Abstract
The treatment of malignant tumors following surgery is important in preventing relapse. Among all the post-surgery treatments, immunomodulators have demonstrated satisfactory effects on preventing recurrence according to recent studies. Ginsenoside is a compound isolated from panax ginseng, which is a famous traditional Chinese medicine. Ginsenoside aids in killing tumor cells through numerous processes, including the antitumor processes of ginsenoside Rh2 and Rg1, and also affects the inflammatory processes of the immune system. However, the role that ginsenoside serves in antitumor immunological activity remains to be elucidated. Therefore, the present study aimed to analyze the effect of ginsenoside Rh2 on the antitumor immunological response. With a melanoma mice model, ginsenoside Rh2 was demonstrated to inhibit tumor growth and improved the survival time of the mice. Ginsenoside Rh2 enhanced T-lymphocyte infiltration in the tumor and triggered cytotoxicity in spleen lymphocytes. In addition, the immunological response triggered by ginsenoside Rh2 could be transferred to other mice. In conclusion, the present study provides evidence that ginsenoside Rh2 treatment enhanced the antitumor immunological response, which may be a potential therapy for melanoma.
Keywords: animals, mice, tumor, melanoma, immunotherapy, cytotoxic T lymphocytes, ginsenoside Rh2 (GRh2)
Introduction
Surgical resection and focal tumor ablation techniques are the first-line treatments for melanoma and have been used for decades; the results have been satisfactory in most cases (1). However, in the majority of cases, surgery alone is not enough to completely remove or kill all the tumor cells and recurrence may occur. Therefore, post-surgical treatment may be as important as the surgery itself. In addition to radiotherapy and traditional chemotherapy, which are the main methods currently used to suppress tumor cell activity (2), immunomodulators have potential antitumor action; previous studies have investigated immunomodulators' effects on the antitumor immunological response have been investigated and demonstrated an antitumor effect (3–5).
Panax ginseng is one of the most famous herbal medicines used in China. It serves an important role in strength recovery, body nourishing, and health defending in the view of traditional Chinese medicine. As it has organ-protecting and spirit-calming effect, panax ginseng is known as ‘herbaceous king’ in China (6). Ginsenoside is the major compound isolated from panax ginseng and the ginsenoside family has>30 subtypes. Previous studies have demonstrated that ginsenoside acts as an immunomodulator in arthritis and other inflammatory processes (7–9). In addition, ginsenoside was considered to possess tumor cell-killing functions and to have a suppressive effect on tumor growth (10–12). Thus, ginsenoside serves a role in immune modulation and tumor treatment (13,14), which may indicate its potential triggering effect on antitumor immunological response. In the present study, a melanoma mouse model was used to examine ginsenoside Rh2′s triggering effect on the immunological response.
Materials and methods
Animals, cell lines and medium
Male C57BL6 mice (3–4 weeks old) were purchased from the laboratory animal research centre of the Fourth Military Medical University (FMMU), Xi'an, China, and maintained in specific pathogen-free (SPF) conditions. Animal experimental protocols were all reviewed and approved by the Ethics Committee of FMMU. The B16-F10 melanoma cell line was purchased from the American Type Culture Collection (Manassas, VA, USA). The B16 cell was grown in RPMI-1640 medium (Hyclone; Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fatal calf serum (FBS; Hyclone; Thermo Fisher Scientific, Inc.), in a humidified incubator containing 5% CO2. When the cells were ~80% confluent, the cells were washed with phosphate buffer saline (PBS; pH 7.4) 3 times, then 0.25% trypsin EDTA (Gibco; Thermo Fisher Scientific, Inc.) was added to passage the cells.
Tumor models
When the B16-F10 melanoma cells reached 90% confluence, the cells were washed with PBS 3 times, then 0.25% trypsin EDTA was added for detachment. Following another 3 washes with PBS, the cells were re-suspended in PBS at the density of 2×107 cells/ml. Under sterile conditions, 50 µl of the suspension was gently injected into the left back (subcutaneous tissue) of each mouse. The mice were then contained in SPF conditions for 5 days, by which point the tumor diameter was ~5–6 mm.
Grouping and ginsenoside arrangement
The mice were randomly arranged into 4 groups of 80 mice: Tumor group, G-L group, G-H group and Control group. G-L and G-H refer to a low or high dose of ginsenoside Rh2 injection. For the tumor group, G-L group and G-H group, the B16-F10 cell line was injected into the mice as described above. These 3 groups became tumor bearing groups. For the control group, the same volume of PBS was injected instead. Ginsenoside Rh2, (National Institute for the Control of Pharmaceutical and Biological Products, Beijing, China), was injected into the left back of mice in the G-L and G-H groups. The dose for the G-H group was 0.5 mg/kg or 0.2 mg/kg for G-L group, every 2 days after day 5. PBS was injected in the tumor and control groups at the same time points.
Histological analysis and immunohistochemistry
Between days 3–12, three mice from each group were sacrificed and necropsied every 3 days. The tumor sizes were measured by a caliper and calculated using the formula [(AxB2) × 0.4]. To evaluate the extent of lymphocyte infiltration in tumor tissue, the tumors were completely dissected and analyzed by immunohistochemistry: 6-µm-thick frozen sections of tumor tissues of the tumor group, G-L group and G-H group were stained with the rat anti-mouse anti-CD4 (dilution, 1:20; catalog no., 550280; BD Biosciences, Franklin Lakes, NJ, USA) antibody; 4-µm-thick paraffin sections were stained with the rat anti-mouse anti-CD8a (dilution, 1:20; catalog no., 550281; BD Biosciences) antibody. All sections were visualized via a three step staining procedure in combination with biotinylated polyclonal goat anti-rat Ig (dilution, 1:500; catalog no., 559286; BD Biosciences) as the secondary antibody and streptavidin-HRP (BD Biosciences) together with the diaminobenzidine (Sangon Biotech, Shanghai, China) detection system. Then the tissue sections were stained with hematoxylin (ZhuangZhi Biotech, Xi'an, China) for nuclear staining. The immunohistochemistry results were examined using light microscopy (Olympus, Tokyo, Japan). Parts of the mice were maintained for survival analysis.
Cytotoxicity assay
At day 15, 3 mice from each group (tumor group, G-L group, G-H group and control group) were sacrificed and their spleens were necropsied. The spleen was ground down and the lymphocytes were isolated using lymphocyte separation medium (Sigma-Aldrich, St. Louis, MO, USA) and primarily cultured. Lymphocytes separated with lymphocyte separation medium were primarily cultured in RPMI-1640 medium supplemented with 10% FBS as suspension, and 1 µg/ml penicillin/streptomycin (ZhuangZhi Biotech) was added in primary culture. All cell flasks were contained in a humidified incubator containing 5% CO2. Lymphocytes from the tumor group, G-L group, G-H group and control group were gathered for cytotoxicity analysis, which was performed using the CytoTox 96 Non-Radioactive LDH Cytotoxicity Assay (Promega Corporation, Madison, WI, USA) according to the manufacturer's protocol.
Adoptive transfers
At day 15, 3 mice from each group were injected with an additional 2×104 B16-F10 cells with the method described above. After 2 days, spleen lymphocytes from each group were isolated and cultured. Then lymphocytes were injected into recipient naïve mice through tail veins. The recipient naïve mice receiving lymphocytes from the tumor group, G-L group, G-H group and control group were named as tumor-trans group, G-L-trans group, G-H-trans group and control-trans group. These mice were injected with 1×106 B16-F10 cells 3 days later. Another 15 days later, these mice were sacrificed and the tumor sizes were measured. The survival time of the naïve mice were recorded after B16 challenge for survival analysis.
Statistical analysis
The majority of the experiments were performed in triplicate and one representative experiment was selected to be presented. All data are expressed as the mean ± standard deviation. Data analyses were performed using SPSS software, version 22.0 (IBM SPSS, Armonk, NY, USA). Significance was determined using Student's t-test for two groups and one-way ANOVA for multiple comparisons. The Kaplan-Meier function was calculated for survival and a log-rank test was used to assess the differences of mice survival. P<0.05 was considered to indicate a statistically significant difference.
Results
Antitumor effect of ginsenoside Rh2
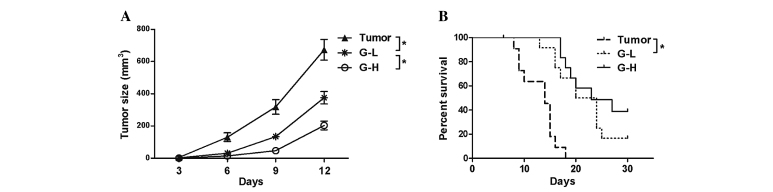
A total of 15 days following B16-F10 cell injection, tumor sizes from the 3 tumor bearing groups were measured. This analysis demonstrated that the tumor sizes in the G-L group and G-H group were reduced compared with the tumor group (Fig. 1A, P<0.05). The survival analysis revealed that the ginsenoside Rh2 treated groups survived longer than the untreated tumor group and the effect was dose-dependent (Fig. 1B, P<0.05), indicating that ginsenoside Rh2 had served an antitumor role in this mouse model.
Figure 1.
Effect of ginsenoside Rh2 treatment. (A) Tumor sizes in G-L group and G-H group were reduced compared with the tumor group (P<0.05). The antitumor effect of ginsenoside Rh2 was greater in the G-H group than in G-L group (P<0.05). (B) Kaplan-Meier survival ratio demonstrated that mice from the G-L group and G-H group had improved survival rates compared with the tumor group (P<0.05). The survival rate in the G-H group was longer compared with the G-L group (P<0.05). *P<0.05. G-L, low dose of ginsenoside Rh2; G-H, high dose of ginsenoside Rh2.
Ginsenoside Rh2 triggers CD4+ and CD8a+ T-lymphocytes' infiltration in tumor tissues
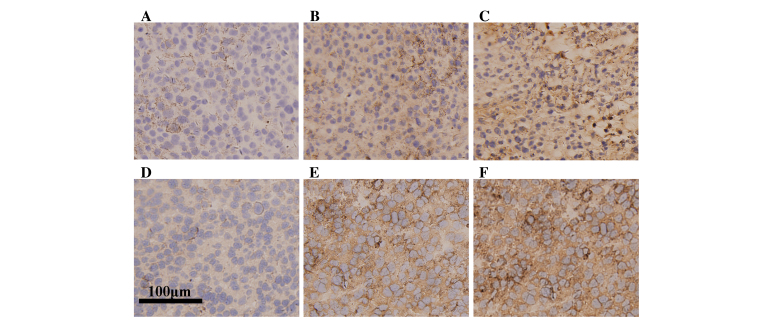
Histologically, the 3 tumor bearing groups exhibited similar general features in tumor shape, smoothness, hardness and looked the same at cross section. However immunohistochemical analysis revealed the tumor group exhibited only sparse infiltration of CD8a+ lymphocytes (Fig. 2A), compared with an increase in infiltrative number within the tumors from the G-L and G-H groups (Fig. 2B and C). In addition, the staining in G-H group was more intense compared with the G-L group. Similarly, the tumor group exhibited low infiltration of CD4+ lymphocytes (Fig. 2D), compared with an increase in infiltrative number within the tumors from the G-L and G-H groups (Fig. 2E and F). These results indicate that ginsenoside Rh2 treatment increases lymphocyte infiltration in tumor tissue, suggesting that the immunological response is enhanced.
Figure 2.
Immunohistochemical staining of CD8a and CD4. CD8a immunostaining of tumors from (A) tumor group, (B) G-L group and (C) G-H group. CD4 staining of tumors from (D) tumor group, (E) G-L group and (F) G-H group. G-L group and G-H group exhibited a greater level of CD4+ or CD8a+ lymphocyte infiltration compared with the tumor group, and compared with the G-L group, the G-H group exhibited greater infiltration levels (magnification 1,000x; bar: 100 µm). G-L, low dose of ginsenoside Rh2; G-H, high dose of ginsenoside Rh2.
Ginsenoside Rh2 treatment increases T-lymphocyte cytotoxicity
Immunohistochemistry analysis revealed that a greater number of CD4+ and CD8a+ T-lymphocytes infiltrated the tumor tissue following ginsenoside Rh2 injection. To investigate the cytotoxicity of the lymphocytes, a non-radioactive cytotoxicity assay kit was used to test whether treatment of ginsenoside Rh2 led to activation of lymphocytes' killing function. It was observed that ginsenoside Rh2 treatment did enhance the lymphocytes' cytotoxicity against B16-F10 cells and this enhancement in cytotoxicity was increased in the G-H group compared with the G-L group (Fig. 3, P<0.05).
Figure 3.
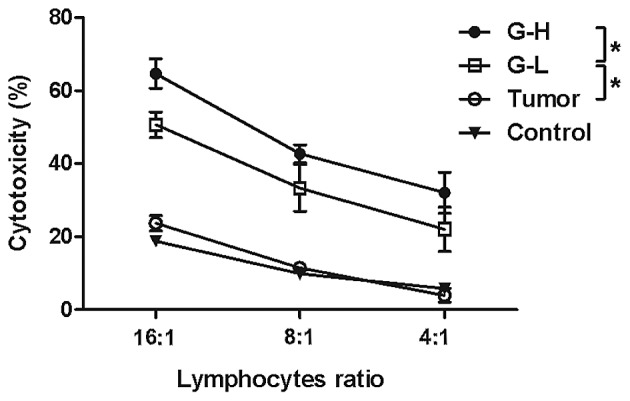
Cytotoxicity of spleen lymphocytes from control group, tumor group, G-L group and G-H group. Mice treated with ginsenoside Rh2 demonstrated increased lymphocyte cytotoxicity compared with control group and tumor group (P<0.05). Cytotoxicity was higher in the G-H group compared to the G-L group (P<0.05). *P<0.05. G-L, low dose of ginsenoside Rh2; G-H, high dose of ginsenoside Rh2.
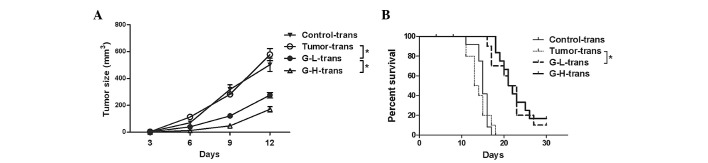
Adoptive transfer of antitumor immunity in ginsenoside Rh2 arranging groups demonstrated improved protection
To further demonstrate the antitumor effect of the ginsenoside Rh2 treated lymphocytes, the present study also investigated whether this antitumor protection of lymphocytes could be transferred from ginsenoside Rh2 treated mice to naïve mice. Delayed tumor growth was observed in recipient naïve mice, which had received lymphocytes from ginsenoside Rh2 treated groups. The G-H-trans group exhibited the smallest tumors (Fig. 4A, P<0.05). No delay in tumor growth was observed in the mice which had received lymphocytes from the tumor or control group. Survival analysis also indicated a difference among these groups: Naïve mice which had received lymphocytes from ginsenoside Rh2 treated groups exhibited improved survival rates (Fig. 4B, P<0.05). These results indicate that the antitumor immunity triggered by ginsenoside Rh2 may be transferred to naïve mice.
Figure 4.
Tumor growth and survival from lymphocytes adoptive transferred groups. The recipient naïve mice receiving lymphocytes from tumor group, G-L group, G-H group and control group were named as tumor-trans group, G-L-trans group, G-H-trans group and control-trans group, respectively. (A) Tumor sizes in G-L-trans group and G-H-trans group were smaller than in control-trans group and tumor-trans group (P<0.05). The antitumor effect of lymphocytes transferred was greater in the G-H-trans group than in the G-L-trans group (P<0.05). (B) Kaplan-Meier survival ratio demonstrated that mice from the G-L-trans group and G-H-trans group survived longer than the control-trans group and tumor-trans group (P<0.05). *P<0.05.
Discussion
Surgery resection or tumor ablation techniques are the primary treatment options for the majority of patients. However, surgery cannot completely remove the entire tumor tissue or kill all the malignant cells. Surgery alone will not prevent recurrence. Therefore, post-surgery therapy is important. Antitumor immunomodulators have potential as post-surgery treatments (4). Anti-cytotoxic T-lymphocyte-associated antigen (CTLA), for example, has been described to be a tumor rejection promoter, which binds to the inhibitory T-cell co-receptor CTLA and enhances T-cell functions. CTLA is located on the surface of T-cells, and acts as an ‘off’ switch when bound to CD80 or CD86 on the surface of antigen-presenting cells. As a classical immunomodulator, anti-CTLA has a great antitumor effect on many kinds of tumors (15–17). Apart from anti-CTLA, IL-2, IFN-gamma, and a number of other immunomodulators also function in antitumor immunological response (18).
Ginsenoside is a compound isolated from panax ginseng, which is popular in China for its nourishing and protecting effect on human body (19). Ginsenoside Rh2 has been reported to have an inhibitory effect on prostatic cancer (10), hepatic carcinoma (11), glioblastoma (20) and numerous other malignant tumors (13,21). In addition to antitumor effects, the ginsenoside family was also discovered to serve an important role in immunomodulation. Ginsenoside Rg1 has been demonstrated to promote immunological response and may enhance T-cell activities (22,23). Ginsenoside Rh2 and Rd also acted as immunomodulators in a lot of physiological and pathological processes (13,24). However, the important relationship between the antitumor effect and immunological response of ginsenoside is poorly reported. The present study hypothesized that ginsenoside Rh2 could enhance antitumor immunological response.
In the present study, ginsenoside Rh2 was injected into tumor bearing mice. This treatment inhibited the tumor growth and prolonged mice survival. Also, a greater number of T-lymphocytes infiltrated the tumor after ginsenoside Rh2 treatment. To investigate the function of the systemic lymphocytes, cytotoxicity experiments were performed and the lymphocytes from ginsenoside Rh2 treated groups exhibited enhanced tumor killing ability. Furthermore, in the adoptive transfer experiment, the immunity from ginsenoside Rh2 treated mice was successfully transferred to naïve mice. In the present cytotoxicity experiments, spleen lymphocytes from ginsenoside Rh2 treated mice were used. Initially another method was used to trigger an enhanced immune response using ginsenoside Rh2 treated lymphocytes. Spleen lymphocytes from the control group were cultured with cell medium containing ginsenoside Rh2, which one might expect to yield similar results. However, ginsenoside Rh2 in the cell medium did not trigger the cytotoxicity of lymphocytes as it did in vivo. Therefore the triggering effect of ginsenoside Rh2 on immunity may rely on the microenvironment in vivo, and perhaps ginsenoside Rh2 does not directly interact with T-lymphocytes (25). The mechanism between ginsenoside Rh2 and lymphocytes or antigen presenting cell (APC) requires further research.
In conclusion, a melanoma mouse model was used to demonstrate that ginsenoside Rh2 enhanced the antitumor immunological response Therefore, this Chinese herbal extract may have potential as an antitumor treatment.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (grant no. 81402574). The authors would like to thank Miss Xin-Yue Zhao for her assistance in English language editing.
References
- 1.Chu KF, Dupuy DE. Thermal ablation of tumours: Biological mechanisms and advances in therapy. Nat Rev Cancer. 2014;14:199–208. doi: 10.1038/nrc3672. [DOI] [PubMed] [Google Scholar]
- 2.Robinson RD, Knudtson JF. Fertility preservation in patients receiving chemotherapy or radiotherapy. Mo Med. 2014;111:434–438. [PMC free article] [PubMed] [Google Scholar]
- 3.Killion JJ, Fidler IJ. Therapy of cancer metastasis by tumoricidal activation of tissue macrophages using liposome-encapsulated immunomodulators. Pharmacol Ther. 1998;78:141–154. doi: 10.1016/S0163-7258(98)00004-7. [DOI] [PubMed] [Google Scholar]
- 4.Sheridan C. Industry pursues co-stimulatory receptor immunomodulators to treat cancer. Nat Biotechnol. 2013;31:181–183. doi: 10.1038/nbt0313-181. [DOI] [PubMed] [Google Scholar]
- 5.Berinstein NL. Enhancing cancer vaccines with immunomodulators. Vaccine. 2007;25:B72–B88. doi: 10.1016/j.vaccine.2007.06.043. (Suppl 2) [DOI] [PubMed] [Google Scholar]
- 6.Yun TK. Brief introduction of Panax ginseng C.A. Meyer. J Korean Med Sci. 2001;16:S3–S5. doi: 10.3346/jkms.2001.16.S.S3. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu H, Chen J, Wang Q, Jia X, Song S, Yuan P, Liu K, Liu L, Zhang Y, Zhou A, Wei W. Ginsenoside metabolite compound K attenuates inflammatory responses of adjuvant-induced arthritis rats. Immunopharmacol Immunotoxicol. 2014;36:124–129. doi: 10.3109/08923973.2014.880717. [DOI] [PubMed] [Google Scholar]
- 8.Liu KK, Wang QT, Yang SM, Chen JY, Wu HX, Wei W. Ginsenoside compound K suppresses the abnormal activation of T lymphocytes in mice with collagen-induced arthritis. Acta Pharmacol Sin. 2014;35:599–612. doi: 10.1038/aps.2014.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen J, Wu H, Wang Q, Chang Y, Liu K, Song S, Yuan P, Fu J, Sun W, Huang Q, et al. Ginsenoside metabolite compound k alleviates adjuvant-induced arthritis by suppressing T cell activation. Inflammation. 2014;37:1608–1615. doi: 10.1007/s10753-014-9887-0. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Q, Hong B, Wu S, Niu T. Inhibition of prostatic cancer growth by ginsenoside Rh2. Tumour Biol. 2015;36:2377–2381. doi: 10.1007/s13277-014-2845-5. [DOI] [PubMed] [Google Scholar]
- 11.Shi Q, Li J, Feng Z, Zhao L, Luo L, You Z, Li D, Xia J, Zuo G, Chen D. Effect of ginsenoside Rh2 on the migratory ability of HepG2 liver carcinoma cells: Recruiting histone deacetylase and inhibiting activator protein 1 transcription factors. Mol Med Rep. 2014;10:1779–1785. doi: 10.3892/mmr.2014.2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang XP, Tang GD, Fang CY, Liang ZH, Zhang LY. Effects of ginsenoside Rh2 on growth and migration of pancreatic cancer cells. World J Gastroenterol. 2013;19:1582–1592. doi: 10.3748/wjg.v19.i10.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou DB, Hu CP, Liang S, Yang HZ. Effect of ginsenoside Rh2 on immunocompetence of alveolar macrophages in patients with non-small cell lung cancer. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2007;32:868–872. (In Chinese) [PubMed] [Google Scholar]
- 14.Wu R, Ru Q, Chen L, Ma B, Li C. Stereospecificity of ginsenoside Rg3 in the promotion of cellular immunity in hepatoma H22-bearing mice. J Food Sci. 2014;79:H1430–H1435. doi: 10.1111/1750-3841.12518. [DOI] [PubMed] [Google Scholar]
- 15.Waitz R, Solomon SB, Petre EN, Trumble AE, Fassò M, Norton L, Allison JP. Potent induction of tumor immunity by combining tumor cryoablation with anti-CTLA-4 therapy. Cancer Res. 2012;72:430–439. doi: 10.1158/0008-5472.CAN-11-1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li F, Guo Z, Yu H, Zhang X, Si T, Liu C, Yang X, Qi L. Anti-tumor immunological response induced by cryoablation and anti-CTLA-4 antibody in an in vivo RM-1 cell prostate cancer murine model. Neoplasma. 2014;61:659–671. doi: 10.4149/neo_2014_081. [DOI] [PubMed] [Google Scholar]
- 17.Kvistborg P, Philips D, Kelderman S, Hageman L, Ottensmeier C, Joseph-Pietras D, Welters MJ, van der Burg S, Kapiteijn E, Michielin O, et al. Anti-CTLA-4 therapy broadens the melanoma-reactive CD8+ T cell response. Sci Transl Med. 2014;6 doi: 10.1126/scitranslmed.3008918. 254ra128. [DOI] [PubMed] [Google Scholar]
- 18.Zhao Q, Tong L, He N, Feng G, Leng L, Sun W, Xu Y, Wang Y, Xiang R, Li Z. IFN-gamma mediates graft-versus-breast cancer effects via enhancing cytotoxic T lymphocyte activity. Exp Ther Med. 2014;8:347–354. doi: 10.3892/etm.2014.1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gu Y, Wang GJ, Sun JG, Jia YW, Wang W, Xu MJ, Lv T, Zheng YT, Sai Y. Pharmacokinetic characterization of ginsenoside Rh2, an anticancer nutrient from ginseng, in rats and dogs. Food Chem Toxicol. 2009;47:2257–2268. doi: 10.1016/j.fct.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Li S, Guo W, Gao Y, Liu Y. Ginsenoside Rh2 inhibits growth of glioblastoma multiforme through mTor. Tumour Biol. 2015;36:6207–2612. doi: 10.1007/s13277-014-2880-2. [DOI] [PubMed] [Google Scholar]
- 21.Li B, Zhao J, Wang CZ, Searle J, He TC, Yuan CS, Du W. Ginsenoside Rh2 induces apoptosis and paraptosis-like cell death in colorectal cancer cells through activation of p53. Cancer Lett. 2011;301:185–192. doi: 10.1016/j.canlet.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JH, Han Y. Ginsenoside Rg1 helps mice resist to disseminated candidiasis by Th1 type differentiation of CD4+ T cell. Int Immunopharmacol. 2006;6:1424–1430. doi: 10.1016/j.intimp.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 23.Lee EJ, Ko E, Lee J, Rho S, Ko S, Shin MK, Min BI, Hong MC, Kim SY, Bae H. Ginsenoside Rg1 enhances CD4(+) T-cell activities and modulates Th1/Th2 differentiation. Int ImmunoPharmacol. 2004;4:235–244. doi: 10.1016/j.intimp.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 24.Yang Z, Chen A, Sun H, Ye Y, Fang W. Ginsenoside Rd elicits Th1 and Th2 immune responses to ovalbumin in mice. Vaccine. 2007;25:161–169. doi: 10.1016/j.vaccine.2006.05.075. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Liu Y, Zhang XY, Xu LH, Ouyang DY, Liu KP, Pan H, He J, He XH. Ginsenoside Rg1 regulates innate immune responses in macrophages through differentially modulating the NF-κB and PI3K/Akt/mTOR pathways. Int Immunopharmacol. 2014;23:77–84. doi: 10.1016/j.intimp.2014.07.028. [DOI] [PubMed] [Google Scholar]