Abstract
Background:
The prevalence of Aspergillus hypersensitivity (AH) and allergic bronchopulmonary aspergillosis (ABPA) has been variably reported. Systematic data regarding Aspergillus sensitization and ABPA are lacking from this part of the country.
Objectives:
The aim of this study was to evaluate the prevalence of AH and ABPA in Uttar Pradesh.
Setting and Design:
This was prospective observational study. All patients attending outpatient Department of Pulmonary Medicine of our institute were included in the study.
Subjects and Methods:
Consecutive asthmatic patients underwent screening for ABPA using Aspergillus skin test (AST). Those showing a positive response to AST were further evaluated for ABPA.
Results:
During the study, 350 patients (192 males, 158 females, mean ± standard deviation age: 38.3 ± 12.8) were screened with AST. One hundred and twenty-three patients (35.1%) were tested positive for AST and 21.7% of patients were diagnosed as ABPA.
Conclusions:
A high prevalence rate of ABPA was observed at our chest clinic. Although comparable with published data from other tertiary centers, it does not represent the true prevalence rates in asthmatics because of high chances of referral bias.
KEY WORDS: Allergic bronchopulmonary aspergillosis, Aspergillus hypersensitivity, bronchial asthma
INTRODUCTION
Bronchial asthma is a global health problem and its prevalence is increasing in various counties including India.[1] In a recent epidemiological study, the prevalence of self-reported asthma was 1.8% among men and 1.9% among women.[2] There is growing concern about the factors leading to the complicated course and poor control of asthma. The presence of hypersensitivity or sensitization to spores of Aspergillus fumigatus is one important factor. Colonization of airways with A. fumigatus leads to IgE sensitization, neutrophilic airway inflammation, and reduced lung function.[3] Aspergillus hypersensitivity (AH), can progress to a complex immunological phenomenon and development of the full syndrome of allergic bronchopulmonary aspergillosis (ABPA). However, only a minority of patients with AH go on to develop the complete clinical picture for ABPA.[4] Allergic aspergillosis is being increasingly reported from India; however, the true community prevalence of ABPA and AH in India still remains unknown. Moreover, systematic data regarding the prevalence of AH/ABPA are sparse from this part of the country. The aim of this study was to describe the prevalence of ABPA in asthmatic patients attending the Chest Clinic of our Institute.
SUBJECTS AND METHODS
Consecutive patients with clinical diagnosis of bronchial asthma being managed in the pulmonary medicine outpatient over 30 months (i.e., from January 2011 to June 2013) were included in the study. The exclusion criteria were pregnancy and the use of systemic corticosteroids for more than 5 days in the preceding 6 weeks. Demographic characteristics were noted and detailed clinical evaluation was performed. All patients underwent chest radiography and spirometry with bronchodilator reversibility. All patients were also screened with Aspergillus skin prick test (AST) and those showing positive response were further evaluated for ABPA.
The Aspergillus skin test was performed using commercially prepared A. fumigatus antigen (Aspergillin; Hollister-Stier Laboratories; Spokane, WA, USA). Type I and III hypersensitivity reactions were recorded as per standard recommendations.[5] Those demonstrating positive type I responses were further investigated with total and A. fumigatus specific IgE levels, peripheral blood eosinophil count and high-resolution computed tomography (HRCT) of the thorax.
The diagnosis of ABPA was made if the patients met the following diagnostic criteria: (a) Bronchial asthma; (b) Type I cutaneous reactivity to A. fumigatus antigen; (c) raised total serum IgE levels (>1000 IU/ml); (d) fleeting or fixed radiological opacities; (e) raised serum IgE specific against A. fumigatus (>0.35 kUA/L); (f) peripheral blood eosinophilia (>1000 cells/ml); and (g) HRCT of thorax showing proximal bronchiectasis.
The levels of serum IgE (total) and IgE (for A. fumigatus) were assayed with commercially available kits using the chemiluminescent enzyme assay (Diagnostic Products Corporation; Los Angeles, CA, USA) and the fluorescent enzyme immunoassay (UniCap Systems; Pharmacia Upjohn; Stockholm, Sweden). Spirometry was done using the ultrasonic transducer based body plethysmography system; Power Cube Body with Diffusion; Ganshorn Medizin Electronic, Germany. Bronchodilator reversibility was assessed after inhalation of 200 µg of salbutamol. The standard diagnostic criteria according to the American Thoracic Society was used.[5]
HRCT scan of the thorax was performed (Brilliance 64 CT Channel Scanner; Philips Healthcare; DA Best, The Netherlands) with a 512-matrix size. The scans were analyzed and radiological abnormalities with specific reference to the presence of central bronchiectasis (CB), nodules, mucus plugging, high-attenuation mucus (HAM), and fibrosis were recorded.
Statistical analysis
Statistical analysis was performed using a statistical software package (SPSS for Microsoft Windows, package version 16; SPSS Inc.; Chicago, IL, USA). The data are presented in a descriptive fashion as the mean standard deviation (SD) or the median (range).
RESULTS
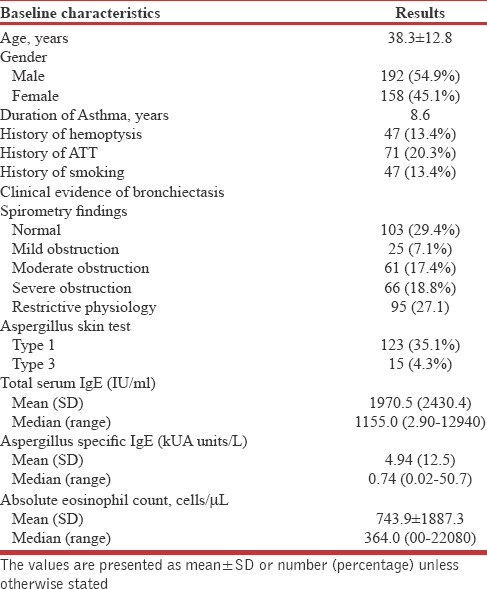
Three hundred and fifty patients with a clinical diagnosis of bronchial asthma were screened during the study. There were 192 males (54.9%) and 158 females (45.1%) in the study population. The mean ± SD age was 38.3 ± 12.8 years. The baseline clinical characteristics are shown in Table 1. The mean duration of asthma was 8.6 years and coexistent history suggestive of allergic rhinitis was elicited in 67% of patients. About 20% of the patients had a history of anti-tubercular treatment intake in the past.
Table 1.
Baseline characteristics of patients screened
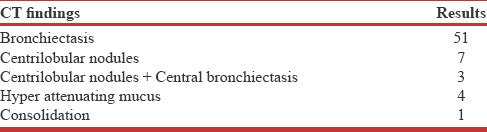
Aspergillus skin test was found to be positive in 123 (35.1%) patients. Of these 76 patients met the criteria for the diagnosis of ABPA. The radiologic findings among the patients diagnosed with ABPA are shown in Table 2.
Table 2.
CT finding among patients diagnosed as ABPA (n=76)
Mean total serum IgE levels were 1970.5 IU/ml and median (range) IgE levels were 1155.0 (2.90–12940). It was observed that mean Aspergillus-specific IgE levels were 4.94 kUA units/L and median (range) specific IgE kUA units/levels were 0.74 (0.02–50.7) kUA/L. These levels were much lower as compared to previous case series. Similarly, mean absolute eosinophil counts were 743.9 per microliter, and the median (range) absolute eosinophil cell count was 364.0 cells (00–22080) per microliter. These values were comparable to published data.
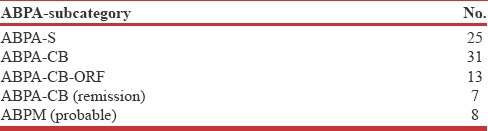
Twenty-five patients had ABPA-serologic (ABPA-S), 31 patients qualified for ABPA-CB and 13 patients had ABPA-other radiologic features (ORF) [Table 3]. Another 7 patients had positive AST, raised specific IgE levels and CB but baseline total IgE levels were within normal limits. Hence, they were classified as ABPA in remission. There were 8 patients who had positive AST, raised total IgE levels and CB, but specific IgE levels were within normal limits. These patients could not be categorized into any particular subgroup, but at best they could be probable ABPM but for confirmation, they would require further evaluation.
Table 3.
Sub classification of patients with diagnosis of ABPA
Some patients had a positive skin test with raised total IgE levels; however, both specific IgE and HRCT were within normal limits. This was an interesting pattern and the most plausible explanation for this was the study population. Isolated raised IgE levels could have been due high prevalence of tropical eosinophilia in this part of the country or due to nonspecific allergy.
Among the patients with isolated AH 14 (29.7%) had moderate to severe obstruction on spirometry. This is a recently described entity termed as severe asthma with fungal sensitization (SAFS).[6] It is characterized by the presence of AH, severe asthma, but without bronchiectasis or other criteria of ABPA. There are limited data on the prevalence of SAFS because this phenotype of asthma has been newly described and its diagnostic criteria are still evolving.
Of the 123 patients with a positive AST 47 patients had normal HRCT scan. The most common radiologic abnormality was CB other radiologic findings were centrilobular nodules, HAM, and consolidation. HAM was seen in only 4 patients (5.26%).
Follow-up data were available for 33 patients only. Of these, thirty patients had a major clinical response to corticosteroid therapy characterized by more 35% fall in total IgE levels at 6 weeks. Three patients had to be initiated on itraconazole therapy due poor response to corticosteroid therapy. The majority of patients had sustained remission at the end of 6 months.
DISCUSSION
The results of our study suggest a high prevalence of ABPA in patients attending the Pulmonary Medicine outpatient of a tertiary care center. Aspergillus is ubiquitous fungal species present in air, soil, vegetation, and fomites.[7] There are more than 250 species of Aspergillus,[8] among which A. fumigatus is the most common pathogens in humans. A. fumigatus is a complex with several species which are named Fumigati. In some individuals airway colonization with A. fumigatus stimulates a T helper Type 2–mediated inflammatory response.[9] ABPA is a result of a similar hypersensitivity phenomenon seen in patients with bronchial asthma and cystic fibrosis.[7,10,11,12,13,14,15,16,17]
In this study, the prevalence of AH and ABPA was 35.1% and 21.7%, respectively. Traditionally, the prevalence of ABPA is believed to be 1–2% in patients with asthma and 2–15% in patients with cystic fibrosis (CF).[17] The condition is being increasingly recognized and the estimated prevalence rates in recent publications have been reported ranging from 5.9% to 20.5% for ABPA and 38–43% for AH.[18,19] Prevalence data from this part of the country are sparse. Prasad et al. reported a prevalence of 30.3% for AH and 7.4% for ABPA in a recent study. Although the prevalence of AH was comparable ABPA was much more common in this study as compared to the study by Prasad et al.[20] The true population prevalence of AH and ABPA remains unknown, but high prevalence rates have been reported from dedicated pulmonary medicine clinics. Higher prevalence rates in these studies are probably a reflection of referral bias as most of these studies are from tertiary care settings. In a recently published systematic review and meta-analysis which included 20 studies, a prevalence of 15–48% for AH was demonstrated.[21]
We observed significantly lower levels of total and Aspergillus-specific IgE in our study. This may represent lower environmental concentrations of fungal antigens in this part of the country which will consequently lead to weaker immune sensitization and subsequent weak immune response.
HAM is considered almost pathognomonic of ABPA and has been variably reported in literature ranging 15–25%. In this study, only 4 patients had HAM reason for which is speculative. The presence of HAM has been linked to stronger inflammatory response and also associated with recurrent relapses.[19] It has been hypothesized that mucus impaction and formation of high-density mucus has some genetic predisposition, and this may be one of the reasons of lower occurrence of HAM in our study.
Isolated AH without ABPA was present in 47 patients. A. fumigatus associated asthma (AFAA) is a term used to describe these patients. Aspergillus sensitization (AS) has been linked to poor lung function, however, a causal relationship has not been established.[3] In another study, a weak association between AS and severity of asthma has been demonstrated. In this study, individuals sensitized to Aspergillus had significantly lower forced expiratory volume in the first second (FEV1) and FEV1 to forced vital capacity ratio. It was also seen that patients without sensitization to Aspergillus had better control in comparison to those with AFAA.[22] Whether airflow limitation is a consequence of colonization or colonization occurs in those with preexisting airflow obstruction is not known. Patients with AFAA should be followed up closely and long-term longitudinal studies need to be performed to observe the clinical behavior of these patients. Among the patient with isolated AH, we found about 30% prevalence of SAFS, overall prevalence being 4%. Although there are sparse data on the prevalence of SAFS it being a under-recognized entity, our prevalence rates were comparable to previous reports. The proposed diagnostic criteria for the diagnosis of SAFS are the presence of “severe asthma”, evidence of fungal sensitization, exclusion of ABPA. Although there are specific guidelines from the American Thoracic Society to define “severe” uncontrolled asthma,[23] we took the presence of moderate to severe obstruction on spirometry as a surrogate of severe asthma. There is an important connotation for correct recognition of SAFS because this subgroup of patient requires close follow-up and the potential role of anti-IgE therapy and antifungals in its treatment are being explored.
The diagnostic criteria for ABPA had been a subject of debate and the method of screening patients with asthma also has evolved overtime. This is the reason for variable prevalence rates of AH and ABPA reported in the literature. Aspergillus skin test had been used for screening the patients with bronchial asthma for AH and ABPA till Agarwal et al. in 2013[24] proposed that specific IgE for A. fumigatus should be screening modality of choice in their revised diagnostic criteria. Although estimation of specific IgE against A. fumigatus is more sensitive[25] and its use for screening is justified, it is also possible that patients colonized with other Aspergillus spp. might be overlooked leading to underdiagnosis. Furthermore, it is prudent to note that 40% of patients with asthma can have AH without ABPA.
ABPA has been classified by Kumar into ABPA-S; ABPA-CB; and ABPA-CB-ORF based on the serologic and radiologic findings.[26] In this study, 25 patients had ABPA-S, 31 patients had ABPA-CB and 13 patients had ABPA-ORF but in the recent consensus conference of International Society for Human and Animal Mycology working group for the ABPA complicating asthma has re-classified ABPA into four categories viz., ABPA-S, ABPA with bronchiectasis, ABPA-HAM, and ABPA with chronic pleuropulmonary fibrosis.[24] The new classification has got prognostic implications and is based on the severity of immunological response. The presence of HAM in ABPA is associated with recurrent relapses and signifies a stronger immunological response to antigen exposure.[19] We had only 4 patients with ABPA-HAM, and this may be refection of lower environmental fungal bioload in this part of the country. None of the patients in our study had pleural involvement.
There was a good clinical response to corticosteroid therapy in most of our patients, and they had sustained remission at the end of 6 months. Long-term follow-up data were not available. Oral glucocorticoids are currently the treatment of choice for ABPA;[7,27] however, there is no consensus about the dose and duration of therapy. In patients poorly responding to systemic corticosteroid therapy oral azoles have been used with reasonable efficacy. Among azoles oral itraconazole has been most common agent evaluated and has shown to be effective steroid dependent ABPA.[28,29]
CONCLUSIONS
The prevalence of AH and ABPA in patients with bronchial asthma in our study were comparable to the rates previously published in the literature. Although routine screening for ABPA in patients with asthma is not recommended in field setting a high index of suspicion should be kept while evaluating patients with bronchial asthma. The diagnostic criteria of ABPA are still evolving, and there are several unresolved issues in its classification and management. There is need of large longitudinal studies from different areas to study the clinical behavior of these patients with specific reference to remission criteria and incidence of progression of AH patients to ABPA.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jindal SK, Aggarwal AN, Gupta D, Agarwal R, Kumar R, Kaur T, et al. Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH) Int J Tuberc Lung Dis. 2012;16:1270–7. doi: 10.5588/ijtld.12.0005. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal S, Pearce N, Ebrahim S. Prevalence and risk factors for self-reported asthma in an adult Indian population: A cross-sectional survey. Int J Tuberc Lung Dis. 2013;17:275–82. doi: 10.5588/ijtld.12.0438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fairs A, Agbetile J, Hargadon B, Bourne M, Monteiro WR, Brightling CE, et al. IgE sensitization to Aspergillus fumigatus is associated with reduced lung function in asthma. Am J Respir Crit Care Med. 2010;182:1362–8. doi: 10.1164/rccm.201001-0087OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bateman ED. A new look at the natural history of Aspergillus hypersensitivity in asthmatics. Respir Med. 1994;88:325–7. doi: 10.1016/0954-6111(94)90035-3. [DOI] [PubMed] [Google Scholar]
- 5.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 6.Denning DW, O’Driscoll BR, Hogaboam CM, Bowyer P, Niven RM. The link between fungi and severe asthma: A summary of the evidence. Eur Respir J. 2006;27:615–26. doi: 10.1183/09031936.06.00074705. [DOI] [PubMed] [Google Scholar]
- 7.Greenberger PA. Allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 2002;110:685–92. doi: 10.1067/mai.2002.130179. [DOI] [PubMed] [Google Scholar]
- 8.Geiser DM, Klich MA, Frisvad JC, Peterson SW, Varga J, Samson RA. The current status of species recognition and identification in Aspergillus. Stud Mycol. 2007;59:1–10. doi: 10.3114/sim.2007.59.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tillie-Leblond I, Tonnel AB. Allergic bronchopulmonary aspergillosis. Allergy. 2005;60:1004–13. doi: 10.1111/j.1398-9995.2005.00887.x. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg M, Patterson R, Mintzer R, Cooper BJ, Roberts M, Harris KE. Clinical and immunologic criteria for the diagnosis of allergic bronchopulmonary aspergillosis. Ann Intern Med. 1977;86:405–14. doi: 10.7326/0003-4819-86-4-405. [DOI] [PubMed] [Google Scholar]
- 11.Greenberger PA, Patterson R, Ghory A, Arkins JA, Walsh T, Graves T, et al. Late sequelae of allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 1980;66:327–35. doi: 10.1016/0091-6749(80)90029-9. [DOI] [PubMed] [Google Scholar]
- 12.Patterson R, Greenberger PA, Radin RC, Roberts M. Allergic bronchopulmonary aspergillosis: Staging as an aid to management. Ann Intern Med. 1982;96:286–91. doi: 10.7326/0003-4819-96-3-286. [DOI] [PubMed] [Google Scholar]
- 13.Patterson R, Greenberger PA, Halwig JM, Liotta JL, Roberts M. Allergic bronchopulmonary aspergillosis. Natural history and classification of early disease by serologic and roentgenographic studies. Arch Intern Med. 1986;146:916–8. doi: 10.1001/archinte.146.5.916. [DOI] [PubMed] [Google Scholar]
- 14.Patterson R, Greenberger PA, Lee TM, Liotta JL, O’Neill EA, Roberts M, et al. Prolonged evaluation of patients with corticosteroid-dependent asthma stage of allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 1987;80:663–8. doi: 10.1016/0091-6749(87)90285-5. [DOI] [PubMed] [Google Scholar]
- 15.Greenberger PA. Allergic bronchopulmonary aspergillosis and fungoses. Clin Chest Med. 1988;9:599–608. [PubMed] [Google Scholar]
- 16.Greenberger PA, Miller TP, Roberts M, Smith LL. Allergic bronchopulmonary aspergillosis in patients with and without evidence of bronchiectasis. Ann Allergy. 1993;70:333–8. [PubMed] [Google Scholar]
- 17.Greenberger PA. Clinical aspects of allergic bronchopulmonary aspergillosis. Front Biosci. 2003;8:s119–27. doi: 10.2741/943. [DOI] [PubMed] [Google Scholar]
- 18.Attapattu MC. Allergic bronchopulmonary aspergillosis in a chronic asthmatic. Ceylon Med J. 1983;28:251–3. [PubMed] [Google Scholar]
- 19.Agarwal R, Gupta D, Aggarwal AN, Saxena AK, Chakrabarti A, Jindal SK. Clinical significance of hyperattenuating mucoid impaction in allergic bronchopulmonary aspergillosis: An analysis of 155 patients. Chest. 2007;132:1183–90. doi: 10.1378/chest.07-0808. [DOI] [PubMed] [Google Scholar]
- 20.Prasad R, Garg R, Sanjay, Dixit RP. A study on prevalence of allergic bronchopulmonary aspergillosis in patients of bronchial asthma. Internet J Pulm Med. 2007;9:1–6. [Google Scholar]
- 21.Agarwal R, Aggarwal AN, Gupta D, Jindal SK. Aspergillus hypersensitivity and allergic bronchopulmonary aspergillosis in patients with bronchial asthma: Systematic review and meta-analysis. Int J Tuberc Lung Dis. 2009;13:936–44. [PubMed] [Google Scholar]
- 22.Agarwal R, Noel V, Aggarwal AN, Gupta D, Chakrabarti A. Clinical significance of Aspergillus sensitisation in bronchial asthma. Mycoses. 2011;54:e531–8. doi: 10.1111/j.1439-0507.2010.01971.x. [DOI] [PubMed] [Google Scholar]
- 23.Proceedings of the ATS workshop on refractory asthma: Current understanding, recommendations, and unanswered questions. American Thoracic Society. Am J Respir Crit Care Med. 2000;162:2341–51. doi: 10.1164/ajrccm.162.6.ats9-00. [DOI] [PubMed] [Google Scholar]
- 24.Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, et al. Allergic bronchopulmonary aspergillosis: Review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013;43:850–73. doi: 10.1111/cea.12141. [DOI] [PubMed] [Google Scholar]
- 25.Agarwal R, Maskey D, Aggarwal AN, Saikia B, Garg M, Gupta D, et al. Diagnostic performance of various tests and criteria employed in allergic bronchopulmonary aspergillosis: A latent class analysis. PLoS One. 2013;8:e61105. doi: 10.1371/journal.pone.0061105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumar R. Mild, moderate, and severe forms of allergic bronchopulmonary aspergillosis: A clinical and serologic evaluation. Chest. 2003;124:890–2. doi: 10.1378/chest.124.3.890. [DOI] [PubMed] [Google Scholar]
- 27.Vlahakis NE, Aksamit TR. Diagnosis and treatment of allergic bronchopulmonary aspergillosis. Mayo Clin Proc. 2001;76:930–8. doi: 10.4065/76.9.930. [DOI] [PubMed] [Google Scholar]
- 28.Wark PA, Hensley MJ, Saltos N, Boyle MJ, Toneguzzi RC, Epid GD, et al. Anti-inflammatory effect of itraconazole in stable allergic bronchopulmonary aspergillosis: A randomized controlled trial. J Allergy Clin Immunol. 2003;111:952–7. doi: 10.1067/mai.2003.1388. [DOI] [PubMed] [Google Scholar]
- 29.Stevens DA, Schwartz HJ, Lee JY, Moskovitz BL, Jerome DC, Catanzaro A, et al. A randomized trial of itraconazole in allergic bronchopulmonary aspergillosis. N Engl J Med. 2000;342:756–62. doi: 10.1056/NEJM200003163421102. [DOI] [PubMed] [Google Scholar]


