Abstract
Although sleep apps are among the most popular commercially available health apps, little is known about how well these apps are grounded in behavioral theory. Three-hundred and sixty-nine apps were initially identified using the term “sleep” from the Google play store and Apple iTunes in September 2015. The final sample consisted of 35 apps that met the following inclusion criteria: 1) Stand-alone functionality; 2) Sleep tracker or monitor apps ranked by 100 + users; 3) Sleep Alarm apps ranked by 1000 + users; and 4) English language. A coding instrument was developed to assess the presence of 19 theoretical constructs. All 35 apps were downloaded and coded. The inter-rater reliability between coders was 0.996. A “1” was assigned if a construct was present in the app and “0” if it was not. Mean scores were calculated across all apps, and comparisons were made between total scores and app ratings using R. The mean behavior construct scores (BCS) across all apps was 34% (5% - 84%). Behavioral constructs for realistic goal setting (86%), time management (77%), and self-monitoring (66%) were most common. Although a positive association was observed between BCS and user ratings, this was not found to be statistically significant (p > 0.05). The mean persuasive technology score was 42% (20% to 80%), with higher scores for paid compared to free apps (p < 0.05). While the overall behavior construct scores were low, an opportunity exists to develop or modify existing apps to support sustainable sleep hygiene practices.
Keywords: Sleep, Apps, Health behavior, Mobile health, Mhealth
1. Introduction
Recent estimates from the Centers for Disease Control and Prevention (CDC) indicate that > 30% of Americans report sleeping less than the recommended 7 h per night (Liu et al., 2016). The inability to meet nightly recommendations for sleep may increase an individual's risk for several adverse health outcomes, including heart disease, overweight and obesity, impaired cognitive functioning, and depression, among others (Altevogt and Colten, 2006, Gallicchio and Kalesan, 2009, Grandner et al., 2014, Liu et al., 2013). Poor sleep also negatively impacts the United States (US) healthcare system. In 2010, an estimated $65 to $165 billion (Mckinsey and Company, 2010) was spent to treat moderate-to-severe obstructive sleep apnea, and the average individual cost to treat insomnia syndrome was $5010 (Daley et al., 2009). Consequently, population-based efforts to encourage good sleeping habits are important for reducing this public health burden.
There is emerging consensus that mobile technology and apps have the potential to support health behavior change to reduce chronic disease risk associated with lifestyle factors such as healthy nutrition, physical activity, and sleep (Tate et al., 2013, Hingle et al., 2010, Knowlden et al., 2012, Staniford et al., 2011, Schoffman et al., 2013). Apps have the unique ability to be highly accessible due to their ubiquity, personal nature, and programming flexibility (e.g., automated sensors) (Tate et al., 2013). Compared to static data collection efforts (e.g., self-reported surveys), mobile technology and apps also allow researchers to collect data in real-time, thus providing immediate, useful information for tailoring health interventions. Given recent estimates that approximately 72% of Americans report owning a smartphone (Aaron, 2015, Poushter, 2016) and that roughly 20% download health apps on their phones (Fox and Duggan, 2012), this provides an excellent opportunity to reach individuals at risk for poor sleeping habits. In fact, Terry (2015) approximates that although 16% of physicians currently prescribe health apps, this figure is predicted to increase to 46% within the next five years. Proponents of the “quantified self” movement also argue that health tracking empowers patients to take charge of their health routines (Van den Bulck, 2015), and allows for the potential for personalized interventions and support outside of the physician's office (Higgins, 2016).
Although sleep apps are among the most popular commercially available health apps, little is known about how well these apps follow evidenced-based guidelines or are grounded in behavioral theory. Moreover, most studies examining the role sleep apps play in sleep behaviors have focused on comparisons in measurement accuracy between laboratory methods such as polysomnography and accelerometer-based apps to track sleep patterns (Bianchi, 2015, Ko et al., 2015, Bhat et al., 2015). As Bianchi (2015) argues, however, an opportunity exists to educate consumers about sleep medicine and wellness using sleep apps. We present an analysis of the incorporation of theoretical constructs of behavior change in popular sleep apps created for smartphones using Android and iOS platforms. Adherence to recommended guidelines has been correlated with the popularity of apps based on user ratings for smoking cessation apps (Abroms et al., 2013), but this correlation was not found for weight loss and physical activity apps (Schoffman et al., 2013, Pagoto et al., 2013). As evidence-based apps have been shown to be the least popular among consumers (Pagoto et al., 2013), however, we also examine the persuasiveness of the apps, as we are interested in both the usability (e.g., app interface), as well as the integration of behavioral constructs. To this end, we reviewed theories that have been successful for diet and physical activity interventions such as the trans-theoretical model, the health belief model, the theory of planned behavior, and social cognitive theory (Van Dorsten and Lindley, 2011). As Azar et al. (2013) note, it is imperative to also examine contemporary theories which incorporate the influence of technology on health behaviors, such as the Fogg Behavioral Model (FBM) of persuasive design (Fogg, 2003, Fogg, 2009). The FBM posits behavior change is predicated on how well design elements of a particular technology motivates an individual to use their ability to respond to triggers to modify behaviors (Fogg, 2003, Fogg, 2009). The specific questions we hope to address with this study are: 1) Which theoretical constructs are commonly included in sleep apps? 2) Is there an association between the presence of behavioral constructs and the popularity of the apps? We hypothesize that apps with more behavioral constructs will provide better evidence for app developers to make informed decisions regarding which behavioral constructs to include in the sleep app development process.
2. Methods
2.1. Study design
This study is a descriptive analysis of the most downloaded and reviewed sleep apps found in the iTunes App Store and the Google Play Store in September 2015. Following the work of Azar et al. (2013), we examined theoretical constructs typically used in behavioral interventions for other lifestyle factors, such as physical activity. Specific examples of the integration of constructs can be found in Table 1. We also used the “persuasive technology score” (PTS) developed by Azar et al. (2013) based on the Fogg Behavioral Model (FBM) (Fogg, 2003, Fogg, 2009) which examines the role of technology in motivating behavior change. Specific aspects of the FBM that were considered as part of the app review process were motivators (e.g., praise or encouragement), features that improve the ability of individuals to engage in a specific behavior (e.g., tailored information), and triggers (e.g., positive feedback) to encourage the promotion of a particular behavior.
Table 1.
Description of theoretical constructs and persuasive technology components for sleep apps, N = 35.
| Construct | Description | Number of apps (%) |
|---|---|---|
| Knowledge: 1 item | ||
| 1. General information about sleep | General information about sleep | 15 (43%) |
| Cognitive: 6 items | ||
| 2. Perceived benefits (pros)/information about benefits | Benefits of sleep | 4 (11%) |
| 3. Perceived barriers (cons)/information about perceived barriers | Barriers to sleep (food, daily habits) | 5 (14%) |
| 4. Perceived risks/information about risks | Risk associated with insufficient sleep (physiological, emotional negative effects) | 4 (11%) |
| 5. Self-efficacy | Confidence about sleep control (time, amount) | 13 (37%) |
| 6. Self-talk | Quote, catchphrase, maxim | 5 (14%) |
| 7. Perceived social norms | Optimal sleep duration | 13 (37%) |
| Behavioral: 8 items | ||
| 8. Self-monitoring | Tracking sleep patterns and time | 23 (66%) |
| 9. Realistic goal-setting | Specific goals for better sleep | 30 (86%) |
| 10. Time management | Managing sleep time | 27 (77%) |
| 11. Stimulus-control (cues and prompts) | Reminder messages for sleep | 6 (17%) |
| 12. Self-reward | Praise, reward points | 1 (3%) |
| 13. Social support | Posting on Social Network System (SNS) (e.g. amount of sleep) | 14 (40%) |
| 14. Modeling/vicarious learning | Positive Imagery related to sleep hygiene, current user's commentary | 6 (17%) |
| 15. Relapse prevention | Guidance for getting back on track to meet goals | 4 (11%) |
| Emotional focused: 2 items | ||
| 16. Stress management | Reduce and decease stress factors | 17 (49%) |
| 17. Negative affect management | Managing negative effect of poor sleep habits | 13 (37%) |
| Therapeutic intervention: 2 items | ||
| 18. Skill building/overview | Evaluation of sleep patterns | 19 (54%) |
| 19. Increasing knowledge | Better understanding about sleep | 10 (29%) |
| Persuasive Technology Component | Description | Number of apps (%) |
|---|---|---|
| Motivation: 2 items | ||
| 1. Social praise | Social Network System (SNS) (e.g. amount of sleep) | 14 (40%) |
| 2. Provides non-financial incentives | Praise | 1 (3%) |
| Simplicity: 1 item | ||
| 3. Provides decreased barriers | User friendly design (e.g. icons, interface) | 33 (94%) |
| Trigger: 2 items | ||
| 4. Provides positive feedback | Evaluation, overview, commentary | 19 (54%) |
| 5. Provides automatic reminders/cues | Reminder messages for sleep | 6 (17%) |
2.2. App selection process
App selection and review occurred in September 2015. Apps were selected from the Google Play Store (N = 272) and the Apple iTunes Store (N = 97) using the term “sleep.” Three-hundred and sixty-nine apps were initially identified. However, 39 apps were found in both the iTunes App Store and Google Play Store, resulting in 330 unique apps. Forty-seven apps were selected based on the following criteria: 1) sleep monitor/tracker apps downloaded by 100 + reviewers; and 2) sleep alarms downloaded by 1000 + reviewers. Apps were excluded if they: 1) did not have stand-alone functionality (e.g., not part of another app), 2) duplicated free apps; 3) were used for meditation; 4) were used for babies; 5) were not English language; or 6) were found not to be actual sleep apps. The final sample for review consisted of 35 apps. Eighty percent (28) of the apps were free, while 20% (7) were paid, with an average price of $2.10 ($0.99–$4.99).
2.3. Evaluation criteria
A coding instrument was developed to assess the presence of 19 theoretical constructs in the following five categories: 1) knowledge (N = 1); 2) cognitive strategies (N = 6), 3) behavior strategies (n = 8), 4) emotion-focused strategies (N = 2), and 5) therapeutic interventions (N = 2). In addition, a persuasive technology score (PTS) was calculated based on the following categories: 1) motivation (N = 2), 2) simplicity (N = 1), and 3) trigger (N = 2). All 35 apps were downloaded and coded to evaluate content. The inter-rater reliability between coders was 0.996. A “1” was assigned if a construct was present in the app and “0” if it was not. Mean scores were calculated across all apps, and comparisons were made between total scores and app ratings using R (R Core Team, 2015). The maximum behavioral construct score (BCS) possible was 19, while the maximum PTS was 5, for a total maximum score of 24. App reviewer scores from the Google Play Store and Apple iTunes were typically on a scale from 0 to 5, with 5 being the highest rating.
2.4. Data analysis
Mean BCS, PTS, and standard deviations were calculated across all apps, and comparisons were made between total scores and user app ratings using the R statistical program version 3.1.3 (R Core Team, 2015). A Pearson's correlation coefficient was calculated to examine the association between app ratings by users and mean BCS and PTS. Mean BCS and PTS were also compared between paid and free apps.
3. Results
High interrater reliability was observed for both BCS (99.91%) and PTS (99.94%) between coders. The mean BCS across all apps was 34% (SD, 21%; range, 5% to 84%). Behavioral constructs for realistic goal setting (86%), time management (77%), and self-monitoring (66%) were most common. iOS apps (33%) had higher BCS compared to android apps (30%), and a positive association was observed between BCS and user ratings, but neither was found to be statistically significant (p > 0.05). The mean PTS across all apps was 42% (SD, 22%; range, 20% to 80%). Factors that contributed most to the persuasiveness of the app were the user interface (94% of all apps) and the provision of positive feedback (54%). Mean PTS was higher for iOS (40%) compared to Android (36%), but this was not found to be significant (p < 0.05). A high Pearson's correlation coefficient (r = 0.907) was observed between the app review ratings and the BCS. Paid apps had slightly higher BCS and PTS compared to free apps (Fig. 1), but this difference was only significant for PTS.
Fig. 1.
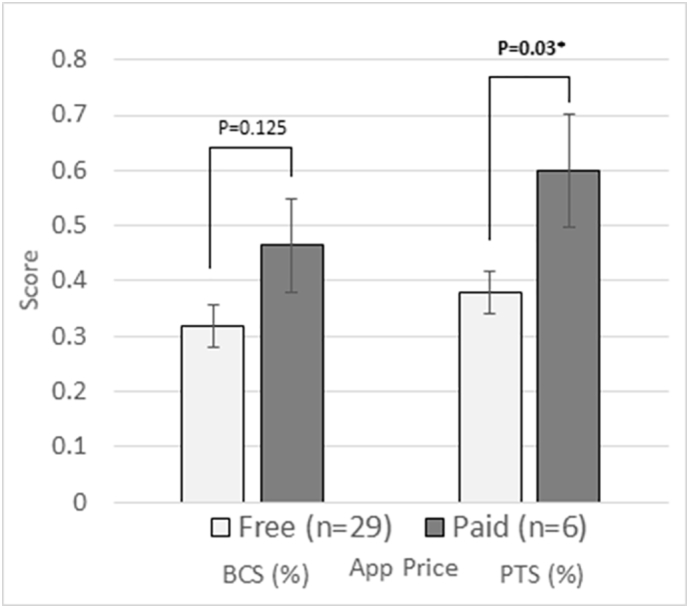
Comparison of Behavior Construct Score (BCS) and Persuasive Technology Score (PTS) between Paid and Free Apps.
4. Discussion
Our study represents one of the few to examine the incorporation of behavioral constructs in sleep apps. While most studies examining sleep apps have focused primarily on comparisons with laboratory procedures, such as polysomnography (Bhat et al., 2015), a limited number have explored the role of apps as tools for behavior change. We found that constructs from the social cognitive theory were the most aligned with the apps examined. App developers have incorporated tools for realistic goal setting, time management and self-monitoring which could be beneficial to individuals with diagnosed sleep disorders. Additionally, we were encouraged by the association between user ratings and BCS and PTS, suggesting that the most popular apps are also well-designed for encouraging healthy sleep hygiene. This also bodes well for future integration of additional behavioral constructs for sleep apps. It is still of concern, however, that many of the constructs are not included in many apps currently on the market. Notwithstanding, these findings are consistent with similar studies that have found limited integration of behavioral constructs for other apps targeting lifestyle behaviors (Azar et al., 2013, Crane et al., 2015).
While our study suggests future development of mobile phone apps integrating behavioral constructs could positively influence sleep behaviors, it is also worth noting that the use of technology close to bedtime has been shown to adversely impact sleep. Chang et al. (2015) for example, found that using light emitting devices (LED) (e.g., eReaders) before bedtime disrupts one's circadian rhythm. Additionally, the positive impact of sleep on one's cognitive function may be impaired after the use of LEDs at bedtime, specifically limited alertness (Chang et al., 2015). The presence of a smart phone in a bedroom has also been shown to disrupt sleep among adolescents (Adachi-Mejia et al., 2014). Since smart phones and other LEDs are commonly found in bedrooms, however, an opportunity still exists to encourage better sleep hygiene. Additional functions of sleep apps may include features that shut off phones once an alarm is set to minimize light exposure, or the disabling of notifications of text messages to minimize sleep disruption.
5. Strengths and limitations
Although our results are somewhat encouraging, we did not download and examine actual sleep data entered into the app by users. Therefore, our app review may not accurately reflect the manner in which actual users will interact with the app in the future. New apps are also constantly being added to the iOS and Android platforms, so our analysis may not reflect the current sleep app landscape. Moreover, the small sample size precluded more advanced statistical analysis. To our knowledge, however, there are no other studies that have systematically examined the integration of behavioral constructs of sleep apps on iOS and android platforms.
6. Conclusions
Mobile technology and apps have the potential to shape behaviors related to healthy sleep habits. While few of the apps examined included features to support behavior change, an opportunity exists to encourage sustainable sleep hygiene practices using mobile phones.
References
- Aaron S. U.S. Smartphone Use in 2015. 2015. http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/ Retrieved from.
- Abroms L.C., Westmaas J.L., Bontemps-Jones J., Ramani R., Mellerson J. A content analysis of popular smartphone apps for smoking cessation. Am. J. Prev. Med. 2013;45(6):732–736. doi: 10.1016/j.amepre.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adachi-Mejia A.M., Edwards P.M., Gilbert-Diamond D., Greenough G.P., Olson A.L. Txt me I'm only sleeping: adolescents with mobile phones in their bedroom. Fam. Community Health. 2014;37(4):252–257. doi: 10.1097/FCH.0000000000000044. [DOI] [PubMed] [Google Scholar]
- Altevogt B.M., Colten H.R. National Academies Press; Washington, DC: 2006. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. [PubMed] [Google Scholar]
- Azar K.M., Lesser L.I., Laing B.Y. Mobile applications for weight management: theory-based content analysis. Am. J. Prev. Med. 2013;45(5):583–589. doi: 10.1016/j.amepre.2013.07.005. [DOI] [PubMed] [Google Scholar]
- Bhat S., Ferraris A., Gupta D. Is there a clinical role for smartphone sleep apps? Comparison of sleep cycle detection by a smartphone application to polysomnography. J. Clin. Sleep Med. 2015;11(7):709–715. doi: 10.5664/jcsm.4840. http://doi.org/10.5664/jcsm.4840/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi M.T. Consumer sleep apps: when it comes to the big picture, it's all about the frame. J. Clin. Sleep Med. 2015;11(7):695. doi: 10.5664/jcsm.4834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang A.M., Aeschbach D., Duffy J.F., Czeisler C.A. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc. Natl. Acad. Sci. 2015;112(4):1232–1237. doi: 10.1073/pnas.1418490112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2015. R: A Language and Environment for Statistical Computing. (Retrieved from https://www.R-project.org/) [Google Scholar]
- Crane D., Garnett C., Brown J., West R., Michie S. Behavior change techniques in popular alcohol reduction apps: content analysis. J. Med. Internet Res. 2015;17(5) doi: 10.2196/jmir.4060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley M., Morin C.M., LeBlanc M., Grégoire J.-P., Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32(1) [PMC free article] [PubMed] [Google Scholar]
- Fogg B.J. Burlington; Massachusetts: 2003. Persuasive Technology: Using Computers to Change what We Think and Do: Morgan Kaufmann Publishers. [Google Scholar]
- Fogg B.J. Paper Presented at the Proceedings of the 4th International Conference on Persuasive Technology. 2009. A behavior model for persuasive design. [Google Scholar]
- Fox S., Duggan M. Retrieved from Washington. USA; D.C.: 2012. Mobile health 2012: half of smartphone owners use their devices to get health information and one-fifth of smartphone owners have health apps. [Google Scholar]
- Gallicchio L., Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J. Sleep Res. 2009;18(2):148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- Grandner M.A., Chakravorty S., Perlis M.L., Oliver L., Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15(1):42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P. Smartphone applications for patients' health and fitness. Am. J. Prev. Med. 2016;129(1):11–19. doi: 10.1016/j.amjmed.2015.05.038. [DOI] [PubMed] [Google Scholar]
- Hingle M.D., O'Connor T.M., Dave J.M., Baranowski T. Parental involvement in interventions to improve child dietary intake: a systematic review. Prev. Med. 2010;51(2):103–111. doi: 10.1016/j.ypmed.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlden A.P., Sharma M., Bernard A.L. A Theory of Planned Behavior research model for predicting the sleep intentions and behaviors of undergraduate college students. J. Prim. Prev. 2012;33(1):19–31. doi: 10.1007/s10935-012-0263-2. [DOI] [PubMed] [Google Scholar]
- Ko P.T., Kientz J.A., Choe E.K., Kay M., Landis C.A., Watson N.F. Consumer sleep technologies: a review of the landscape. J. Clin. Sleep Med. 2015;11:1455–1461. doi: 10.5664/jcsm.5288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Wheaton A.G., Chapman D.P., Croft J.B. Sleep duration and chronic diseases among US adults age 45 years and older: evidence from the 2010 behavioral risk factor surveillance system. Sleep. 2013;36(10):1421. doi: 10.5665/sleep.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Wheaton A.G., Chapman D.P., Cunningham T.J., Lu H., Croft J.B. Prevalence of healthy sleep duration among adults-United States, 2014. MMWR Morb. Mortal. Wkly Rep. 2016:65. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- McKinsey & Company . 2010. The Price of Fatigue: The Surprising Economic Costs of Unmanaged Sleep Apnea. (Retrieved from https://www.sleep.med.harvard.edu/file_download/100/) [Google Scholar]
- Pagoto S., Schneider K., Jojic M., DeBiasse M., Mann D. Evidence-based strategies in weight-loss mobile apps. Am. J. Prev. Med. 2013;45(5):576–582. doi: 10.1016/j.amepre.2013.04.025. [DOI] [PubMed] [Google Scholar]
- Poushter J. 2016. Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economies: But Advanced Economies Still Have Higher Rates of Technology Use. (Retrieved from http://www.pewglobal.org/2016/02/22/smartphone-ownership-and-internet-usage-continues-to-climb-in-emerging-economies/) [Google Scholar]
- Schoffman D.E., Turner-McGrievy G., Jones S.J., Wilcox S. Mobile apps for pediatric obesity prevention and treatment, healthy eating, and physical activity promotion: just fun and games? Trans. Behav. Med. 2013;3(3):320–325. doi: 10.1007/s13142-013-0206-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staniford L.J., Breckon J.D., Copeland R.J., Hutchison A. Key stakeholders' perspectives towards childhood obesity treatment: a qualitative study. J. Child Health Care. 2011;15(3):230–244. doi: 10.1177/1367493511404722. [DOI] [PubMed] [Google Scholar]
- Tate E.B., Spruijt-Metz D., O’Reilly G. Behav. Med. Pract. Policy Res. 2013;3:406. doi: 10.1007/s13142-013-0222-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry K. 2015. Prescribing Mobile Apps: What to Consider-lessons That Other Physicians Have Learned About Using Mobile Apps to Help Treat Patients. (Retrieved from http://medicaleconomics.modernmedicine.com/medical-economics/news/prescribing-mobile-apps-what-consider?page=full) [Google Scholar]
- Van den Bulck J. Sleep apps and the quantified self: blessing or curse? J. Sleep Res. 2015;24(2):121–123. doi: 10.1111/jsr.12270. [DOI] [PubMed] [Google Scholar]
- Van Dorsten B., Lindley E.M. Cognitive and behavioral approaches in the treatment of obesity. Med. Clin. N. Am. 2011;95(5):971–988. doi: 10.1016/j.mcna.2011.06.008. [DOI] [PubMed] [Google Scholar]


