Abstract
Background
Informed consent is a pillar of ethical medicine which requires patients to fully comprehend relevant issues including the risks, benefits, and alternatives of an intervention. Given the average reading skill of US adults is at the 8th grade level, the American Medical Association (AMA) and the National Institutes of Health (NIH) recommend patient information materials should not exceed a 6th grade reading level. We hypothesized that text provided in invasive procedure consent forms would exceed recommended readability guidelines for medical information.
Materials and methods
To test this hypothesis, we gathered procedure consent forms from all surgical inpatient hospitals in the state of Rhode Island. For each consent form, readability analysis was measured with the following measures: Flesch Reading Ease Formula, Flesch–Kincaid Grade Level, Fog Scale, SMOG Index, Coleman–Liau Index, Automated Readability Index, and Linsear Write Formula. These readability scores were used to calculate a composite Text Readability Consensus Grade Level.
Results
Invasive procedure consent forms were found to be written at an average of 15th grade level (i.e., third year of college), which is significantly higher than the average US adult reading level of 8th grade (p < 0.0001) and the AMA/NIH recommended readability guidelines for patient materials of 6th grade (p < 0.0001).
Conclusion
Invasive procedure consent forms have readability levels which makes comprehension difficult or impossible for many patients. Efforts to improve the readability of procedural consent forms should improve patient understanding regarding their healthcare decisions.
Keywords: consent form, comprehension, readability, informed consent, health literacy
Introduction
Informed consent is a pillar of ethical medical practice. Informed consent is achieved when patients fully understand the procedure they are considering. Ideally, informed consent is achieved through patient–physician conversation regarding the risks and benefits of all available interventions, resulting in voluntary permission to proceed with the procedure. Legally, intervention without informed consent may be grounds for negligence, malpractice, or battery and assault.1 Ethically, the patient's understanding of the proposed procedure is paramount for them to make an informed decision.
The consent form was developed to document the informed consent conversation and to ensure that all necessary information is conveyed. The process of informed consent is particularly relevant as surgeons and other procedure‐based physicians are burdened with increasing malpractice insurance costs and liability threats.2 Improved understanding of the informed consent process is critical.
The level of patient comprehension during the informed consent process is frequently overestimated.3 In a prospective evaluation of patient comprehension of informed consent, Crepeau et al. found that surgical patient comprehension and recall immediately following a thorough discussion of the consent form was unexpectedly low.4 Previous investigations have examined the readability of consent forms use in research protocols as a contributing factor to poor comprehension.5, 6, 7 These research protocol consent forms are substantially different from consent forms used in daily clinical practice, and to our knowledge, no study has evaluated the readability of invasive procedure consent forms used in daily practice.
Because the average US adult reads at an 8th grade level,8, 9 the National Institutes of Health (NIH) and the American Medical Association (AMA) recommend the readability of patient materials be ≤6th grade reading level.20, 21, 22, 23, 24 Patient materials have been repeatedly shown to be too complex.9, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24
In this study, we evaluate the readability of invasive procedure consent forms used in daily clinical practice. We hypothesized that text provided in consent forms would exceed the AMA/NIH‐recommended readability guidelines for medical information (i.e., reading level >6th grade).
Methods and Materials
Invasive procedure consent forms from each hospital type (private, public, government, community, and academic) were sampled by gathering consent forms from all hospitals in the state of Rhode Island that perform procedures. For each consent form, readability was analyzed using eight well‐validated tests.
Consent forms
There are 17 hospitals in the state of Rhode Island, 14 of which perform invasive procedures. Due to several hospitals from the same hospital system sharing consent forms, there are 11 unique invasive procedure consent forms used statewide. All 11 (100%) of these consent forms were obtained between May and August, 2014.
Text from the consent forms was copied in plain text format into individual Microsoft Office Word 2010 documents (Microsoft Corporation, Redmond, WA, USA). As recommended by Flesch and others, all decimals, numbers, paragraph breaks, bullets, abbreviations, semicolons, colons, and dashes within a sentence were removed in order to avoid underestimating the readability level.25, 26
Readability analysis
Readability analysis was performed using well‐validated scales that have been commonly used to evaluate healthcare‐related materials.15, 16, 17, 18, 19, 20, 22, 23, 24, 27, 28, 29, 30, 31, 32, 33, 34, 35 Readability scores were measured using the following tests: Flesch Reading Ease Formula, Flesch–Kincaid Grade Level, Fog Scale, SMOG Index, Coleman–Liau Index, Automated Readability Index, Linsear Write Formula, including the composite Text Readability Consensus Calculator (Table 1). The readability software utilized is publically available at http://www.readabilityformulas.com/freereadability‐formula‐tests.php.
Table 1.
| Assessment scale | Formula | Output |
|---|---|---|
| Flesch Reading Ease Formula | = 206.835 – (1.015 × ASL) – (84.6 × ASW) |
|
| Flesch–Kincaid Grade Level | = (0.39 × ASL) + (11.8 × ASW) – 15.59 |
|
| Fog Scale | = 0.4 (ASL + PHW) |
|
| SMOG Index | = 1.043 × √ (C × (30/S)) + 3.1291 | Average student of the grade can read the text |
| Coleman–Liau Index | = 0.0588L – 0.00296S – 15.8 | Average student of the grade can read the text |
| Automated Readability Index | = 4.71 (characters/words) + 0.5 (words/sentences) – 21.43 | Average student of the grade can read the text |
| Linsear Write Formula |
|
Average student of the grade can read the text |
ASL = average sentence length (i.e., the number of words divided by the number of sentences [S]); ASW = average number of syllables per word (i.e., the number of syllables divided by the number of words); PHW = percentage of hard words (i.e., the number of 3+ syllable words [C] divided by the number or words in the sample passage); R = the number of words ≤2 syllables; L = the average number of letters per 100 words; average student of the grade can read the text = US school grade level (e.g., 7.4 = 7th grade).
Each of the readability measures is based on the English language and US grade levels, and uses different criteria to compute the readability (e.g., length of sentence, number of characters, number of syllables, number of words, or combinations thereof). The Readability Consensus formula combines the output of these measures and computes a composite grade level score across all seven methods.
Statistical analysis
Unpaired t‐tests were utilized to compare the mean Text Readability Consensus Grade Level of consent forms with the readability level recommended by the AMA and NIH (6th grade), as well as with the average American adult reading level (8th grade). GraphPad Software (GraphPad Software, Inc., La Jolla, CA, USA) was used for statistical analysis. The p < 0.05 was used to establish statistical significance.
Results
All 11 consent forms were obtained and assessed (100%). The average grade level readability of invasive procedure consents forms was 15.0 (SD = 3.6) (Table 2). None (0/11) of the consent forms had a readability score below the 6th grade level. The readability of the consent forms exceeded this level by an average of 9.0 grade levels (95% CI, 6.7–11.3; p < 0.0001). None (0/11) of the consent forms had a readability score ≤8th grade level. The readability of the articles exceeded this level by an average of 7.0 grade levels (95% CI, 4.7–9.3; p < 0.0001) (Figure 1). Hospital names and affiliations have been de‐identified for the sake of privacy.
Table 2.
Readability levels calculated by Flesch Reading Ease Formula (FRE), Flesch–Kincaid Grade Level (FKGL), Fog Scale (Fog), SMOG Index (SMOG), Coleman–Liau Index (CLI), Automated Readability Index (ARI), Linsear Write Formula (LW), and Text Readability Consensus Grade Level (Consensus)
| Hospitals with unique consent forms | Health system | FRE | FKGL | Fog | SMOG | CLI | ARI | LW | Consensus |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Private hospital system 1 | 41.1 | 11.8 | 14.9 | 11.4 | 13 | 11.8 | 12.5 | 12 |
| 2 | Private hospital system 2 | 27.8 | 15.2 | 18 | 13.9 | 13 | 14.7 | 17.5 | 15 |
| 3 | Private hospital system 2 | 46.5 | 10.4 | 14.5 | 10.6 | 13 | 10.2 | 10.6 | 11 |
| 4 | Independent | 32.1 | 14.1 | 18 | 13.1 | 14 | 14.6 | 15.8 | 14 |
| 5 | Independent | 30.1 | 15.5 | 18.7 | 13.7 | 14 | 16.9 | 18.6 | 16 |
| 6 | Independent | 2.7 | 22.6 | 20.7 | 18.8 | 15 | 24.7 | 30.4 | 22 |
| 7 | Independent | 28.3 | 15.1 | 18.4 | 13.9 | 14 | 15.6 | 17.5 | 15 |
| 8 | Independent | 14 | 20.7 | 22.6 | 18 | 14 | 22.7 | 28.8 | 21 |
| 9 | State owned | 30.5 | 14.2 | 17.1 | 13.3 | 15 | 15.4 | 15.9 | 15 |
| 10 | Federally owned | 35 | 12.9 | 14.8 | 12 | 14 | 12.9 | 13.4 | 13 |
| 11 | Federally owned | 41.3 | 11.4 | 14.5 | 11 | 13 | 11 | 11.4 | 11 |
| Average ± SD | – | 29.9 ± 12.5 | 14.9 ± 3.8 | 17.5 ± 2.7 | 13.6 ± 2.6 | 13.8 ± 0.8 | 15.5 ± 4.6 | 17.5 ± 6.5 | 15.0 ± 3.6 |
Figure 1.
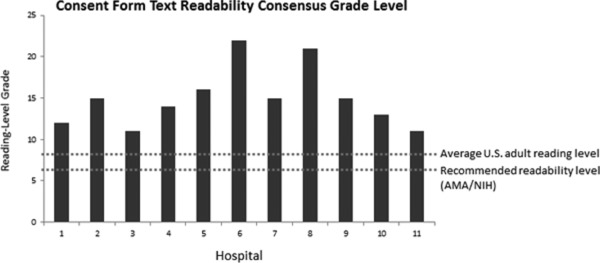
Consent form text readability consensus grade level.
Discussion
This investigation revealed that the readability level of invasive procedure consent forms exceeds the average patient's comprehension level by seven grade levels. The average consent form was significantly more difficult to read than both the NIH/AMA readability recommendations and the average reading level of adults in the United States. In 2003, Paasche‐Orlow et al. found that the readability level of research‐related consent forms from across the country to be 10.6.5 Our findings suggest today's clinically‐used invasive procedure consent forms may be of even greater complexity.
Patient understanding of health information is at the core of informed consent validity. Consent forms may thus fail to effectively inform a substantial portion of the patient population because they cannot properly understand the content. Additionally, the sizeable patient population that does not read English fluently is likely to comprehend even less. Without comprehension, completely informed consent cannot be realized. One might argue that a comprehensive verbal discussion of the proposed procedure is sufficient for informed consent which, in fact, may be true. However, the record should reflect what actually occurs during patient care including informed consent. If a patient is asked to sign a document that they cannot comprehend due to their reading skill level, have they actually completed the process of true informed consent? Inadequacy of informed consent has the potential for significant legal and ethical consequences.
Furthermore, poor understanding may negatively impact health literacy, which is an important factor in health outcomes and costs. Health literacy is the “capacity to obtain, interpret, and understand basic health information and services and the competence to use such information and services to enhance health” —is therefore central to informed consent.36 Nearly 50% of adults “experience considerable difficulty in performing tasks that required them to integrate or synthesize information from complex or lengthy texts.”37 Although the average US adult reads at an 8th grade level,8, 9 approximately one‐fifth of these adults are unable to comprehend 4th grade‐level text.9 Most importantly, health literacy predicts health‐related quality of life,38, 39, 40 worse overall health,41, 42, 43, 44, 45, 46 along with complication and hospitalization rates.42, 47, 48 Lower health literacy is associated with substantial additional annual healthcare costs.49, 50, 51, 52, 53, 54, 55, 56, 57 This study highlights an important gap between relevant and understandable healthcare information and patient comprehension.
This study has several possible limitations. We assumed those reading the consent forms possess comparable reading skills to the general population, which may or may not be the case. Additionally, nonhospital clinical settings’ consent forms were not sampled. Furthermore, the 11 consent forms analyzed may not represent similar content to forms from the entire country, although they do represent private, public, and government hospitals including community health centers and large trauma centers. Many patients treated at these hospitals speak English as a second language, and consent forms are available in many additional languages as well. The present study does not address this issue, which in some regions may be significant. It is likely that the English reading level in areas with large immigrant populations may in fact be far lower than the national average. Foreign‐language consent forms may represent a level of sophistication exceeding the population they target. This was not addressed in the current study. Finally, the consent form is only one aspect of informed consent, and obtaining appropriate informed consent is a process requiring verbal communication rather than just the completion of a form, and no assessment of verbal consent processes was completed.
Screening and testing of the readability of invasive procedure consent forms is an important initiative to ensure health literacy. Certain consent form revision strategies may be of particular benefit. For example, shorter sentences, simpler terms, and pictures can improve readability.14, 15 Innovative approaches, such as video informed consent, aimed at improving patient comprehension show promise.58 Enhancing patient understanding and health literacy through modifying readability of consent forms has the potential to improve patient outcomes.
Conflict of Interest
None of the authors have directly pertinent conflicts of interest.
References
- 1. The Metaphysics Resaerch Lab . In The Stanford Encyclopedia of Philosophy. “Informed Consent,” 2011. http://plato.stanford.edu/entries/informed‐consent (Accessed July 15, 2015).
- 2. Mello MM, Studdert DM, DesRoches CM, Peugh J, Zapert K, Brennan TA, Sage WM. Effects of a malpractice crisis on specialist supply and patient access to care. Ann Surg. 2005; 242(5): 621–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sugarman J, McCrory DC, Powell D, Krasny A, Adams B, Ball E, Cassell C. Empirical research on informed consent: an annotated bibliography. Hastings Cent Rep. 1999; 29(1): S1–S42. [PubMed] [Google Scholar]
- 4. Crepeau AE, McKinney BI, Fox‐Ryvicker M, Castelli J, Penna J, Wang ED. Prospective evaluation of patient comprehension of informed consent. J Bone Joint Surg Am. 2011; 93(19): e114 (1–7). [DOI] [PubMed] [Google Scholar]
- 5. Paasche‐Orlow MK, Taylor HA, Brancati FL. Readability standards for informed‐consent forms as compared with actual readability. N Engl J Med. 2003; 348(8): 721–726. [DOI] [PubMed] [Google Scholar]
- 6. Williams BF, French JK, White HD; HERO‐2 consent substudy investigators. Informed consent during the clinical emergency of acute myocardial infarction (HERO‐2 consent substudy): a prospective observational study. Lancet. 2003; 361: 918–922. [DOI] [PubMed] [Google Scholar]
- 7. Jackson RH, Davis TC, Bairnsfather LE, George RB, Crouch MA, Gault H. Patient reading ability: an overlooked problem in health care. Southern Med J. 1991; 84: 1172–1175. [DOI] [PubMed] [Google Scholar]
- 8. Doak CC, Doak LG, Friedell GH, Meade CD. Improving comprehension for cancer patients with low literacy skills: strategies for clinicians. CA: Cancer J Clin. 1998; 48(3): 151–162. [DOI] [PubMed] [Google Scholar]
- 9. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. 2nd edn Philadelphia, PA: JB Lippincott; 1996. [Google Scholar]
- 10. Weiss BD. Health Literacy: A Manual for Clinicians. Chicago, IL: American Medical Association, American Medical Foundation; 2003. [Google Scholar]
- 11. U.S. National Library of Medicine, U.S. Department of Health and Human Services, National Institutes of Health . How to write easy‐to‐read health materials. https://www.nlm.nih.gov?medlineplus/etr.html (Accessed July 8, 2015).
- 12. Weiss BD, Coyne C. Communicating with patients who cannot read. N Engl J Med. 1997; 337(4): 272–274. [DOI] [PubMed] [Google Scholar]
- 13. Doak LG, Doak CC, Meade CD. Strategies to improve cancer education materials. Oncol Nurs Forum. 1996; 23(8): 1305–1312. [PubMed] [Google Scholar]
- 14. Cotugna N, Vickery CE, Carpenter‐Haefele KM. Evaluation of literacy level of patient education pages in health‐related journals. J Commun Health. 2005; 30(3): 213–219. [DOI] [PubMed] [Google Scholar]
- 15. Albright J, de Guzman C, Acebo P, Paiva D, Faulkner M, Swanson J. Readability of patient education materials: implications for clinical practice. Appl Nurs Res. 1996; 9(3): 139–143. [DOI] [PubMed] [Google Scholar]
- 16. Cooley ME, Moriarty H, Berger MS, Selm‐Orr D, Coyle B, Short T. Patient literacy and the readability of written cancer educational materials. Oncol Nurs Forum. 1995; 22(9): 1345–1351. [PubMed] [Google Scholar]
- 17. Badarudeen S, Sabharwal S. Readability of patient education materials from the American Academy of Orthopaedic Surgeons and Pediatric Orthopaedic Society of North America web sites. J Bone Joint Surg Am. 2008; 90(1): 199–204. [DOI] [PubMed] [Google Scholar]
- 18. Sabharwal S, Badarudeen S, Unes Kunju S. Readability of online patient education materials from the AAOS web site. Clin Orthop Relat Res. 2008; 466(5): 1245–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang SW, Capo JT, Orillaza N. Readability and comprehensibility of patient education material in hand‐related web sites. J Hand Surg Am. 2009; 34(7): 1308–1315. [DOI] [PubMed] [Google Scholar]
- 20. Vives M, Young L, Sabharwal S. Readability of spine‐related patient education materials from subspecialty organization and spine practitioner websites. Spine (Phila Pa 1976). 2009; 34(25): 2826–2831. [DOI] [PubMed] [Google Scholar]
- 21. Murero M, D‧Ancona G, Karamanoukian H. Use of the Internet by patients before and after cardiac surgery: telephone survey. J Med Internet Res. 2001; 3(3): E27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Eltorai AE, Sharma P, Wang J, Daniels AH. Most American academy of orthopaedic surgeons‧ online patient education material exceeds average patient reading level. Clin Orthop Relat Res. 2015; 473(4): 1181–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Eltorai AE, Han A, Truntzer J, Daniels AH. Readability of patient education materials on the American Orthopaedic Society for Sports Medicine website. Phys Sports Med. 2014; 42(4): 125–130. [DOI] [PubMed] [Google Scholar]
- 24. Eltorai AE, Ghanian S, Adams CA Jr, Born CT, Daniels AH. Readability of patient education materials on the American association for surgery of trauma website. Arch Trauma Res. 2014; 3(2): e18161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Flesch RF. How to Write Plain English: A Book for Lawyers, Consumers. 1st edn New York, NY: Barnes and Noble; 1981. [Google Scholar]
- 26. Friedman DB, Hoffman‐Goetz L. A systematic review of readability and comprehension instruments used for print and web‐based cancer information. Health Educ Behav. 2006; 33(3): 352–373. [DOI] [PubMed] [Google Scholar]
- 27. Bluman EM, Foley RP, Chiodo CP. Readability of the patient education section of the AOFAS website. Foot Ankle Int. 2009; 30(4): 287–291. [DOI] [PubMed] [Google Scholar]
- 28. Yi PH, Ganta A, Hussein KI, Frank RM, Jawa A. Readability of arthroscopy‐related patient education materials from the American Academy of Orthopaedic Surgeons and Arthroscopy Association of North America Web sites. Arthroscopy. 2013; 29(6): 1108–1112. [DOI] [PubMed] [Google Scholar]
- 29. Polishchuk DL, Hashem J, Sabharwal S. Readability of online patient education materials on adult reconstruction Web sites. J Arthroplast. 2012; 27(5): 716–719. [DOI] [PubMed] [Google Scholar]
- 30. Lam CG, Roter DL, Cohen, KJ . Survey of quality, readability, and social reach of websites on osteosarcoma in adolescents. Patient Educ Counsel. 2013; 90(1): 82–87. [DOI] [PubMed] [Google Scholar]
- 31. Langbecker D, Janda M. Quality and readability of information materials for people with brain tumours and their families. J Cancer Educ. 2012; 27(4): 738–743. [DOI] [PubMed] [Google Scholar]
- 32. Ellimoottil C, Polcari A, Kadlec A, Gupta G. Readability of websites containing information about prostate cancer treatment options. J Urol. 2012; 188(6): 2171–2175. [DOI] [PubMed] [Google Scholar]
- 33. Stossel LM, Segar N, Gliatto P, Fallar R, KaraniR. Readability of patient education materials available at the point of care. J Gen Inter Med. 2012; 27(9): 1165–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Charbonneau DH. Readability of menopause web sites: a cross‐sectional study. J Women Aging. 2012; 24(4): 280–291. [DOI] [PubMed] [Google Scholar]
- 35. Colaco M, Svider PF, Agarwal N, Eloy JA, Jackson IM. Readability assessment of online urology patient education materials. J Urol. 2013; 189(3): 1048–1052. [DOI] [PubMed] [Google Scholar]
- 36. United States Institute of Medicine . Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 37. Kirsch IS, Jenkins L, Kolstad A. Adult literacy in America: a first look at the results of the National Adult Literacy Survey. National Center for Educational Statistics; 1993. [Google Scholar]
- 38. Wang C, Li H, Li L, Xu D, Kane RL, Meng Q. Health literacy and ethnic disparities in health‐related quality of life among rural women: results from a Chinese poor minority area. Health Qual Life Outcom. 2013; 11(1): 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wallace LS, Rogers ES, Weiss BD. Relationship between health literacy and health‐related quality of life among Tennesseans. Tenn Med. 2008; 101(5): 35–39. [PubMed] [Google Scholar]
- 40. Song L, Mishel M, Bensen JT, Chen RC, Knafl GJ, Blackard B, Farnan L, Fontham E, Su LJ, Brennan CS, et al. How does health literacy affect quality of life among men with newly diagnosed clinically localized prostate cancer? Findings from the North Carolina‐Louisiana Prostate Cancer Project (PCaP). Cancer. 2012; 118(15): 3842–3851. [DOI] [PubMed] [Google Scholar]
- 41. Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self‐reported health and use of health services. Am J Public Health. 1997; 87(6): 1027–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002; 288(4): 475–482. [DOI] [PubMed] [Google Scholar]
- 43. Kalichman SC, Rompa D. Functional health literacy is associated with health status and health‐related knowledge in people living with HIV‐AIDS. J Acquir Immune Defic Syndr. 2000; 25(4): 337–344. [DOI] [PubMed] [Google Scholar]
- 44. Weiss BD, Hart G, McGee DL, D‧Estelle S. Health status of illiterate adults: relation between literacy and health status among persons with low literacy skills. J Am Board Fam Pract. 1992; 5(3): 257–264. [PubMed] [Google Scholar]
- 45. Bennett CL, Ferreira MR, Davis TC, Kaplan J, Weinberger M, Kuzel T, Seday MA, Sartor O. Relation between literacy, race, and stage of presentation among low‐income patients with prostate cancer. J Clin Oncol. 1998; 16(9): 3101–3104. [DOI] [PubMed] [Google Scholar]
- 46. Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, Newman AB, Rosano C, Rooks R, Rubin SM, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006; 21(8): 806–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Ren J, Peel J. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002; 92(8): 1278–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998; 13(12): 791–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Weiss BD, Palmer R. Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. J Am Board Fam Pract. 2004; 17(1): 44–47. [DOI] [PubMed] [Google Scholar]
- 50. Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med. 2005; 118(4): 371–377. [DOI] [PubMed] [Google Scholar]
- 51. Friedland RB. Understanding Health Literacy: New Estimates of the Costs of Inadequate Health Literacy. Washington, DC: National Academy on an Aging Society; 1998. [Google Scholar]
- 52. Vernon J. Low health literacy: An economic drain on the US healthcare system. Washington, DC: Presented at National Press Club; 10 October 2007. [Google Scholar]
- 53. Affairs Ad Hoc Committee on Health Literacy for the Council on Scientific. Health literacy: report of the Council on Scientific Affairs. JAMA. 1999; 281: 552–557. [PubMed] [Google Scholar]
- 54. Baker DW. Access to health care and preventable hospitalizations. JAMA. 1995; 274: 1759. [DOI] [PubMed] [Google Scholar]
- 55. Kickbusch I, Ratzan SC. Health literacy: making a difference in the USA. J Health Commun. 2001; 6: 87–88. [DOI] [PubMed] [Google Scholar]
- 56. Rudd RE, Moeykens BA, Colton TC. Health and literacy: a review of medical and public health literature In: Comings J, Garners B, Smith C, eds. Health and Literacy. New York: Jossey‐Bass; 1999. [Google Scholar]
- 57. Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self‐care. Chest. 1998; 114: 1008–1015. [DOI] [PubMed] [Google Scholar]
- 58. Rossi MJ, Guttmann D, MacLennan MJ, Lubowitz JH. Video informed consent improves knee arthroscopy patient comprehension. Arthroscopy. 2005; 21(6): 739–743. [DOI] [PubMed] [Google Scholar]
- 59. Ryan L, Logsdon MC, McGill S, Stikes R, Senior B, Helinger B, Small B, Davis DW. Evaluation of printed health education materials for use by low‐education families. J Nurs Scholarsh. 2014; 46(4): 218–228. [DOI] [PubMed] [Google Scholar]
- 60. Pringle MB, Natesh BG, Konieczny KM. Patient information leaflet on mastoid surgery risks: assessment of readability and patient understanding. J Laryngol Otol. 2013; 127(11): 1078–1083. [DOI] [PubMed] [Google Scholar]
- 61. http://www.readabilityformulas.com/free‐readability‐formula‐tests.php


