Abstract
Lay Health Advisor (LHA) programs hold tremendous promise for reducing health disparities and addressing social determinants of health in medically underserved communities, including African American populations. Very little is understood about the capacity of LHAs in these roles and the broader contributions they make to their communities. This paper seeks to address this gap by describing the characteristics and capacity of a sample of 76 female African American LHAs from a nationally disseminated evidence-based LHA program for breast and cervical cancer screening (The National Witness Project), as well as potential differences between cancer survivors and non-survivors who serve as LHAs. A conceptual model for understanding LHA capacity and contributions in underserved communities at the individual, social, and organizational levels is presented. We describe LHA experiences and characteristics (e.g. experiences of mistrust and discrimination; racial pride; sociodemographics), capacity at the individual-level (e.g., psychological and physical health, health behaviors), capacity at the social-level (e.g., social networks, social support), and capacity at the organizational-level (e.g., role-related competencies, self-efficacy, leadership, role benefits/challenges). Data was obtained through interview-administered telephone surveys between 2010 and 2012. Findings highlight the critical capacity that LHAs bring to their communities and the importance of supporting LHAs to sustain these programs and to address racial/ethnic health disparities.
Keywords: Lay Health Advisors, Community capacity, Cancer Screening, African Americans, Implementation
Lay Health Advisor (LHA) programs hold tremendous promise for reducing health disparities and addressing social determinants of health (Balcazar et al., 2011; N. Wiggins & Bourbón, 1998). LHAs are trained community members who work in community-based and clinical settings (Simoni, Franks, Lehavot, & Yard, 2011), and share social, economic, cultural, and linguistic characteristics with the populations of interest (Brownstein, Hirsch, Rosenthal, & Rush, 2011; Eng, Parker, & Harlan, 1997). While responsibilities vary (South, White, Branney, & Kinsella, 2013), LHAs typically act as a trusted liaison between community members and health or social service organizations and deliver culturally appropriate health education programs and support (Lewin et al., 2005).
LHAs are highly effective in improving behavior, attitudes, barriers, knowledge and access in cancer screening programs (Brownstein et al., 2011; Earp et al., 2002; Legler et al., 2002; Viswanathan et al., 2009), particularly among African American women (Earp et al., 2002; Erwin, Spatz, Stotts, Hollenberg, & Deloney, 1996; Russell et al., 2010; Viswanathan et al., 2009; Wells et al., 2011). Historical and ongoing racism and discrimination and the resulting mistrust of medical institutions make LHA programs fitting for African Americans. LHA programs are consistent with African American historical social movements where health activism is a central part of political culture and the importance of addressing health inequities, power, medical mistrust, and discrimination through community engagement is recognized (Nelson, 2011).
The National Witness Project (NWP) is an evidence-based LHA program that effectively increases breast and cervical cancer screening among African American women (Erwin et al., 2003; Erwin et al., 1996). African American LHAs provide culturally-appropriate education, empowerment messages, resources, and navigation in community settings, and African American breast/cervical cancer survivors (called Role Models; both referred to as LHAs in this paper) provide narratives about their experiences. LHAs are often volunteers or are provided with stipends for their participation. Over the past 25 years, NWP has been replicated and implemented in 40 sites nationally, with over 400 LHAs, reaching 15,000 women annually, and is one of the National Cancer Institute’s ‘Research Tested Intervention Programs (Division of Cancer Control and Population Sciences, 2012; Erwin et al., 2003)’.
Despite a proliferation of LHA programs over the past 20–30 years (Perry, Zulliger, & Rogers, 2014), research has focused on the outcomes of LHA programs, and less is known about the LHAs themselves. Our research contributes to the growing literature on the characteristics and capacity of community-based LHAs in under-resourced settings, building off of prior research that has been conducted in the past among African Americans (Eng & Parker, 2002; Eng & Young, 1992; Jackson & Parks, 1997) and Hispanics (Rhodes, Foley, Zometa, & Bloom, 2007).
This paper seeks to describe the characteristics and capacity of a sample of 76 African American LHAs from NWP. We sought to provide a deeper and more contextualized understanding of the individual, social, and organizational capacity of LHAs and how such programs have the potential to make important contributions to the lives of LHAs themselves, their social networks, and their communities. An additional goal was to explore whether there were differences in the characteristics and capacity of LHAs based on their status as cancer survivors. On the one hand, cancer survivors may be influential messengers (Gilkey, Garcia, & Rush, 2011) that help address emotional and cultural-specific issues (e.g. fatalism, mistrust, and cultural narratives about cancer as stigmatizing) (Erwin, 2009; Kreuter et al., 2007; Mathews, 2009), and may gain social and psychological benefits through their role as LHAs. However, little is known about the survivors who participate in such programs and whether they experience strains related to their participation. This is important to examine given that survivors are increasingly taking on roles as LHAs (Vijaykumar, Wray, Jupka, Clarke, & Shahid, 2013).
Conceptual Framework
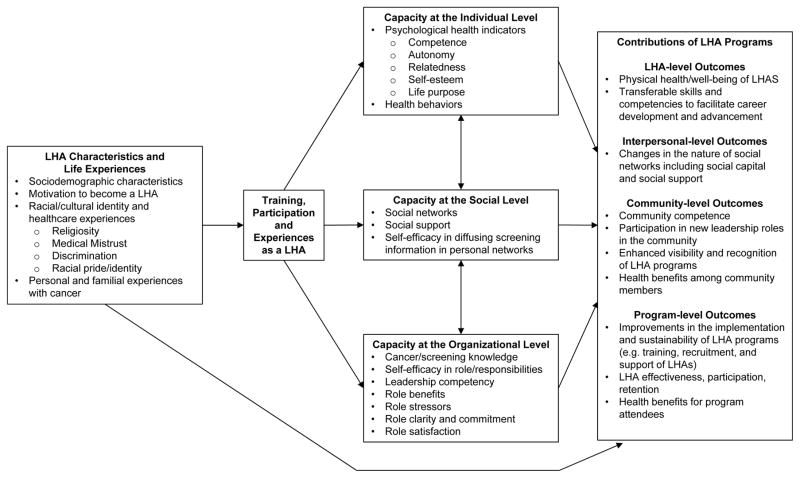
Figure 1 introduces a theoretically-grounded model for understanding LHA capacity across multiple levels (Framework for Assessing LHA Capacity and Contributions).
Figure 1.
Framework for Assessing LHA Capacity and Contributions: A conceptual framework for understanding lay health advisor capacity and contributions at the individual, social, and organizational levels.
LHA Characteristics and Personal Life Experiences
LHAs may experience the same issues (e.g. racism, mistrust) as the populations with whom they work. Pride in one’s racial and ethnic identity (the extent to which one’s racial/ethnic group is a significant aspect of one’s identity) (Sellers, Smith, Shelton, Rowley, & Chavous, 1998), experiences of discrimination in healthcare (Bird & Bogart, 2000; Krieger, Smith, Naishadham, Hartman, & Barbeau, 2005) and medical mistrust may influence motivation and commitment to being a LHA, particularly for programs focused on addressing disparities. Personal experiences with cancer and religiosity may also motivate LHAs’ desire to take on this role.
Capacity at the Individual Level
Psychological health and well-being
Serving as a LHA may provide a source of self-esteem and meet basic psychological needs such as competence (feeling effective), autonomy (low powerlessness), and relatedness (a sense of belonging) (Deci & Ryan, 2000). Participation in LHA programs may also provide a mechanism through which people can stay engaged and provide life purpose (Carver & Scheier, 1998).
Physical health and healthy behaviors
LHAs may feel empowered and motivated to improve their own health or health-related behaviors. Alternatively, they may also personally experience the same structural impediments to healthcare (Landers & Stover, 2011).
Capacity at the Social Level
LHA programs build upon and expand social networks (Eng & Young, 1992). LHAs are often well-connected in the community; they are also often trained and work together in groups. Thus, participation may increase the size and composition of one’s network and enhance perceived social support. Providing support is an important aspect of social relationships that has health-related benefits (Brown, Nesse, Vinokur, & Smith, 2003; Cutrona & Russell, 1987). This is consistent with Riessman’s Helper Therapy Principle, suggesting that LHAs may receive social and psychological benefits from their work that reinforce participation (Riessman, 1965). Participation may also build social capital in their communities, and LHAs may diffuse health education content in their broader networks and communities.
Capacity at the Organizational Level
Role-related competencies and experiences
LHAs may develop transferable competencies, skills, and self-efficacy related to their LHA role. These skills, role-related benefits, and role expectations may have important implications for their effectiveness and job satisfaction. Leadership competence is a dimension of psychological empowerment (Zimmerman & Zahniser, 1991). By training and supporting individuals to gain new or enhance existing competencies, LHAs may apply these new skills in other domains and take on new leadership roles, providing long-term benefits to their communities (e.g. enhanced community competence). LHAs may also experience role-related stressors or challenges that may limit their participation and impact program sustainability.
Methods
Recruitment
We contacted eight NWP sites in the northeast, south, and mid-west. These sites were selected from 20 sites that had attended the most recent NWP Annual Meeting. The NWP local Program Director and the study Principal Investigator informed LHAs about the study through a letter, phone, and/or presentations at scheduled local meetings and trainings. LHAs interested in participating provided written permission to be contacted. All interested LHAs were contacted by telephone to consent them and schedule the telephone-based study assessment. Institutional Review Board approval was awarded through Columbia’s Mailman School of Public Health. A total of 84 eligible LHAs were identified and provided their contact information; of those, a total of 76 women participated in the study (response rate=91%).
Eligibility and Data Collection
To participate in the study, individuals had to be: 1) African American or black; 2) female; 3) a LHA from the NWP (currently or within the past two years); 4) over the age of 18; and 5) English-speaking. Baseline interview-administered telephone surveys took place between 2010 and 2012 at eight sites (see Table 1). Study participants received a $25 gift card per survey.
Table 1.
Sociodemographic and Health-related Characteristics of the Sample of African American Lay Health Advisors from The National Witness Project (NWP), Overall and by Cancer Survivorship Status (n=76)
| LHA (no history of cancer) (n=38) | Cancer Survivor LHA (n=38) | p-value | All LHAs (N=76) | |
|---|---|---|---|---|
| Study Site | ||||
| 1 Harlem, NY | 8 (21%) | 6 (16%) | 0.88 | 14 (18%) |
| 2 Syracuse, NY | 3 (8%) | 7 (18%) | 10 (13%) | |
| 3 Little Rock, AR | 10 (26%) | 7 (18%) | 17 (22%) | |
| 4 Long Island, NY | 2 (5%) | 3 (8%) | 5 (7%) | |
| 5 Tampa, FL | 3 (8%) | 3 (8%) | 6 (8%) | |
| 6 Chicago, IL | 2 (5%) | 2 (5%) | 4 (5%) | |
| 7 Buffalo, NY | 8 (21%) | 9 (24%) | 17 (22%) | |
| 8 Wichita, KS | 2 (5%) | 1 (3%) | 3 (4%) | |
| Type of Institution | ||||
| Academic | 29 (76%) | 25 (66%) | 0.45 | 54 (71%) |
| Non-academic | 9 (24%) | 13 (34%) | 22 (29%) | |
| Length of activity in role (months) mean (SD) [range] | 62.7 (50.2) [0–180] | 69.0 (56.2) [1–192] | 0.61 | 65.8 (53.0) [0–192] |
| Employed | ||||
| Employed by NWP | 4 (11%) | 2 (5%) | 0.75 | 6 (8%) |
| Employed FT outside of NWP | 13 (34%) | 11 (29%) | 24 (32%) | |
| Employed PT outside of NWP | 3 (8%) | 4 (11%) | 7 (9%) | |
| Not employed | 18 (47%) | 21 (55%) | 29 (51%) | |
| Position in NWP | ||||
| Paid | 4 (11%) | 2 (5%) | 0.67 | 6 (8%) |
| Voluntary | 34 (89%) | 36 (95%) | 70 (92%) | |
| Age mean (SD) [range] | 50.7 (15.0) [21–76] | 59.0 (10.5) [35–78] | 0.006 | 54.9 (13.5) [21–78] |
| Education | ||||
| ≤ Some college | 14 (37%) | 16 (42%) | 0.65 | 30 (39%) |
| Associate’s or University graduate | 16 (42%) | 17 (45%) | 33 (43%) | |
| Graduate or Professional Degree | 8 (21%) | 5 (13%) | 13 (17%) | |
| Annual Household Income | ||||
| <$10,000 – $24,999 | 9 (24%) | 7 (18%) | 0.03 | 16 (21%) |
| $25,000 – $49,999 | 7 (18%) | 15 (39%) | 22 (29%) | |
| >$50,000 | 21 (55%) | 11 (29%) | 32 (42%) | |
| Refused | 1 (3%) | 5 (13%) | 6 (8%) | |
| Marital Status | ||||
| Married | 15 (39%) | 17 (45%) | 0.49 | 32 (42%) |
| Never married | 14 (37%) | 9 (24%) | 23 (30%) | |
| Separated/divorced/widowed | 9 (24%) | 11 (29%) | 20 (26%) | |
| Did not respond | 0 (3%) | 1 (3%) | 1 (1%) | |
| Healthcare summary | ||||
| Have primary care provider (Yes) | 32 (84%) | 37 (97%) | 0.11 | 69 (91%) |
| Primary Insurance | ||||
| Medicaid or Medicare | 10 (26%) | 21 (55%) | 0.002 | 31 (41%) |
| Employer-provided insurance | 17 (45%) | 16 (42%) | 33 (43%) | |
| None/other | 11 (29%) | 1 (3%) | 12 (16%) | |
| General self-assessment of health | ||||
| Excellent/Very Good | 6 (16%) | 9 (24%) | 0.14 | 24 (32%) |
| Good | 16 (42%) | 21 (55%) | 37 (49%) | |
| Fair/poor | 16 (42%) | 8 (21%) | 15 (19%) | |
| Regular Current Smoker | 2 (5%) | 4 (11%) | 0.67 | 6 (8%) |
| Average number of servings of fruits/veg per day | 3.4 (1.6) [1–10] | 2.8 (1.4) [1–5] | 0.08 | 3.1 (1.5) [1–10] |
| Average days/week of exercise | 2.8 (2.1) [0–7] | 2.8 (2.3) [0–7] | 1.0 | 2.8 (2.2) [0–7] |
| Ever colonoscopy* | 21 (84%) | 29 (94%) | 0.39 | 50 (89%) |
| Any CRC Screening in past year* | 20 (80%) | 29 (94%) | 0.22 | 49 (88%) |
in the 56 women age 50+
Measures: LHA Characteristics and Personal Life Experiences
Sociodemographic information included: age, income, education, insurance, healthcare provider, and employment. Racial Pride was evaluated using a 7-item scale developed for African Americans (Lukwago, Kreuter, Bucholtz, Holt, & Clark, 2001) (α = .80). Participants were asked how much they agreed with statements about their pride of being African American on a Likert scale of 1 to 4 to create a mean score. Medical Mistrust was assessed using a 3-item sub-scale on ‘disparities in health’ from the Group-Based Medical Mistrust Scale (Thompson, Valdimarsdottir, Winkel, Jandorf, & Redd, 2004) (α = .89). The mean score assessed how much they agreed that members of their racial group are treated fairly by healthcare workers. Healthcare Discrimination was measured with one question from The Experiences of Discrimination Measure (Krieger et al., 2005). Response options included never, 1–2 times, 3–4 times or 5 or more times, with a corresponding score of 0–3. Religiosity was measured using a 9-item scale developed by Lukwago et al. (2001) for African Americans (α = .86).
Capacity at the Individual Level
Psychological health and well-being
Autonomy, competence, and relatedness were assessed using the 20-item Basic Psychological Needs Scale (Deci & Ryan, 2000) (α=.61), with higher scores reflecting higher autonomy, competence, and relatedness. Life Engagement was assessed with a 6-item scale (Scheier et al., 2006) that measured the extent to which they participated in activities in their life on a 5-point Likert scale. (α=.51). Self-esteem was assessed using the 6-item Rosenberg self-esteem scale (Rosenberg, 1965) (α=.70). Physical health and behaviors: Self-rated health was assessed by a 1-item validated measure (Idler & Angel, 1990), and participation in other cancer prevention behaviors (e.g. smoking, cancer screening, physical activity) was assessed by self-report, based on items from the Behavioral Risk Factor Surveillance System survey.
Capacity at the Social Level
Social Networks were measured using Cohen’s Social Network Index (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997). For each of 12 different types of relationships, participants were asked to indicate if they speak to someone (in person or by telephone) in that network at least biweekly. For each network type endorsed, that network was assigned one point (max score = 12) and summed to include the number of people they speak to regularly. The Social Provisions Scale, a validated 10-item scale developed by Cutrona and Russell (1987) measured social support on a scale of 1 to 4 (α = .85). Self-efficacy in diffusing cancer screening information was measured using four items that asked participants how confident they were to talk to family members, friends, church members, and other members of their social network outside of NWP about breast/cervical cancer screening (Likert scale of 1 to 4).
Capacity at the Organizational Level
Knowledge of Breast Cancer and Screening was assessed using a 13-item scale developed by the NWP with a score based on the percentage of correct answers (α=.62). LHA Role self-efficacy was assessed using a 21-item scale validated among black LHAs (Russell et al., 2010) (ratings from 1 to 4 to assess their confidence in NWP responsibilities) (α = .69–.85). Leadership competence was measured using Zimmerman and Zahniser’s (1991) Sociopolitical Control Scale with eight items averaged to determine an overall leadership score (α = .73).
The 25-item Helper’s Perception Measure (Roman, Lindsay, Moore, & Shoemaker, 1999) assessed mean perceptions of role benefits and challenges (1=Strongly Disagree and 5= Strongly Agree). Role clarity and expectations were measured using 9 items that assessed how much participants agreed or disagreed with statements about their LHA role on a 5-point scale (α = .86). LHA job satisfaction was measured using a 6-item adapted version of the validated Job Satisfaction Index (Schriesheim & Tsui, 1980) (α=.60).
Analyses
Data were summarized using percentages, means, standard deviations, and ranges. To compare differences between cancer survivors and non-survivors, Fisher’s exact test or a chi-squared test was used for categorical variables, while t-tests were used for continuous measures. Analyses were conducted using SAS v. 9.2 (Cary, NC).
Results
Site and position characteristics
Participating LHAs represented a diversity of urban, suburban, and rural geographic sites and locations (see Table 1). The mean length of time involved in the program was 65.8 months, (range: 0 months to 16 years). Most women (92%) were in unpaid, voluntary LHA positions. Using self-report, 78% reported being currently active in the NWP (e.g. actively conducting educational sessions).
LHA Characteristics and Personal Life Experiences
Sociodemographic characteristics are displayed in Table 1. Over 40% had Associate’s or University degrees and about half were unemployed (predominately related to retirement). Half of participants (50%) (n=38) were breast or cervical cancer survivors. Consistent with the characteristics of cancer survivors, survivors were older (59 years old vs. 50 years old), more likely to be on Medicaid/Medicare, and had lower incomes than non-survivors (see Table 1). Participants reported high levels of religiosity, with a mean score of 33.7 (Possible Range or PR: 9 to 36). Survivor LHAs had higher religiosity than non-survivor LHAs (p=.005). Racial pride was high for all participants, at a mean score of 24.2 (PR: 7 to 28). Medical mistrust mean score was 2.2 (PR: 1 to 5), and reports of discrimination in healthcare settings had a mean score of 1.0 (PR: 0 to 3) (see Table 2 for full results).
Table 2.
Individual, Social, and,Organizational Capacity Measured among the Sample of African American Lay Health Advisors from The National Witness Project (NWP), Overall and by Cancer Survivorship Status (n=76)*
| LHA (no history of cancer)(n=38) | Cancer Survivor LHA (n=38) | p-value | All LHAs(N=76) | |
|---|---|---|---|---|
| Capacity at the Individual Level | ||||
| Psychological Health | ||||
| Autonomy | 6.0 (0.7) [4.0–7.0] | 6.2 (0.6) [5.0–7.0] | 0.21 | 6.1 (0.6) [4.0–7.0] |
| Competence | 6.4 (0.6) [4.8–7.0] | 6.3 (1.0) [2.6–7.2] | 0.49 | 6.3 (0.8) [2.6–7.0] |
| Relatedness | 6.1 (0.7) [4.4–7.0] | 6.3 (0.5) [5.1–7.0] | 0.24 | 6.4 (0.6) [4.4–7.0] |
| Life Engagement | 28.9 (1.4) [24–30] | 28.7 (1.5) [24–30] | 0.43 | 28.8 (1.4) [24–30] |
| Self-Esteem | 22.8 (1.6) [18–24] | 23.1 (1.3) [19–24] | 0.39 | 22.9 (1.5) [18–24] |
| Prior Personal Experiences | ||||
| Religiosity | 32.7 (4.0) [18–36] | 34.7 (1.5) [30–36] | 0.005 | 33.7 (3.2) [18–36] |
| Racial Pride | 23.9 (3.5) [10.0–28.0] | 24.5 (2.4) [20.0–28.0] | 0.40 | 24.2 (3.0) [10.0–28.0] |
| Medical Mistrust | 2.0 (0.9) [1.0–4.0] | 2.2 (0.8) [1.0–4.0] | 0.16 | 2.2 (0.8) [1.0–4.0] |
| Discrimination in Healthcare Settings | 0.9(1.3) [0–3] | 1.0 (1.2) [0–3] | 0.78 | 1.0 (1.2) [0–3] |
| Capacity at the Social Level | ||||
| Social Networks | 7.4 (1.6) [3–10] | 7.4 (1.8) [3–10] | 0.97 | 7.4 (1.7) [3–10] |
| Social Network Size | 46.6 (44.2) [14–219] | 54.5 (49.7) [13–272] | 0.47 | 50.5 (46.8) [13–272] |
| Social Support | 37.2 (3.7) [26–40] | 37.8 (2.9) [26–40] | 0.42 | 37.5 (3.3) [26–40] |
| Self-Efficacy for Diffusing Info in Community | 3.9 (0.2) [3.0–4.0] | 3.9 (0.2) [3.0–4.0] | 0.78 | 3.9 (0.2) [3.0–4.0] |
| Capacity at the Organizational Level | ||||
| Breast Cancer Knowledge (% correct) | 88 (11) [62–100] | 81 (16) [46–100] | 0.02 | 84 (14) [46–100] |
| Role Self-efficacy | ||||
| Overall self-efficacy | 3.7 (0.2) [3.1–4.0] | 3.7 (0.3) [2.8–4.0] | 0.77 | 3.7 (0.3) [2.8–4.0] |
| Skill-related self-efficacy | 3.6 (0.3) [2.9–4.0] | 3.7 (0.3) [2.9–4.0] | 0.54 | 3.7 (0.3) [2.9–4.0] |
| Growth self-efficacy | 3.7 (0.3) [3.0–4.0] | 3.7 (0.3) [2.8–4.0] | 1.0 | 3.7 (0.3) [2.9–4.0] |
| Collective self-efficacy | 3.9 (0.3) [3.0–4.0] | 3.9 (0.3) [2.7–4.0] | 0.91 | 3.9 (0.3) [2.7–4.0] |
| Perception of LHA Role | ||||
| Benefits | 4.5 (0.4) [3.4–5] | 4.6 (0.4) [0–5.0] | 0.25 | 4.5 (0.4) [3.4–5.0] |
| Stressors | 1.7 (0.5) [1.0–3.0] | 1.6 (0.5) [1.0–2.7] | 0.32 | 1.6 (0.5) [1.0–3.0] |
| Role clarity and commitment | 4.5 (0.5) [3.2–5.0] | 4.6 (0.4) [3.5–5.0] | 0.12 | 4.6 (0.4) [3.2–5.0] |
| Job Satisfaction | 4.3 (0.5) [3.4–5.0] | 4.5 (0.5) [3.8–5.0] | 0.07 | 4.4 (0.5) [3.4–5.0] |
| Leadership Competence | 4.0 (0.5) [2.8–4.9] | 4.1 (0.5) [3.0– 5.0] | 0.95 | 4.1 (0.5) [2.8–5.0] |
For continuous measures: Mean (SD) [actual range]
Capacity at the Individual Level
Psychological and physical health
Participants scored high on psychological well-being, as measured by autonomy, competence, and relatedness, with mean scores of 6.1 to 6.4 (PR: 1 to 7). Life purpose and engagement was high at a mean of 28.8 (PR: 6 to 30), as was self-esteem at a mean score of 22.9 (PR: 6 to 24) (Table 2). About 20% of LHAs reported their health as ‘poor/fair’. No differences in health indicators were found between survivors and non-survivors (see Tables 1 and 2).
Capacity at the Social Leve
Participant social networks were expansive in different domains (e.g. family, friends, social groups), with a mean overall score of 7.4 (PR: 0 to 12), and a mean of 50.5 network members (range: 13 to 272). Participants reported high levels of social support, with a mean of 37.5 (PR: 10 to 40) and had high levels of self-efficacy for diffusing breast or cervical cancer screening information within their networks outside of NWP program, with a mean score of 3.9 (range: 1 to 4) (see Table 2). Table 3 provides detailed information about their social networks. On average, LHAs had 4–5 close friends and 4–5 close relatives that they speak to often; 18% had children at home, and of those, 11% care for their grandchildren. Most women belonged to a religious group (89%), volunteered outside of the NWP (75%), were active members of other social groups (77%) (e.g. unions, community service groups). Differences between survivors and non-survivors were minimal (see Table 2 and 3).
Table 3.
Social Network Characteristics of the Sample of African American Lay Health Advisors from The National Witness Project, and differences between cancer survivors and non-survivors (n=76) (table presents median [range] of responses, or n(%))
| Social Networks | LHA (no history of cancer)(n=38) | Cancer Survivor LHA (n=38) | P-value (Differences between survivors and non-survivors) | All (N=76) |
|---|---|---|---|---|
| Number of children | 1 [0–6] | 2 [0–8] | 0.30 | 2 [0–8] |
| Number see/speak to every ≤2 weeks | 2 [0–4] | 2 [0–8] | 0.22 | 2 [0–8] |
| Have children living at home | 8 (29%) | 6 (19%) | 0.54 | 14 (18%) |
| Care for any grandchildren (of those with children) | 1 (4%) | 7 (23%) | 0.055 | 8 (11%) |
| Either Parents living | 19 (50%) | 16 (43%) | 0.65 | 35 (46%) |
| See/speak to parents every ≤2 weeks | 18 (95%) | 14 (93%) | 1.0 | 32 (94%) |
| Any In-Laws living | 6 (16%) | 5 (14%) | 1.0 | 11 (15%) |
| See/speak to parents every ≤2 weeks | 3 (50%) | 1 (20%) | 0.55 | 4 (36%) |
| Number of other relatives close to | 5 [0–7+] | 7 [0–7+] | 0.05 | 7 [0–7+] |
| Number relatives see/speak to every ≤2 weeks | 3 [0–7+] | 5.5 [0–7+] | 0.003 | 4 [0–7+] |
| Number of close friends | 5 [1–7+] | 5 [1–7+] | 0.70 | 5 [1–7+] |
| Number of close friends see/speak to every ≤2 weeks | 4 [0–7+] | 4 [1–7+] | 0.54 | 4 [0–7+] |
| Belong to a religious Group | 33 (87%) | 35 (95%) | 0.43 | 68 (89%) |
| Number of religious org. members see/speak to every ≤2 weeks | 7 [1–7+] | 7 [0–7+] | 0.84 | 7 [0–7+] |
| Attend Classes | 12 (32%) | 6 (16%) | 0.18 | 18 (24%) |
| Number of classmates see/speak to every ≤2 weeks | 4 [0–7+] | 4.5 [0–7+] | 0.68 | 4.5 [0–7+] |
| Employed outside of witness | 20 (53%) | 17 (46%) | 0.84 | 37 (49%) |
| Number supervising | 0 [0–7+] | 0 [0–2+] | 0.19 | 0 [0–7+] |
| Number coworkers see/speak to every ≤2 weeks | 4.5 [0–7+] | 5 [1–7+] | 0.37 | 5 [0–7+] |
| Number neighbors see/speak to every ≤2 weeks | 3 [0–7+] | 2 [0–7+] | 0.61 | 3 [0–7+] |
| Currently Volunteering | 27 (71%) | 30 (81%) | 0.42 | 57 (76%) |
| Number volunteers see/speak to every ≤2 weeks | 4 [1–7+] | 5.5 [0–7+] | 0.46 | 5 [0–7+] |
| Other Social Groups | 29 (76%) | 29 (78%) | 1.0 | 58 (77%) |
Capacity at the Organizational Level
Role-related competencies and experiences
Participants had relatively high breast cancer knowledge, with a mean score of 84 out of 100 (range: 46 to 100). Cancer survivors had lower cancer knowledge (p=.02) than non-survivors. Participants also had high role self-efficacy, with mean scores of 3.7 to 3.9 (PR: 1 to 4), and reported high job satisfaction with a mean of 4.4 (PR: 1 to 5) and high leadership competence (mean= 4.1, PR: 1 to 5). Table 4 provides detailed information about LHAs’ role-related benefits and stressors. LHAs reported high levels of role benefits (mean=4.5; PR: 1 to 5) and relatively low levels of role stressors (mean=1.6; PR: 1 to 5). In terms of role clarity and commitment to the position, participants reported a mean score of 4.6 (PR: 1 to 5) (Table 2). The greatest role benefits included: feeling ‘energized’; helping people; and feeling good about ‘giving’ help because they have received help. The greatest challenges were: worrying more about one’s own health; feeling more stressed in meeting one’s own needs; having less energy for their own family; and feeling emotionally drained. The benefits and barriers experienced by survivors and non-survivor LHAs were similar, though LHA survivors experienced stronger benefits for several items (see Table 4).
Table 4.
Perceived Benefits and Stressors related to LHA Role among a sample of LHWs from The National Witness Project (NWP) (n=76)
| Question Items* | LHA (no history of cancer) (n=38) | Cancer Survivor LHA (n=38) | P-value (Differences between survivors and non-survivors) | All (N=76) Mean (SD) |
|---|---|---|---|---|
| Perceived Benefits | ||||
| I find more ways to cope with my own problems. | 4.18 (0.77) | 4.39 (0.73) | 0.24 | 4.28 (0.75) |
| I feel better about myself as a person. | 4.39 (0.75) | 4.69 (0.52) | 0.052 | 4.54 (0.67) |
| I am able to find more resources (such as health care services and information) that could help me and my friends/family. | 4.58 (0.60) | 4.56 (0.69) | 0.88 | 4.57 (0.64) |
| I am more skilled in talking and listening to others. | 4.42 (0.68) | 4.39 (0.90) | 0.86 | 4.41 (0.79) |
| I have felt ‘energized’ helping people. | 4.87 (0.34) | 4.78 (0.48) | 0.35 | 4.82 (0.42) |
| I have felt good about ‘giving’ help because I have received help. | 4.74 (0.45) | 4.92 (0.28) | 0.04 | 4.82 (0.38) |
| I have been able to gain valuable work experience and new skills. | 4.5 (0.76) | 4.42 (0.60) | 0.61 | 4.46 (0.69) |
| I have more confidence in my abilities to take care of my own health and needs. | 4.42 (0.68) | 4.67 (0.53) | 0.09 | 4.54 (0.62) |
| I have received support from other LHAs in coping with any stress or difficulties I’ve experienced in this role. | 4.05 (0.90) | 4.17 (0.88) | 0.58 | 4.11 (0.88) |
| I have received adequate supervision in this role. | 4.24 (0.85) | 4.5 (0.77) | 0.17 | 4.36 (0.82) |
| I have received help in getting the support services or medical referrals that I need for my clients. | 4.32 (0.74) | 4.39 (0.77) | 0.68 | 4.35 (0.75) |
| I have received resources and encouragement to develop my job skills. | 4.29 (0.77) | 4.28 (0.81) | 0.95 | 4.28 (0.79) |
| I have received encouragement to change a health habit (for example, smoking, eating healthy, obtaining recommended cancer screening). | 4.50 (0.86) | 4.47 (0.61) | 0.87 | 4.49 (0.74) |
| I have gained valuable information about cancer. | 4.79 (0.47) | 4.86 (0.35) | 0.46 | 4.82 (0.42) |
| I have made new friends who really care about me. | 4.21 (0.74) | 4.61 (0.49) | 0.01 | 4.41 (0.66) |
| I have experienced a sense of being involved in good work. | 4.74 (0.45) | 4.75 (0.44) | 0.90 | 4.74 (0.44) |
| The National Witness Project is a place where I feel I belong. | 4.66 (0.67) | 4.78 (0.42) | 0.33 | 4.72 (0.56) |
| I believe that participating in this program has helped me plan my future. | 4.21 (0.91) | 4.28 (0.97) | 0.76 | 4.24 (0.93) |
| Perceived Stressors | ||||
| I worry more about my own health. | 2.87 (1.44) | 2.42 (1.46) | 0.18 | 2.65 (1.46) |
| I feel emotionally drained from this work. | 1.61 (0.92) | 1.39 (0.64) | 0.25 | 1.50 (0.80) |
| I have felt inadequate in my ability to help other women. | 1.37 (0.63) | 1.33 (0.76) | 0.83 | 1.35 (0.69) |
| I have felt more stressed in meeting my own needs. | 1.68 (0.96) | 1.5 (0.65) | 0.34 | 1.59 (0.83) |
| I have had less energy for my own family. | 1.58 (0.89) | 1.42 (0.60) | 0.36 | 1.50 (0.76) |
| I have experienced stress in my relationship with my family members or friends because of my support work. | 1.29 (0.65) | 1.36 (0.54) | 0.61 | 1.32 (0.60) |
| I have experienced strain from the expenses of volunteering in this program. | 1.37 (0.82) | 1.5 (0.91) | 0.52 | 1.43 (0.86) |
Item responses ranged from 1=Strongly Disagree to 5= Strongly Agree
Discussion
This paper examines the characteristics and capacity of a sample of 76 female African American LHAs from NWP. Women represented a diversity of ages, educational levels, and incomes. While most LHAs were in good physical health, which will facilitate their ability to be active in LHA programs, there are opportunities for improvement since nearly 20% reported fair/poor health. Given the age of the LHA sample (mean 54.9 years), many may face new health issues as they advance in age. It will be important for LHA programs to provide support and resources to promote LHA health, particularly because LHAs serve as influential role models in their communities (Herman, 2011). LHAs reported high levels of autonomy, competence, relatedness in life, self-esteem, and purpose in life, indicating high levels of capacity at the individual-level in terms of psychological health and well-being. Research is needed to better understand whether people with these characteristics may gravitate towards LHA roles, experience enhanced psychological well-being related to these roles, or both.
Benefits experienced through program participation were numerous, including building new skills (e.g. communication) and knowledge (e.g. cancer information for self, friends and family), enhanced self-esteem, and health-related benefits (e.g. increased confidence to care for own health), which is consistent with one other small study that has examined LHA benefits (e.g. Noelle Wiggins et al. (2009)). Additionally, many of the skills and competencies reported are potentially transferable outside of the program, including those related to gaining work experience. As LHA programs expand, it will be important that the benefits that LHAs receive are better understood, as this may have implications for recruitment, their involvement in the program, and capacity-building in African American communities more broadly. Low levels of stressors were reported. Other researchers have noted the potential of LHA/CHW ‘burnout’ and emotional stress (Brownstein et al., 2011; Capner & Caltabiano, 1993). In recruiting and training LHAs, it may be important to be clear about role expectations, benefits, and potential stressors and to have support structures in place to mitigate and monitor potential stresses.
For African American LHAs, prior life experiences related to one’s racial/ethnic identity (e.g. racial pride, experiences of healthcare discrimination) may be more common among women who chose to be LHAs, particularly in programs like NWP that focus on eliminating racial disparities for cancer screening. We found racial pride to be very high and moderate experiences of medical mistrust and discrimination in healthcare were present. While there is a larger literature that has examined key motivations for volunteering (e.g. Akintola (2010)), few studies have examined motivations among LHAs, particularly among African American LHAs. These socioculturally relevant factors should be further explored as potential motivators of engagement for LHAs in racial/ethnic minority communities.
LHAs reported large and expansive social networks (with a mean of 50 members) and high levels of social support, suggesting that LHA programs are successful in recruiting women with high reach in their communities. LHAs were well-connected and are critical community resources for building capacity and promoting health. LHAs also reported extensive social network involvement in volunteerism outside of NWP, including religious and other social groups. While programs may need to be flexible to meet possible competing demands, this also indicates that there is tremendous social capital available in their networks. As such, these programs may have much broader impact and reach through naturally occurring ‘ripple effects’ of health behavior change across their communities.
Few differences were found between survivors and non-survivors, and most were consistent with differences that would be expected among women experiencing cancer (e.g. older age, lower income). There may be some room for improvement for cancer-specific knowledge, particularly among cancer survivors, and booster training may be important to consider. More research is needed to understand the experiences of survivors, including possible benefits (e.g. healing to share their story; (Pelusi & Krebs, 2005) or possible distress. It is important that LHA programs with survivors have support structures in place and consider the provision of incentives to facilitate participation.
Our findings reflect tensions in the literature about appropriate formalization and payment in the context of LHA roles, and concerns that formalizing programs will damage community relationships (Cherrington et al., 2010; Jackson & Parks, 1997). Jackson and Parks (1997) reviewed 87 African American LHA programs and found that over half paid LHAs. In our sample, almost all of the sites (three of the eight programs provided gift cards or stipends) used an unpaid volunteer model, similar to the NWP model. Paying LHAs or CHWs is a clear way to encourage LHA commitment and retention, but worker recognition, expressions of respect, opportunities for career advancement and personal growth, and supportive supervision have also been suggested as viable means of encouragement and retention (Carter-Pokras et al., 2011; Herman, 2011).
Limitations should be noted. Findings are generalizable to female-led LHA programs in African American communities, particularly those that incorporate faith or spirituality given that many of the NWP programs include spiritual or faith-based elements (e.g. hymns or prayer). Though we had excellent participation, there may be bias and differences between those that participated and those who did not given that the sample was not randomly selected. Findings presented here are cross-sectional. Longitudinal work is needed to help disentangle baseline characteristics of LHAs from characteristics built and nurtured through participation in LHA programs. Qualitative research is also needed to gain in-depth understanding of the characteristics, motivations, and capacity of LHAs.
Implications for Practice: This is the first large-scale, in-depth study of African American LHAs, and provides depth and breadth in understanding the characteristics, capacity, and contributions of LHAs and LHA programs in African American communities. LHAs in NWP have strong psychological health and engagement in life, high educational levels, and the knowledge and skills to be effective as LHAs. Our results indicate that LHAs have high levels of role satisfaction and gain numerous benefits through their participation. Given their large social networks, they have the potential and capacity to serve as leaders in their broader communities and social networks.
Despite tremendous strengths and capacity, LHAs often experience the same stressors that the populations they serve face (e.g. racial discrimination) and tend to be older, retired, and some reported poor/fair health. Furthermore, many LHAs programs are not paid and LHAs may experience some stressors given competing demands. As such, it is important that resources and structures are in place to support LHAs and more attention should be paid to understanding stressors they experience and how they can be mitigated. This may be particularly important for cancer survivors LHAs, who may also be dealing with recurrence or other issues related to their cancer experience.
The conceptual framework presented (The Framework for Assessing LHA Capacity and Contributions) can help advance theoretical and empirical research and ultimately public health impact, by advancing understanding of the individual, social and organizational capacity of LHAs and multi-level contributions and benefits of LHAs and LHAs programs. It is critical that we implement programs that are not only effective and evidence-based, but that also have high reach and impact in their broader communities. The research presented here suggests that the impact of LHAs and LHA programs are multi-level and broad-reaching, and go well-beyond the participants who attend LHA educational sessions through the NWP. We encourage researchers and practitioners to use the framework presented here to more rigorously understand these broader contributions of LHA programs, including their potential impact on: 1) LHAs themselves (e.g. their health, well-being, and career advancement); 2) the nature of LHA social networks and development of social support and capital in these networks; 3) the development of community competence and LHA participation in new roles and leadership positions in their communities; and 4) the health of program participants, members of their social networks and communities. The tremendous potential for LHA programs in addressing health disparities will require greater investment in answering these important research questions.
Acknowledgments
We are grateful to the Project Directors, Coordinators, LHAs, and Role Models from the National Witness Program who contributed their time to this study. In particular, we would like to thank and acknowledge Detric ‘Dee’ Johnson and Mattye Willis for all of their efforts and support. This research was funded by a grant from the National Cancer Institute (5R03CA150543-03, “Serving as a Lay Health Advisor: The Impact on Self and Community). The authors thank Danielle Crookes for her assistance with editing the manuscript.
References
- Akintola O. What motivates people to volunteer? The case of volunteer AIDS caregivers in faith-based organizations in KwaZulu-Natal, South Africa. Health Policy and Planning. 2010:czq019. doi: 10.1093/heapol/czq019. [DOI] [PubMed] [Google Scholar]
- Balcazar H, Rosenthal EL, Brownstein JN, Rush CH, Matos S, Hernandez L. Community health workers can be a public health force for change in the United States: three actions for a new paradigm. American Journal of Public Health. 2011;101(12):2199–2203. doi: 10.2105/AJPH.2011.300386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird ST, Bogart LM. Perceived race-based and socioeconomic status (SES)-based discrimination in interactions with health care providers. Ethnicity & Disease. 2000;11(3):554–563. [PubMed] [Google Scholar]
- Brown SL, Nesse RM, Vinokur AD, Smith DM. Providing social support may be more beneficial than receiving it results from a prospective study of mortality. Psychological Science. 2003;14(4):320–327. doi: 10.1111/1467-9280.14461. [DOI] [PubMed] [Google Scholar]
- Brownstein JN, Hirsch GR, Rosenthal EL, Rush CH. Community health workers “101” for primary care providers and other stakeholders in health care systems. The Journal of ambulatory care management. 2011;34(3):210–220. doi: 10.1097/JAC.0b013e31821c645d. [DOI] [PubMed] [Google Scholar]
- Capner M, Caltabiano ML. Factors affecting the progression towards burnout: A comparison of professional and volunteer counsellors. Psychological Reports. 1993;73(2):555–561. doi: 10.2466/pr0.1993.73.2.555. [DOI] [PubMed] [Google Scholar]
- Carter-Pokras OD, Jaschek G, Martinez IL, Brown PB, Mora SE, Newton N, Luciani I. Perspectives on Latino lay health promoter programs: Maryland, 2009. Am J Public Health. 2011;101(12):2281–2286. doi: 10.2105/ajph.2011.300317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. On the self-regulation of behavior. New York: Cambridge University Press; 1998. [Google Scholar]
- Cherrington A, Ayala GX, Elder JP, Arredondo EM, Fouad M, Scarinci I. Recognizing the diverse roles of community health workers in the elimination of health disparities: from paid staff to volunteers. Ethnicity & Disease. 2010;20(2):189. [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. Jama. 1997;277(24):1940–1944. [PubMed] [Google Scholar]
- Cutrona CE, Russell DW. In: The provisions of social relationships and adaptation to stress. Jones WH, Perman D, editors. Vol. 1. Greenwich, Connecticut: JAI Press; 1987. [Google Scholar]
- Deci EL, Ryan RM. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychological inquiry. 2000;11(4):227–268. [Google Scholar]
- Division of Cancer Control and Population Sciences, National Cancer Institute. The Witness Project: Products. Research-tested Intervention Programs (RTIPs) 2012 Apr 27; Retrieved February 13, 2015, from http://rtips.cancer.gov/rtips/productDownloads.do?programId=270521.
- Earp JA, Eng E, O’Malley MS, Altpeter M, Rauscher G, Mayne L, … Qaqish B. Increasing use of mammography among older, rural African American women: results from a community trial. American Journal of Public Health. 2002;92(4):646–654. doi: 10.2105/ajph.92.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng E, Parker E. Natural helper models to enhance a community’s health and competence. In: Diclemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research: Strategies for improving public health. San Francisco, CA: Jossey-Bass; 2002. pp. 126–156. [Google Scholar]
- Eng E, Parker E, Harlan C. Lay health advisor intervention strategies: A continuum from natural helping. Health Education & Behavior. 1997;24(4):413–417. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- Eng E, Young R. Lay health advisors as community change agents. Family & community health. 1992;15(1):24–40. [Google Scholar]
- Erwin DO. The Witness Project: Narratives that shape the cancer experience for African American women. In: McMullin J, Weiner D, editors. In confronting cancer: metaphors, advocacy, and anthropology. Sante Fe, CA: School for Advanced Research Seminar Series; 2009. pp. 125–146. [Google Scholar]
- Erwin DO, Ivory J, Stayton C, Willis M, Jandorf L, Thompson H, … Hurd TC. Replication and dissemination of a cancer education model for African American women. Cancer Control. 2003;10(5 SUPP):13–21. doi: 10.1177/107327480301005s03. [DOI] [PubMed] [Google Scholar]
- Erwin DO, Spatz TS, Stotts RC, Hollenberg JA, Deloney LA. Increasing mammography and breast self-examination in African American women using the witness project™ model. Journal of Cancer Education. 1996;11(4):210–215. doi: 10.1080/08858199609528430. [DOI] [PubMed] [Google Scholar]
- Gilkey M, Garcia CC, Rush C. Professionalization and the experience-based expert: Strengthening partnerships between health educators and community health workers. Health Promotion Practice. 2011;12(2):178–182. doi: 10.1177/1524839910394175. [DOI] [PubMed] [Google Scholar]
- Herman AA. Community health workers and integrated primary health care teams in the 21st century. The Journal of ambulatory care management. 2011;34(4):354–361. doi: 10.1097/JAC.0b013e31822cbcd0. [DOI] [PubMed] [Google Scholar]
- Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. American Journal of Public Health. 1990;80(4):446–452. doi: 10.2105/ajph.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson EJ, Parks CP. Recruitment and training issues from selected lay health advisor programs among African Americans: a 20-year perspective. Health Education & Behavior. 1997;24(4):418–431. doi: 10.1177/109019819702400403. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Green MC, Cappella JN, Slater MD, Wise ME, Storey D, … Holmes K. Narrative communication in cancer prevention and control: a framework to guide research and application. Annals of Behavioral Medicine. 2007;33(3):221–235. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Social Science & Medicine. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Landers SJ, Stover GN. Community health workers—practice and promise. American Journal of Public Health. 2011;101(12):2198. doi: 10.2105/AJPH.2011.300371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiology Biomarkers & Prevention. 2002;11(1):59–71. [PubMed] [Google Scholar]
- Lewin S, Dick J, Pond P, Zwarenstein M, Aja G, van Wyk B, … Patrick M. Lay health workers in primary and community health care. Cochrane Database of Systematic Reviews. 2005;1:CD004015. doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- Lukwago SN, Kreuter MW, Bucholtz DC, Holt CL, Clark EM. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Family & community health. 2001;24(3):63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- Mathews HF. Cancer support groups and health advocacy: One size doesn’t fit all. In: McMullin J, Weiner D, editors. Confronting cancer: Metaphors, advocacy, and anthropology. Vol. 1. Santa Fe: School of American Research; 2009. pp. 43–86. [Google Scholar]
- Nelson A. Body and soul: The Black Panther Party and the fight against medical discrimination. Minneapolis, MN: University of Minnesota Press; 2011. [Google Scholar]
- Pelusi J, Krebs LU. Understanding cancer-understanding the stories of life and living. Journal of Cancer Education. 2005;20(S1):12–16. doi: 10.1207/s15430154jce2001s_04. [DOI] [PubMed] [Google Scholar]
- Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annual Review of Public Health. 2014;35:399–421. doi: 10.1146/annurev-publhealth-032013-182354. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. American Journal of Preventive Medicine. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Riessman F. The “helper” therapy principle. Social Work. 1965:27–32. [Google Scholar]
- Roman LA, Lindsay JK, Moore JS, Shoemaker AL. Community health workers: Examining the helper therapy principle. Public Health Nursing. 1999;16(2):87–95. doi: 10.1046/j.1525-1446.1999.00087.x. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Russell KM, Champion VL, Monahan PO, Millon-Underwood S, Zhao Q, Spacey N, … Paskett ED. Randomized trial of a lay health advisor and computer intervention to increase mammography screening in African American women. Cancer Epidemiology Biomarkers & Prevention. 2010;19(1):201–210. doi: 10.1158/1055-9965.EPI-09-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier MF, Wrosch C, Baum A, Cohen S, Martire LM, Matthews KA, … Zdaniuk B. The life engagement test: Assessing purpose in life. Journal of Behavioral Medicine. 2006;29(3):291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- Schriesheim C, Tsui AS. Development and validation of a short satisfaction instrument for use in survey feedback interventions. Paper presented at the Western Academy of Management Meeting.1980. [Google Scholar]
- Sellers RM, Smith MA, Shelton JN, Rowley SA, Chavous TM. Multidimensional model of racial identity: A reconceptualization of African American racial identity. Personality and Social Psychology Review. 1998;2(1):18–39. doi: 10.1207/s15327957pspr0201_2. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Franks JC, Lehavot K, Yard SS. Peer interventions to promote health: conceptual considerations. American Journal of Orthopsychiatry. 2011;81(3):351. doi: 10.1111/j.1939-0025.2011.01103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South J, White J, Branney P, Kinsella K. Public health skills for a lay workforce: findings on skills and attributes from a qualitative study of lay health worker roles. Public Health. 2013;127(5):419–426. doi: 10.1016/j.puhe.2013.02.014. [DOI] [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med. 2004;38(2):209–218. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- Vijaykumar S, Wray RJ, Jupka K, Clarke R, Shahid M. Prostate Cancer Survivors as Community Health Educators: Implications for Informed Decision Making and Cancer Communication. Journal of Cancer Education. 2013;28(4):623–628. doi: 10.1007/s13187-013-0559-9. [DOI] [PubMed] [Google Scholar]
- Viswanathan M, Kraschnewski J, Nishikawa B, Morgan LC, Thieda P, Honeycutt A, … Jonas D. Outcomes of community health worker interventions. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [PMC free article] [PubMed] [Google Scholar]
- Wells KJ, Luque JS, Miladinovic B, Vargas N, Asvat Y, Roetzheim RG, Kumar A. Do community health worker interventions improve rates of screening mammography in the United States? A systematic review. Cancer Epidemiology Biomarkers & Prevention. 2011 doi: 10.1158/1055-9965.EPI-11-0276. cebp.0276.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins N, Bourbón IA. Final report of the National Community Health Advisor Study. Baltimore, MD: Annie E. Casey Foundation; 1998. Core roles and competencies of community health workers; pp. 15–49. [Google Scholar]
- Wiggins N, Johnson D, Avila M, Farquhar SA, Michael YL, Rios T, Lopez A. Using popular education for community empowerment: perspectives of Community Health Workers in the Poder es Salud/Power for Health program. Critical Public Health. 2009;19(1):11–22. [Google Scholar]
- Zimmerman MA, Zahniser JH. Refinements of sphere-specific measures of perceived control: Development of a sociopolitical control scale. Journal of Community Psychology. 1991;19(2):189–204. [Google Scholar]