Abstract
Objective
We aimed to evaluate the association between breast arterial calcification (BAC) and carotid plaque formation.
Materials and Methods
The study group comprised 47 consecutive BAC (+) women, whereas the control group comprised 33 BAC (−) women (total, 80 women). All mammograms were examined by a specialist without being any apartheid that it was come from central or not. For the exist and density of calcification was used classification method. When we evaluate carotid arterial plaque with Doppler US used scale method. For analyzing categorical variables, we used chi-square test, and for numeric variables, we used independent t-test.
Results
As nearly all BAC+ women had all types of carotid plaques, weighted of them was found that they were fatty plaque type (n=13 %46.4). Only one BAC+ patient was grade 2 and had no carotid plaques (n=1 %3.6). MAK– patients had nearly no plaque types.
Conclusion
Breast cancer mammographic evaluation is an already important, cheap, and simple imaging method. In our study, we report a similar cheap, simple method that can be useful for evaluating atherothrombotic atherosclerosis, which is the most important cause of ischemic infarct.
Keywords: Doppler ultrasonography, vascular calcification, arteries, peripheral arterial disease, breast
Introduction
Mammography is critical for early detection and characterization of breast disease. Obtaining information on extra-mammarian diseases with this modality and reducing the risk of future diseases are at least as important as early detection of breast cancer. It will be beneficial if several mammography signs can be identified to be related to ischemic stroke, which is associated with high morbidity and mortality rates. A correlation between calcification types detected on mammograms and atherothrombotic events, which are the main source of ischemic stroke and can originate from carotid plaques, can provide such information.
The objective of our study was to assess the correlation of breast arterial calcifications (BAC) on mammography with carotid plaque forms detected by color Doppler ultrasound.
Materials and Methods
80 women including 47 with arterial calcifications on mammograms and 33 control patients without arterial calcification (47 BAC + study group, 33 BAC− control group) were included in the study. Informed consents were obtained. Ethics committee approval was not obtained. Female patients aged 39–86 years and who applied for screening or diagnostic mammography were enrolled in the study. Those above or below the specified age limit, with a previous history of stroke, transient ischemic or coronary artery disease, those who did not give consent, pregnant patients and those with infection or chronic inflammatory diseases such as autoimmune diseases, hepatic and/or renal failure were excluded from the study. Inclusion and exclusion criteria were applied for both groups. Mammograms were analyzed under supervision of a specialist for presence of BAC, whether they were performed at another center or our hospital. Mammograms that have been previously performed in other centers were evaluated in mediolateral oblique position with a standard negatoscope. There were 22 mammograms obtained in other centers; 15 of them had a 100% magnification, while 7 were reduced in the range of 70–85% due to the large breast size.
The mammograms in our hospital were obtained in the mediolateral and oblique views with Siemens Mammomat 3000® digital device. Digital mammography was assessed at Totoku 21.3″ dual display at 5 megapixel resolution. There was no significant difference between analog and digital assessment. The presence and intensity of calcifications were graded as follows: 0 (None): no vascular calcification; 1 (mild): minimal calcification with distances greater than 10 mm between calcified areas; 2 (moderate): clearly detectable calcifications in most part of the arteries; and 3 (severe): diffuse calcification affecting most of the arteries detected in at least two branches in the form of a continuous column. The intensity of calcification was analyzed independently of the number of calcified vessels. Doppler evaluation was performed with 7–13 MHz multifrequency linear probe. (EUB 6500; Hitachi, Tokyo, Japan and Aplio 500; Toshiba, Tokyo, Japan). A single radiologist performed mammographic and sonographic evaluations. Doppler assessment of carotid artery plaques was classified according to the method by Gray-Weale et al (1). Plaque types were divided into three categories as Type 1; fatty homogeneous and anechoic plaque, Type 2; mixed plaque, and Type 3; calcified plaques. The plaque-free groups were considered as type 0, regardless of the classification. In our study, the BAC+ and control groups were compared in terms of differences in the mean blood glucose level, number of births, presence of diabetes mellitus and hypertension.
Statistical analysis
SPSS 20.0 for Windows IBM Virginia USA statistical software was used for analysis. Chi-square test was used for comparison of categorical variables between groups, and independent t-test was used for numeric variables. In addition, logistic regression analysis was used to estimate the status of a binary variable. The p significance was set at 5%.
Results
The age of our patients ranged from 39–86 years. The mean age of 47 BAC + female patients and 33 BAC− female patients was 59.12±8.62 and 50.06±7.88, respectively (p>0.05).
The most common calcification types in BAC + cases was grade 2 breast arterial calcification (n = 15 50%) (Table 1).
Table 1.
BAC (+,−) Breast arterial calcification classification
| Group | ||||
|---|---|---|---|---|
| BAC+ | BAC− | Total | ||
| Breast arterial calcification | None | 0 | 32 | 32 |
| 0.0% | 100.0% | 53.3% | ||
| Grade 1 | 4 | 0 | 4 | |
| 14.3% | 0.0% | 6.7% | ||
| Grade 2 | 14 | 0 | 14 | |
| 50.0% | 0.0% | 23.3% | ||
| Grade 3 | 8 | 0 | 8 | |
| 28.6% | 0.0% | 13.3% | ||
| Grade 4 | 2 | 0 | 2 | |
| 7.1% | 0.0% | 3.3% | ||
| Total | 28 | 32 | 60 | |
| 100.0% | 100.0% | 100.0% | ||
BAC: Breast arterial calcification
Twenty-seven of BAC + patients had carotid plaque types, 13 of which were fatty plaque type (n=13, 46.4%). Only one patient with grade 2 BAC+ (n=1, 3.6%) had no detectable carotid plaque formation. In BAC− cases, the total number of those without plaque formation was 25 (78.1%) while fatty plaque formation was observed in six patients (18.8%) (Table 2). It was detected that the number of fatty plaques at risk for thrombosis was significantly higher in patients with Grade 2 BAC+ (Table 3).
Table 2.
Carotid plaque and BAC (+,−) group cross-table
| BAC+ | BAC− | Total | ||
|---|---|---|---|---|
| Carotid plaque | none | 1 | 25 | 26 |
| 3.6% | 78.1% | 43.3% | ||
| fatty | 13 | 6 | 19 | |
| 46.4% | 18.8% | 31.7% | ||
| calcified | 6 | 1 | 7 | |
| 21.4% | 3.1% | 11.7% | ||
| mixed | 8 | 0 | 8 | |
| 28.6% | 0.0% | 13.3% | ||
| Total | 28 | 32 | 60 | |
| 100.0% | 100.0% | 100.0% |
BAC: Breast arterial calcification
Table 3.
Breast arterial calcification and carotid plaque cross-table
| Carotid plaque | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| none | fatty | calcified | mixed | Total | ||
| Breast arterial calcification | Grade | 1 | 1 | 6 | 1 | 0 |
| Grade 2 | 1 | 18 | 1 | 6 | 26 | |
| Grade 3 | 0 | 2 | 3 | 3 | 8 | |
| Grade 4 | 0 | 0 | 4 | 1 | 5 | |
| Total | 2 | 26 | 9 | 10 | 47 | |
According to the partial regression analysis on the effects of breast calcifications on the frequency and type of atheroma plaques regardless of age, the −2 log likelihood was calculated as 57.72 and R square as 60,6%. We found that the presence of carotid plaque could be detected in 60.6% of BAC + and − cases (Table 4). According to our cross-table, the BAC classification that we have used to assess the presence of carotid plaque regardless of age correctly identified 25 out of 27 patients without carotid plaque, while detecting only eight patients with plaques. The general accuracy rate of the classification was 86.7% (Table 5). At the significance level, the presence of a carotid plaque was found to be 22.9 times higher in those with breast arterial calcification. This finding indicates the frequency of carotid plaque in BAC + patients as compared to BAC− cases (p<0.05) (Table 6).
Table 4.
Logistic regression analysis for BAC and carotid plaque
| Step | −2 Log likelihood | Cox & Snell R Square | Nagelkerke R Square |
|---|---|---|---|
| 1 | 57.722* | 0.452 | 0.606 |
Estimation terminated at iteration number 6 because parameter estimates changed by less than 0.001.
Table 5.
Frequency of plaques in BAC+ and BAC− groups
| Classification Table* | ||||
|---|---|---|---|---|
| Detected | ||||
|
|
||||
| Observed | Max+ | Percent frequency | ||
| 0.00 | 1.00 | |||
| Max− | .00 | 25 | 8 | 75.8 |
| 1.00 | 2 | 40 | 95.2 | |
| Total percent | 86.7 | |||
The cut value is 0.500
BAC: Breast arterial calcification
Table 6.
Comparison of age, gender, blood glucose and number of births between groups
| Group statistics | |||||
|---|---|---|---|---|---|
| Group | Number | Mean | Std. Deviation | Std. Med. Err. | |
| Age | BAC+ | 47 | 59.1277 | 8.62155 | 1.25758 |
| BAC− | 33 | 50.0606 | 7.88170 | 1.37203 | |
| Gender | BAC+ | 47 | 1.0000 | 0.00000a | 0.00000 |
| BAC− | 33 | 1.0000 | 0.00000a | 0.00000 | |
| Blood glucose | BAC+ | 47 | 121.8085 | 31.98956 | 4.66616 |
| BAC− | 33 | 97.2121 | 20.14131 | 3.50615 | |
| NB | BAC+ | 47 | 3.3191 | 1.40041 | 0.20427 |
| BAC− | 33 | 2.3939 | 1.27327 | 0.22165 | |
BAC: Breast arterial calcification; a: iki grup arasındaki standart deviasyon farkı hesaplanmadı.
The number of hypertensive patients was higher in the BAC + group (n=32, 86.5%) as compared to BAC− cases (n=5 13.5%) (p<0.05) (Table 9) (Figure 1). Similarly, the presence of diabetes mellitus was significantly higher in BAC + patients than BAC− cases (p<0.05) (Table 10) (Figure 2).
Table 9.
Hypertension and Groups cross-table
| Hypertension ve Group Cross Table | |||||
|---|---|---|---|---|---|
| Group | |||||
|
|
|||||
| BAC+ | BAC− | Total | |||
| present | Number | 32 | 5 | 37 | |
| Hypertension | % | 86.5% | 13.5% | 100.0% | |
| none | Number | 15 | 28 | 43 | |
| % | 34.9% | 65.1% | 100.0% | ||
| Total | Number | 47 | 33 | 80 | |
| % | 58.8% | 41.2% | 100.0% | ||
Figure 1.
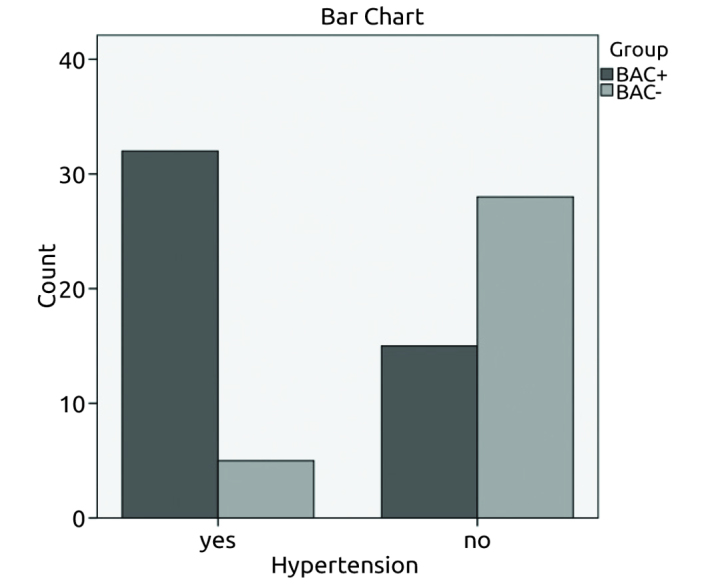
The frequency of hypertension in both groups
Table 10.
Presence of Diabetes and Groups cross table
| Diabetes ve Group cross table | |||||
|---|---|---|---|---|---|
| Group | |||||
|
|
|||||
| BAC+ | BAC− | Total | |||
| present | Number | 30 | 7 | 37 | |
| Diabetes | %Diabetes | 81.1% | 18.9% | 100.0% | |
| none | Number | 17 | 26 | 43 | |
| %Diabetes | 39.5% | 60.5% | 100.0% | ||
| Total | Number | 47 | 33 | 80 | |
| %Diabetes | 58.8% | 41.2% | 100.0% | ||
BAC: Breast arterial calcification
Figure 2.
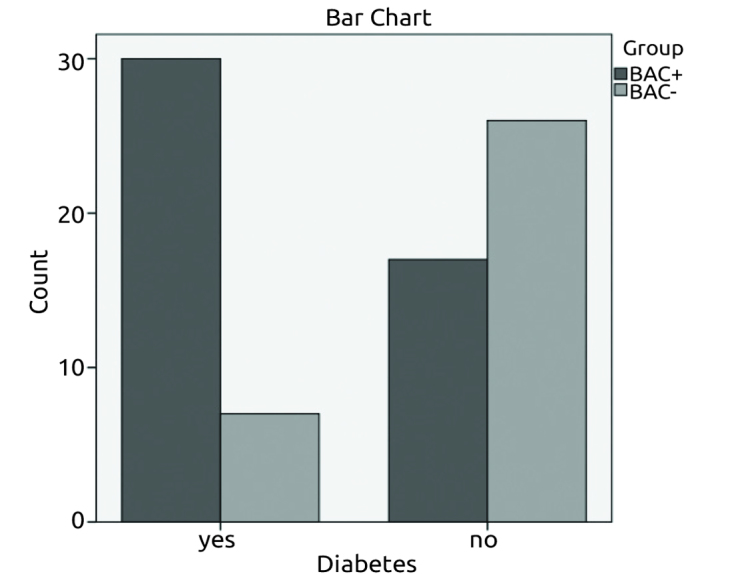
The frequency of diabetes in both groups
The mean blood glucose level in BAC + and − patients was 121.80±31.98 and 97.21±20.14, respectively (p<0.05). The number of births was 3.31±1.4 in BAC + patients, and 2.39±1.27 in BAC− patients (p>0.05) (Table 7). There was a statistically significant difference between the two groups in terms of number of birth (p<0.05). However, a significant correlation was not detected between an increased in the number of births and degree of calcification in the intra-group assessment of BAC + patients (p>0.05) (Table 8) (Figure 3).
Table 7.
Frequency of carotid plaque in BAC+ cases
| B | S.E. | Wald | df | Sig. | Exp(B) | ||
|---|---|---|---|---|---|---|---|
| Step 1* | CP | 3.132 | .702 | 19.895 | 1 | .000 | 22.927 |
| Constant | −2.120 | .609 | 12.104 | 1 | .001 | .120 |
Variable (s) entered on step 1:
BAC: Breast arterial calcification; CP: Carotid plaque; Sig: significance; Exp: exponential; df: degrees of freedom; SE: standard error; B: constant coefficient
Table 8.
Number of births and breast arterial calcification cross-table
| Breast arterial calcification | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | Total | |||
| NB | 1.00 | Number | 1 | 2 | 0 | 1 | 4 |
| % DS | 25.0% | 50.0% | 0.0% | 25.0% | 100.0% | ||
| 2.00 | Number | 1 | 6 | 2 | 1 | 10 | |
| % DS | 10.0% | 60.0% | 20.0% | 10.0% | 100.0% | ||
| 3.00 | Number | 2 | 10 | 1 | 1 | 14 | |
| % DS | 14.3% | 71.4% | 7.1% | 7.1% | 100.0% | ||
| 4.00 | Number | 1 | 6 | 2 | 0 | 9 | |
| % DS | 11.1% | 66.7% | 22.2% | 0.0% | 100.0% | ||
| 5.00 | Number | 3 | 1 | 1 | 1 | 6 | |
| % DS | 50.0% | 16.7% | 16.7% | 16.7% | 100.0% | ||
| 6.00 | Number | 0 | 1 | 2 | 1 | 4 | |
| % DS | 0.0% | 25.0% | 50.0% | 25.0% | 100.0% | ||
| Total | Number | 8 | 26 | 8 | 5 | 47 | |
| % DS | 17.0% | 55.3% | 17.0% | 10.6% | 100.0% | ||
NB: number of births
Figure 3.
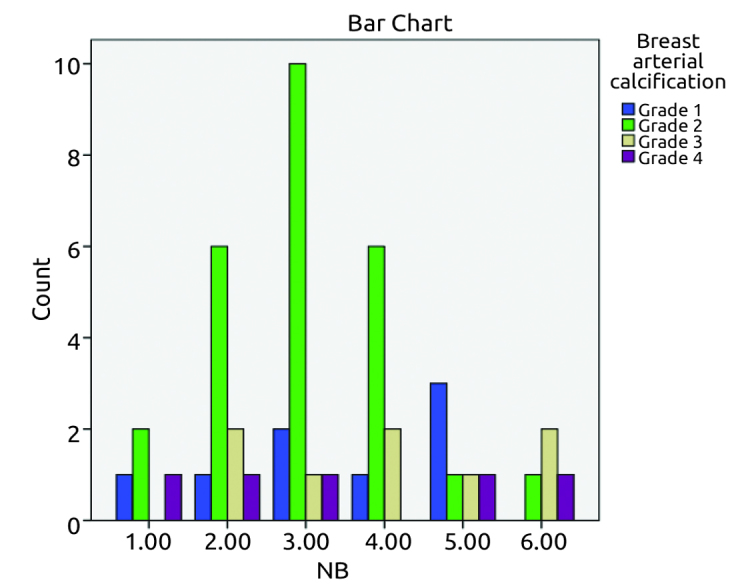
The frequency of number of births in BAC+ cases
Discussion and Conclusions
Cardiovascular diseases are associated with systemic arterial diseases. Arterial calcification is an indicator for atherosclerotic and accompanying cardiovascular diseases that may occur in the future (2).
Although there are many studies emphasizing the correlation of BAC with cardiovascular diseases, there are no studies showing an association between carotid plaque type and presence of BAC on mammography. The correlation between plaque morphology types and BAC types were especially emphasized in our study.
Arterial calcification is classified into two groups according to its location in the intimal or medial layer. Arterial intimal calcifications are in the form of wide, irregular and intermittent calcium deposits. On the other hand, medial calcifications are smooth, granular, and circumferential. Intimal calcification occurs in large muscular and elastic arteries, while medial calcification occurs in smaller muscular arteries (Mönckeberg medial calcific sclerosis) (3). The medial type is often seen in extremity arteries. This calcification type can be detected in the breast by its typical image. They appear in the shape of a ‘railroad track’ with linear parallel calcifications (4). Mönckeberg’s medial calcific sclerosis was defined in diabetes and end-stage renal patients (5, 6). Intimal calcifications are components of atherosclerotic disease, while medial calcification is part of the aging process (3, 6, 7). Different methods are used in the evaluation of BAC. Various studies have suggested numerical classifications (3, 8). Several researchers have used visual scoring methods as in our study (9, 10). Although computer-aided programs that can be used as more quantitative methods are currently available, these methods are relatively new with limited study results. In our study, the mean blood glucose level and incidence of diabetes mellitus were significantly higher in BAC+ patients as compared to BAC− cases. These findings were consistent with other studies (11, 12). In accordance with another study, presence of hypertension was significantly higher as an independent factor in BAC+ patients as compared to BAC− cases (13).
In addition, there was a significant and independent correlation between the number of births and BAC +. However, a significant correlation was not detected between an increased in the number of births and degree of calcification in the intra-group assessment of BAC + patients (Table 8, Figure 3). Sedighi et al. (7) reported similar findings, although they did not report the intra-group correlation data (8).
In our study, the presence of carotid plaque was significantly higher in BAC+ group as compared to BAC− patients. Sedighi et al. (7) similarly reported a positive correlation between the presence of plaques and BAC. However, there was no information on the correlation between plaque types (7–16).
In our study, it was noticed that the plaque types at risk for future neurovascular disease such as fatty plaque were especially detected in Grade 2 BAC+ patients, and that the age of this group was younger as compared to patients with Grade 4 BAC + cases (Table 11).
Table 11.
Age *Carotid plaque *Breast arterial calcification cross-table
| Carotid plaque | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Breast arterial calcification | none | fatty | calcified | mixed | Total | |
| Grade 1 | Age between 43–66 | 1 | 6 | 1 | 8 | |
| Grade 2 | Age between 45–86 | 1 | 18 | 1 | 6 | 26 |
| Grade 3 | Age between 48–72 | 2 | 3 | 3 | 8 | |
| Grade 4 | Age between 67–91 | 4 | 1 | 5 | ||
Different from our study, a prospective study on young adults reported that increased carotid intima-media thickness (c-IMT), which is an early stage of carotid plaque, is associated with coronary artery calcification and cardiovascular disease that may develop in the future (11–14). Intimal changes may reflect cardiovascular and neurovascular diseases. While a number of studies analyzed the correlation between cardiovascular disease and BAC, studies on the association of BAC and carotid plaque are very rare (7–16).
Similar to other studies, the frequency of hypertension and diabetes were significantly higher in the study group as compared to the control group, as well as blood glucose levels (8, 9). Our findings also indicated that the presence of Grade 2 BAC on mammography could be used as a marker for the presence of early atherosclerosis (Table 3).
One of the limitations of this study is relying on patient’s verbal statements for various data (hypertension, pregnancy, etc.) rather than objective criteria or measurements. Other limiting factors include the small sample size and inclusion of mammograms from other centers therefore lack of standardization in imaging. In addition to these, the radiologist who evaluated Doppler US was not blinded to mammography results.
Mammography is already an important, cheap and simple screening method for breast cancer. In our study, we found that such an inexpensive and straightforward method may provide helpful information for women on the presence of carotid plaques, which is one of the main reasons of ischemic stroke.
Footnotes
Ethic Committee Approval: Ethics committee approval was not received due to the retrospective nature of this study.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externallypeer-reviewed.
Conflict of Interest: No conflict of interest was declared by the author.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Gray W, Rumack CM, Wilson SR, Charboneau JW. Diagnostic Ultrasound. Second Edition. New York: Mosby; 1998. pp. 885–891. [Google Scholar]
- 2.Kataoka M, Warren R, Luben R, Camus J, Denton E, Sala E, Day N, Khaw KT. How predictive is breast arterial calcification of cardiovascular disease and risk factors when found at screening mammography? AJR. 2006;187:73–80. doi: 10.2214/AJR.05.0365. http://dx.doi.org/10.2214/AJR.05.0365. [DOI] [PubMed] [Google Scholar]
- 3.Rotter MA, Schnatz PF, Currier AA, Jr, O’Sullivan DM. Breast arterial calcifications (BACs) found on screening mammography and their association with cardiovascular disease. Menopause. 2008;15:276–281. doi: 10.1097/gme.0b013e3181405d0a. http://dx.doi.org/10.1097/gme.0b013e3181405d0a. [DOI] [PubMed] [Google Scholar]
- 4.Taşkın F, Akdilli A, Karaman C, Unsal A, Koseoğlu K, Ergin F. Mammographically detected breast arterial calcifications: Indicators for arteriosclerotic diseases? Eur J Radiol. 2006;60:250–255. doi: 10.1016/j.ejrad.2006.06.006. http://dx.doi.org/10.1016/j.ejrad.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Sickles EA, Galvin HB. Breast Arterial Calcification in Association with Diabetes Mellitus: Too Weak a Correlation to Have Clinical Utility. Radiology. 1985;155:577–579. doi: 10.1148/radiology.155.3.4001355. http://dx.doi.org/10.1148/radiology.155.3.4001355. [DOI] [PubMed] [Google Scholar]
- 6.Duhn V, D’Orsi ET, Johnson S, D’Orsi CJ, Adams AL, O’Neill WC. Breast arterial calcification: a marker of medial vascular calcification in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:377–382. doi: 10.2215/CJN.07190810. http://dx.doi.org/10.2215/CJN.07190810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sedighi N, Radmard AR, Radmehr A, Hashemi P, Hajizadeh A, Taheri AP. Breast arterial calcification and risk of carotid atherosclerosis: focusing on the preferentially affected layer of the vessel wall. Eur J Radiol. 2011;79:250–256. doi: 10.1016/j.ejrad.2010.04.007. http://dx.doi.org/10.1016/j.ejrad.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Kataoka M, Warren R, Luben R, Camus J, Denton E, Sala E, Day N, Khaw KT. How predictive is breast arterial calcification of cardiovascular disease and risk factors when found at screening mammography? AJR. 2006;187:73–80. doi: 10.2214/AJR.05.0365. http://dx.doi.org/10.2214/AJR.05.0365. [DOI] [PubMed] [Google Scholar]
- 9.Maas AH, van der Schouw YT, Mali WP, van der Graaf Y. Prevalence and determinants of breast arterial calcium in women at high risk of cardiovascular disease. Am J Cardiol. 2004;94:655–659. doi: 10.1016/j.amjcard.2004.05.036. http://dx.doi.org/10.1016/j.amjcard.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 10.Erdoğmuş B, Buyukkaya R, Buyukkaya A, Yazıcı B. Relationship between breast arterial calcifications detected on mammography and brachial artery intima-media thickness. Wien Klin Wochenschr. 2013;125:100–104. doi: 10.1007/s00508-013-0322-6. http://dx.doi.org/10.1007/s00508-013-0322-6. [DOI] [PubMed] [Google Scholar]
- 11.Davis PH, Dawson JD, Mahoney LT, Lauer RM. Increased carotid intimal-medial thickness and coronary calcification are related in young and middle-aged adults. The Muscatine study. Circulation. 1999;100:838–842. doi: 10.1161/01.cir.100.8.838. http://dx.doi.org/10.1161/01.CIR.100.8.838. [DOI] [PubMed] [Google Scholar]
- 12.Salonen JT, Salonen R. Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb. 1991;11:1245–1259. doi: 10.1161/01.atv.11.5.1245. http://dx.doi.org/10.1161/01.ATV.11.5.1245. [DOI] [PubMed] [Google Scholar]
- 13.Wada H, Hirano F, Kuroda T, Shiraki M. Breast arterial calcification and hypertension associated with vertebral fracture. Geriatr Gerontol Int. 2012;12:330–335. doi: 10.1111/j.1447-0594.2011.00775.x. http://dx.doi.org/10.1111/j.1447-0594.2011.00775.x. [DOI] [PubMed] [Google Scholar]
- 14.Corrado E, Muratori I, Tantillo R, Contorno F, Coppola G, Strano A. Relationship between endothelial dysfunction, intima media thickness and cardiovascular risk factors in asymptomatic subjects. Int Angiol. 2005;24:52–58. [PubMed] [Google Scholar]
- 15.Salonen JT, Salonen R. Ultrasound B-mode imaging in observational studies of atherosclerotic progression. Circulation. 1993;87:56–65. [PubMed] [Google Scholar]
- 16.Yıldız S, Yıldız A, Ertuğ N, Kaya I, Yılmaz R, Yuksel E, Ziylan SZ. Association of breast arterial calcification and carotid intimamedia thickness. Heart Vessels. 2008;23:376–382. doi: 10.1007/s00380-008-1058-5. http://dx.doi.org/10.1007/s00380-008-1058-5. [DOI] [PubMed] [Google Scholar]


