Abstract
Despite community health centers’ substantial role in local communities and in the broader safety‐net healthcare system, very limited research has been conducted on community health center research experience, infrastructure, or needs from a national perspective. A national survey of 386 community health centers was conducted in 2011 and 2012 to assess research engagement among community health centers and their perceived needs, barriers, challenges, and facilitators with respect to their involvement in public health and health services research. This paper analyzes the differences between health centers that currently conduct or participate in research and health centers that have no prior research experience to determine whether prior research experience is indicative of different perceived challenges and research needs in community health center settings.
Introduction
With over 8,500 healthcare delivery sites serving more than 20 million low‐income and underserved patients in every state and territory in the United States, community health centers (CHCs) are not only an essential source of comprehensive primary care but also a largely untapped wealth of community‐based resources, knowledge, and expertise for public health and health services research.1 Not only do health centers provide high quality and culturally competent healthcare to populations that experience the most severe health disparities, but they understand their local community and have a deep, significant knowledge of the people they serve. Health center‐based research often builds off of health centers’ existing experience and skills in conducting formal and regular needs assessments, engaging in quality improvement activities, mining electronic health data for trends, and participating in various networks. Furthermore, health centers balance their mission of delivering quality health services in high‐need communities with often limited funding and scarce resources, requiring them to seek innovative operating strategies and clinical interventions to improve the health of their communities. These unique characteristics across health centers’ mission, clinical operations, and community knowledge place health centers at the intersection where research translates to practice.
Despite health centers’ substantial role in both local communities and in the broader safety‐net, very limited research has been conducted on health center research experience, infrastructure, or needs on a national basis, although many health centers have participated in local assessments. Only a few studies reveal barriers and facilitators experienced by a small group of health centers, but no national compendium of these key factors has been developed to date.2, 3, 4, 5, 6, 7 Understanding the most substantial barriers to conducting research in health center settings will help to provide valuable insight around what resources are needed to continue building capacity for health centers to address high‐priority community research questions. Building off a previous report on health center research engagement, this paper analyzes the differences between health centers that currently conduct or participate in research and health centers that currently do not participate in research to determine whether prior research experience is indicative of different perceived challenges and research needs in health center settings.8
Methods
The Clinical and Translational Science Institute at Children's National Medical Center, in partnership with the George Washington University, collaborated with the National Association of Community Health Centers, the Community Health Applied Research Network (CHARN), the South Carolina Primary Health Care Association (SCPHCA), and the University of South Carolina (USC) Cancer Prevention and Control Research Network to field a national survey that assesses health centers’ participation in research, their research interests, and their research capacity needs. For the purposes of this survey, research was defined as “a systematic investigation designed with the intention of (1) advancing knowledge (e.g., designed to draw conclusions or inferences), and (2) publishing or otherwise publicly disseminating the results to audiences outside the local community served (e.g., scholarly journal article, conference presentation, report or brief posted online, or community forum). In many cases, research is also intended to produce results that can be generalized or spread to new patients and settings. Research is often but not exclusively conducted in collaboration or partnership with external researchers and/or through a research consortium.” The survey was fielded to all federally funded health centers (also known as federally qualified health centers) over several months between 2011 and 2012, with a 35.3% response rate (n = 386). Further discussion on the survey fielding, administration methods, and limitations is referenced elsewhere.8
For the purposes of identifying differences between health centers that currently participate in research and those that do not, we conducted bivariate analysis using unpaired t‐tests on health centers’ perceived challenges and barriers. We used similar methods to determine whether significant differences exist among the training and technical assistance (T/TA) needs of those health centers with research experience and those with no such experience.
Results
Of the 386 respondent health centers representing a 35% response rate, over half (56%) reported that they have ever conducted or participated in research, either as the lead researcher or as a partner. Figure 1 indicates health centers’ involvement in research activities from participating in research as partner organizations (71%) to conducting or leading research on their own (23%).
Figure 1.
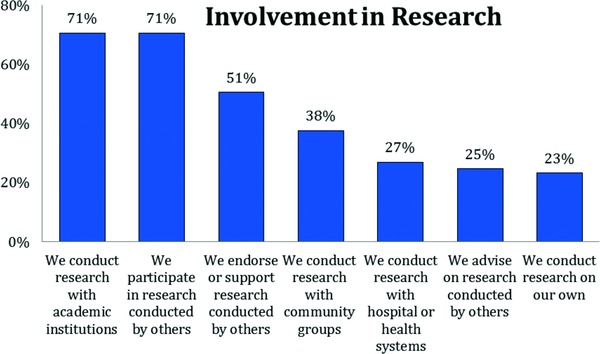
Health centers’ involvement in research.
Among those that do not currently participate in research, 58% responded that they would be interested in participating in research in the future, with 13% indicating interest in leading research activities and 45% interested in partnering with external researchers. Sixty‐nine percent of health centers that already have research experience are interested in enhancing or expanding their research activities, indicating that there is a considerable desire for growth in research and capacity to conduct research activities. Figure 2 shows the interest and participation in research activities reported by our respondents.
Figure 2.
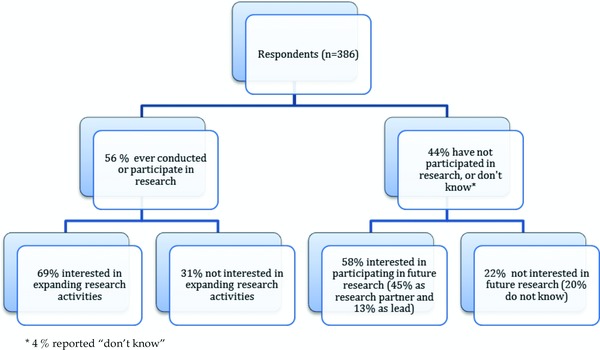
Respondents’ interest and participation in research efforts.
Perceived barriers to participating in research
We asked health centers to indicate barriers to their participation in research. Among the health centers responding to the survey questions about research barriers, the most frequently reported barriers1 to research participation across all respondents were lack of dedicated staff time to do research (87%), concerns about loss of productivity or income (80%), lack of training in conducting research (72%), and lack of eligible funding opportunities (72%). Table 1 illustrates the percent of health centers that currently engage in research and those that do not do research who reported experiencing barriers in a number of research‐related areas.
Table 1.
Barriers to research participation, by research engagement
| All health centers (N = 363–365)† % | Health centers with research experience (N = 211‒214)† % | Health centers with no prior research experience (N = 150–153)† % | Statistical significance p‐value* | ||
|---|---|---|---|---|---|
| (a) Dedicated staff time to conduct or participate in research | 86.57 | 83.64 | 90.73 | 0.0508 | |
| (b) Concern about loss of productivity or income during research activities | 80.33 | 73.83 | 89.47 | 0.0002 | * |
| (c) Funding opportunities for which our health center is eligible | 71.70 | 73.24 | 69.54 | 0.4411 | |
| (d) Training in applying for and conducting research (e.g., developing protocols) | 72.25 | 62.91 | 85.43 | 0.0001 | * |
| (e) Methods to publish/disseminate findings | 63.53 | 55.45 | 74.83 | 0.0001 | * |
| (f) Data analysis | 60.00 | 53.52 | 69.08 | 0.0027 | * |
| (g) Ability to recruit and retain research subjects | 55.80 | 40.57 | 74.83 | 0.0001 | * |
| (h) Data collection infrastructure (including information technology) | 55.89 | 50.23 | 63.82 | 0.0099 | * |
| (i) An understanding about what is involved to conduct research | 53.15 | 43.92 | 66.23 | 0.0001 | * |
| (j) Policies or procedures specifying how to prioritize research projects and/or select partners | 52.47 | 40.38 | 69.54 | 0.0001 | * |
| (k) Incentives for partnerships between academic and community organizations (e.g., financial and nonfinancial resources) | 51.24 | 51.17 | 51.33 | 0.9762 | |
| (l) Support or interest from clinical staff | 49.73 | 45.07 | 56.21 | 0.0356 | * |
| (m) Access to research collaborators/partners | 49.04 | 36.45 | 66.89 | 0.0001 | * |
| (n) Institutional Review Board (IRB) or ethical review expertise | 47.80 | 33.33 | 68.21 | 0.0001 | * |
| (o) Writing/editorial expertise | 48.63 | 43.19 | 56.29 | 0.0137 | * |
| (p) Technology needs (e.g., information technology/electronic records, audio/video conferencing, computer hardware/software) | 45.32 | 41.51 | 50.66 | 0.0840 | |
| (q) Alignment of research‐related activities with health center's mission | 41.40 | 43.46 | 38.56 | 0.3492 | |
| (r) Support or interest from nonclinical staff | 41.60 | 39.91 | 44.08 | 0.4267 | |
| (s) Support or interest from governing board | 22.90 | 13.08 | 36.84 | 0.0001 | * |
| (t) Prior research experiences that staff perceived as negative | 18.68 | 19.25 | 17.88 | 0.7423 | |
| (u) Other | 10.37 | 8.75 | 12.72 | 0.4600 |
*Statistically significant at α = 0.05. This indicates that the difference between health centers that have conducted or participated in research and those that have not is statistically different. Where * does not appear, results can be interpreted to be comparable or not statistically different.
†Differences in total number of respondents vary by whether respondents answered the full set of survey questions.
Not surprisingly, health centers with no previous research experience reported higher percentages of barriers in nearly all categories, compared with health centers that have participated in research activities before. These significant differences in barriers to research engagement reported between health centers currently participating in research and those without research experience are included in Table 1. “Lack of dedicated staff time” and “concern about loss of productivity or income” remained the two highest reported barriers across the two groups. However, health centers who had not done research in the past were significantly more concerned about loss of productivity (89%) than health centers who were currently or formerly engaged in research activities (74%) (p = 0.002). While similar proportions of health centers across both groups identified a lack of eligible funding opportunities as a barrier, research‐engaged health centers reported this as the third highest barrier to research participation while it dropped to the sixth most frequently reported barrier among health centers with no prior research experience, although this difference was not statistically significant (p = 0.4411).
Health centers with no prior research experience were also significantly more concerned with gaining support from key players including clinical staff (p‐value = 0.0356) and their governing board (p = 0.0001) compared with health centers that are engaged in research activities. In addition, higher proportions of health centers with no research experience reported that a lack of understanding about what is involved in the research experience was a perceived barrier, compared with health centers that already do research (p = 0.001). A focus on partnerships and policies for research participation also emerged in the survey data with higher reported barriers in access to research partners among health centers that were not engaged in research at the time of the survey (p = 0.0001). Policies to prioritize research were also more frequently reported by this group compared to health centers that already had research experience (p < 0.0001).
Other differences in reported barriers between the groups are most pronounced in internal capacity factors such as infrastructure and research expertise, training, or support. For example, compared to health centers engaged in research, higher proportions of health centers with no previous research experience reported barriers in data collection infrastructure (p = 0.0099) and data analysis capabilities (p = 0.0027) as well as methods to disseminate and publish research findings (p = 0.0001). Similarly, training in applying for research (p = 0.0001), ability to recruit research subjects (p = 0.0001), writing/editorial expertise (p = 0.0137), and IRB expertise (p = 0.0001) were more frequently reported among health centers with no previous research experience when compared with their research‐engaged counterparts.
The fact that health centers that were not engaged in research more frequently reported barriers in nearly every category reveals key opportunities to develop activities and partnerships to engage health centers in the research process as well as offer tools and training to enhance their expertise, infrastructure, and roles as active research leaders and partners. Of note, both groups of health centers reported lack of eligible funding opportunities at similarly high levels.
Topics of interest for training
In order to provide insight into the training and resources needs related to research engagement at health centers, we asked respondents to indicate topics on which they were either interested or very interested in receiving training. The reported T/TA interests align with the health centers’ reported barriers. Table 2 shows the percent of health centers in both groups that reported interest in receiving training or technical assistance across a range of topics.
Table 2.
Topics of interest for training and technical assistance, by research engagement
| All health centers (N = 281–284) % | Health centers with research experience (N = 212–214) % | Health centers with no prior research experience (N = 68–70) % | p‐Value | ||
|---|---|---|---|---|---|
| (a) Finding and capitalizing on funding opportunities | 86.57 | 85.05 | 91.30 | 0.1862 | |
| (b) Using research to inform programs and services | 70.67 | 68.22 | 78.26 | 0.1121 | |
| (c) Using research to inform public policy | 64.41 | 62.44 | 70.59 | 0.2233 | |
| (d) Grant and proposal writing for research and evaluation | 60.77 | 54.93 | 78.57 | 0.0004 | * |
| (e) Finding, developing, and sustaining community‐academic partnerships | 56.54 | 50.93 | 73.91 | 0.0008 | * |
| (f) Dissemination and reporting of research findings | 56.18 | 51.87 | 69.57 | 0.0099 | * |
| (g) Data collection methods (e.g., surveys, focus groups) | 54.57 | 49.53 | 70.00 | 0.0027 | * |
| (h) Developing research aims or research questions | 54.06 | 49.53 | 68.12 | 0.0070 | * |
| (i) Research ethics (e.g., ethical review, issues of HIPAA and/or privacy) | 53.71 | 49.53 | 66.67 | 0.0130 | * |
| (j) Recruitment of and follow‐up with research participants | 52.84 | 46.48 | 72.46 | 0.0002 | * |
| (k) Conducting statistical data analyses | 52.30 | 46.73 | 69.57 | 0.0009 | * |
| (l) Project management for research | 52.11 | 47.66 | 65.71 | 0.0086 | * |
| (m) Finding and using information from health and medical articles | 48.58 | 42.72 | 66.67 | 0.0005 | * |
| (n) Study design and research methods | 46.83 | 42.06 | 61.43 | 0.0047 | * |
| (o) Developing a database | 47.70 | 41.12 | 68.12 | 0.0001 | * |
| (p) Data entry, cleaning, and coding | 45.04 | 38.97 | 63.77 | 0.0003 | * |
| (q) Obtaining buy‐in from staff and/or governing board | 37.81 | 33.18 | 52.17 | 0.0045 | * |
| (r) Building a research department in your organization | 35.11 | 33.80 | 39.13 | 0.4222 | |
| (s) Other | 8.04 | 6.15 | 13.63 | 0.2700 |
*Statistically significant at α = 0.05.
Both health centers that currently engage in research and health centers that currently do not engage in research had top T/TA interests that addressed their top five barriers, including finding and capitalizing on funding opportunities and grant and proposal writing. Also coinciding with their top barriers, health centers that do not do research ranked recruitment and follow‐up with participants and finding and developing community‐academic partnerships as two of their top T/TA interests whereas health centers that do research ranked dissemination of research findings as top five T/TA interests. Interestingly, both groups listed using research to inform programs and services as a top T/TA interest. This suggests health centers’ desire to integrate research into their routine clinical care operations to utilize the benefits of research while reducing its burdens. Both groups also considered using research to inform public policy as a top topic of interest for T/TA (ranked third for health centers that do research, ranked seventh for health centers that do not do research). This notable finding suggests that health centers want to tackle larger structural issues that are influenced by policies, such as funding and staffing, to make it more feasible for health centers to better reach underserved populations.
Coinciding with reported barriers, health centers that do not currently engage in research were significantly more interested in receiving training to improve their internal capacities, such as developing research aims and research questions (68% vs. 50%; p = 0.007), study design and research methods (61% vs. 42%; p = 0.0047), data collection (70% vs. 50%; p = 0.0027), and research ethics (67% vs. 50%; p = 0.0130). Similarly, health centers with no prior research experience reported higher interest in conducting statistical analyses (70% vs. 47%; p = 0.0009), developing a database (68% vs. 41%; p = 0.0001), data entry and coding (64% vs. 39%; p = 0.0003), and finding and using information from medical articles (67% vs. 43%; p = 0.0005). This suggests that health centers that have conducted or participated in research are developing skills and internal capacity, and/or have external partnerships in place to fulfill these capacity needs.
Mirroring the findings in reported barriers to research engagement, a high level of interest in developing partnerships and fostering favorable research relationships was reported by responding health centers. Health centers not doing research are significantly more interested in finding, developing, and sustaining partnerships (74% vs. 51%; p = 0.0008) and over half are interested in learning how to obtain buy‐in from staff and governing boards (52%) compared to only one‐third of health centers that currently do research (p = 0.0045). This high level of interest in building sustainable internal capacity and external partnerships for research engagement points to a high level of interest in community‐academic partnerships on the part of health centers. Although health centers reported high interest in learning more about how research can inform their program, they were not as interested in learning how to build a research department in their organization. In fact, this was the topic that both groups were least interested in for receiving T/TA (39% for health centers that do not do research, and 34% for health centers that do research; p = 0.4222). This may indicate that health centers are concerned about the staff time and costs involved in this, or that it is not considered an immediate need.
Preferred modes of training
In order to identify the best mechanisms for T/TA, we asked health centers to report their preferred modes for accessing these resources (Table 3). Free webinars were, by far, the most preferred choice for training modes with 89% of research engaged health centers and 76% of nonresearch engaged health centers indicating this preference (p = 0.005). This was the only mode of training for which there was a statistical significant difference across the two groups. Health centers engaged in research or not engaged in research had statistically comparable responses to other training modes, including online tools, research seminars, multiday seminars, and webinars that require purchase.
Table 3.
Preferred modes of training and technical assistance
| All health centers (N = 291) % | Health centers doing research (N = 215) % | Health centers not doing research (N = 76) % | p‐Value | |
|---|---|---|---|---|
| (a) Free webinars | 85.9 | 89.3 | 76.3 | 0.0050* |
| (b) Cost < webinars | 29.2 | 29.8 | 27.6 | 0.7260 |
| (c) Seminars | 58.8 | 58.1 | 60.5 | 0.7175 |
| (d) Multiday training | 19.2 | 17.7 | 23.7 | 0.2548 |
| (e) Online tools | 71.8 | 73.0 | 68.4 | 0.4451 |
| (f) Other | 2.7 | 2.8 | 2.6 | 0.9421 |
Discussion
The first national survey of health center research experience finds that more than half of health centers already participate in research, the majority of whom are interested in expanding their research activities. Meanwhile, many health centers that are not currently engaged in research are interested in participating. Health centers seem to view research as a way to build on their mission for improving access to care and reducing health disparities. Most research is conducted in partnership with external researchers, usually in partnership with academics and other health centers. These nuances around health center engagement in research is consistent with the limited evidence on health center research engagement in the literature that state the importance of health centers’ relationships with research partners.2, 3, 5, 6, 7, 9, 10
Despite this, health centers face many barriers that limit their ability to actively pursue community research priorities and build the body of evidence for primary care generally and safety‐net settings specifically. These barriers also differ by whether health centers have had previous experience conducting or participating in research activities. In most cases, health centers without prior research experience more frequently reported experiencing barriers in nearly all categories, when compared with health centers that had previously engaged in research.
In addition, health centers tend to report T/TA needs that correspond with their perceived barriers. Not surprisingly, health centers with no prior research experience report greater training needs addressing structural, organizational, and conceptual challenges to engaging in research than those health centers that are already engaged in research. Many of the needs identified by health centers in this survey are being addressed in a free, online research training catalog for health centers (www.CDNetwork.org/NACHC), developed by the Clinical Directors Network (CDN), the National Association of Community Health Centers (NACHC), CTSI‐CN, George Washington University, and the Association of Asian Pacific Community Health Organizations (AAPCHO). Further information on health centers’ preferences for T/TA will provide research and health center leaders with valuable information for developing tools, measures, and resources for successful engagement of health centers in future research efforts.
Conclusion
Regardless of health centers’ level of research engagement, they tend to experience shared barriers and challenges to engaging in health‐related research, although these barriers are surely experienced at differing degrees. Although most health centers partner with academic institutions to engage in research, the findings suggests a need to better develop bidirectional partnerships that are more equitable and collaborative. Indeed, our findings suggest that not only are health centers generally interested in enhancing and expanding their role in the research process, but are also interested in additional T/TA resources to better meet the healthcare needs of their community.
Given that health centers not engaged in research reported similar preferences in the mechanisms for learning more about research and how to address their perceived research barriers also represent a significant opportunity for local academic institutions to more effectively translate research relevant to population health. While funding and financing remain common barriers on both sides, partnerships that are characterized as truly bidirectional which involve shared resources and expertise are most likely to have a sustainable research infrastructure.
Funding
This project was supported by the Clinical and Translational Science Institute at Children's National Medical Center and The George Washington University (through the NIH CTSA program #UL1TR000075) with additional support from the RCHN Community Health Foundation. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Acknowledgments
The authors thank individuals at the CHARN, SCPHCA, and USC for their partnership in designing and fielding the survey instrument. Special thanks goes to Vicki Young, Ph.D., and Dayna Campbell, M.S. (SCPHCA); Heather M. Brandt, Ph.D., and Tisha Felder, Ph.D. (USC); and Rosy Chang Weir, Ph.D., Shelly Enos, M.P.H., Suzanne Gillespie, M.A., M.S., Stefan Massimino, M.S., Reesa Laws, Christine Nelson, Ph.D., R.N., Mary Oneha, Ph.D., Thu Quach, Ph.D., Shao‐Chee Sim, Ph.D., Robbie Singal, M.P.H., Hui Song, M.P.H., M.S., and Fikirte Wagaw, M.P.H. (CHARN). The authors would also like to thank the following individuals for their input on designing the survey instrument and/or providing feedback on the analysis: Franco Basanti, Pharm.D. (Urban Health Plan, Inc.), Mickey Eder, Ph.D. (Access Community Health Network), William Hobston, M.S. (WATTS Healthcare Corporation), Paloma Hernandez, M.P.H., M.S. (Urban Health Plan, Inc.), Vanesscia John, M.S.W., M.P.A. (California Primary Care Association), Patrick McShane (Beaufort‐Jasper Hampton Comprehensive Health Services), Chaya Merrill, M.P.H., Dr.P.H. (Children's National Medical Center), Mark Minier, M.D. (Unity Health Care, Inc.), Greg Nycz (Family Health Center of Marshfield, Inc.), Luis Padilla, M.D. (Unity Health Care, Inc.), Perry Payne, M.D., M.J., M.P.P. (The George Washington University), Sara Rosenbaum, J.D. (The George Washington University), Sarena Seifer, M.D. (Community‐Campus Partnership for Health), Jonathan Tobin, Ph.D. (Clinical Directors Network, Inc.), Rosy Chang Weir, Ph.D. (AAPCHO), Vicki Young, Ph.D. (South Carolina Primary Health Care Association).
Footnotes
Health centers that indicated barriers as “moderate” or “huge” for each question were considered to have experienced barriers in each respective category.
References
- 1. National Association of Community Health Centers . Community Health Centers: A Unique Approach to Primary Care Fact Sheet, August 2012. Available at: http://www.nachc.com/client/documents/UniqueModel.pdf. Accessed December 14, 2012.
- 2. Weiss SM, Tobin JN, Antoni M, Ironson G, Ishii M, Vaughn A, Cassells A, Jones D, Schneiderman N, Brondolo E, et al.; SMART/EST Women's Project Team . Enhancing the health of women living with HIV: the SMART/EST women's project. Int J Womens Health. Feb 15 2011; 3: 63–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Riedy CA, Ly KA, Ybarra V, Milgrom P. An FQHC research network in oral health: enhancing the workforce and reducing disparities. Public Health Rep. Sep–Oct 2007; 122(5): 592–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daniels EC, Bacon J, Denisio S, Fry YW, Murray V, Quarshie A, Rust G. Translation squared: improving asthma care for high‐disparity populations through a safety net practice‐based research network. J Asthma. Jul–Aug 2005; 42(6): 499–505. [DOI] [PubMed] [Google Scholar]
- 5. Devoe JE, Gold R Spofford M, Chauvie S, Muench J, Turner A, Likumahuwa S, Nelson C. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice‐based Research Network (SNW‐PBRN). J Am Board Fam Med. Sep–Oct 2011; 24(5): 597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Davis RM, Hitch AD, Nichols M, Rizvi A, Salaam M, Mayer‐Davis EJ. A collaborative approach to the recruitment and retention of minority patients with diabetes in rural community health centers. Contemp Clin Trials. Jan 2009; 30(1): 63–70. [DOI] [PubMed] [Google Scholar]
- 7. Khankari K, Eder M, Osborn CY, Makoul G, Clayman M, Skripkauskas S, Diamond‐Shapiro L, Makundan D, Wolf MS. Improving colorectal cancer screening among the medically underserved: a pilot study within a federally qualified health center. J Gen Intern Med. Oct 2007; 22(10):1410–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shin P, Sharac J, Beeson T, Proser M, Jester M. Identifying key patient demographics and organizational factors that contribute to health center participation in research. J Ambul Care Manage. In Press. [DOI] [PubMed] [Google Scholar]
- 9. Lemon SC, Zapka JG, Estabrook B, Benjamin E. Challenges to research in urban community health centers. Am J Pub Health 2006; 96(3): 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kwon S, Rideout C, Tseng W, Islam N, Cook WK, Ro M, Trinh‐Shevrin C. Developing the community empowered research training program: building research capacity for community‐initiated and community‐driven research. Prog Community Health Partnersh. 2012; 6(1): 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]


