Abstract
The efficacy and safety of chidamide, a new subtype-selective histone deacetylase (HDAC) inhibitor, have been demonstrated in a pivotal phase II clinical trial, and chidamide has been approved by the China Food and Drug Administration (CFDA) as a treatment for relapsed or refractory peripheral T cell lymphoma (PTCL). This study sought to further evaluate the real-world utilization of chidamide in 383 relapsed or refractory PTCL patients from April 2015 to February 2016 in mainland China. For patients receiving chidamide monotherapy (n = 256), the overall response rate (ORR) and disease control rate (DCR) were 39.06 and 64.45%, respectively. The ORR and DCR were 51.18 and 74.02%, respectively, for patients receiving chidamide combined with chemotherapy (n = 127). For patients receiving chidamide monotherapy and chidamide combined with chemotherapy, the median progression-free survival (PFS) was 129 (95% CI 82 to 194) days for the monotherapy group and 152 (95% CI 93 to 201) days for the combined therapy group (P = 0.3266). Most adverse events (AEs) were of grade 1 to 2. AEs of grade 3 or higher that occurred in ≥5% of patients receiving chidamide monotherapy included thrombocytopenia (10.2%) and neutropenia (6.2%). For patients receiving chidamide combined with chemotherapy, grade 3 to 4 AEs that occurred in ≥5% of patients included thrombocytopenia (18.1%), neutropenia (12.6%), anemia (7.1%), and fatigue (5.5%). This large real-world study demonstrates that chidamide has a favorable efficacy and an acceptable safety profile for refractory and relapsed PTCL patients. Chidamide combined with chemotherapy may be a new treatment choice for refractory and relapsed PTCL patients but requires further investigation.
Electronic supplementary material
The online version of this article (doi:10.1186/s13045-017-0439-6) contains supplementary material, which is available to authorized users.
Keywords: Chidamide, Peripheral T cell lymphoma, Treatment, Chemotherapy
Letter to the editor
Peripheral T cell lymphomas (PTCLs) are a set of rare and highly heterogeneous tumors derived from mature T cells or natural killer cells and are typically characterized by poor prognosis and aggressive clinical behavior [1]. PTCL accounts for 23 to 26% of all non-Hodgkin’s lymphoma (NHL) in China, which is significantly higher than the rates in Western countries [2, 3]. A consensus has not been reached on standard treatments for PTCL patients, and most commonly used traditional chemotherapy regimens are associated with a poor response [1, 4]. Moreover, a majority of patients may experience disease relapse even if they receive high-dose chemotherapy and autologous stem cell transplantation (ASCT) [5, 6]
Since 2009, the US Food and Drug Administration (FDA) has approved four new drugs for the treatment of relapsed or refractory PTCL, including the histone deacetylase (HDAC) inhibitors romidepsin and belinostat, the dihydrofolate reductase inhibitor pralatrexate, and the CD30 antibody-drug conjugate brentuximab vedotin for CD30-positive anaplastic large cell lymphoma (ALCL) patients [7, 8].
Chidamide, an innovative new drug independently developed in China, is designed to selectively inhibit the activity of HDAC1, 2, 3, and 10 following oral administration and was approved in December 2014 by the China Food and Drug Administration (CFDA) for the treatment of relapsed or refractory PTCL [9].
The efficacy and safety of chidamide have been demonstrated in a pivotal phase II clinical trial [10], yet further evaluation of its real-world utility is urgently needed. Therefore, we conducted a real-world multicenter efficacy and safety monitoring study to further test the clinical practice value of chidamide in relapsed or refractory PTCL patients in mainland China.
We analyzed 383 patients from April 2015 to February 2016. The cutoff date was February 19, 2016. The methods are shown in Additional file 1. The baseline characteristics of all patients are presented in Additional file 2.
For patients receiving chidamide monotherapy (n = 256), the overall response rate (ORR) and disease control rate (DCR) were 39.06 and 64.45%, respectively. In previous phase II study, the AITL patients received chidamide have a higher ORR of 50%. Higher ORR and superior survival were also observed for AITL patients received romidepsin and belinostat. In this real world study, AITL patients also tend to have higher ORR and DCR of 49.23% and 75.38% which were comparable with previous results. It has been reported that epigenetic regulation plays an important role in AITL pathogenesis, which may be relevant to more clinical benefits by HDAC inhibitors to AITL. The ORR and DCR seem higher for ALK+ ALCL patients receiving chidamide of 66.67% and 83.33%, but only 13 ALK+ ALCL patients receiving chidamide were included in this study and ALK+ ALCL alone has a better prognosis than other subtypes. Given that HDAC inhibitors can impair DNA repair mechanisms, thereby inducing DNA damage, the effects of HDAC inhibitors may be synergistic with the effects of chemotherapy. Several studies have shown that HDAC inhibitors combined with chemotherapy constitute an efficient treatment for PTCL patients, yet the optimal combination regimen remains unknown. This study found that the ORR and DCR were 51.18 and 74.02%, respectively, for patients receiving chidamide combined with chemotherapy (n = 127). For patients with an International Prognostic Index (IPI) of 2–3, the ORR in the chidamide combined with chemotherapy group (n = 55) was 58% higher than that in the chidamide single-agent group (n = 141), with an ORR of 41% (P = 0.0031). Chidamide combined with chemotherapy also increased the ORR for patients with an IPI of 4–5 (n = 26) relative to the ORR of patients receiving chidamide alone (n = 40) with ORRs of 42 and 10%, respectively (P = 0.006). The results of a subgroup analysis showed that the ORRs for patients receiving chidamide combined with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP)-like regimens, platinum-containing regimens, and other regimens were 53.13, 45.83, and 55.32%, respectively, with DCRs of 81.25, 66.67, and 76.60%, respectively (Table 1).
Table 1.
Tumor response of different pathologic subtypes
| AITL | ALK unknown ALCL | ALK+ ALCL | ALK− ALCL | ENKL | PTCL others | PTCL-NOS | All | |
|---|---|---|---|---|---|---|---|---|
| Chidamide alone | ||||||||
| ORR n (%) | 32 (49.23) | 4 (44.44) | 4 (66.67) | 3 (37.50) | 5 (15.15) | 5 (55.56) | 47 (37.30) | 100 (39.06) |
| CR n (%) | 6 (9.23) | 1 (11.11) | 4 (66.67) | 2 (25.00) | 2 (6.06) | 1 (11.11) | 11 (8.73) | 27 (10.55) |
| PR n (%) | 26 (40.00) | 3 (33.33) | 0 (0.00) | 1 (12.50) | 3 (9.09) | 4 (44.44) | 36 (28.57) | 73 (28.52) |
| DCR n (%) | 49 (75.38) | 6 (66.67) | 5 (83.33) | 6 (75.00) | 14 (42.42) | 6 (66.67) | 79 (62.70) | 165 (64.45) |
| Chidamide combined with chemotherapy regimens | ||||||||
| ORR n (%) | 25 (71.43) | 1 (33.33) | 2 (100.00) | 1 (14.29) | 8 (40.00) | 3 (75.00) | 25 (44.64) | 65 (51. 18) |
| CR n (%) | 4 (11.43) | 0 (0.00) | 1 (50.00) | 0 (0.00) | 2 (10.00) | 1 (25.00) | 7 (12.50) | 15 (11.81) |
| PR n (%) | 21 (60.00) | 1 (33.33) | 1 (50.00) | 1 (14.29) | 6 (30.00) | 2 (50.00) | 18 (32.14) | 50 (39.37) |
| DCR n (%) | 31 (88.57) | 1 (33.33) | 2 (100.00) | 5 (71.43) | 10 (50.00) | 4 (100.00) | 41 (73.21) | 94 (74.02) |
| Combined with CHOP-like regimens | ||||||||
| ORR n (%) | 7 (77.78) | 1 (50.00) | 0 (0.00) | 0 (0.00) | 1 (33.33) | 2 (100.00) | 6 (40.00) | 17 (53.13) |
| CR n (%) | 2 (22.22) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (33.33) | 1 (50.00) | 0 (0.00) | 4 (12.50) |
| PR n (%) | 5 (55.56) | 1 (50.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (50.00) | 6 (40.00) | 13 (40.63) |
| DCR n (%) | 9 (100.00) | 1 (50.00) | 0 (0.00) | 1 (100.00) | 2 (66.67) | 2 (100.00) | 11 (73.33) | 26 (81.25) |
| Combined with platinum-containing regimens | ||||||||
| ORR n (%) | 9 (75.00) | 0 (0.00) | 1 (100.00) | 0 (0.00) | 3 (42.86) | 0 (0.00) | 9 (37.50) | 22 (45.83) |
| CR n (%) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 4 (16.67) | 4 (8.33) |
| PR n (%) | 9 (75.00) | 0 (0.00) | 1 (100.00) | 0 (0.00) | 3 (42.86) | 0 (0.00) | 5 (20.83) | 18 (37.50) |
| DCR n (%) | 11 (91.67) | 0 (0.00) | 1 (100.00) | 2 (66.67) | 3 (42.86) | 0 (0.00) | 15 (62.50) | 32 (66.67) |
| Combined with other regimens | ||||||||
| ORR n (%) | 9 (64.29) | 0 (0.00) | 1 (100.00) | 1 (33.33) | 4 (40.00) | 1 (50.00) | 10 (58.82) | 26 (55.32) |
| CR n (%) | 2 (14.29) | 0 (0.00) | 1 (100.00) | 0 (0.00) | 1 (10.00) | 0 (0.00) | 3 (17.65) | 7 (14.89) |
| PR n (%) | 7 (50.00) | 0 (0.00) | 0 (0.00) | 1 (33.33) | 3 (30.00) | 1 (50.00) | 7 (41.18) | 19 (40.43) |
| DCR n (%) | 11 (78.57) | 0 (0.00) | 1 (100.00) | 2 (66.67) | 5 (50.00) | 2 (100.00) | 15 (88.24) | 36 (76.60) |
PTCL-NOS peripheral T cell lymphoma-not otherwise specified, AITL angioimmunoblastic T cell lymphoma, ENKL extranodal natural killer/T cell lymphoma, ALCL anaplastic large cell lymphoma, ORR overall response rate, DCR disease control rate
For patients receiving chidamide monotherapy and chidamide combined with chemotherapy, the median progression-free survival (PFS) was 129 (95% CI 82 to 194) days and 152 (95% CI 93 to 201) days, respectively (P = 0.3266) (Fig. 1) and the median duration of response (DOR) was 148 (95% CI 132 to 171) days and 169 (95% CI 154 to 192) days, respectively (P = 0.3215). In the chidamide monotherapy group, the PFS for AITL and peripheral T cell lymphoma-not otherwise specified (PTCL-NOS) patients were 144.5 days and 133 days, respectively. In the combination group, the PFS for AITL and PTCL-NOS patients were 176 days and 124 days, respectively. The results of a subgroup analysis showed that the median PFS for patients receiving chidamide combined with CHOP-like regimens, platinum-containing regimens, and other regimens was 172, 119, and 160 days, respectively. The median DOR for patients receiving chidamide combined with CHOP-like regimens, platinum-containing regimens, and other regimens was 180, 165, and 172 days, respectively.
Fig. 1.
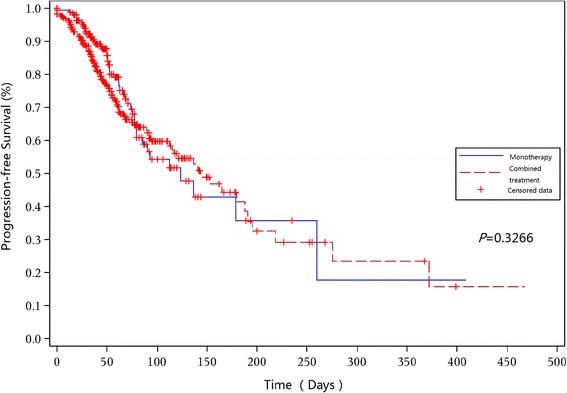
Progression-free survival for patients receiving chidamide monotherapy and patients receiving chidamide combined with chemotherapy
Drug-related adverse events (AEs) that occurred in ≥5% of patients receiving chidamide alone included thrombocytopenia (25.0%), neutropenia (19.1%), fatigue (18.4%), nausea/vomiting (14.1%), and anemia (11.3%). Drug-related AEs that occurred in ≥5% of patients receiving chidamide combined with chemotherapy included thrombocytopenia (28.4%), neutropenia (25.2%), fatigue (24.4%), anemia (17.3%), nausea/vomiting (12.7%), increased alanine aminotransferase (ALT) (9.5%), and increased aspartate aminotransferase (AST) (6.3%). Most AEs were of grade 1 to 2. AEs of grade 3 or higher that occurred in ≥5% of patients receiving chidamide alone included thrombocytopenia (10.2%) and neutropenia (6.2%). For patients receiving chidamide combined with chemotherapy, grade 3 to 4 AEs that occurred in ≥5% of patients included thrombocytopenia (18.1%), neutropenia (12.6%), anemia (7.1%), and fatigue (5.5%) (Additional file 3).
In summary, this real-world study conducted with 383 patients demonstrates that chidamide has a favorable efficacy and an acceptable safety profile for refractory and relapsed PTCL patients, confirming the pivotal phase II study in a more representative real-world population. Moreover, this study indicated the potential benefit of chidamide when combined with chemotherapy, which had not been previously examined. Chidamide combined with chemotherapy may be a new treatment choice for PTCL, especially for PTCL patients with an IPI ≥2, although further investigation is warranted.
Acknowledgments
The authors thank the patients, medical staff, and physicians who participated in this study. The authors thank Jun Ma, Jun Zhu, Jianyong Li, Zhixiang Shen, and Wenqi Jiang for their contribution to this study. The authors also acknowledge Meta Clinical Technology Co., Ltd. for the data analysis.
Funding
This study was sponsored by Chipscreen Biosciences, Ltd., Shenzhen, China.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and additional files.
Authors’ contributions
YS contributed to the conception and design of this study. All authors contributed to the provision of the patients in this study, the collection of data, and the writing of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Chidamide was approved in December 2014 by the China Food and Drug Administration (CFDA) for the treatment of relapsed or refractory PTCL, and the treatment choice was made by oncologists in each center. All patients signed the chemotherapy informed consent before the treatment, and the anonymity of the patients has been maintained.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- AEs
Adverse events
- ALT
Alanine aminotransferase
- ASCT
Autologous stem cell transplantation
- AST
Aspartate aminotransferase
- CFDA
China Food and Drug Administration
- DCR
Disease control rate
- DOR
Duration of response
- FDA
Food and Drug Administration
- HDAC
Histone deacetylase
- IPI
International Prognostic Index
- NHL
Non-Hodgkin’s lymphoma
- ORR
Overall response rate
- PFS
Progression-free survival
- PTCL
Peripheral T cell lymphoma
Additional files
Methods (DOCX 16 kb)
Patients’ baseline characteristics (DOCX 16 kb)
Drug-related adverse events in ≥5% of patients (DOCX 21 kb)
References
- 1.Vose J, Armitage J, Weisenburger D. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26(25):4124–4130. doi: 10.1200/JCO.2008.16.4558. [DOI] [PubMed] [Google Scholar]
- 2.Yang QP, Zhang WY, Yu JB, Zhao S, Xu H, Wang WY, et al. Subtype distribution of lymphomas in Southwest China: analysis of 6,382 cases using WHO classification in a single institution. Diagn Pathol. 2011;6(1):77. doi: 10.1186/1746-1596-6-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun J, Yang Q, Lu Z, He M, Gao L, Zhu M, et al. Distribution of lymphoid neoplasms in China: analysis of 4,638 cases according to the World Health Organization classification. Am J Clin Pathol. 2012;138(3):429–434. doi: 10.1309/AJCP7YLTQPUSDQ5C. [DOI] [PubMed] [Google Scholar]
- 4.Jia B, Hu S, Yang J, Zhou S, Liu P, Qin Y, et al. Comparison of gemcitabin, cisplatin, and dexamethasone (GDP), CHOP, and CHOPE in the first-line treatment of peripheral T-cell lymphomas. Hematology. 2016;21(9):536–541. doi: 10.1080/10245332.2016.1152084. [DOI] [PubMed] [Google Scholar]
- 5.Jung KS, Cho SH, Kim SJ, Ko YH, Kang ES, Kim WS. L-asparaginase-based regimens followed by allogeneic hematopoietic stem cell transplantation improve outcomes in aggressive natural killer cell leukemia. J Hematol Oncol. 2016;9(1):1–4. doi: 10.1186/s13045-016-0271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gui L, Shi YK, He XH, Lei YH, Zhang HZ, Han XH, et al. High-dose therapy and autologous stem cell transplantation in peripheral T-cell lymphoma: treatment outcome and prognostic factor analysis. Int J Hematol. 2014;99(1):69–78. doi: 10.1007/s12185-013-1465-y. [DOI] [PubMed] [Google Scholar]
- 7.O’Connor OA, Pro B, Pinter-Brown L, Bartlett N, Popplewell L, Coiffier B, et al. Pralatrexate in patients with relapsed or refractory peripheral T-cell lymphoma: results from the pivotal PROPEL study. J Clin Oncol. 2011;29(9):1182–1189. doi: 10.1200/JCO.2010.29.9024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coiffier B, Pro B, Prince HM, Foss F, Sokol L, Greenwood M, et al. Results from a pivotal, open-label, phase II study of romidepsin in relapsed or refractory peripheral T-cell lymphoma after prior systemic therapy. J Clin Oncol. 2012;30(6):631–636. doi: 10.1200/JCO.2011.37.4223. [DOI] [PubMed] [Google Scholar]
- 9.Lu X, Ning Z, Li Z, Cao H, Wang X. Development of chidamide for peripheral T-cell lymphoma, the first orphan drug approved in China. Intractable Rare Dis Res. 2016;5(3):185–191. doi: 10.5582/irdr.2016.01024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi Y, Dong M, Hong X, Zhang W, Feng J, Zhu J, et al. Results from a multicenter, open-label, pivotal phase II study of chidamide in relapsed or refractory peripheral T-cell lymphoma. Ann Oncol. 2015;26(8):1766–1771. doi: 10.1093/annonc/mdv237. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and additional files.


