Abstract
Background:
Tobacco smoking has been recognized as the most important risk factor for chronic obstructive pulmonary disease (COPD) for a long time, but recent studies have shown that nonsmokers also contribute to a significant proportion of COPD. This study was performed to find out the proportion of nonsmoker individuals among COPD patients and to determine various etiologies in nonsmoker COPD patients.
Materials and Methods:
This study was an observational cross-sectional study conducted in Department of Pulmonary Medicine, MLN Medical College, Allahabad. A total of 200 COPD patients, aged >18 years of either gender with COPD, diagnosed by clinical and spirometric criteria (GOLD guideline) were included in the study.
Results:
Of the 200 COPD patients, the proportion of nonsmoker patients was 56.5%, and the smoker was 43.5%. Among 113 nonsmoker COPD patients, maximum number of patients (69.03%) belonged to low socioeconomic status but most important and statistically significant risk factor was exposure to biomass smoke (53.98%), other significant risk factors were treated pulmonary tuberculosis (32.74%), and long-standing asthma (14.16%). Risk factors that were not statistically significant were occupational exposure (9.73%), exposure to outdoor air pollution (3.54%), and lower respiratory tract infection during childhood (1.77%). The patients who were exposed to more than one risk factors, developed COPD at an earlier age.
Conclusions:
This study revealed that nonsmokers contribute a significant proportion of COPD patients. Multiple risk factors other than smoking also play a major role in the development of COPD, particularly exposure to biomass smoke, treated pulmonary tuberculosis, and long-standing asthma.
KEY WORDS: Chronic obstructive pulmonary disease, nonsmoker, risk factor, spirometry
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide.[1,2,3] It is projected to rank third among all causes of death by 2020.[4] Tobacco smoking has been recognised as the most important risk factor for COPD for a long time. Previously most of the studies on COPD mainly focused on smoking as a risk factor[5] but recent studies showed that nonsmokers also contribute a significant proportion of COPD. The burden of COPD in nonsmoker is higher than previously believed in both developed and developing countries.[6]
Risk factors of COPD in nonsmokers may include genetic factors, long-standing asthma, environmental tobacco smoke, outdoor air pollution (from traffic and other sources), biomass smoke, occupational exposure, recurrent respiratory tract infection in early childhood, pulmonary tuberculosis, and low socioeconomic status. This study was conducted to find out the proportion of nonsmoker individuals among COPD patients and to determine various risk factors in nonsmoker COPD patients.
MATERIALS AND METHODS
This study was conducted in the Department of Pulmonary Medicine, MLN Medical College, Allahabad, over a period of 1 year, from August 2014 to July 2015. It was an observational cross-sectional study. Total 200 patients of COPD, after a screening of consecutive 315 patients attending indoor and outdoor having clinical presentation suggestive of COPD, were selected for the study. All patients aged >18 years of either sex with COPD diagnosed by clinical and spirometric criteria (GOLD guideline) were included in the study.
All the patients qualifying inclusion criteria were explained in detail about study and procedures involved, and informed consent was taken. A detailed history was taken about symptoms such as a cough, expectoration, breathlessness, fever, weight loss, hemoptysis, and chest pain. Clinical examination and necessary investigation were done including chest radiograph posteroanterior view, sputum acid-fast bacilli stain, and spirometry. Further patients were subjected to a questionnaire for determining the history of exposure to various types of risk factors for COPD. The study data were analyzed by Chi-square test, Z-test and one-way ANOVA with Tukey's test using GraphPad Prism 5 (GraphPad Software, San Diego, CA, USA), P < 0.05 was considered significant.
RESULTS
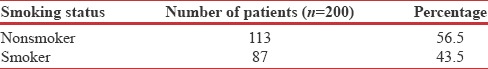
Total 200 COPD patients were included in the study, and they were classified on the basis of history of smoking into two groups - nonsmoker and smoker. The proportion of nonsmoker individuals among total COPD patients was found to be higher than smokers [Table 1].
Table 1.
Distribution of patients according to smoking status
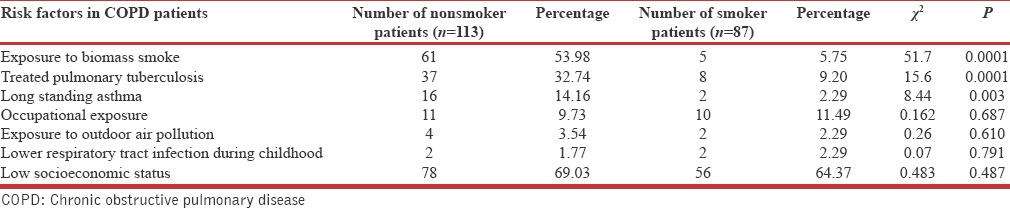
Of 113 nonsmoker COPD patients, maximum number of patients (69.03%) belong to low socioeconomic status, but most important and statistically significant risk factor was exposure to biomass smoke (53.98%), other significant risk factors were treated pulmonary tuberculosis (32.74%), and chronic asthma (14.16%). Risk factors that were not statistically significant were occupational exposure (9.73%), exposure to outdoor air pollution (3.54%), and lower respiratory tract infection during childhood (1.77%) [Table 2].
Table 2.
Distribution of patients according to risk factors for chronic obstructive pulmonary disease
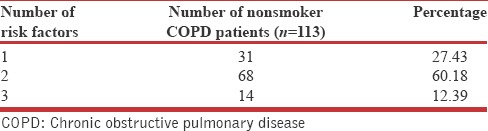
Most of the nonsmoker COPD patients (82, i.e., 72.57%) had more than 1 risk factor with majority of patients (68, i.e., 60.18%) having 2 risk factors [Table 3].
Table 3.
Distribution of nonsmoker chronic obstructive pulmonary disease patients according to number of risk factors
It was found that as the number of risk factors in nonsmoker COPD patients increased, mean age for development of COPD decreased. The difference between mean age of patients with 1 risk factor and 2 risk factors, and between 1 and 3 risk factors was found to be statistically significant (P < 0.05). Difference between 2 and 3 risk factors was not significant (P > 0.05) [Table 4 and Figure 1].
Table 4.
Correlation between number of risk factors and mean age of nonsmoker chronic obstructive pulmonary disease patients
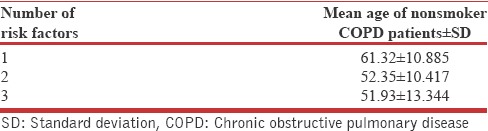
Figure 1.
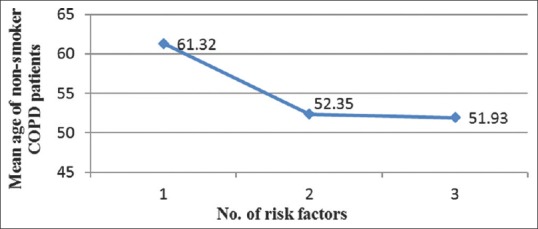
Relation between number of risk factors and mean age of nonsmoker chronic obstructive pulmonary disease patients
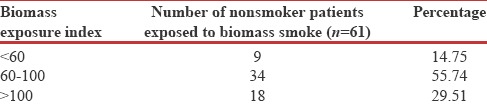
Maximum number of nonsmoker COPD patients (52, i.e., 85.25%) exposed to biomass smoke had biomass exposure index more than sixty with majority of patients (34, i.e., 55.74%) having biomass exposure index between 60 and 100 [Table 5].
Table 5.
Distribution of nonsmoker chronic obstructive pulmonary disease patients exposed to biomass smoke according to biomass exposure index
In this study, among nonsmoker COPD patients who were exposed to biomass smoke, the severity of disease increased as the biomass exposure index increased. The data were analyzed using one-way ANOVA with Turkey's test and the difference between mean biomass exposure index of any two stage was not found to be significant (P > 0.05), [Table 6 and Figure 2].
Table 6.
Correlation between severity of disease (Global Initiative for Chronic Obstructive Lung Disease stage) and mean biomass exposure index in nonsmoker chronic obstructive pulmonary disease patients
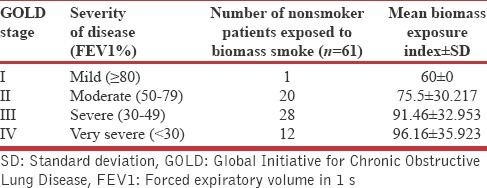
Figure 2.
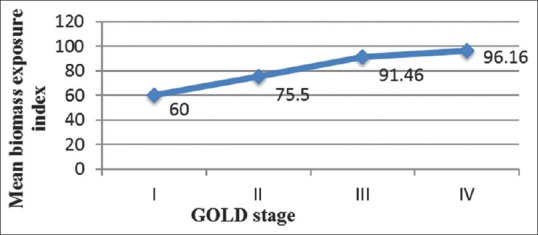
Relationship between severity of disease (Global Initiative for Chronic Obstructive Lung Disease stage) and mean biomass exposure index
DISCUSSION
Proportion of COPD in nonsmokers among all COPD patients in India showed wide variation (9.4–68.6%) in different studies. In this study, proportion of nonsmoker COPD patients among total COPD patients was found to be 56.5%. A similar result was found by Brashier et al.[7] who stated that proportion of COPD patients who never smoked among 12055 participants above 45 years in India was 68.6%. Furthermore, Ehrlich et al.[8] reported that never smokers made up 47.6% of patients with airway obstruction among 13826 adults in South Africa aged more than 18 years. In both studies, a respiratory symptom questionnaire was used to define airway obstruction.
Of total 113 nonsmoker COPD patients, maximum number of patients belong to low socioeconomic status, which appears to be most important risk factor in this group, but it was not found to be statistically significant (P = 0.487). According to GOLD guideline 2015, poverty is a risk factor for COPD but which components of poverty contribute to COPD are not clear. There is strong evidence that the risk of COPD is inversely related to socioeconomic status.
Among total nonsmoker COPD patients, exposure to biomass smoke was most important (53.98%) and statistically significant (P = 0.0001) risk factor for the development of COPD. A similar association has been found by Lindström et al. 2001 in Finland and Sweden.[9] In India, where more than 70% of people use biomass fuel for cooking purposes compared to 25% who smoke, exposure to biomass fuel may be a bigger risk factor for COPD in India.[10]
History of pulmonary tuberculosis was found in 32.74% of nonsmoker COPD patients, which was found to be a statistically significant (P = 0.0001) risk factor for development of COPD. Similar result was also found by Ehrlich et al. 2004 in South Africa[8] because in these countries prevalence of pulmonary tuberculosis is high as in India. In a nationwide survey of 13,826 adults in South Africa, a history of pulmonary tuberculosis was associated with COPD with odds of 4.9 for men and 6.6 for women.[11] The prevalence of airflow obstruction varies from 28% to 68% of patients with treated pulmonary tuberculosis.[12]
Long standing asthma as a risk factor for COPD was found in 14.16% of patients of nonsmoker COPD group, which was statistically significant (P = 0.003) risk factor for the development of COPD. In a report from a longitudinal cohort of the Tuscon epidemiological study of airway obstructive disease, adults with asthma were found to have a twelve-fold higher risk of acquiring COPD over time than those without asthma, after adjusting for smoking.[13] Another longitudinal study of people with asthma found that around 20% of subjects developed irreversible airflow limitation and reduced transfer coefficient.[14]
In this study, history of occupational exposure was present in 9.73% nonsmoker COPD patients, which was not found to be statistically significant (P = 0.687) risk factor for development of COPD. According to American Thoracic Society, occupational exposure account for 10–20% of either symptoms or functional impairment consistent with COPD.[15] Occupational exposure as a risk factor among nonsmoker COPD patients was also found by Lamprecht et al. 2008 in Austria[16] and Ehrlich et al. 2004 in South Africa.[8]
Exposure to outdoor air pollution as a risk factor for COPD in nonsmoker group was found in 3.54% patients, which was not statistically significant (P = 0.610) risk factor for development of COPD. The role of outdoor air pollution in causing COPD is unclear but appears to be small when compared with that of cigarette smoking. Air pollution from fossil fuel combustion, primarily from motor vehicle emissions in cities, is associated with decrements of respiratory function.[17]
History of lower respiratory tract infection during childhood was found in 1.77% of nonsmoker COPD patients, and this was not a statistically significant (P = 0.791) risk factor for development of COPD. According to GOLD guideline 2015, a history of severe childhood respiratory infection has been associated with reduced lung function and increased respiratory symptoms in adulthood.[18,19] Susceptibility to infections plays a role in exacerbations of COPD, but the effect on the development of disease is less clear.
In this study, most of the nonsmoker COPD patients (82, i.e. 72.57%) were exposed to more than 1 risk factor for development of COPD with majority of patients (68, i.e. 60.18%) having 2 risk factors. It was found in the study that patients exposed to 1 risk factor had mean age of 61.32 years, 2 risk factors had mean age of 52.35 years and 3 risk factors had a mean age of 51.93 years. This shows that as the number of risk factors for nonsmoker COPD patients increased, mean age of patients decreased. Hence, if patients are exposed to multiple risk factors responsible for COPD, they tend to develop COPD at an earlier age.
Maximum number of nonsmoker COPD patients (52, i.e., 85.25%) exposed to biomass smoke had biomass exposure index more than sixty with majority of patients (34, i.e., 55.74%) having biomass exposure index between 60 and 100. Mahesh et al.[20] in 2013 in his study in Mysore found that minimum biomass exposure index of sixty was significantly associated with chronic bronchitis. Furthermore, the severity of COPD increased with increase in mean biomass exposure index.
CONCLUSIONS
On the basis of these findings, it can be concluded that nonsmokers contribute a significant proportion of COPD patients. Multiple risk factors other than smoking also play a major role in development of COPD, particularly exposure to biomass smoke, treated pulmonary tuberculosis, and long standing asthma. Other nonsmoking risk factors are occupational exposure, exposure to outdoor air pollution, lower respiratory tract infection during childhood and low socioeconomic status. Further studies are required to explain the involved risk factors and their contributions to this disease to achieve reduction of the burden of COPD in nonsmokers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aziz F, Penupolu S, Xu X, He J. Lung transplant in end-staged chronic obstructive pulmonary disease (COPD) patients: A concise review. J Thorac Dis. 2010;2:111–6. [PMC free article] [PubMed] [Google Scholar]
- 2.van Gestel AJ, Steier J. Autonomic dysfunction in patients with chronic obstructive pulmonary disease (COPD) J Thorac Dis. 2010;2:215–22. doi: 10.3978/j.issn.2072-1439.2010.02.04.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kathiresan G, Jeyaraman SK, Jaganathan J. Effect of upper extremity exercise in people with COPD. J Thorac Dis. 2010;2:223–36. doi: 10.3978/j.issn.2072-1439.2010.11.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global burden of disease study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 5.Tzanakis N, Anagnostopoulou U, Filaditaki V, Christaki P, Siafakas N COPD Group of the Hellenic Thoracic Society. Prevalence of COPD in Greece. Chest. 2004;125:892–900. doi: 10.1378/chest.125.3.892. [DOI] [PubMed] [Google Scholar]
- 6.Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374:733–43. doi: 10.1016/S0140-6736(09)61303-9. [DOI] [PubMed] [Google Scholar]
- 7.Brashier B, Gangavane S, Valsa S, Gaikwad SN, Ghorpade SV, Mandrekar S, et al. 2007. Almost Half the Patients Treated for Pulmonary Tuberculosis (TB) Show Evidence of Obstructive Airways Disease (OAD). European Respiratory Society Annual Congress, Stockholm, Sweden; 15-19 September. [Abstr. E2585] [Google Scholar]
- 8.Ehrlich RI, White N, Norman R, Laubscher R, Steyn K, Lombard C, et al. Predictors of chronic bronchitis in South African adults. Int J Tuberc Lung Dis. 2004;8:369–76. [PubMed] [Google Scholar]
- 9.Lindström M, Kotaniemi J, Jönsson E, Lundbäck B. Smoking, respiratory symptoms, and diseases: A comparative study between Northern Sweden and Northern Finland: Report from the FinEsS study. Chest. 2001;119:852–61. doi: 10.1378/chest.119.3.852. [DOI] [PubMed] [Google Scholar]
- 10.Salvi S, Barnes PJ. Is exposure to biomass smoke the biggest risk factor for COPD globally? Chest. 2010;138:3–6. doi: 10.1378/chest.10-0645. [DOI] [PubMed] [Google Scholar]
- 11.Limaye S, Salvi S. Jindal SK. Textbook of Pulmonary and Critical Care Medicine. 1st ed. New Delhi: Jaypee Publications Pvt Ltd; 2011. Risk factors for COPD; pp. 987–92. [Google Scholar]
- 12.Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med. 1989;83:195–8. doi: 10.1016/s0954-6111(89)80031-9. [DOI] [PubMed] [Google Scholar]
- 13.Silva GE, Sherrill DL, Guerra S, Barbee RA. Asthma as a risk factor for COPD in a longitudinal study. Chest. 2004;126:59–65. doi: 10.1378/chest.126.1.59. [DOI] [PubMed] [Google Scholar]
- 14.Vonk JM, Jongepier H, Panhuysen CI, Schouten JP, Bleecker ER, Postma DS. Risk factors associated with the presence of irreversible airflow limitation and reduced transfer coefficient in patients with asthma after 26 years of follow up. Thorax. 2003;58:322–7. doi: 10.1136/thorax.58.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balmes J, Becklake M, Blanc P, Henneberger P, Kreiss K, Mapp C, et al. American Thoracic Society Statement: Occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167:787–97. doi: 10.1164/rccm.167.5.787. [DOI] [PubMed] [Google Scholar]
- 16.Lamprecht B, Schirnhofer L, Kaiser B, Buist S, Studnicka M. Non-reversible airway obstruction in never smokers: Results from the Austrian BOLD study. Respir Med. 2008;102:1833–8. doi: 10.1016/j.rmed.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Abbey DE, Burchette RJ, Knutsen SF, McDonnell WF, Lebowitz MD, Enright PL. Long-term particulate and other air pollutants and lung function in nonsmokers. Am J Respir Crit Care Med. 1998;158:289–98. doi: 10.1164/ajrccm.158.1.9710101. [DOI] [PubMed] [Google Scholar]
- 18.Barker DJ, Godfrey KM, Fall C, Osmond C, Winter PD, Shaheen SO. Relation of birth weight and childhood respiratory infection to adult lung function and death from chronic obstructive airways disease. BMJ. 1991;303:671–5. doi: 10.1136/bmj.303.6804.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Marco R, Accordini S, Marcon A, Cerveri I, Antó JM, Gislason T, et al. Risk factors for chronic obstructive pulmonary disease in a European cohort of young adults. Am J Respir Crit Care Med. 2011;183:891–7. doi: 10.1164/rccm.201007-1125OC. [DOI] [PubMed] [Google Scholar]
- 20.Mahesh PA, Jayaraj BS, Prabhakar AK, Chaya SK, Vijaysimha R. Identification of a threshold for biomass exposure index for chronic bronchitis in rural women of Mysore district, Karnataka, India. Indian J Med Res. 2013;137:87–94. [PMC free article] [PubMed] [Google Scholar]


