 | 0.1 |
| Organ dysfunction (%) | ||||||
| Cardiovascular | 51.6 | 33.0 | 37.8 | 47.9 | 51.6 | 55.9 |
| Respiratory | 47.2 | 43.8 | 47.2 | 45.3 | 48 | 47.5 |
| Neurologic | 7.5 | 7.7 | 8.2 | 7.4 | 7 | 7.6 |
| Hematologic | 15.6 | 11.4 | 11.2 | 13.6 | 15.5 | 17.1 |
| Hepatic | 6.6 | 3.2 | 3.6 | 5.1 | 6.2 | 7.9 |
| Renal | 56.9 | 45.6 | 49.6 | 53.9 | 54.9 | 60.2 |
| Metabolic | 19.0 | 9.4 | 11.3 | 15.7 | 18 | 21.9 |
| Discharge Disposition (%)e | ||||||
| Home | 9.8 | 6.7 | 6.6 | 8.7 | 9.8 | 10.7 |
| Other short-term hospital | 5.1 | 15.6 | 11.2 | 6.4 | 4.1 | 3.5 |
| Skilled nursing/intermediate care |
51.4 | 45.6 | 50.3 | 50.1 | 50.1 | 52.8 |
| Other or unknown | 0.6 | 0.4 | 0.3 | 0.6 | 0.6 | 0.6 |
| Number of Organ Dysfunction (%) | ||||||
| Any 1 | 34.3 | 54.7 | 46.5 | 37.8 | 34.4 | 30.1 |
| Any 2 | 23.5 | 24.9 | 26.1 | 26 | 23.8 | 22.4 |
| Any 3 | 18.6 | 12.9 | 16 | 17.8 | 19.5 | 19.2 |
| Any 4+ | 23.6 | 7.4 | 11.4 | 18.5 | 22.4 | 28.3 |
| Primary payer (%) | ||||||
| Medicare | 69.3 | 77.6 | 75.5 | 73.2 | 69.5 | 66.8 |
| Medicaid | 9.3 | 4.3 | 6.1 | 7.5 | 9.9 | 10.2 |
| Private insurance | 16.7 | 15.0 | 14.8 | 15 | 16 | 17.7 |
| Self-pay | 2.2 | 1.2 | 1.3 | 1.7 | 2.1 | 2.5 |
| No charge | 0.2 | 0.1 | 0.2 | 0.1 | 0.1 | 0.2 |
| Other | 2.4 | 1.8 | 2 | 2.4 | 2.3 | 2.6 |
| Median income in zip code (%) | ||||||
| Quartile 1 | 31.3 | 41.9 | 38.4 | 30 | 30.3 | 30.1 |
| Quartile 2 | 26.8 | 28.3 | 27.2 | 28.3 | 28.8 | 25.6 |
| Quartile 3 | 22.5 | 19.6 | 19.2 | 22 | 21.5 | 23.7 |
| Quartile 4 | 19.4 | 10.2 | 15.2 | 19.7 | 19.5 | 20.6 |
Includes all severe sepsis cases, both transferred and non-transferred patients
Includes only transferred patients
P=0.15 All other comparisons statistically significant to P < 0.001 by ANOVA test of independence
Surgery as defined by HCUP Surgical Software “narrow” definition
Death as a disposition not included
APR-DRG – All Patient Refined-Diagnosis Related Group
Severe Sepsis Case Volume and Hospital Mortality
In-hospital mortality among transferred patients with severe sepsis was 33.2%. This compares to a mortality of 28.8% among non-transferred patients, who have been the focus of prior studies of case volume associations in severe sepsis (P<0.001; Supplemental Table 2). Unadjusted mortality among transferred patients was similar in highest case volume quintile when compared to the lowest case volume quintile (Q5 vs. Q1 32.4%, 31.8%; Supplemental Table 3). Multivariable adjusted models showed lower mortality for patients transferred into high case volume hospitals - OR Q5 vs. Q1: 0.80, (95% CI: 0.67–0.95) (Figure 2). We explored the relationship between hospital volume of severe sepsis and mortality stratified by number of organ dysfunction (P<0.001 for interaction of case volume by organ failure). Two-thirds (65.7%) of transferred patients with severe sepsis had two or more organ dysfunctions. Highest volume hospitals were more likely to treat patients with four or more organ dysfunctions (Table 1). Among patients with a single organ dysfunction, patients treated at the higher volume hospitals had improved odds of inpatient survival - OR Q5 vs. Q1: 0.66, (95% CI: 0.55–0.80). In contrast, there was no significant difference in mortality between hospital volume groups in severe sepsis patients with greater than one organ dysfunction (Table 2).
Figure 2.
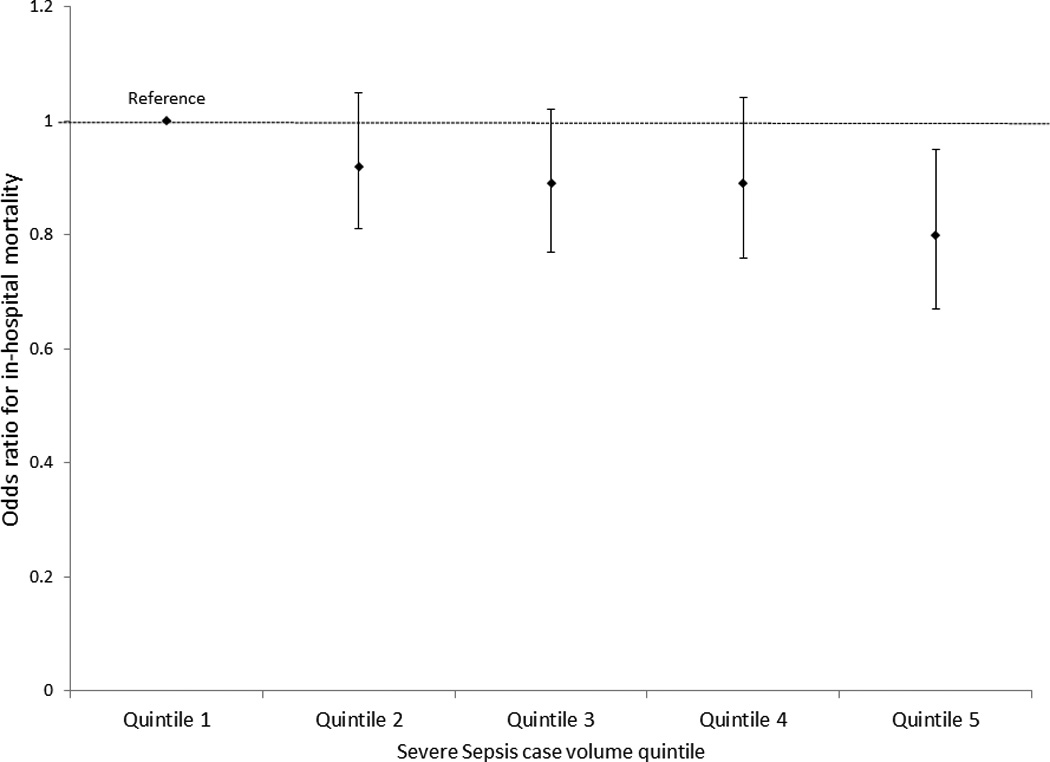
Odds Ratio and 95% Confidence Intervals for In-hospital Mortality by Quintiles of Severe Sepsis Case Volume
Table 2.
Case Volume and Adjusted Risk of In-hospital Mortality by Number of Organ Dysfunction
| Organ Dysfunction | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 |
|---|---|---|---|---|---|
| Any 1, N=48,605 | (reference) | 0.84 (0.72, 0.98) | 0.79 (0.67, 0.94) | 0.77 (0.64, 0.93) | 0.66 (0.55, 0.80) |
| Any 2, N=33,301 | (reference) | 1.04 (0.86, 1.25) | 1.03 (0.85, 1.25) | 0.97 (0.80, 1.18) | 0.87 (0.70, 1.08) |
| Any 3, N=26,358 | (reference) | 1.12 (0.89, 1.40) | 1.06 (0.85, 1.33) | 1.09 (0.86, 1.37) | 0.93 (0.73, 1.18) |
| Any 4+, N=33,443 | (reference) | 0.89 (0.69, 1.16) | 0.94 (0.72, 1.21) | 1.05 (0.80, 1.37) | 1.03 (0.78, 1.34) |
P < 0.001 for Case Volume by Organ Failure interaction term
In sensitivity analysis, 76.8% of our study cohort (N=108,815) had a principal diagnosis for sepsis, severe sepsis, or septic shock. Analysis of this patient subgroup showed association between hospital mortality and severe sepsis case volume similar to the primary analysis - OR Q5 vs. Q1: 0.61, (95% CI: 0.49–0.76) among patients with single organ dysfunction (Supplemental Tables 4A & 4B).
In post hoc exploratory analysis, we identified 26% (N=36,804) of transferred patients with severe sepsis as surgical hospitalizations. Subgroup analysis stratified by surgical and non-surgical hospitalizations showed results similar to the primary analysis of the general sample (Supplemental Tables 5A and 5B).
Organ-Support Therapy and Mortality
The most prevalent organ system dysfunctions in our NIS cohort of transferred patients with severe sepsis were renal (56.9%), cardiovascular (51.6%) and respiratory (47.2%). In exploratory analysis, we identified 40,783 patients with early need for hemodialysis or mechanical ventilation. In this patient subgroup, there was no difference in adjusted in-hospital mortality between the lowest volume hospitals and other hospital volume groups - OR Q5 vs. Q1: 1.08 (95% CI: 0.86 – 1.37) (Supplemental Table 6).
Severe Sepsis Case Volume and Secondary Outcomes
Crude LOS and total charges by case volume quintiles are illustrated in Supplemental Table 3. In adjusted analysis (Table 3), severe sepsis patients treated at higher-volume (quintiles 3 to 5) hospitals had significantly shorter adjusted length of stay, compared to the lowest-volume hospitals - IRR Q5 vs Q1: 0.86, (95% CI: 0.75–0.98). We found no association between severe sepsis case volume and adjusted total charges - % charge difference Q5 vs. Q1: (−)18.8, (95% CI: (−)37.9 – (+) 0.3).
Table 3.
Incidence Rate Ratio for Length of Stay and Percentage Total Charge Difference with 95% Confidence Intervals
| Variable | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 |
|---|---|---|---|---|---|
|
Length of Stay IRR (95% CI) |
(reference) | 0.98 (0.90, 1.06) | 0.86 (0.77, 0.97) | 0.85 (0.75, 0.96) | 0.86 (0.75, 0.98) |
|
Total Charges % Difference (95% CI) |
(reference) | −3.2 (−16.6, 10.2) | −8.9 (−24.3, 6.6) | −16.5 (−33.1, 0.1) | −18.8 (−37.9, 0.3) |
DISCUSSION
In this 9-year serial cross-sectional study using a nationally representative sample of patients transferred to another hospital with severe sepsis, we found significant association between higher case volume and lower adjusted in-hospital mortality. Patients with severe sepsis transferred into the highest volume hospitals generally had higher predicted mortality risks and a greater number of acute organ dysfunctions. However, improved mortality associated with high case volume was limited to transferred patients with a single acute organ dysfunction. Mortality benefits of high case volume was also similar for surgical hospitalizations compared to non-surgical hospitalizations among transferred patients with severe sepsis. Although LOS was shorter at higher severe sepsis case volume hospitals, costs did not differ based upon case volume.
The evidence for volume-outcome associations among severe sepsis patients in the United States continues to evolve, with two previous studies having evaluated case volume and mortality among severe sepsis patients in the United States. In a study of 124 academic US hospitals, Walkey et al demonstrated a 7% absolute reduction in adjusted mortality from severe sepsis in the highest case volume quartile academic hospitals compared to their lowest volume quartile counterparts. Gaeski and colleagues, in a study of 900,000 patients with severe sepsis over a 7-year period from a diverse mix of hospitals in the NIS demonstrated a 2–3% decrease in hospital mortality for every increase of 100 cases/year in annual hospital volume of severe sepsis, with the volume outcome relationship limited to patients who had fewer than 4 organ dysfunctions. Our study adds to the body of knowledge on volume-outcome relationships in severe sepsis by specifically evaluating patients transferred with severe sepsis, who may better represent the care processes implemented during regionalization. Our findings suggest that patients currently transferred to other hospitals with severe sepsis are more severely ill than non-transferred patients, with higher mortality (33.2% vs 28.1%). Despite the generally higher severity of illness of transferred patients, higher case volume hospitals had potential mortality benefits only among the least severely ill transferred patients with severe sepsis. Taken in the context of prior studies, higher case volume appeared to benefit a more narrow group of transferred patients than non-transferred patients.
The limited potential benefits of case volume among transferred patients may be attributable to different processes of care involved with inter-hospital transfer during severe sepsis. A recent single-center study(40) showed that inter-hospital transfer from local community hospitals to a tertiary academic center delayed appropriate antibiotic therapy and timely fluid administration for patients with severe sepsis and septic shock - cornerstones of early severe sepsis treatment. It is possible that the presence of greater organ dysfunction in our study may represent progression of sepsis-induced organ dysfunction during inter-hospital transfer, a hypothesis that requires further study.
Our study suggests a possible mismatch between current care for patients with severe sepsis and apparent benefits of inter-hospital transfer. Severe sepsis patients with higher severity of illness and greater numbers of acutely dysfunctional organ systems are more likely to be transferred to hospitals with higher case volume. However, increasing organ dysfunction was associated with declining benefits of transfer to high case volume hospitals among transferred patients.
The need for surgical interventions may trigger transfer to higher volume centers. In fact, surgical hospitalizations were more prevalent among high case volume hospitals in our sample of transferred patients with severe sepsis. However, associations between case volume and mortality were similar regardless of whether transferred patients with sepsis received a surgical intervention. Prior studies that excluded transferred patients had not identified case volume-outcome associations for surgical patients with severe sepsis.(25)
The need for advanced organ support with mechanical ventilation and dialysis may also trigger transfer to higher volume hospitals. Indeed, in our US cohort, dialysis and mechanical ventilation were more prevalent among high case volume hospitals. However, the evidence supporting volume-outcome associations with these critical care procedures is not consistent. For example some studies have found inverse relationships between mortality and hospital volume of mechanically ventilated patients and critically ill patients who receipt renal replacement therapy,(37, 41) while other studies have failed to demonstrate such relationships.(42–44) Our study did not demonstrate associations between need for respiratory support or renal-replacement therapy and benefit of high case volume hospitals for patients with severe sepsis.
A key component of a potentially regionalized system of severe sepsis care is a system of triage that is sufficiently sensitive and specific to identity patients that will benefit from inter-hospital transfer. The effect modification by organ dysfunction of the relationship between case volume and mortality implies that regionalization of severe sepsis care is not simple and may not yield expected benefits among all patients with severe sepsis.
If number of organ failures is to be utilized as a potential triage consideration for the inter-hospital transfer of severe sepsis patients in a regionalized care setting, accurately categorizing and quantifying organ failure in the prehospital setting will be inherently challenging. This would imply that acutely ill sepsis patients may have to be triaged directly from a local hospital setting in order to accurately classify organ failures, potentially delaying care for the approximately 40% of severe sepsis cases that are transported via prehospital emergency medical service providers.(45)
Operations research methodologies utilizing simulated models of prehospital care can advance our understanding of the potential effects of regionalized system of care for critical illness. For example, in a simulated study of non-trauma, nonarrest critical illness, Seymour et al(46) demonstrated that prehospital regionalization does not drastically increase travel times, overburden referral center ICUs, or deplete non-referral hospitals. Although simulation models suggest that healthcare systems may not bear strain from inter-hospital transfers, studies are needed to identify changes in patient severity of illness and evolution of organ dysfunction during the process of inter-hospital transfer.
The strength of our study lies in the large sample size of transferred patients, the representative, population-based mix of patients from diverse hospital settings including academic, nonacademic, urban and rural hospitals, the long period of observation spanning 9 years, adjustments for numerous demographic and hospital characteristics, co-morbid and severity of illness characteristics and sensitivity analysis. Despite these strengths, there are also several limitations. Although we identified patients with sepsis who were transferred between hospitals, we could not identify the case volume of the transferring hospital, specific reasons for transfer, or processes of care during transfer. Our study assumes the accuracy of ICD-9 codes and appropriate differentiation of pre-existing organ dysfunction from acute organ dysfunction in the NIS. The NIS lacks ‘present on admission’ modifiers to ICD-9 codes. ICD-9-CM codes on their own cannot discern the temporality of the onset of infection and organ dysfunction in cases without both infection and acute organ dysfunction present on admission. However it is unlikely that these limitations confounded the association between transfer status and outcomes since our sensitivity analysis yielded similar results. The NIS is also further limited in its ability to distinguish between patients with severe sepsis who were managed in intensive care versus non-intensive care. Thus, unmeasured confounding by severity of illness may introduce bias in effect estimates, a potential explanation for the failure to detect outcome benefits with increasing severity of illness. Our primary outcome of in-hospital mortality may also not be directly attributable to severe sepsis alone as patients may have died of other unrelated causes.
CONCLUSIONS
In conclusion, we demonstrated that patients with severe sepsis who were transferred to highest volume hospitals had higher predicted mortality and greater number of acute organ dysfunction. Mortality benefits of high case volume hospitals was limited to a subset of transferred patients with a single organ dysfunction and suggests a possible mismatch between current care for patients with severe sepsis and apparent benefits of inter-hospital transfer. Further studies should evaluate care processes and evolution of organ dysfunction during inter-hospital transfer of severe sepsis patients.
Supplementary Material
Acknowledgments
Financial Support: Geisinger Health System Foundation (SRC-S-40)
Dr. Ofoma received support for article research from Geisinger Scientific Review Committee. Dr. Maeng received support for article research from Geisinger Clinic internal grant. Dr. Walkey’s institution received funding from NHLBI/NIH Career Development Award. He received funding from UpToDate.
Footnotes
Conflict of Interest: The authors declare no conflict of interest
Supplemental Content
Supplemental Table 1: ICD 9 Coding for Organ Dysfunction and Sepsis
Supplemental Table 2: Comparison of Characteristics of Transferred and Non-transferred Patients with Severe Sepsis
Supplemental Table 3: Unadjusted Mortality, Length of Stay and Total Charges by Quintiles of Severe Sepsis Case Volume
Supplemental Table 4A: Distribution of Principal Diagnosis Codes
Supplemental Table 4B: Case Volume and Adjusted Risk of In-hospital Mortality by Number of Organ Dysfunction in Subgroup of Transferred Patients with Principal Diagnosis Codes of 0.38, 785 or 995
Supplemental Table 5A: Case Volume and Adjusted Risk of In-hospital Mortality by Number of Organ Dysfunction among Surgical Hospitalizations
Supplemental Table 5B: Case Volume and Adjusted Risk of In-hospital Mortality by Number of Organ Dysfunction among Non-Surgical Hospitalizations
Supplemental Table 6: Odds Ratio And 95% Confidence Intervals for In-hospital Mortality by Case Volume Quintile in Early Renal and Respiratory Organ Dysfunction
REFERENCES
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Critical care medicine. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. The New England journal of medicine. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 3.Gaieski DF, Edwards JM, Kallan MJ, et al. Benchmarking the incidence and mortality of severe sepsis in the United States. Critical care medicine. 2013;41(5):1167–1174. doi: 10.1097/CCM.0b013e31827c09f8. [DOI] [PubMed] [Google Scholar]
- 4.Kaukonen KM, Bailey M, Suzuki S, et al. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. Jama. 2014;311(13):1308–1316. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 5.Stevenson EK, Rubenstein AR, Radin GT, et al. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Critical care medicine. 2014;42(3):625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pro CI, Yealy DM, Kellum JA, et al. A randomized trial of protocol-based care for early septic shock. The New England journal of medicine. 2014;370(18):1683–1693. doi: 10.1056/NEJMoa1401602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu V, Escobar GJ, Greene JD, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. Jama. 2014;312(1):90–92. doi: 10.1001/jama.2014.5804. [DOI] [PubMed] [Google Scholar]
- 8.Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Rep. 2012;61(6):1–51. [PubMed] [Google Scholar]
- 9.Lagu T, Rothberg MB, Shieh MS, et al. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Critical care medicine. 2012;40(3):754–761. doi: 10.1097/CCM.0b013e318232db65. [DOI] [PubMed] [Google Scholar]
- 10.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. The New England journal of medicine. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical care medicine. 2006;34(6):1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 12.Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Critical care medicine. 2010;38(4):1045–1053. doi: 10.1097/CCM.0b013e3181cc4824. [DOI] [PubMed] [Google Scholar]
- 13.Lee SJ, Ramar K, Park JG, et al. Increased fluid administration in the first three hours of sepsis resuscitation is associated with reduced mortality: a retrospective cohort study. Chest. 2014 doi: 10.1378/chest.13-2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Critical care medicine. 2010;38(2):367–374. doi: 10.1097/CCM.0b013e3181cb0cdc. [DOI] [PubMed] [Google Scholar]
- 15.Schumacher HC, Bateman BT, Boden-Albala B, et al. Use of thrombolysis in acute ischemic stroke: analysis of the Nationwide Inpatient Sample 1999 to 2004. Ann Emerg Med. 2007;50(2):99–107. doi: 10.1016/j.annemergmed.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 16.Saposnik G, Baibergenova A, O'Donnell M, et al. Hospital volume and stroke outcome: does it matter? Neurology. 2007;69(11):1142–1151. doi: 10.1212/01.wnl.0000268485.93349.58. [DOI] [PubMed] [Google Scholar]
- 17.Nuno M, Patil CG, Lyden P, et al. The effect of transfer and hospital volume in subarachnoid hemorrhage patients. Neurocrit Care. 2012;17(3):312–323. doi: 10.1007/s12028-012-9740-y. [DOI] [PubMed] [Google Scholar]
- 18.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. The New England journal of medicine. 2006;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 19.Canto JG, Every NR, Magid DJ, et al. The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. The New England journal of medicine. 2000;342(21):1573–1580. doi: 10.1056/NEJM200005253422106. [DOI] [PubMed] [Google Scholar]
- 20.Magid DJ, Calonge BN, Rumsfeld JS, et al. Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy. Jama. 2000;284(24):3131–3138. doi: 10.1001/jama.284.24.3131. [DOI] [PubMed] [Google Scholar]
- 21.Carr BG, Kahn JM, Merchant RM, et al. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009;80(1):30–34. doi: 10.1016/j.resuscitation.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Peelen L, de Keizer NF, Peek N, et al. The influence of volume and intensive care unit organization on hospital mortality in patients admitted with severe sepsis: a retrospective multicentre cohort study. Critical care. 2007;11(2):R40. doi: 10.1186/cc5727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reinikainen M, Karlsson S, Varpula T, et al. Are small hospitals with small intensive care units able to treat patients with severe sepsis? Intensive Care Med. 2010;36(4):673–679. doi: 10.1007/s00134-009-1688-9. [DOI] [PubMed] [Google Scholar]
- 24.Gaieski DF, Edwards JM, Kallan MJ, et al. The Relationship between Hospital Volume and Mortality in Severe Sepsis. American journal of respiratory and critical care medicine. 2014;190(6):665–674. doi: 10.1164/rccm.201402-0289OC. [DOI] [PubMed] [Google Scholar]
- 25.Walkey AJ, Wiener RS. Hospital case volume and outcomes among patients hospitalized with severe sepsis. American journal of respiratory and critical care medicine. 2014;189(5):548–555. doi: 10.1164/rccm.201311-1967OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dodek PM. Volume-outcome relationships in critical care. Understanding the mechanism. American journal of respiratory and critical care medicine. 2014;190(6):601–603. doi: 10.1164/rccm.201401-0132ED. [DOI] [PubMed] [Google Scholar]
- 27.Kahn JM. Volume, outcome, and the organization of intensive care. Critical care. 2007;11(3):129. doi: 10.1186/cc5776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis 3) Jama. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 30.Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. 1992. Chest. 2009;136(5 Suppl):e28. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 31.Iwashyna TJ, Odden A, Rohde J, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Medical care. 2014;52(6):e39–e43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walkey AJ, Wiener RS, Ghobrial JM, et al. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. Jama. 2011;306(20):2248–2254. doi: 10.1001/jama.2011.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Medical care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Baram D, Daroowalla F, Garcia R, et al. Use of the All Patient Refined-Diagnosis Related Group (APR-DRG) Risk of Mortality Score as a Severity Adjustor in the Medical ICU. Clin Med Circ Respirat Pulm Med. 2008;2:19–25. doi: 10.4137/ccrpm.s544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Austin PC, Rothwell DM, Tu JV. A Comparison of Statistical Modeling Strategies for Analyzing Length of Stay after CABG Surgery. Health Services and Outcomes Research Methodology. 2002;3(2):107–133. [Google Scholar]
- 36. [cited 2016 August 29];Surgery Flag Software. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/surgflags/surgeryflags.jsp#pubs.
- 37.Kahn JM, Goss CH, Heagerty PJ, et al. Hospital volume and the outcomes of mechanical ventilation. The New England journal of medicine. 2006;355(1):41–50. doi: 10.1056/NEJMsa053993. [DOI] [PubMed] [Google Scholar]
- 38.Waikar SS, Wald R, Chertow GM, et al. Validity of International Classification of Diseases, Ninth Revision, Clinical Modification Codes for Acute Renal Failure. Journal of the American Society of Nephrology : JASN. 2006;17(6):1688–1694. doi: 10.1681/ASN.2006010073. [DOI] [PubMed] [Google Scholar]
- 39.Mehta AB, Syeda SN, Wiener RS, et al. Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. Journal of critical care. 2015;30(6):1217–1221. doi: 10.1016/j.jcrc.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Faine BA, Noack JM, Wong T, et al. Interhospital Transfer Delays Appropriate Treatment for Patients With Severe Sepsis and Septic Shock: A Retrospective Cohort Study. Critical care medicine. 2015;43(12):2589–2596. doi: 10.1097/CCM.0000000000001301. [DOI] [PubMed] [Google Scholar]
- 41.Vaara ST, Reinikainen M, Kaukonen KM, et al. Association of ICU size and annual case volume of renal replacement therapy patients with mortality. Acta anaesthesiologica Scandinavica. 2012;56(9):1175–1182. doi: 10.1111/j.1399-6576.2012.02747.x. [DOI] [PubMed] [Google Scholar]
- 42.Cooke CR, Kennedy EH, Wiitala WL, et al. Despite variation in volume, Veterans Affairs hospitals show consistent outcomes among patients with non-postoperative mechanical ventilation. Critical care medicine. 2012;40(9):2569–2575. doi: 10.1097/CCM.0b013e3182591eee. [DOI] [PubMed] [Google Scholar]
- 43.Needham DM, Bronskill SE, Rothwell DM, et al. Hospital volume and mortality for mechanical ventilation of medical and surgical patients: a population-based analysis using administrative data. Critical care medicine. 2006;34(9):2349–2354. doi: 10.1097/01.CCM.0000233858.85802.5C. [DOI] [PubMed] [Google Scholar]
- 44.Nguyen YL, Milbrandt EB, Weissfeld LA, et al. Intensive care unit renal support therapy volume is not associated with patient outcome. Critical care medicine. 2011;39(11):2470–2477. doi: 10.1097/CCM.0b013e3182257631. [DOI] [PubMed] [Google Scholar]
- 45.Seymour CW, Rea TD, Kahn JM, et al. Severe sepsis in pre-hospital emergency care: analysis of incidence, care, and outcome. American journal of respiratory and critical care medicine. 2012;186(12):1264–1271. doi: 10.1164/rccm.201204-0713OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seymour CW, Alotaik O, Wallace DJ, et al. County-Level Effects of Prehospital Regionalization of Critically Ill Patients: A Simulation Study. Critical care medicine. 2015;43(9):1807–1815. doi: 10.1097/CCM.0000000000001133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


