Abstract
External jugular vein thrombosis is a rare vascular event which may lead fatal complication such as sepsis and pulmonary embolism. Its relation to the visceral solid tumor as an etiologic factor has been established well. Although external jugular vein thrombosis may be seen in malignancy, it is unusual to see as a sign of breast cancer. Most of the external jugular vein thrombosis occurs secondary to compression of the vein. Vascular thrombosis due to hypercoagulability is known as Trousseau syndrome. Herein, we present a case of metastatic breast cancer which presented with external jugular vein thrombosis; Trousseau syndrome.
Keywords: Jugular vein, venous thrombosis, breast cancer
Introduction
Superficial Vein Thrombosis (SVT) is an important disease that can cause life-threatening complications such as Deep Vein Thrombosis (DVT) Pulmonary Embolism (PE), contrary to what was accepted in the past. The risk of developing DVT and PE would be particularly high if superficial thrombophlebitis emerges in the veins close to the junction of the deep vein system. The risk of observing DVT and PE is 3.4% within 3 months following by isolated SVT. The risk remains increased for 5 times 5 years later following SVT (1). External Jugular Vein Thrombosis (EJVT) that occurs 5 months later and a breast cancer case diagnosed accordingly in a patient operated for thyroid carcinoma are presented in this article.
Case Presentation
Unilateral lobectomy was conducted as the result of the needle biopsy performed from thyroid dominant nodule of a euthyroid, 30-year-old female patient with multinodular goiter reported as follicular neoplasia. The final pathological examination of the specimen was reported papillary thyroid carcinoma-solid variant. Depending on the cervical ultrasonography (US) imaging, fine needle aspiration biopsy for the suspected lymph nodes diagnosed at the right level 3 nearby the jugular vein and at the left level 6 was not considered appropriate due to the close neighborhood.
Thereupon, complementary thyroidectomy and central lymph node dissection were performed for the patient by intra-operative frozen section of the suspected lymph nodes. While six lymph nodes were considered reactive depending on the final pathological examination, the histopathological examination of the thyroid tissue specimen was reported lymphocytic thyroiditis. The patient was administered 75 MCI radioactive iodine therapy in the post-operative month three. On the cervical US performed in post-operative month five, soft tissue in peripheral of the left sternocleidomastoid muscle was found edematous and heterogeneous and the EJV was found to be thrombosed.
A non-compressed EJV was observed without flow on the Doppler US imaging. The patient had never experienced such a picture before. There were no cervical trauma, cannulation of the jugular veins, spontaneous hemorrhage, chronic pain, fever, night sweating, and appetite and weight losses in the medical history. A suspected lesion was diagnosed during examination of the patient who specified swelling of the right breast. However, cervical and the other systemic examinations revealed normal findings. There were no special characteristics observed in coagulation tests. The lesion in dimension of 4 cm was considered BIRADS-5 on the mammography (Figure 1). While thrombus of the left EJV was observed on the fraction of the thoracoabdominal angiographic computed tomography (CT), lesions consistent with diffuse lytic-sclerotic metastasis of bones were diagnosed (Figure 2, 3). A lesion in homogeneous fusiform soft tissue density with dimensions of 47×40×66 mm was observed in the area nearby the anterior segment of the right vertebral body, in the posterior segment of the VCS and in the posterolateral segment of the trachea and right bronchus (Figure 4). The patient refused further examination and treatment recommendations and left the hospital voluntarily. It was found out from the patient contacted by phone two months later that her treatment was currently ongoing in a third party medical oncology clinic and she was hospitalized in the intensive care unit for about one month at that time. Informed consent was obtained from the patient who participated in this case.
Figure 1. a, b.
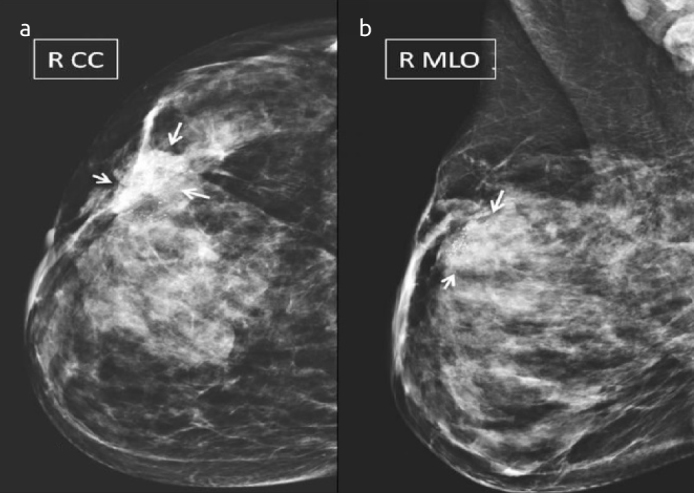
There are dense solid lesions (arrows) on the mammograms and magnification of the right breast including craniocaudal (a) and mediolateral oblique (b) projections, which have spiculated contours, is expanding to peripheral breast parenchyma and the skin, causes retraction of the adjacent skin, with internal diffuse grouped pleomorphic calcifications
Figure 2. a, b.
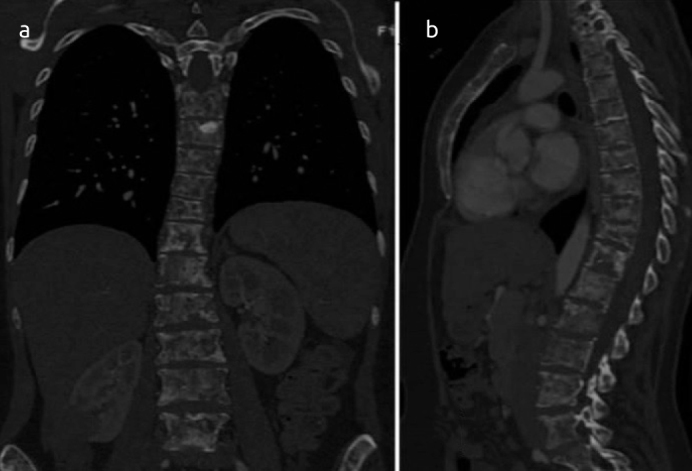
Diffuse osteoblastic and osteolytic metastatic lesions of the vertebrae and sternum are observed on the coronal (a) and sagittal (b) reformatted computed tomography fractions
Figure 3.
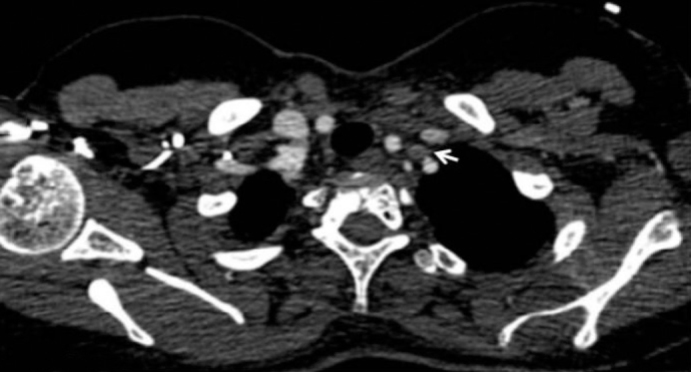
Thrombosed external jugular vein (white arrow) is observed in the anterior segment of the left vertebral artery on the axial thorax computed tomography fraction with contrast agent
Figure 4.

A solid mass (white arrows) of the right breast involving the upper outer quadrant, which is expanding to the skin and with lobulated contour and a mass lesion (curved arrows) of the mediastinum in retrocarinal localization, with lower density on the axial thorax computed tomography fraction with contrast agent
Discussion
Interventions for the breast and thyroid are the most commonly used procedures in surgical practice. However, EJVT is not a common lesion either in post-thyroidectomy or as a symptom of breast cancer. The relationship between cancer and thrombosis was first described by Jean-Baptiste Bouillard in 1823. Later in 1865, Armand Trousseau reported the relationship between gastric carcinoma and thrombosis. The relationship between SVT and cancer was frequently described by Trousseau in unusual places like arm and chest as a superficial vein inflammation in recurrent and mobile characteristic (2). However, reporting of thrombosis as the first symptom of occult cancer was happened much later.
The risk of venous thromboembolism (VTE) has increased in particular for certain types of cancer. Thus, while pancreas (5.3–26%), brain (1.6–26%) have the maximum risk for VTE, the breast (0.4–8.1%) and prostate (0.5–1.4%) have the minimum risk (3). When compared to other tumors, although the risk of VTE is less in breast cancer, the relative high prevalence of the disease makes the vein thrombosis a widespread and important clinical problem for patients with breast cancer.
The temporal interest between SVT and DVT/PE has three types (4). Firstly, DVT or PE may be diagnosed concurrently with the superficial case and this is observed in 29% of patients with acute SVT clinical diagnosis. Secondly, DVT or PE may be developed after a short while of the isolated superficial case. In a study involving 600 patients with symptomatic SVT without thromboembolic history, it was found that DVT or PE developed in 18 patients (3%) within 3 months despite receiving mostly anticoagulant treatment. And thirdly, patients with a SVT history are at risk of development lifelong SVT or PE increased 4 to 6 times.
Physiopathology of thrombosis was described with factors related to endothelial injury, stasis of blood flow and hypercoagulability which are known as “Virchow’s triad” and mostly corresponding to DVT of the lower extremity (5). In the presence of muscle weakness or an incompetent valve, stasis of blood and thrombosis are inevitable. Moreover, more amount of blood in the lower extremity than the upper extremity provides contribution to occurrence of thrombosis in the lower extremity more frequently. The EJV contains valves including a pair at the entry point to the subclavian vein and second pair approximately 4 cm above of this; these valves do not stop the reflux of blood to the EJV. The section between the valves are dilated and called sinus. Jugular veins are more resistant to thrombosis than the lower extremity veins. The major central veins have no valves and have expandable walls that allow recurrent expansion and collapse during respiration. Moreover, the flow direction of the jugular veins are descending by gravity.
External Jugular Vein Thrombosis is rare and diagnosis is often ignored. Central venous catheterization, head and neck infections, malignancy, aneurysm, intravenous drug abuse, iatrogenic injury, advanced age and obesity, and factors with external pressure to the vein were accused as the reason of EJVT in the reported patients, and some of them were considered idiopathic (6). EJVT may be a symptom of a cancer that has been diagnosed and sometimes not yet diagnosed. Suggested mechanisms for the developed thrombosis in this case are the direct effect of the metastatic tumor or hypercoagulability and mobile thrombophlebitis developing secondary to underlying malignancy known as Trousseau syndrome.
In Trousseau syndrome, mobile thrombophlebitis developing secondary to distant organ malignancy may cause thrombosis of unusual places such as the jugular vein and the superior vena cava. In a study involving 541 patients with Trousseau syndrome, the underlying malignancy was classified as lung (25%), pancreas (17.4%), stomach (16.8%) colon (15.2%), prostate (6.5%) and others (7).
External Jugular Vein Thrombosis may appear in cervical region as a painful, thin long and protuberant mass. Contrasted venography is the gold standard in diagnosis of EJVT. However, differential diagnosis must be in wide spectrum for patients who specify limitation, pain and swelling of the cervical movements. Therefore, computed tomography should be taken into account to assess possible infection, neoplasm and vascular dissection. However, cost-effectiveness profile of the Doppler US is better since it is portable and easy accessible, and does not subject the patient to radiation. However, US does not provide information in detail about the condition of the neighboring tissues, and magnetic resonance imaging or CT imaging would be required following it, which provide valuable information in diagnosing the underlying pathology.
With the SVT treatment, a decrease in progression to VTE and improvement in the patient comfort are ensured. Thus, the ‘American College of Chest Physicians’ suggests that the treatment of SVT should be performed using anticoagulants (8).
Conclusion
External Jugular Vein Thrombosis associated with the Trousseau syndrome is rarely observed. Early diagnosis is critical to prevent the vital complications caused by thrombosis, besides it can be the first finding of occult malignancy.
Footnotes
Informed Consent: Informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed
Conflict of Interest: No conflict of interest was declared by the authors.
Author Contributions: Concept - M.Y., M.T.K.; Design - M.Y., M.T.K., A.P.D.; Supervision - M.Y., E.Y.Ç., A.P.D.; Funding - M.Y., E.Y.Ç., A.P.D.; Materials - M.Y., E.Y.Ç, A.P.D.; Data Collection and/or Processing - M.Y., M.T.K., E.Y.Ç.; Analysis and/or Interpretation - M.Y., A.P.D.; Literature Review - M.Y., M.T.K.; Writer - M.Y., M.T.K.; Critical Review - M.T.K., A.P.D.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Cannegieter SC, Horváth-Puhó E, Schmidt M, Dekkers OM, Pedersen L, Vandenbroucke JP, Sørensen HT. Risk of venous and arterial thrombotic events in patients diagnosed with superficial vein thrombosis: a nationwide cohort study. Blood. 2015;125:229–235. doi: 10.1182/blood-2014-06-577783. https://doi.org/10.1182/blood-2014-06-577783. [DOI] [PubMed] [Google Scholar]
- 2.Varki A. Trousseau’s syndrome: multiple definitions and multiple mechanisms. Blood. 2007;110:1723–1729. doi: 10.1182/blood-2006-10-053736. https://doi.org/10.1182/blood-2006-10-053736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Timp JF, Braekkan SK, Versteeg HH, Cannegieter SC. Epidemiology of cancer-associated venous thrombosis. Blood. 2013;122:1712–1723. doi: 10.1182/blood-2013-04-460121. https://doi.org/10.1182/blood-2013-04-460121. [DOI] [PubMed] [Google Scholar]
- 4.Decousus H, Frappé P, Accassat S, Bertoletti L, Buchmuller A, Seffert B, Merah A, Becker F, Queré I, Leizorovicz A. Epidemiology, diagnosis, treatment and management of superficial-vein thrombosis of the legs. Best Pract Res Clin Haematol. 2012;25:275–284. doi: 10.1016/j.beha.2012.07.005. https://doi.org/10.1016/j.beha.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Dickson BC. Venous thrombosis: on the history of Virchow’s triad. Univ Toronto Med J. 2004;81:166–171. [Google Scholar]
- 6.Hindi Z, Fadel E. Idiopathic Bilateral External Jugular Vein Thrombosis. Am J Case Rep. 2015;16:554–557. doi: 10.12659/AJCR.895124. https://doi.org/10.12659/AJCR.895124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sack GH, Jr, Levin J, Bell WR. Trousseau’s syndrome and other manifestations of clinical disseminated coagulopathy in patients with neoplasms: clinical, pathophysiologic and therapeutic features. Medicine (Baltimore) 1977;56:1–37. https://doi.org/10.1097/00005792-197756010-00001. [PubMed] [Google Scholar]
- 8.Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR American College of Chest Physicians. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e419S–494S. doi: 10.1378/chest.11-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]


