Abstract
Gastric cancer is a multifactorial disease and a leading cause of mortality and the risk factors for this include environmental factors and factors that influence host-pathogen interaction and complex interplay between these factors. Gastric adenocarcinomas are of two types, namely intestinal and diffuse type, and Helicobacter pylori (H. pylori) infection has been suspected of being causally linked to the initiation of chronic active gastritis, which leads to adenocarcinoma of the intestinal type. Even though most individuals with H. pylori infection do not show any clinical symptoms, long-term infection leads to inflammation of gastric epithelium and approximately 10% of infected patients develop peptic ulcers and 1–3% of patients develop gastric adenocarcinoma. Among the several mechanisms involved in tumorigenesis, CagA and peptidoglycan of H. pylori, which enter the infected gastric epithelial cells play an important role by triggering oncogenic pathways. Inflammation induced by H. pylori in gastric epithelium, which involves the cyclooxygenase-2/prostaglandin E2 pathway and IL-1β, is also an important factor that triggers chronic active gastritis and adenocarcinoma. H. pylori infection induced oxidative stress and dysregulated E-cadherin/β-catenin/p120 interactions and function also play a critical role in tumorigenesis. Environmental and dietary factors, in particular salt intake, are known to modify the pathogenesis induced by H. pylori. Gastric cancer induced by H. pylori appears to involve several mechanisms, making this mode of tumorigenesis a highly complicated process. Nevertheless, there are many events in this tumorigenesis that remain to be clarified and investigated.
Keywords: inflammation, gastric cancer, Helicobater pylori
1. Introduction
Gastric cancer is a leading cause of cancer-related mortality worldwide, with nearly 1 million new cases and approximately 750,000 mortalities annually (1). Gastric cancer is a multifactorial disease and the risk factors for this include environmental factors and factors that influence host-pathogen interaction and complex interplay between these factors. Gastric cancer occurrence is more predominant in developing countries in Eastern Europe, South America, and Asia, accounting for approximately two thirds of all cases globally, with China representing approximately 42% of all new cases (2). Development of gastric cancer likely originates with the onset of chronic active gastritis and follows with atrophic gastritis, intestinal metaplasia, and dysplasia, eventually leading to gastric cancer (3). Besides environmental, diet and genetic factors, gastric cancer is closely associated with Helicobacter pylori (H. pylori) infection (4) and related host gene polymorphisms (5). Gastric adenocarcinomas constitute 90–95% of gastric cancers and are of two types, intestinal and diffuse type. Although there is no known precursor lesion for the development of diffuse type of gastric cancers, H. pylori infection has been suspected of being causally linked to the initiation of chronic active gastritis, which leads to adenocarcinoma (6). Infection of H. pylori is one of the thoroughly studied risk factors of gastric cancer.
After its identification in 1984, H. pylori was classified as a type I carcinogen and epidemiological studies indicated that H. pylori is the most common etiological agent for cancers that are related to infection (7,8). H. pylori is a gram-negative bacterial pathogen and is colonized in gastric epithelium despite the harsh acidic environment, because of its ability to conduct urease-mediated breakdown of urea to ammonia to release ammonia and neutralize its surrounding environment (9). Even though most individuals with H. pylori infection do not exhibit any clinical symptoms, long-term infection potentially leads to inflammation of gastric epithelium and approximately 10% of infected patients develop peptic ulcers and 1–3% subjects develop gastric adenocarcinoma (10,11).
In this review, we address the molecular basis by which H. pylori acts as a carcinogen, the potential factors that enhance the risk from H. pylori and the accumulating epidemiological evidence for H. pylori infection and its effect on gastric cancer incidence.
2. Events leading to gastric carcinogenesis following H. pylori infection
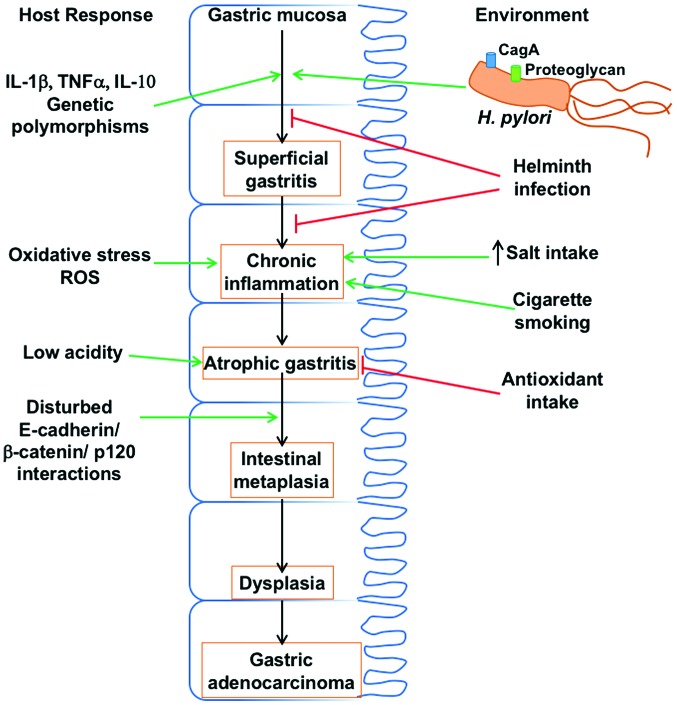
H. pylori infection of gastric epithelium leads to the development of intestinal-type adenocarcinoma with the primary event being the transition from normal mucosa to chronic superficial gastritis. Subsequently, atrophic gastritis ensues followed by intestinal metaplasia, leading to dysplasia and adenocarcinoma (Fig. 1) (12). Men are twice as susceptible as women to the intestinal type of gastric adenocarcinoma (13). Notably, the location of infection and formation of gastritis influences the outcomes. Thus, corpus-predominant gastritis leads to gastric cancer, probably because of lower acid secretion, whereas, infection of the gastric antrum, which increases acid production predisposes individuals to duodenal ulcer, actually decreases the risk of gastric cancer (14).
Figure 1.
Interaction between host responses, changes in gastric mucosa and environment during gastric carcinogenesis induced by Helicobacter pylori (H. pylori). A combination of several host responses, bacterial pathogen-mediated events, and environmental factors contribute to the precancerous cascade that culminates in gastric adenocarcinoma.
cag pathogenicity island and CagA
Several virulence factors present in H. pylori that are influenced by its genetic heterogeneity, are critical in the pathogenesis of gastric cancer. CagA, which is present in the DNA insertion element, cag pathogenicity island (cagPAI), was found to be important in carcinogenesis and thus, only H. pylori strains that contain cagPAI element enhance the risk of atrophic gastritis and gastric cancer, even though all strains of this bacterium can cause gastritis (15,16). H. pylori CagA is a 120 to 140-kDa protein, which translocates into host cells following attachment of the bacteria to the cell. Inside the host cell, CagA is phosphorylated by Abl and Src kinases, on tyrosine residue at four distinct glutamate-proline-isoleucine-tyrosine-alanine (EPIYA) motifs present at the C-terminal region of the protein, leading to morphological changes in the cell, including increased cell migration (17,18). The number and phosphorylation status of these EPIYA motifs is a determinant and indicator of risk for gastric cancer (19). Tyr-phospho-CagA activates tyrosine phosphatase (SHP-2) in the host cell, leading to sustained activation of ERK1/2, Crk adaptor, and C-terminal Src kinase (20). Interaction between phosphor-CagA and SHP leads to cell elongation by different mechanisms (21). Even non-phosphorylated CagA has pathogenic effects by causing aberrant activation of β-catenin, disruption of apical-junctional complexes, and a loss of cellular polarity (22). Additionally, non-phosphorylated CagA targets E-cadherin, the hepatocyte growth factor receptor c-Met, phospholipase C-γ, the adaptor protein Grb2, and other components that lead to proinflammatory and mitogenic responses, disruption of cell-cell junctions, and loss of cell polarity (Fig. 1) (23). Preclinical studies confirmed a role for CagA in the pathogenesis of gastric cancer, by demonstrating that transgenic mice expressing CagA show gastric epithelial cell proliferation and carcinoma, in a CagA phosphorylation-dependent manner (24).
Peptidoglycan
Along with CagA, H. pylori peptidoglycan can also be delivered into host cells and peptidoglycan binds with NodI (25), which triggers the NF-κB dependent pro-inflammatory pathway and interleukin (IL)-8, an inflammatory cytokine, secretion. Peptidoglycan is also shown to activate the PI3K-Akt pathway leading to cell proliferation, migration and prevention of apoptosis (26).
Other virulence factors present in H. pylori include VacA and outer membrane proteins, which are associated with ulceration as well as gastric cancer (27,28).
3. Inflammatory response to H. pylori infection
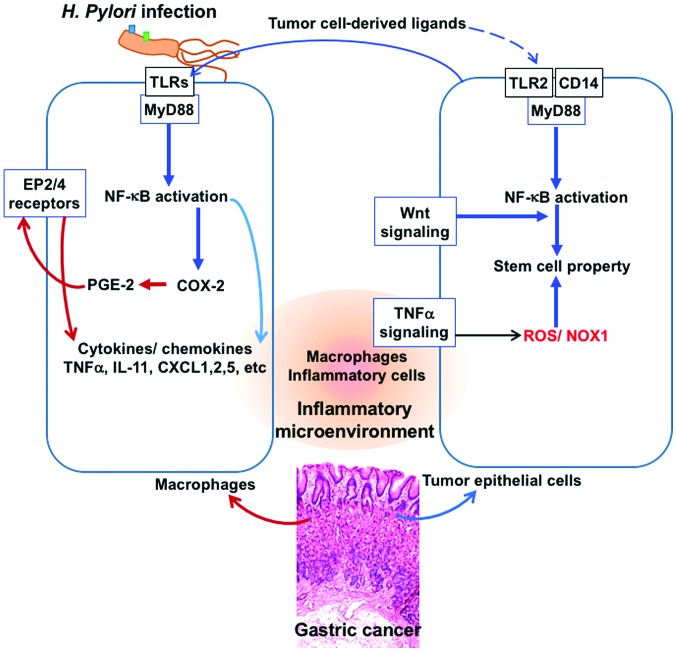
COX-2⁄PGE2 pathway
Inflammation of gastric epithelium is known to be associated with the development of gastric cancer (29). There are several mechanisms by which inflammation may promote cancer development and the induction of the cyclooxygenase-2/prostaglandin E2 (COX-2⁄PGE2) pathway and activation of NF-κB and Stat3 appear to be major pathways (Fig. 2) (30). Besides these, innate immune responses through the TLR/MyD88 adapter signaling also play a role in tumorigenesis (31,32). In fact, it has been shown that almost all the gastric tumors show an induction of COX-2 expression (33) and H. pylori infection is known to lead to COX-2 induction (34). Inflammation in combination with oncogenic activation, promotes tumorigenesis and also Wnt signaling activation (Fig. 2) with the accumulation of β-catenin, which facilitate tumor growth and this altered signaling has been observed in over 50% of gastric cancers (35). PGE2 signaling, through the EP4 receptor, is known to induce the expansion of CD133+ CD44+ cancer stem cells in intestinal tumors through the activation of PI3K and MAPK signaling (36), which potentially aggravates tumor growth.
Figure 2.
Tumor inflammatory microenvironment: Interplay of factors derived from H. pylori and tumor cells. A crosstalk between tumor cell-derived inflammatory factors and macrophage-derived factors during infection of Helicobacter pylori (H. pylori) results in aggravation of the inflammatory microenvironment and the tumor cells acquiring stem cell property and progression of tumor in gastric epithelium. Signaling through the TLR/MyD88/NF-κB pathways to activate cyclooxygenase-2 (COX-2) and production of prostaglandin E2 (PGE-2), release of cytokines such as TNF-α and production of ROS, in macrophages and in tumor cells facilitate this tumor inflammatory environment.
Infection of H. pylori induces inflammation through CagA injection into host cells followed by the activation of SHP and TLRs leading to chronic active gastritis and eventually gastric cancer. However, the expression pattern of inflammation markers is not always comparable between gastritis and gastric cancer. Thus, IL-8 and IL-11 expression is predominantly induced in gastric cancer, whereas in gastritis mostly TNF-α expression is increased. It has been suggested that once tumor growth starts, tumor cells also contribute to the inflammation of local microenvironment through different pathways, known as ‘tumor-elicited inflammation’, which is different from infection-induced inflammation, thereby resulting in different cytokine profiles from H. pylori infection-induced gastritis (29). Nevertheless, gastritis and gastric cancer demonstrate common increases in inflammatory cytokines CXCL1, CXCL2, CXCL5, CCL3, CCL4, and TLR2 (Fig. 2) (29). Inasmuch as these cytokines are effective in causing immune suppression, the ‘infection-associated’ and ‘tumor- elicited’ inflammation appears to promote and accelerate gastric tumorigenesis by activating the COX-2/PGE2 pathway and subsequent induction of tumor-promoting cytokines.
IL-1β
Another important cytokine, IL-1β is known to play a role in a variety of cellular activities such as inflammatory response and acid secretion by gastric epithelium (37). Disturbances in the regulation of IL-1β are observed in several cancer types and in particular, in IL-1β gene polymorphisms including IL-1β −31 (T>C) and IL-1β −511 (C>T) which are closely related to gastric cancer (Fig. 1) (38,39). Of note, it has been shown that IL-1β-511T polymorphism is present in all the Mozambican subjects with intestinal metaplasia (40). This polymorphism is also associated with the prevalence of dysplasia (41), indicating that the IL-1β T alleles are related to premalignant gastric lesions. Apparently, the same polymorphism of IL-1β is involved in the intestinal type of gastric cancers, which are triggered by H. pylori infection and not diffusive type (42). IL-1β gene polymorphisms also increase the production of IL-1β, which suppresses gastric acid secretion, and is related to the grade of gastric atrophy in patients with H. pylori infection (43). Additionally, H. pylori infection leads to elevated secretion of IL-1β and reduction in acid secretion (44). It has been suggested that a combination of IL-1β-511T/T polymorphism and H. pylori infection aggravates the development of gastric tumor more than either of these agents alone (45). Thus, infection of H. pylori promotes the expression of IL-1β, which leads to gastric carcinogenesis through its actions on both inflammatory and epithelial cells (46). Even though the precise molecular basis of these actions is not clear, it seems that hypochlorhydria and atrophic gastritis induced by IL-1β polymorphisms, which depends on H. pylori infection are critical in gastric cancer development (47).
4. Oxidative stress induced by H. pylori
A primary factor that is important in the events that lead to the progression of the inflammation-to-carcinoma is oxidative DNA damage induced by H. pylori infection (48), which is probably due to infiltrating neutrophils, and also direct effects of H. pylori (49). Production of reactive oxygen species in the H. pylori-infected gastric epithelium is linked to the presence of cagPAI and contribute to the oxidative stress response in gastric epithelial cells (50). It is well known that H. pylori infection causes elevated level of polyamines, in particular spermine and this is associated with an induction of spermine oxidase (51). Action of spermine oxidase on spermine leads to the production of elevated levels of hydrogen peroxide, which is a powerful oxidizing agent and also contributes to the production of free radicals such as hydroxyl radical (52). Besides, H. pylori also activates macrophages which show a significant upregulation of spermine oxidase, contributing to oxidative stress and damage to the gastric epithelial cells (53). Besides, altered polyamine metabolism and overexpression of arginase enzyme in the infected gastric epithelium leads to lowered NO production and increased production of spermine and hydrogen peroxide.
5. H. pylori and E-cadherin
E-cadherin, which is an adhesion molecule in epithelial tissues that is important in maintaining proper cellular architecture, is regulated by the binding of p120 to the cadherin juxtamembrane domain (54). Furthermore, the cytoplasmic domain of E-cadherin interacts with β-catenin and p120, which, in turn, interact with the cytoskeletal component actin. It has been documented that there is a loss of E-cadherin function in gastric cancer, and in fact promoter methylation of E-cadherin gene is induced by H. pylori infection, leading to reduction in E-cadherin expression (55). Following H. pylori infection, the translocated CagA in the gastric epithelial cells binds with E-cadherin, resulting in the dissociation of the E-cadherin-β-catenin complex and accumulation of β-catenin in cytoplasm and nucleus, where it transactivates β-catenin-dependent genes involved in carcinogenesis (23,56). Along with the downregulation of E-cadherin, a decreased expression or aberrant subcellular localization of p120, from membrane to the cytosol or nucleus, is commonly seen in gastric cancer (57). In the cytoplasm, p120 interacts with Rho GTPases and promotes motility and metastasis (58). Aberrant localization of p120 to the nucleus in gastric epithelia infected with H. pylori has been reported and p120 in nucleus can relieve transcriptional repression of the mmp-7 gene, which is involved in gastric tumorigenesis, leading to its enhanced expression (59).
6. Environmental factors and H. pylori-mediated gastric carcinogenesis
Gastric adenocarcinoma is strongly influenced by dietary salt intake, with high salt intake aggravating tumorigenesis (60). Epidemiological studies indicated that high salt intake increases the prevalence of H. pylori infection (61) and the incidence of gastric adenocarcinoma in infected patients (62). Experimental studies indicated that a high-salt diet and H. pylori infection exert synergistic effects on the development of premalignant lesions or gastric cancer (63), probably by elevating the production of inflammatory cytokines IL-1, IL-6 and TNF-α (64). However, the precise molecular events that underlie this synergistic effect on cancer development are not known. It has been suggested that high salt increases the expression of CagA, the potential carcinogen in H. pylori (65), which may be the reason for the observed synergy between H. pylori and salt for gastric cancer induction (Fig. 1).
In addition to salt, other factors that influence H. pylori infection-associated gastric cancer include helminth infections and dietary antioxidant intake, both of which seem to have a negative effect on the ability of H. pylori to induce gastritis and thus cancer. On the other hand, cigarette smoking is a potential risk factor for enhancing the tumorigenesis induced by H. pylori infection (21).
7. Conclusion
Intestinal type gastric adenocarcinomas are known to be causally linked to H. pylori infection, which leads to the initiation of chronic active gastritis, and adenocarcinoma. Even though most individuals with H. pylori infection do not show any clinical symptoms, 1–3% people with long-term infection develop gastric adenocarcinoma. Of the several mechanisms of the tumorigenesis induced by H. pylori, CagA and peptidoglycan of H. pylori, inflammation, oxidative stress and dysregulated E-cadherin/β-catenin/p120 interactions play an important role. Environmental and dietary factors, in particular salt intake and cigarette smoking are known to aggravate H. pylori-induced carcinogenesis. Thus, H. pylori infection appears to invoke multi-thronged mechanisms, to induce gastric adenocarcinoma. Nevertheless, many events in this tumorigenic process remain to be clarified and investigated.
References
- 1.Ferro A, Peleteiro B, Malvezzi M, Bosetti C, Bertuccio P, Levi F, Negri E, La Vecchia C, Lunet N. Worldwide trends in gastric cancer mortality (1980–2011), with predictions to 2015, and incidence by subtype. Eur J Cancer. 2014;50:1330–1344. doi: 10.1016/j.ejca.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.Correa P. Human gastric carcinogenesis: a multistep and multifactorial process - first American cancer society award lecture on cancer epidemiology and prevention. Cancer Res. 1992;52:6735–6740. [PubMed] [Google Scholar]
- 4.Herrera V, Parsonnet J. Helicobacter pylori and gastric adenocarcinoma. Clin Microbiol Infect. 2009;15:971–976. doi: 10.1111/j.1469-0691.2009.03031.x. [DOI] [PubMed] [Google Scholar]
- 5.He C, Tu H, Sun L, Xu Q, Li P, Gong Y, Dong N, Yuan Y. Helicobacter pylori-related host gene polymorphisms associated with susceptibility of gastric carcinogenesis: a two-stage case-control study in Chinese. Carcinogenesis. 2013;34:1450–1457. doi: 10.1093/carcin/bgt079. [DOI] [PubMed] [Google Scholar]
- 6.Souza RF, Spechler SJ. Concepts in the prevention of adenocarcinoma of the distal esophagus and proximal stomach. CA Cancer J Clin. 2005;55:334–351. doi: 10.3322/canjclin.55.6.334. [DOI] [PubMed] [Google Scholar]
- 7.Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311–1315. doi: 10.1016/S0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- 8.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 9.Weeks DL, Eskandari S, Scott DR, Sachs G. A H+-gated urea channel: the link between Helicobacter pylori urease and gastric colonization. Science. 2000;287:482–485. doi: 10.1126/science.287.5452.482. [DOI] [PubMed] [Google Scholar]
- 10.Peek RM, Jr, Blaser MJ. Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer. 2002;2:28–37. doi: 10.1038/nrc703. [DOI] [PubMed] [Google Scholar]
- 11.Peek RM, Jr, Crabtree JE. Helicobacter infection and gastric neoplasia. J Pathol. 2006;208:233–248. doi: 10.1002/path.1868. [DOI] [PubMed] [Google Scholar]
- 12.Sipponen P, Marshall BJ. Gastritis and gastric cancer. Western countries. Gastroenterol Clin North Am. 2000;29:579–592. doi: 10.1016/S0889-8553(05)70131-X. [DOI] [PubMed] [Google Scholar]
- 13.Correa P, Houghton J. Carcinogenesis of Helicobacter pylori. Gastroenterology. 2007;133:659–672. doi: 10.1053/j.gastro.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 14.Atherton JC. The pathogenesis of Helicobacter pylori-induced gastro-duodenal diseases. Annu Rev Pathol. 2006;1:63–96. doi: 10.1146/annurev.pathol.1.110304.100125. [DOI] [PubMed] [Google Scholar]
- 15.Shimoyama T, Fukuda S, Tanaka M, Mikami T, Munakata A, Crabtree JE. CagA seropositivity associated with development of gastric cancer in a Japanese population. J Clin Pathol. 1998;51:225–228. doi: 10.1136/jcp.51.3.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Torres J, Pérez-Pérez GI, Leal-Herrera Y, Muñoz O. Infection with CagA+ Helicobacter pylori strains as a possible predictor of risk in the development of gastric adenocarcinoma in Mexico. Int J Cancer. 1998;78:298–300. doi: 10.1002/(SICI)1097-0215(19981029)78:3<298::AID-IJC6>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 17.Stein M, Bagnoli F, Halenbeck R, Rappuoli R, Fantl WJ, Covacci A. c-Src/Lyn kinases activate Helicobacter pylori CagA through tyrosine phosphorylation of the EPIYA motifs. Mol Microbiol. 2002;43:971–980. doi: 10.1046/j.1365-2958.2002.02781.x. [DOI] [PubMed] [Google Scholar]
- 18.Segal ED, Cha J, Lo J, Falkow S, Tompkins LS. Altered states: involvement of phosphorylated CagA in the induction of host cellular growth changes by Helicobacter pylori. Proc Natl Acad Sci USA. 1999;96:14559–14564. doi: 10.1073/pnas.96.25.14559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basso D, Zambon CF, Letley DP, Stranges A, Marchet A, Rhead JL, Schiavon S, Guariso G, Ceroti M, Nitti D, et al. Clinical relevance of Helicobacter pylori cagA and vacA gene polymorphisms. Gastroenterology. 2008;135:91–99. doi: 10.1053/j.gastro.2008.03.041. [DOI] [PubMed] [Google Scholar]
- 20.Higashi H, Tsutsumi R, Muto S, Sugiyama T, Azuma T, Asaka M, Hatakeyama M. SHP-2 tyrosine phosphatase as an intracellular target of Helicobacter pylori CagA protein. Science. 2002;295:683–686. doi: 10.1126/science.1067147. [DOI] [PubMed] [Google Scholar]
- 21.Wroblewski LE, Peek RM, Jr, Wilson KT. Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbiol Rev. 2010;23:713–739. doi: 10.1128/CMR.00011-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bagnoli F, Buti L, Tompkins L, Covacci A, Amieva MR. Helicobacter pylori CagA induces a transition from polarized to invasive phenotypes in MDCK cells. Proc Natl Acad Sci USA. 2005;102:16339–16344. doi: 10.1073/pnas.0502598102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murata-Kamiya N, Kurashima Y, Teishikata Y, Yamahashi Y, Saito Y, Higashi H, Aburatani H, Akiyama T, Peek RM, Jr, Azuma T, et al. Helicobacter pylori CagA interacts with E-cadherin and deregulates the beta-catenin signal that promotes intestinal transdifferentiation in gastric epithelial cells. Oncogene. 2007;26:4617–4626. doi: 10.1038/sj.onc.1210251. [DOI] [PubMed] [Google Scholar]
- 24.Ohnishi N, Yuasa H, Tanaka S, Sawa H, Miura M, Matsui A, Higashi H, Musashi M, Iwabuchi K, Suzuki M, et al. Transgenic expression of Helicobacter pylori CagA induces gastrointestinal and hematopoietic neoplasms in mouse. Proc Natl Acad Sci USA. 2008;105:1003–1008. doi: 10.1073/pnas.0711183105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Viala J, Chaput C, Boneca IG, Cardona A, Girardin SE, Moran AP, Athman R, Mémet S, Huerre MR, Coyle AJ, et al. Nod1 responds to peptidoglycan delivered by the Helicobacter pylori cag pathogenicity island. Nat Immunol. 2004;5:1166–1174. doi: 10.1038/ni1131. [DOI] [PubMed] [Google Scholar]
- 26.Nagy TA, Frey MR, Yan F, Israel DA, Polk DB, Peek RM., Jr Helicobacter pylori regulates cellular migration and apoptosis by activation of phosphatidylinositol 3-kinase signaling. J Infect Dis. 2009;199:641–651. doi: 10.1086/596660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miehlke S, Kirsch C, AghaAmiri K, Günther T, Lehn N, Malfertheiner P, Stolte M, Ehninger G, Bayerdörffer E. The Helicobacter pylori vacA s1, m1 genotype and cagA is associated with gastric carcinoma in Germany. Int J Cancer. 2000;87:322–327. doi: 10.1002/1097-0215(20000801)87:3<322::AID-IJC3>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 28.Dossumbekova A, Prinz C, Gerhard M, Brenner L, Backert S, Kusters JG, Schmid RM, Rad R. Helicobacter pylori outer membrane proteins and gastric inflammation. Gut. 2006;55:1360–1361. [PMC free article] [PubMed] [Google Scholar]
- 29.Echizen K, Hirose O, Maeda Y, Oshima M. Inflammation in gastric cancer: interplay of the COX-2/prostaglandin E2 and Toll-like receptor/MyD88 pathways. Cancer Sci. 2016;107:391–397. doi: 10.1111/cas.12901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pradere JP, Dapito DH, Schwabe RF. The yin and yang of toll-like receptors in cancer. Oncogene. 2014;33:3485–3495. doi: 10.1038/onc.2013.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maeda Y, Echizen K, Oshima H, Yu L, Sakulsak N, Hirose O, Yamada Y, Taniguchi T, Jenkins BJ, Saya H, et al. Myeloid differentiation factor 88 signaling in bone marrow-derived cells promotes gastric tumorigenesis by generation of inflammatory microenvironment. Cancer Prev Res (Phila) 2016;9:253–263. doi: 10.1158/1940-6207.CAPR-15-0315. [DOI] [PubMed] [Google Scholar]
- 33.Saukkonen K, Rintahaka J, Sivula A, Buskens CJ, Van Rees BP, Rio MC, Haglund C, Van Lanschot JJ, Offerhaus GJ, Ristimaki A. Cyclooxygenase-2 and gastric carcinogenesis. APMIS. 2003;111:915–925. doi: 10.1034/j.1600-0463.2003.1111001.x. [DOI] [PubMed] [Google Scholar]
- 34.Sung JJ, Leung WK, Go MY, To KF, Cheng AS, Ng EK, Chan FK. Cyclooxygenase-2 expression in Helicobacter pylori-associated premalignant and malignant gastric lesions. Am J Pathol. 2000;157:729–735. doi: 10.1016/S0002-9440(10)64586-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oshima H, Matsunaga A, Fujimura T, Tsukamoto T, Taketo MM, Oshima M. Carcinogenesis in mouse stomach by simultaneous activation of the Wnt signaling and prostaglandin E2 pathway. Gastroenterology. 2006;131:1086–1095. doi: 10.1053/j.gastro.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 36.Wang D, Fu L, Sun H, Guo L, DuBois RN. Prostaglandin E2 promotes colorectal cancer stem cell expansion and metastasis in mice. Gastroenterology. 2015;149:1884–1895. doi: 10.1053/j.gastro.2015.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jayaraman P, SadaOvalle I, Nishimura T, Anderson AC, Kuchroo VK, Remold HG, Behar SM. IL-1β promotes antimicrobial immunity in macrophages by regulating TNFR signaling and caspase-3 activation. J Immunol. 2013;190:4196–4204. doi: 10.4049/jimmunol.1202688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumar S, Kumar A, Dixit VK. Evidences showing association of interleukin-1B polymorphisms with increased risk of gastric cancer in an Indian population. Biochem Biophys Res Commun. 2009;387:456–460. doi: 10.1016/j.bbrc.2009.07.033. [DOI] [PubMed] [Google Scholar]
- 39.Garza-González E, BosquesPadilla FJ, ElOmar E, Hold G, TijerinaMenchaca R, MaldonadoGarza HJ, Pérez-Pérez GI. Role of the polymorphic IL-1B, IL-1RN and TNF-A genes in distal gastric cancer in Mexico. Int J Cancer. 2005;114:237–241. doi: 10.1002/ijc.20718. [DOI] [PubMed] [Google Scholar]
- 40.Peleteiro B, Lunet N, Carrilho C, Durães C, Machado JC, La Vecchia C, Barros H. Association between cytokine gene polymorphisms and gastric precancerous lesions: systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2010;19:762–776. doi: 10.1158/1055-9965.EPI-09-0917. [DOI] [PubMed] [Google Scholar]
- 41.Marcos-Pinto R, DinisRibeiro M, Carneiro F, Wen X, Lopes C, Figueiredo C, Machado JC, Ferreira RM, Reis CA, Canedo P, et al. First-degree relatives of early-onset gastric cancer patients show a high risk for gastric cancer: phenotype and genotype profile. Virchows Arch. 2013;463:391–399. doi: 10.1007/s00428-013-1458-5. [DOI] [PubMed] [Google Scholar]
- 42.Kamangar F, Cheng C, Abnet CC, Rabkin CS. Interleukin-1B polymorphisms and gastric cancer risk - a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15:1920–1928. doi: 10.1158/1055-9965.EPI-06-0267. [DOI] [PubMed] [Google Scholar]
- 43.Waghray M, Zavros Y, SaquiSalces M, ElZaatari M, Alamelumangapuram CB, Todisco A, Eaton KA, Merchant JL. Interleukin-1beta promotes gastric atrophy through suppression of Sonic Hedgehog. Gastroenterology. 2010;138:562–572. doi: 10.1053/j.gastro.2009.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang M, Furuta T, Takashima M, Futami H, Shirai N, Hanai H, Kaneko E. Relation between interleukin-1beta messenger RNA in gastric fundic mucosa and gastric juice pH in patients infected with Helicobacter pylori. J Gastroenterol. 1999;34:10–17. (Suppl 11) [PubMed] [Google Scholar]
- 45.Zeng ZR, Hu PJ, Hu S, Pang RP, Chen MH, Ng M, Sung JJ. Association of interleukin 1B gene polymorphism and gastric cancers in high and low prevalence regions in China. Gut. 2003;52:1684–1689. doi: 10.1136/gut.52.12.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shigematsu Y, Niwa T, Rehnberg E, Toyoda T, Yoshida S, Mori A, Wakabayashi M, Iwakura Y, Ichinose M, Kim YJ, et al. Interleukin-1β induced by Helicobacter pylori infection enhances mouse gastric carcinogenesis. Cancer Lett. 2013;340:141–147. doi: 10.1016/j.canlet.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 47.Furuta T, ElOmar EM, Xiao F, Shirai N, Takashima M, Sugimura H. Interleukin 1beta polymorphisms increase risk of hypochlorhydria and atrophic gastritis and reduce risk of duodenal ulcer recurrence in Japan. Gastroenterology. 2002;123:92–105. doi: 10.1053/gast.2002.34156. [DOI] [PubMed] [Google Scholar]
- 48.Farinati F, Cardin R, Degan P, Rugge M, Mario FD, Bonvicini P, Naccarato R. Oxidative DNA damage accumulation in gastric carcinogenesis. Gut. 1998;42:351–356. doi: 10.1136/gut.42.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Obst B, Wagner S, Sewing KF, Beil W. Helicobacter pylori causes DNA damage in gastric epithelial cells. Carcinogenesis. 2000;21:1111–1115. doi: 10.1093/carcin/21.6.1111. [DOI] [PubMed] [Google Scholar]
- 50.Ding SZ, Minohara Y, Fan XJ, Wang J, Reyes VE, Patel J, DirdenKramer B, Boldogh I, Ernst PB, Crowe SE. Helicobacter pylori infection induces oxidative stress and programmed cell death in human gastric epithelial cells. Infect Immun. 2007;75:4030–4039. doi: 10.1128/IAI.00172-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cheng Y, Chaturvedi R, Asim M, Bussière FI, Scholz A, Xu H, Casero RA, Jr, Wilson KT. Helicobacter pylori-induced macrophage apoptosis requires activation of ornithine decarboxylase by c-Myc. J Biol Chem. 2005;280:22492–22496. doi: 10.1074/jbc.C500122200. [DOI] [PubMed] [Google Scholar]
- 52.Xu H, Chaturvedi R, Cheng Y, Bussiere FI, Asim M, Yao MD, Potosky D, Meltzer SJ, Rhee JG, Kim SS, et al. Spermine oxidation induced by Helicobacter pylori results in apoptosis and DNA damage: implications for gastric carcinogenesis. Cancer Res. 2004;64:8521–8525. doi: 10.1158/0008-5472.CAN-04-3511. [DOI] [PubMed] [Google Scholar]
- 53.Chaturvedi R, Cheng Y, Asim M, Bussière FI, Xu H, Gobert AP, Hacker A, Casero RA, Jr, Wilson KT. Induction of polyamine oxidase 1 by Helicobacter pylori causes macrophage apoptosis by hydrogen peroxide release and mitochondrial membrane depolarization. J Biol Chem. 2004;279:40161–40173. doi: 10.1074/jbc.M401370200. [DOI] [PubMed] [Google Scholar]
- 54.Jo TY, Jeon TY, Chae KH, Kim DH, Sim MS, Park DY, Suh KS. RImmunohistochemical evaluation of E-cadherin/catenin (alpha-, beta-, gamma-catenin and p120CTN) complex expression in early gastric cancer. Cancer Res Treat. 2003;35:16–24. doi: 10.4143/crt.2003.35.1.16. [DOI] [PubMed] [Google Scholar]
- 55.Perri F, Cotugno R, Piepoli A, Merla A, Quitadamo M, Gentile A, Pilotto A, Annese V, Andriulli A. Aberrant DNA methylation in non-neoplastic gastric mucosa of H. pylori infected patients and effect of eradication. Am J Gastroenterol. 2007;102:1361–1371. doi: 10.1111/j.1572-0241.2007.01284.x. [DOI] [PubMed] [Google Scholar]
- 56.Oliveira MJ, Costa AM, Costa AC, Ferreira RM, Sampaio P, Machado JC, Seruca R, Mareel M, Figueiredo C. CagA associates with c-Met, E-cadherin, and p120-catenin in a multiproteic complex that suppresses Helicobacter pylori-induced cell-invasive phenotype. J Infect Dis. 2009;200:745–755. doi: 10.1086/604727. [DOI] [PubMed] [Google Scholar]
- 57.Jawhari AU, Noda M, Pignatelli M, Farthing M. Up-regulated cytoplasmic expression, with reduced membranous distribution, of the src substrate p120(ctn) in gastric carcinoma. J Pathol. 1999;189:180–185. doi: 10.1002/(SICI)1096-9896(199910)189:2<180::AID-PATH414>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 58.Noren NK, Liu BP, Burridge K, Kreft B. p120 catenin regulates the actin cytoskeleton via Rho family GTPases. J Cell Biol. 2000;150:567–580. doi: 10.1083/jcb.150.3.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ogden SR, Wroblewski LE, Weydig C, RomeroGallo J, O'Brien DP, Israel DA, Krishna US, Fingleton B, Reynolds AB, Wessler S, et al. p120 and Kaiso regulate Helicobacter pylori-induced expression of matrix metalloproteinase-7. Mol Biol Cell. 2008;19:4110–4121. doi: 10.1091/mbc.E08-03-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tsugane S. Salt, salted food intake, and risk of gastric cancer: epidemiologic evidence. Cancer Sci. 2005;96:1–6. doi: 10.1111/j.1349-7006.2005.00006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Beevers DG, Lip GY, Blann AD. Salt intake and Helicobacter pylori infection. J Hypertens. 2004;22:1475–1477. doi: 10.1097/01.hjh.0000133736.77866.77. [DOI] [PubMed] [Google Scholar]
- 62.Shikata K, Kiyohara Y, Kubo M, Yonemoto K, Ninomiya T, Shirota T, Tanizaki Y, Doi Y, Tanaka K, Oishi Y, et al. A prospective study of dietary salt intake and gastric cancer incidence in a defined Japanese population: the Hisayama study. Int J Cancer. 2006;119:196–201. doi: 10.1002/ijc.21822. [DOI] [PubMed] [Google Scholar]
- 63.Gamboa-Dominguez A, Ubbelohde T, SaquiSalces M, RomanoMazzoti L, Cervantes M, Domínguez-Fonseca C, de la Luz Estreber M, Ruíz-Palacios GM. Salt and stress synergize H. pylori-induced gastric lesions, cell proliferation, and p21 expression in Mongolian gerbils. Dig Dis Sci. 2007;52:1517–1526. doi: 10.1007/s10620-006-9524-3. [DOI] [PubMed] [Google Scholar]
- 64.Sun J, Aoki K, Zheng JX, Su BZ, Ouyang XH, Misumi J. Effect of NaCl and Helicobacter pylori vacuolating cytotoxin on cytokine expression and viability. World J Gastroenterol. 2006;12:2174–2180. doi: 10.3748/wjg.v12.i14.2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gancz H, Jones KR, Merrell DS. Sodium chloride affects Helicobacter pylori growth and gene expression. J Bacteriol. 2008;190:4100–4105. doi: 10.1128/JB.01728-07. [DOI] [PMC free article] [PubMed] [Google Scholar]