Abstract
One of the rare but most challenging issues in the management of the locally-advanced breast cancer (LABC) is life-threatening bleeding from the fungating and/or ulcerating focus (foci) of these tumors. Breast surgeons may need the assistance of interventional radiologists to solve this urgent condition if surgery cannot provide sufficient benefit. Herein, we report a case of recurrent locally-advanced breast cancer that presented with sudden severe bleeding, which was stopped by an interventional radiologist via transcatheter arterial embolization (TAE). In addition, we evaluate the role of interventional radiology in patients with breast cancer who present with bleeding from the breast by reviewing the relevant literature.
Keywords: Breast cancer, embolization, hemorrhage, interventional radiology
Introduction
Breast cancers, particularly those that are locally advanced, may rarely present with acute severe bleeding. They usually appear in the form of fungating and/or ulcerating tumors. This condition can be difficult to manage through a surgical procedure. Interventional radiology has gained an increased role in coping with this problem. The most frequently used method to achieve safe and efficacious hemostasis is transcatheter arterial embolization (TAE). This method was also reported to ensure a reduction in tumor size.
Case Presentation
A woman aged 47 years who had recently undergone a toilet mastectomy plus axillary dissection for locally-advanced breast cancer, presented with sudden severe bleeding from a loco-regionally recurrent tumor that had developed rapidly. She had been diagnosed as having locally-advanced left breast cancer with axillary metastasis at the age of 46 years, which was histopathologically determined as a triple-negative breast cancer. The tumor had remained unresponsive to the neoadjuvant of chemotherapy (NACT), therefore she underwent toilet mastectomy plus axillary dissection to prevent further complications. However, in the very early postoperative period, a locoregional recurrent tumor began to develop on the chest wall and in the axillary region. Recurrent masses, especially the ones in the axilla, tended to ulcerate over the course of time. Owing to ulceration, radiotherapy (RT) was not considered as an option in the treatment. Finally, approximately three months after the operation, the patient presented with sudden severe bleeding from the recurrent breast tumor. She was admitted to our general surgery clinic for treatment of this acute bleeding. On physical examination, the patient was alert, conscious, and cooperative. She had moderate pallor. Her initial blood pressure was 100/60 mmHg, and heart rate of 90 bpm. Inspection of the chest wall showed that there was a very large loco-regionally recurrent breast tumor on the left side along the incision line; the bleeding originated from the deep part of the left axilla where many large ulcerated recurrent tumors were located. She also had an apparent upper limb edema. The results of the lab tests on admission showed a low hemoglobin level of 6 mg/dL and hematocrit of 20.9%. The platelet count was found 241 × 103/microliter. INR and aPTT were within normal ranges. First, a temporary control of bleeding was performed by dressing the wound with sterile gauze pads and compressing them with an elastic bandage around the chest wall. Soon after, an intravenous access was established and replacement of isotonic fluid was initiated. Three units of red cell suspension were transfused consecutively as quickly as possible. Following these resuscitative measures, her vital signs improved with a blood pressure of 120/90 mmHg, and heart rate of 76 bpm. Hemoglobin and hematocrit increased to 11.1 mg/dL and 33.7%, respectively.
An interventional radiologist’s opinion was requested to aid in providing safer hemostasis and the patient was transferred to interventional radiology where a digital subtraction angiography (DSA) of the left axillary artery was performed. The images revealed a giant tumoral blush with many feeders including the costocervical branch and internal mammary artery (IMA) (Figure 1, 2). Through a 5F Cobra catheter, a microcatheter was advanced into all branches coming off the axillary artery and then embolized up to the occurrence of reflux with 300-micron-sized particles (Embosphere; Biosphere Medical, Rockland, Mass). A test DSA showed nearly total devascularization of the tumor (Figures 3, 4). On the first day after the procedure, the patient was well with stable vital signs. When the dressings were opened, complete hemostasis was seen to be present (Figure 5). She was discharged on the second day and scheduled for daily wound care. At one month follow-up examination, there was no obvious bleeding on the left chest Wall.
Figure 1.

Preembolization DSA image acquired during left axillary artery run, giant hypervascular tumoral blush invading left upper part of thoracic wall
Figure 2.

Preembolization DSA image acquired during internal mammary artery (IMA) run, hypervascular tumoral blush invading left anterior part of thoracic wall
Figure 3.
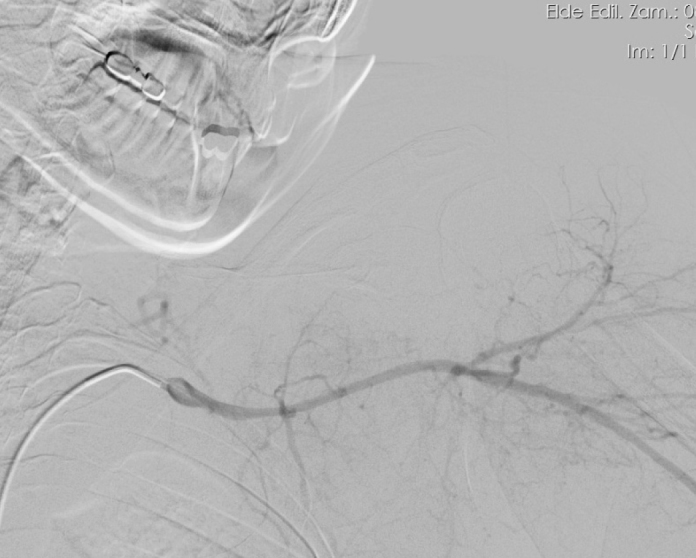
Postembolization DSA image of the axillary artery reflected devascularization of the tumor
Figure 4.

Postembolization DSA image of the IMA reflected devascularization of the tumor
Figure 5.

Complete hemostasis at the bleeding site
Discussion and Conclusion
A high rate of recurrence during the course of LABC is a well-known issue. Katz et al. (1) evaluated a total of 1031 patients who had been treated with mastectomy and doxorubicine-based chemotherapy without RT and found that locoregional recurrence was seen in more than 20% of patients who presented with tumors sized ≥4 cm or with at least four node involvement. In addition, they determined that patients with one to three involved nodes and large tumors, extranodal extension ≥2 mm, or inadequate axillary dissections experienced high rates of recurrence. In both situations, the authors suggested complementary RT. In another report, it was demonstrated that higher tumor stage (T4), higher nodal stage (N2N3), and locally-advanced stage were associated with higher rates of locoregional recurrence and distant metastases (2).
Our patient also had rapid locoregional recurrence that consisted of a number of masses on the left chest wall and in the left axilla. The masses were about to ulcerate, the one in the axilla had ulcerated with subsequent severe bleeding, which required urgent management. The tumor had been found intractable to NACT in the beginning. It was not suitable for hormonotherapy and RT because it was a triple-negative tumor, and ulceration on the relevant region, respectively. Both at the beginning of recurrence and during the bleeding phase of the disease, neither chemo-/hormonotherapy nor RT were considered to be able to provide any benefit.
Bleeding from breast cancer is a rare condition, except in cases of LABC; surgery is the usual treatment under appropriate circumstances. Nagasawa et al. (3), and Kijima et al. (4), reported cases of breast cancer bleeding from open cavities in breasts that had no histopathologic skin invasions. Both authors treated their patients with modified radical mastectomy. Maekawa et al. (5), reported a patient who presented with a huge bleeding breast mass. The authors found that it resulted from ruptured breast cancer vessels into an adjacent cyst due to invasion. The treatment was modified radical mastectomy.
Nevertheless, owing to the skin involvement in LABC, severe bleeding from ulcerating and/or fungating lesions, especially in case of locoregional recurrence, can be seen more often. In these cases, TAE can be chosen a very practical and safe treatment option to control the bleeding instead of surgery, at which point an interventional radiologist should be called for this purpose. Embolization is an endovascular procedure that involves occlusion of arterial or venous structures with the aim of therapeutic outcomes. Interventional radiology has gained an increasing role in this field, particularly with respect to hemostasis for many advanced cancers of the body. A number of substances have been used as embolization agents, including gelatin foam, polyvinyl alcohol particles (PVA), tris-acryl gelatin microspheres, a number of various coils, detachable sack vascular occlusion devices, detachable balloons, amplatzer vascular plugs, n-butyl-2 cyanoacrylate, ethylene vinyl alcohol copolymer, calcium alginate gel, and absolute alcohol (6).
Tokunaga et al. (7), reported a case of breast cancer with chest wall recurrence, which was managed with chemotherapy, TAE, and chest wall resection. The authors advocated that performance of TAE to supply arteries would provide hemostasis and promote mass reduction.
Transcatheter arterial embolization was also reported to be effective in a case of breast angiosarcoma that presented with hemorrhage and was managed using radiologic embolization using PVA, as a temporary measure before the definitive surgery. In the same patient, embolization of the main hepatic artery was also performed for multiple liver metastases (8).
Moriarty et al. (9), reported successful control of a life-threatening bleed that originated from a fungating LABC via TAE with microspheres. The authors suggested using this method with minimal risk when conventional treatment modalities fail or are too morbid to perform.
Another endovascular treatment method performed by interventional radiologists is the placement of a stent into vessels. Ugras et al. (10) achieved successful hemostasis in a patient with a catastrophic hemorrhage from a recurrent fungating axillary breast cancer via placement of an endovascular stent into the axillary artery. Surgical exploration was limited due to arm edema and decreased shoulder immobility in their patient. The authors later found an intimal disruption in the axillary artery under angiography as the probable origin of pseudoaneurysm, and then placed a covered stent across the defect under fluoroscopy.
The clinical pictures of the last two cases were similar to that of our case. In all, there was nothing that could be done surgically and the assistance of interventional radiology was needed.
As in the other cases, TAE was performed in the present case with an entirely palliative intent and did not ensure any benefit on overall survival for the patient; however, it saved the patient’s life in a safe and practical way against a troublesome bleed. This inspired us to keep this modality in mind for use in hard times while managing of breast cancer.
In conclusion, locally-advanced breast cancer and its recurrence can rarely cause sudden severe bleeding. Many of these tumors present in the form of fungating and/or ulcerating lesions, for which the benefit of surgery can be limited. Transcatheter arterial embolization seems as an optimal option in such situations. Breast surgeons should remember to remain in close contact with interventional radiologists during the management of these patients.
Footnotes
Informed Consent: Informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - Ş.A., B.A., Ö.K.; Design - Ş.A., B.A., Ö.K.; Supervision - Ş.A., B.A., Ö.K., R.U.G., M.S.Ç., M.A.N., A.A.; Data Collection and/or Processing - Ş.A., B.A., Ö.K., R.U.G., M.S.Ç., M.A.N., A.A.; Analysis and/or Interpretation - Ş.A., B.A., Ö.K., R.U.G., M.S.Ç, M.A.N.; Literature Review - A.A., B.A.; Writer - B.A., A.A.; Critical Review - Ş.A., B.A., Ö.K., A.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Katz A, Strom EA, Buchholz TA, Thames HD, Smith CD, Jhingran A, Hortobagyi G, Buzdar AU, Theriault R, Singletary SE, McNeese MD. Locoregional recurrence patterns after mastectomy and doxorubicin-based chemotherapy: implications for postoperative irradiation. J Clin Oncol. 2000;18:2817–2827. doi: 10.1200/JCO.2000.18.15.2817. [DOI] [PubMed] [Google Scholar]
- 2.Yadav BS, Sharma SC, Singh R, Singh G. Patterns of relapse in locally advanced breast cancer treated with neoadjuvant chemotherapy followed by surgery and radiotherapy. J Cancer Res Ther. 2007;3:75–80. doi: 10.4103/0973-1482.34683. http://dx.doi.org/10.4103/0973-1482.34683. [DOI] [PubMed] [Google Scholar]
- 3.Nagasawa M, Iino Y, Horiguchi J, Takei H, Maemura M, Horii Y, Matsumoto H, Nagaoka H, Oyama T, Nakajima T, Morishita Y. Sudden hemorrhage of the breast caused by breast cancer: a case report and review of the literature. Breast Cancer. 2000;7:176–178. doi: 10.1007/BF02967454. http://dx.doi.org/10.1007/BF02967454. [DOI] [PubMed] [Google Scholar]
- 4.Kijima Y, Umekita Y, Ehi K, Yoshinaka H, Funasako Y, Owaki T, Yoshida H, Aikou T. Sudden hemorrhage without skin invasion in a Patient with Breast Cancer: A Case Report and literature review. Breast Cancer. 2006;13:317–321. doi: 10.2325/jbcs.13.317. http://dx.doi.org/10.2325/jbcs.13.317. [DOI] [PubMed] [Google Scholar]
- 5.Maekawa S, Shimoda K, Furuyama M, Ikejeri k, Takeo S, Ichiyoshi Y, Saku M. Case report of breast cancer concomitant with huge cyst due to rapture of the tumor vessels. J Jpn Surg Assoc. 1992;53:2091–2094. [Google Scholar]
- 6.Vaidya S, Tozer KR, Chen J. An overview of embolic agents. Semin Intervent Radiol. 2008;25:204–215. doi: 10.1055/s-0028-1085930. http://dx.doi.org/10.1055/s-0028-1085930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tokunaga Y, Hosogi H, Nakagami M, Tokuka A, Ohsumi K. A case of chest wall recurrence of breast cancer treated with paclitaxel weekly, 5′-deoxy-5-fluorouridine, arterial embolization and chest wall resection. Breast Cancer. 2003;10:366–370. doi: 10.1007/BF02967659. http://dx.doi.org/10.1007/BF02967659. [DOI] [PubMed] [Google Scholar]
- 8.Taib N, Yip Ch, Ranganathan S, Moosa F, Mun K. Haemorrhaging lesion in the breast: is there a role for embolisation? Biomed Imaging Interv J. 2006;2:e30. doi: 10.2349/biij.2.3.e30. http://dx.doi.org/10.2349/biij.2.3.e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moriarty JM, Xing M, Loh CT. Particle embolization to control life-threatening hemorrhage from a fungating locally advanced breast carcinoma: a case report. J Med Case Rep. 2012;6:186. doi: 10.1186/1752-1947-6-186. http://dx.doi.org/10.1186/1752-1947-6-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ugras S, Gemignani ML, Connolly PH, Finley DJ. Endovascular Approach to Acute Hemorrhage in Locally Advanced Breast Cancer. Breast J. 2015;21:189–191. doi: 10.1111/tbj.12373. http://dx.doi.org/10.1111/tbj.12373. [DOI] [PubMed] [Google Scholar]


