Abstract
This protocol describes the generation of bladder tumors in female C57BL/6J mice using the murine bladder cancer cell line MB49, which has been modified to secrete human Prostate Specific Antigen (PSA), and the procedure for the confirmation of tumor implantation. In brief, mice are anesthetized using injectable drugs and are made to lay in the dorsal position. Urine is vacated from the bladder and 50 µL of poly-L-lysine (PLL) is slowly instilled at a rate of 10 µL/20 s using a 24 G IV catheter. It is left in the bladder for 20 min by stoppering the catheter. The catheter is removed and PLL is vacated by gentle pressure on the bladder. This is followed by instillation of the murine bladder cancer cell line (1 x 105 cells/50 µL) at a rate of 10 µL/20 s. The catheter is stoppered to prevent premature evacuation. After 1 h, the mice are revived with a reversal drug, and the bladder is vacated. The slow instillation rate is important, as it reduces vesico-ureteral reflux, which can cause tumors to occur in the upper urinary tract and in the kidneys. The cell line should be well re-suspended to reduce clumping of cells, as this can lead to uneven tumor sizes after implantation.
This technique induces tumors with high efficiency. Tumor growth is monitored by urinary PSA secretion. PSA marker monitoring is more reliable than ultrasound or fluorescence imaging for the detection of the presence of tumors in the bladder. Tumors in mice generally reach a maximum size that negatively impacts health by about 3 - 4 weeks if left untreated. By monitoring tumor growth, it is possible to differentiate mice that were cured from those that were not successfully implanted with tumors. With only end-point analysis, the latter may be mistakenly assumed to have been cured by therapy.
Keywords: Cancer Research, Issue 119, bladder, tumor, mice, orthotopic, model, detection, urine
Introduction
The goal of this method is to generate murine orthotopic bladder tumors and to monitor the implanted tumors as accurately as possible, so that mice without tumor implantation are not thought to have been cured at end-point analysis. Overall, the method shown will reduce the need for large numbers of mice for experimental analysis and ensure greater accuracy in determining therapeutic outcomes.
The development of an orthotopic model for cancer is important, as implanting tumor cells subcutaneously does not recapitulate the environment of the clinical disease or enable the development of therapeutic strategies. The architecture of the bladder permits the instillation of bladder cancer therapies directly into the bladder with minimal systemic effects. Thus, animal models that recapitulate this environment, such as an orthotopic model, are important to evaluate new therapies. The conclusions drawn from any experimental set-up are dependent upon the limitations of the model.
Several techniques have been developed for the production of orthotopic bladder tumors in mice. These rely on damaging the glycosaminoglycan layer of the bladder, enabling tumor cells to be implanted. The techniques used include electrocautery, which results in a single point of damage in the bladder wall, leading to tumor development at one site in the bladder1,2. However, the success rate of tumor implantation using electrocautery is operator-dependent varying from 10 - 90%, and it includes the danger that the bladder wall will be punctured, leading to tumors developing in the peritoneal cavity. Chemical cautery is performed using silver nitrate, which damages the bladder wall3. Similarly, acid has been used to damage the bladder wall4. Trypsin has also been used to damage the bladder as well5. These methods may result in the development of more than one tumor in the bladder. Furthermore, there is a danger of severe damage to the bladder if the chemicals are left in contact with the bladder wall for too long. The method developed by Ninalga et al. uses the positively charged poly-L-lysine (PLL)6 molecules to coat the bladder wall; this enables the negatively charged tumor cells to stick to the glycosaminoglycan layer of the bladder. This method generally results in more than one tumor developing in the bladder, but tumor implantation is at 80 - 100%4,7. Technically, it is also the easiest procedure to perform. To ensure that the tumors that develop are fairly even in size, it is important that the tumor cells are not grouped in large clumps before implantation.
In order to evaluate therapeutic efficacy, it is best to perform this study on mice with fairly similar-sized tumors. Thus, a good detection system that can quantify tumor size soon after implantation is important. Several strategies have been used to evaluate tumors. These include magnetic resonance imaging (MRI)8-10, fluorescence11, bioluminescence12,13, ultrasound14, and enzyme-linked immunosorbent assay (ELISA)15,16. While MRI and ultrasound do not require modifications of the tumor cells, there is a need for sensitive equipment and contrast agents for MRI. The fluorescence-, luminescence-, and ELISA-based assays require modification of the tumor cells to express marker proteins that can be detected by these methods. For luminescence, a substrate is required for the detection of the luciferase activity; thus, there is an added step and increased cost. Both luminescence and fluorescence require specialized equipment. To produce fluorescence, green fluorescent protein (GFP) cyclization, which is catalyzed by molecular oxygen, is required. Thus, GFP expression may be variable within a tumor mass depending on access to oxygen, making this a rather unreliable marker17. Modification of the murine bladder cancer cell line MB49 to secrete human Prostate Specific Antigen (PSA)15,16 as a surrogate marker is another strategy. These markers also provide an alternative means of confirming tumor presence at the termination of the experiment, making them an alternative to immunohistochemistry. This study reports the PLL method of orthotopic tumor implantation and presents a comparison of tumor detection systems, namely ELISA, fluorescence, and ultrasound imaging.
Protocol
All animal work adhered to the Institutional Animal Care and Use Committee (IACUC) guidelines on animal use and handling (Protocol number 084/12) at the National University of Singapore.
1. Growing MB49-PSA Cells In Vitro and Measuring PSA Secretion
Maintain murine bladder cancer cells MB49-PSA15 in complete Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 2 mmol/L L-glutamine, and 0.05 mg/mL Penicillin-Streptomycin in an incubator at 37 °C and 5% CO2. Add 200 μg/mL Hygromycin B to maintain the selection pressure of PSA-secreting cells.
To determine PSA secretion, plate 1 x 106 cells in a 6-well culture plate and incubate it at 37 °C in the presence of 5% CO2 for 48 h.
- Two days later, collect the supernatant for the PSA measurement.
- Using a Pasteur pipette, transfer the supernatant to a 15 mL centrifuge tube.
- Centrifuge for 5 min at 250 x g to remove floating cells and debris. If the PSA assay is carried out on a different day, store the supernatant at - 30 °C in a 1.5 mL microcentrifuge tube. If not, proceed to the next step immediately.
- Determine the PSA concentration using a human-free PSA ELISA kit7.
- Enumerate the plated cells.
- Using a Pasteur pipette, wash the cells gently with 1 mL of DMEM. Aspirate and completely remove the media.
- Add 1 mL of fresh media and scrape gently with a cell scraper to dislodge the cells from the well.
- Transfer the cells to a microcentrifuge tube and re-suspend them thoroughly to ensure a single-cell suspension.
- Mix equal volumes of the cell suspension and a 0.4% trypan blue solution. Count the live cells (which do not take up the dye) using a hemocytometer.
Calculate the PSA expression as ng of PSA/mL of media/106 cells. The PSA expression of MB49-PSA cells for implantation in mice is 80 - 120 ng/mL/106 cells.
2. Determining the Sensitivity of PSA Measurements by ELISA and Real-time PCR Analysis
Plate MB49-PSA cells in complete DMEM media in a 6-well culture plate with different amounts of parental MB49 cells such that there is a maximum of 1 x 106 cells per well (i.e., 100, 101, 102, 103, 104, 105, or 106 MB49-PSA cells are cultured with 106, 105, 104, 103, 102, 101, or 100 MB49 cells, respectively).
One day later, collect the supernatant for PSA measurement, as described in step 1.3. Determine the PSA concentration using a human-free PSA ELISA kit7.
- Extract the RNA from the cells.
- Lyse the cells directly in the plate by adding 1 mL of RNA extraction reagent.
- Incubate for 5 min at room temperature and transfer the cell lysate to a microcentrifuge tube. Add 0.2 mL of chloroform and vortex the samples vigorously for 15 s. Incubate them for 3 min at room temperature.
- Centrifuge the samples at 12,000 x g for 15 min at 4 °C. Carefully transfer the upper aqueous phase (0.5 mL) to a fresh tube without disturbing the interphase.
- Add 0.5 mL of isopropyl alcohol. Incubate for 10 min at room temperature. Centrifuge the samples at 12,000 x g for 10 min at 4 °C. Remove the supernatant completely, without disturbing the RNA precipitate at the bottom of the tube.
- Wash the pellet once with 1 mL of 75% ethanol. Centrifuge at 7,500 x g for 5 min at 4 °C. Remove all ethanol and allow the pellet to air dry for 10 min.
- Dissolve the RNA in 30 µL of nuclease-free water. Incubate for 5 min at 60 °C to increase the solubility.
- Quantitate the RNA by measuring the absorbance using ultraviolet (UV) spectroscopy at 260 nm (A260). To assess RNA purity, measure the absorbance at 280 nm (A280) and calculate the A260/A280 ratio which should be above 1.6.
- Reverse-transcribe cDNA from 2 µg of RNA.
- Prepare the reaction mixture on ice and transfer it to 0.2 mL tubes.
- Briefly centrifuge the tubes to spin down the contents and to eliminate air bubbles.
- Load the tubes into the thermal cycler and perform reverse transcription at the following conditions: 60 min at 37 °C followed by 5 min at 95 °C. Once the run is completed, keep the cDNA samples at 4 °C.
- Store the samples at - 30 °C for long-term storage.
Perform a real-time PCR analysis for PSA and cytoplasmic beta actin. Beta actin is used to normalize the samples. Perform the assay on 100 ng of reverse-transcribed RNA in a 96-well plate. Assay all samples in triplicate. Perform 40 cycles with the following parameters: 2 min at 50 °C, 10 min at 95 °C, 15 s at 95 °C for denaturation, and 1 min at 60 °C. Set the lowest limit of detection at a cycle threshold (CT) of 35; thus, any sample with a CT value beyond 35 is considered not detectable.
3. Maintaining the Tumorigenicity of the MB49-PSA Cell Line
NOTE: Prolonged growth in vitro leads to a loss of tumorigenicity. To maintain tumorigenicity, the MB49-PSA cell line is passaged through the mouse at least once every 2 years.
- Cells.
- Harvest exponentially growing cells by scraping them gently with a sterile cell scraper. Mix equal volumes of the cell suspension and a 0.4% trypan blue solution. Count the live cells using a hemocytometer. Do not implant if more than 20% of the cells are dead.
- Calculate the amount of live cells required (1 x 107 cells/mL) and transfer them to a 15 mL centrifuge tube. Centrifuge at 250 x g for 5 min at 4 °C and discard the supernatant. Re-suspend the cell pellet in DMEM blank media. Repeat the wash three times to remove all traces of FBS before implantation.
- Keep the cell suspension on ice until the mice are ready for implantation.
- Implant the tumor cells subcutaneously in mice on the dorsal flank.
- Anesthetize a 4- to 6-week-old C57BL6/J mouse using a mixture of the anesthetics ketamine and medetomidine (75 mg/kg and 1 mg/kg, respectively), injected intraperitoneally at 0.1 mL per 10 g of bodyweight.
- Shave the right flank to expose the skin.
- Using a pair of forceps, lift the skin to separate it from the underlying muscle and inject 0.1 mL of the cell suspension (1 x 106 cells) subcutaneously with a 24 G needle. While removing the needle, pinch the injection site for 5 to 10 s so that the tumor cells do not leak out of the injection site.
- Revive the mouse with a subcutaneous injection of atipamezole (1 mg/kg) at 0.1 mL per 10 g of bodyweight.
Monitor tumor growth every two days by measuring tumor diameter using calipers. The tumor volume is calculated using the formula v = (ab2)/2, where "a" is the longest dimension and "b" is the perpendicular width, both in mm.
When the tumor volume is at least 50 mm3 (approximately 7 days), euthanize the mouse with CO2. Excise the tumor mass with a pair of sterile forceps and scissors under aseptic conditions and place in DMEM.
In a 6-well culture plate, mince the tumor into small pieces using sterile scalpels. Use a 1 mL syringe plunger as a "pestle" to further disaggregate the tumor.
Add 3 mL of complete DMEM and maintain the cells in an incubator at 37 °C and 5% CO2.
Once the cells adhere to the plate (between one and two days), remove the media, debris, and non-adherent cells by aspirating gently with a sterile Pasteur pipette. Wash twice with DMEM. Take care to not disturb the cells.
Add 1 mL of DMEM and harvest the cells by scraping them with a cell scraper. To select and expand single colonies, count the cells using a hemocytometer and plate 1 cell per well in a 96-well culture plate. Culture cells in DMEM with 200 μg/mL Hygromycin B at 37 °C and 5% CO2.
Change the media and antibiotic every 4 - 5 days. Monitor the cells until they are at about 80-90% confluent. Re-plate the cells on a 24-well culture plate by pipetting to dislodge cells from the well.
Once the cells in the 24-well culture plate are confluent, dislodge them by scraping with a cell scraper and plate them in a 6-well culture plate.
Screen the different clones for PSA secretion, as described in step 1. Cryo-preserve the clone with the highest PSA secretion and use it for future mouse experiments.
4. Implanting the Tumor
NOTE: Each mouse is implanted with 1 x 105 MB49-PSA cells in 50 µL of DMEM blank media in the bladder. Due to the dead space in the catheter, always prepare extra volume (at least 100 µL extra per mouse). An alternative approach would be to use an air filled syringe as described by Kasman et al.5 rather than a filled syringe.
- Cells.
- One day before implantation, when the cells are approximately 80% confluent, passage the MB49-PSA tumor cells in complete DMEM media (supplemented with 10% FBS, 2 mmol/L L-glutamine, 0.05 mg/mL Penicillin-Streptomycin, and 200 µg/mL Hygromycin B) at 37 °C and 5% CO2 at a split ratio of 1:2.
- On the day of the procedure, harvest the cells by scraping them gently with a sterile cell scraper. Mix equal volumes of the cell suspension and a 0.4% trypan blue solution. Count the live cells using a hemocytometer. Do not implant if more than 20% of the cells are dead.
- Calculate the amount of live cells required (2 x 106 cells/mL) and transfer them to a 15 mL centrifuge tube. Centrifuge at 250 x g for 5 min at 4 °C and discard the supernatant. Re-suspend the cell pellet in DMEM blank media. Repeat the wash three times to remove all traces of FBS before implantation.
- Keep the cell suspension on ice until the mice are ready for implantation.
- Allow the 4- to 6-week-old female C57BL/6J mice to acclimatize for one week before the procedure. All animal work must be performed in a biological safety cabinet to maintain sterile conditions.
- Weigh each mouse and inject anesthesia (75 mg/kg ketamine and 1 mg/kg medetomidine) intraperitoneally at 0.1 mL per 10 g of bodyweight. Bodyweights should be between 17 and 22 g. Confirm anesthetization by observing no response after a toe pinch.
- For identification, mark the ear using an ear punch.
- Inject Hartmann's solution or compound sodium lactate intraperitoneally at 0.1 mL per 10 g of bodyweight every 1 - 2 h for hydration.
- Apply sterile ophthalmic ointment to both eyes using a sterile cotton bulb, since the blinking reflex is lost under anesthesia and the eyes dry out. Reapply when necessary.
- Lay the mice in supine position on paper towels on top of a heat pack (activated by contact with air) to maintain body temperature and tape the hind legs down.
With a finger, apply gentle pressure to the lower abdominal region and collect urine from the bladder into a 1.5-mL microcentrifuge tube. This sample serves as the basal value of urinary PSA.
Withdraw sterile poly-L-lysine (PLL) into a 1 mL syringe and attach a 24-gauge IV catheter, with the needle stylet removed. Apply lubricant to the tip of the catheter and insert the catheter through the urethra into the bladder using forceps to guide the catheterization. Stop when resistance is felt. NOTE: Researchers should discuss with their veterinary staff about the need for the use of a lubricating gel with anesthetic for intravesical instillations and the use of post–procedure analgesics.
Instill 50 µL of PLL slowly, at a rate of 10 µL every 20 s, to avoid vesico-ureteral reflux18. Leave the catheter in the bladder for 20 min with a stopper to prevent out-flow.
After 20 min, remove the catheter and vacate the bladder of any contents by gently pressing on the lower abdominal region. Using an empty 1 mL syringe, flush any remaining contents out of the catheter.
Mix MB49-PSA cells thoroughly by pipetting and withdraw them into a 1 mL syringe. Attach the catheter and apply lubricant. Instill 50 µL of 1 x 105 cells at a slow rate of 10 µL every 20 s. Replace the stopper on the catheter. Give control mice 50 µL of saline.
After 1 h, remove the catheters and vacate the bladder of any contents. Remove the tape on the hind legs and place the mice on their ventral sides. Revive the mice by subcutaneously injecting the reversal drug (1 mg/kg atipamezole) at 0.1 mL per 10 g of bodyweight.
Monitor the mice until motility is observed. Return the mice to their cages.
Upon completion of a tumor detection protocol (sections 5, 7, or 8), euthanize the mice using CO2. Post-mortem tumor detection is described in section 6.
5. Monitoring Tumor Growth with ELISA
NOTE: Tumor presence and growth is monitored in mice by measuring PSA secretion in urine. Researchers should consult with their veterinary staff on monitoring animal health and well-being post-tumor implantation and humane endpoints.
- There are two methods to collect urine from mice.
- Collect urine overnight by placing a single mouse in an individual metabolic cage designed to separate urine from fecal material. If the set-up does not have refrigeration, add a protease inhibitor (100 µL) into the urine collection tube to prevent degradation of PSA overnight. However, the number of available metabolic cages limits the utility of this method of urine collection.
- Where it is logistically impossible to use metabolic cages (such as in the ABSL2 rooms), collect spot urine by using a finger to exert gentle pressure on the lower abdominal region while the mice are anesthetized as described in step 4.2.1. This is usually done before the therapy is instilled. From our experience, at least 150 µL of urine can be collected 1 h after anesthesia.
Immediately place the collected urine on ice. Hematuria may be visible from the second week after tumor implantation. Highly hemolyzed samples may affect ELISA analysis. Therefore, urine must be placed on ice and processed quickly after collection.
Centrifuge the urine tubes at 6,700 x g for 5 min at 4 °C to remove cells or debris.
To normalize the difference in urine output between the mice, aliquot the urine into new tubes and store them at -30 °C until performing the analyses for PSA using an ELISA kit7 and creatinine using an assay kit7. Even though mice do not produce PSA, there are low levels of non-specific binding detected using the ELISA. For samples to be considered positive, the threshold must be set at values greater than in normal mice + 3 Standard Deviations (SD)15.
6. Detecting Tumor Presence with Real-time PCR
At termination, dissect the abdominal cavity of the mouse and locate the bladder. Excise the bladder and place it into a cryovial. Freeze immediately in liquid nitrogen.
Extract the RNA by homogenizing the tissues in an RNA extraction reagent.
Perform reverse transcription and real-time PCR analysis for PSA, as described above in section 2.
7. Monitoring Tumor Growth with Fluorescence Imaging
Label 1 x 107 MB49-PSA cells with a near-infrared fluorescent dye19.
Re-plate and harvest the labeled cells on days 4, 7, 11, 14, 18, and 21 to check if cells retain viability and fluorescence by flow cytometry20.
Implant the labeled MB49-PSA cells in mice bladders, as described above in section 4.
Monitor the tumor growth using a fluorescence imaging system every two days.
On the day of imaging, weigh and anesthetize the mice using a mixture of the anesthetics ketamine and medetomidine (75 mg/kg and 1 mg/kg, respectively), injected intraperitoneally at 0.1 mL per 10 g of bodyweight.
Shave the abdominal area to expose the skin.
Place mice in the imaging chamber and acquire images of the bladders using the software provided with the imaging system.
Revive the mice by subcutaneously injecting a reversal drug (1 mg/kg atipamezole) at 0.1 mL per 10 g of bodyweight.
8. Monitoring Tumor Growth with High-frequency Ultrasound Imaging
Implant tumors in mice, as described above in section 4.
Every two days, monitor tumor growth using ultrasound imaging.
On the day of imaging, weigh and anesthetize the mice using a mixture of the anesthetics ketamine and medetomidine (75 mg/kg and 1 mg/kg, respectively), injected intraperitoneally at 0.1 mL per 10 g of bodyweight.
Shave the abdominal area to expose the skin.
Instill 100 μL of sterile 0.9% saline into the bladder using a 24-gauge IV catheter. The saline will distend the bladder and improve visibility during the ultrasound imaging.
Place the mouse on the ultrasound platform and apply conductive gel to the lower abdomen.
Lower the handheld probe to the skin and acquire B-mode images of the bladder on the imaging platform21.
Revive the mice by subcutaneously injecting reversal drug (1 mg/kg atipamezole) at 0.1 mL per 10 g of bodyweight.
Representative Results
PSA secretion from MB49 cells was found to vary with the growth media. MB49-PSA is grown in DMEM media because this results in increased PSA secretion (Figure 1A). In order to determine the sensitivity of the PSA ELISA and real-time PCR, different numbers of MB49-PSA-secreting cells were mixed with MB49 parental cells. PSA ELISA detects a minimum of 1 x 105 PSA-secreting cells/1 x 106 cells (Figure 1B), while real-time PCR analysis detects 100 PSA-secreting cells/1 x 106 cells (Figure 1C). Thus, real-time PCR is more sensitive than ELISA, but it can only be performed on the whole bladder. This limits its utility to end-point analysis. The PLL method of tumor implantation results in multiple tumors (Figure 2A) developing in the bladder. Both overnight collection of urine using metabolic cages (Figure 2B, upper panel) and spot urine samples (Figure 2B, lower panel) can be used to measure PSA by ELISA. For all animal studies, mouse weight is noted as a measure of health (Figure 2C, upper panel), and urinary PSA is monitored on a weekly basis (Figure 2C, lower panel) as a measure of tumor growth. There is generally a good correlation between mouse weight and tumor size, as measured by PSA. Mice with large tumors start to lose weight (Figure 2C, mice 3 and 5). Some mice observed in Figure 2C may have a large tumor but still display a normal bodyweight. Thus, bodyweight alone is not a sufficient measure of tumor growth. PSA serves as a good surrogate marker of tumor growth (Figure 3A-D). Mice were euthanized about 3 - 5 days after urine analysis for PSA on day 14. The images of the bladder cross-sections show tumor size and the corresponding day 14 PSA/creatinine x 106 reading. The variation in tumor size is related to the treatment the mice received. Figure 3, panels A-D represent mice from 3 different treatment arms. An alternative strategy to PSA modification of cells is the labeling of cells with a dye. This strategy eliminates the need for cell transformation and selection. Labeling of MB49-PSA cells with a fluorescent dye is easy to perform (Figure 4A), and in vitro monitoring showed promise in terms of the survival of the signal, despite cell replication (Figure 4B and C). However, in vivo imaging was not successful, because the mouse feed also had natural red fluorescence (Figure 4D), which resulted in non-specific fluorescence in the abdominal region. A comparison was performed between ultrasound imaging, PSA urinary secretion, and PSA end-point analysis. Ultrasound imaging of the bladder (Figure 5A-H) was good for identifying large tumors, but it was not so successful with small tumors.
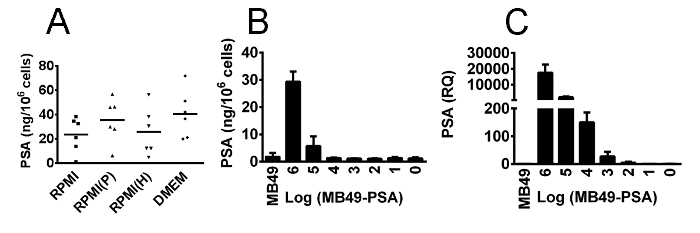 Figure 1.PSA Secretion from MB49-PSA Cells and the Determination of Detection Limits Using ELISA and Real-time PCR Analysis. (A) 1 x 106 MB49-PSA cells were grown in different growth media, and PSA secretion in the supernatant was detected 2 days later by ELISA. The growth media were: RPMI with FBS- (RPMI), RPMI with Premium FBS (RPMI(P)), RPMI with an alternative FBS (RPMI(H)), and DMEM with FBS (DMEM). MB49-PSA cells grown in DMEM media had higher PSA secretion. (B) MB49-PSA cells (106 cells to 1 cell) were mixed with parental MB49 cells (1 cell to 106 cells) and plated for 24 h. PSA ELISA was performed on the supernatant, and RNA was extracted from the cells. A minimum of 1 x 105 PSA-secreting cells/1 x 106 cells were detectable by ELISA. (C) 100 PSA-secreting cells/1 x 106 cells were detectable by real-time PCR analysis. The y axis values represent the mean RQ (relative quantification) ± standard deviation. RQ values are relative fold changes, obtained by normalizing CT values of PSA to beta actin gene and compared with a control bladder which is set at 1. Please click here to view a larger version of this figure.
Figure 1.PSA Secretion from MB49-PSA Cells and the Determination of Detection Limits Using ELISA and Real-time PCR Analysis. (A) 1 x 106 MB49-PSA cells were grown in different growth media, and PSA secretion in the supernatant was detected 2 days later by ELISA. The growth media were: RPMI with FBS- (RPMI), RPMI with Premium FBS (RPMI(P)), RPMI with an alternative FBS (RPMI(H)), and DMEM with FBS (DMEM). MB49-PSA cells grown in DMEM media had higher PSA secretion. (B) MB49-PSA cells (106 cells to 1 cell) were mixed with parental MB49 cells (1 cell to 106 cells) and plated for 24 h. PSA ELISA was performed on the supernatant, and RNA was extracted from the cells. A minimum of 1 x 105 PSA-secreting cells/1 x 106 cells were detectable by ELISA. (C) 100 PSA-secreting cells/1 x 106 cells were detectable by real-time PCR analysis. The y axis values represent the mean RQ (relative quantification) ± standard deviation. RQ values are relative fold changes, obtained by normalizing CT values of PSA to beta actin gene and compared with a control bladder which is set at 1. Please click here to view a larger version of this figure.
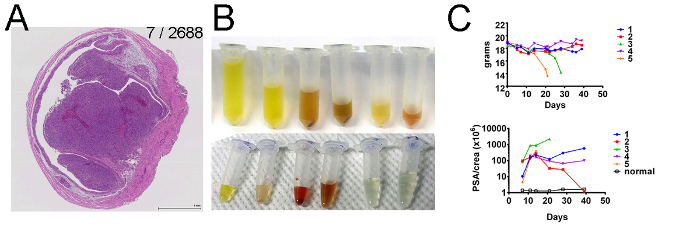 Figure 2.Bladder Tumor Growth and Detection. (A) Histological examination of a bladder 13 days after tumor implantation. The paraffin-embedded bladder was sectioned and stained with hematoxylin (dark blue), which stains the nuclei, and eosin (pink), which stains the remaining cellular components. The PSA/creatinine x 106 value for this bladder on days 5 and 13 are shown as 7/2688. The magnification is at 44.8X. The scale bar represents 1 mm. (B) Urine was collected by either placing mice in metabolic cages overnight and transferring the urine from the collection tube into 2 mL tubes (upper panel) or by on-the-spot urine collection from anesthetized mice (lower panel) into 1.5 mL tubes, which were then transferred to 0.6 mL tubes. (C) After tumor implantation, mice weight was monitored twice weekly (upper panel). Urinary PSA was measured to monitor tumor implantation and growth in mice (lower panel). The y axis PSA/crea represents urinary PSA normalized to creatinine x 106. Mice were terminated once there was a loss of more than 20% of the bodyweight. Note: PSA gene expression was detected in the bladder of mouse 2 at day 40, when it was terminated, even though it had low urinary PSA. Please click here to view a larger version of this figure.
Figure 2.Bladder Tumor Growth and Detection. (A) Histological examination of a bladder 13 days after tumor implantation. The paraffin-embedded bladder was sectioned and stained with hematoxylin (dark blue), which stains the nuclei, and eosin (pink), which stains the remaining cellular components. The PSA/creatinine x 106 value for this bladder on days 5 and 13 are shown as 7/2688. The magnification is at 44.8X. The scale bar represents 1 mm. (B) Urine was collected by either placing mice in metabolic cages overnight and transferring the urine from the collection tube into 2 mL tubes (upper panel) or by on-the-spot urine collection from anesthetized mice (lower panel) into 1.5 mL tubes, which were then transferred to 0.6 mL tubes. (C) After tumor implantation, mice weight was monitored twice weekly (upper panel). Urinary PSA was measured to monitor tumor implantation and growth in mice (lower panel). The y axis PSA/crea represents urinary PSA normalized to creatinine x 106. Mice were terminated once there was a loss of more than 20% of the bodyweight. Note: PSA gene expression was detected in the bladder of mouse 2 at day 40, when it was terminated, even though it had low urinary PSA. Please click here to view a larger version of this figure.
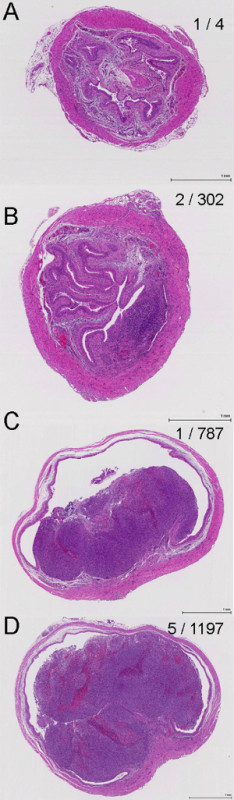 Figure 3.PSA and Bladder Tumor Growth. (A-D) Histological sections of mice bladders harvested at day 19 (A and B), day 17 (C) and day 13 (D) after tumor implantation. The day 4 and day 13 or day 14 urinary PSA/creatinine x 106 values for each bladder is shown on the right side of each image in the format day 4 / day 13 or 14. The urinary PSA/creatinine values increase with tumor size. The mice in images A-D received different therapies accounting for the tumor size differences. The magnification is at 41.4X. The scale bar represents 1 mm. Please click here to view a larger version of this figure.
Figure 3.PSA and Bladder Tumor Growth. (A-D) Histological sections of mice bladders harvested at day 19 (A and B), day 17 (C) and day 13 (D) after tumor implantation. The day 4 and day 13 or day 14 urinary PSA/creatinine x 106 values for each bladder is shown on the right side of each image in the format day 4 / day 13 or 14. The urinary PSA/creatinine values increase with tumor size. The mice in images A-D received different therapies accounting for the tumor size differences. The magnification is at 41.4X. The scale bar represents 1 mm. Please click here to view a larger version of this figure.
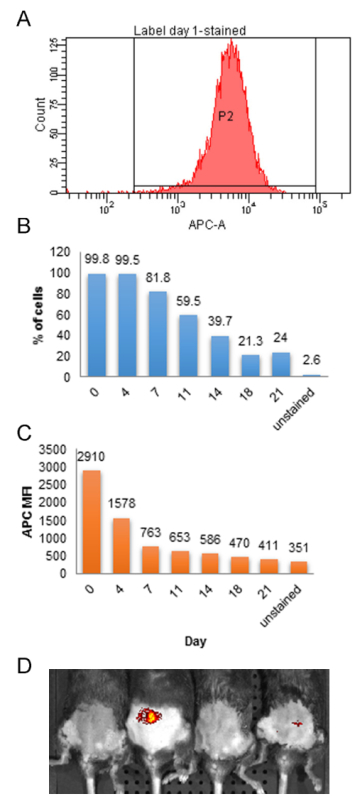 Figure 4. Profile of MB49-PSA Cells Labeled with a Fluorescent Dye. (A) Stained cells were analyzed by flow cytometry before plating. Labeled cells were harvested every few days to analyze the intensity of the fluorescent dye. (B) Percentage of labeled MB49-PSA cells within the P2 gate from (A) at specified days post- labeling. (C) Intensity of the fluorescent dye measured by mean fluorescence intensity (MFI) of the signal. (D) Images of mice 10 days after implantation with labeled MB49-PSA cells using an in vivo imaging system showed non-specific fluorescence in the abdominal region. Please click here to view a larger version of this figure.
Figure 4. Profile of MB49-PSA Cells Labeled with a Fluorescent Dye. (A) Stained cells were analyzed by flow cytometry before plating. Labeled cells were harvested every few days to analyze the intensity of the fluorescent dye. (B) Percentage of labeled MB49-PSA cells within the P2 gate from (A) at specified days post- labeling. (C) Intensity of the fluorescent dye measured by mean fluorescence intensity (MFI) of the signal. (D) Images of mice 10 days after implantation with labeled MB49-PSA cells using an in vivo imaging system showed non-specific fluorescence in the abdominal region. Please click here to view a larger version of this figure.
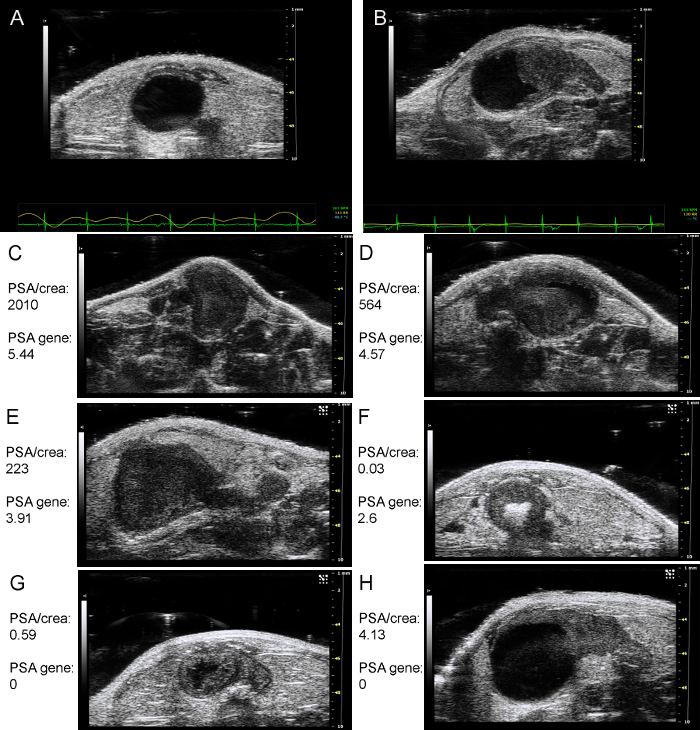 Figure 5. Ultrasound Images of Murine Bladders. Mice bladders (A) before tumor implantation and (B) 8 days after tumor implantation. (C) to (H) are ultrasound images of mice bladders two weeks after implantation. PSA/crea: urinary PSA normalized to creatinine (106). PSA gene: gene expression of PSA in the bladders (log RQ) are shown for each bladder. Please click here to view a larger version of this figure.
Figure 5. Ultrasound Images of Murine Bladders. Mice bladders (A) before tumor implantation and (B) 8 days after tumor implantation. (C) to (H) are ultrasound images of mice bladders two weeks after implantation. PSA/crea: urinary PSA normalized to creatinine (106). PSA gene: gene expression of PSA in the bladders (log RQ) are shown for each bladder. Please click here to view a larger version of this figure.
| Urinary PSA | Fluorescence Imaging | Ultrasound Imaging | |
| Steps (time required) | Anesthetize mice. Collect 110 μL urine. (~ 1 h) Perform PSA ELISA (total incubation time: 2 h 30 min) Creatinine assay (incubation time: 5 min) | Anesthetize mice. Shave fur on abdominal region. Perform imaging. | Anesthetize mice. Shave fur on abdominal region. Catheterize and instill 100 μL of saline into the bladder. Apply conductive gel to lower abdomen and obtain ultrasound images. |
| Specialized equipment | ELISA plate reader (at wavelength of 450 nm and 510 nm) | Imaging System | Ultrasound Imaging System |
| Modification of tumor cells | Required (expressing PSA) | Required (fluorescence) | Not required |
| Advantages | Reliable | Simple and quick | Can detect large tumors |
| Limitations | May not get enough urine A negative value does not mean absence of tumor (PSA gene expression analysis increases sensitivity but is limited to end-point analysis) | Careful selection of fluorescence dye is needed to prevent high background. | Cannot detect small tumors. One mouse at a time. |
Table 1. Comparison of Methods for Monitoring Tumor Growth in Mouse Bladders.
Discussion
The most critical steps in the protocol are 1) successfully maintaining the tumorigenicity of the cell line; 2) ensuring measurable PSA secretion before tumor cell implantation in mice; 3) generating a single-cell suspension for implantation so as to reduce variation in tumor size; and 4) instilling cells at a slow rate to prevent vesico-ureteral reflux, resulting in tumor cell implantation in the kidney.
After prolonged passage in vitro, MB49/MB49-PSA cells can lose their tumorigenicity, as demonstrated by their inability to produce tumors in mice. This could be a confounding factor as to whether or not mice are cured after therapy. In the absence of tumors, it is not possible to differentiate mice cured by therapy from mice cured spontaneously due to immunogenic tumors or from mice with no tumors at all because the cell line is unable to form tumors. One way to counter this is to re-passage the cells in mice by producing sub-cutaneous tumors. If this re-passaging is performed too frequently, overly aggressive tumors are generated. A fine balance is needed to determine when the cells need to be re-passaged. Generally, before a major series of experiments, the cell line is revived and then implanted in mice subcutaneously to confirm their ability to form tumors. The tumors are monitored for several weeks to ensure that there are no spontaneous cures. However, if spontaneous cures are observed, then the protocol in step 3 should be performed. Similarly, the ability of MB49-PSA cells to produce PSA should always be confirmed before the cells are used for tumor implantation.
Urinary PSA can be used to monitor the growth of bladder tumors established using MB49-PSA cells. However, a negative or "normal" urinary PSA value does not necessarily mean an absence of tumor cells, but only that less than 1 x 105 cells are present. As urinary PSA is determined around day 4 to day 7, mice that appear to have no tumor, based on the value of normal mice + 3 SD, can be removed from the experiment. Some of these mice may develop a tumor at a later date. Removing mice with no tumors ensures that tumors are very similar in size before commencing any therapy. This reduces variation due to tumor size in response to therapy. A major cause of tumor size variation is the clumping of cells before implantation, so efforts should be made to re-suspend cells before implantation.
However, when small numbers of mice are used, it may be necessary to keep all mice in the study, even if the tumors are not measurable by days 4 - 7. By monitoring PSA on day 11, it may still be possible to categorize these mice as having had small tumors, and end-point analysis can be performed with respect to the initial tumor size (based on the presence of measurable urinary PSA on days 4 - 7 versus day 11). The advantage of being able to quantify tumors with different PSA values is that all mice may be included in the study, and the response to therapy can be determined based on their PSA/creatinine values with respect to the original tumor size. Another point of concern is vesico-ureteral reflux. This can result in tumor development in the kidneys. Reducing the volume to be instilled from 100 µL to 50 µL and performing the instillation slowly reduces the likelihood of this occurring.
One problem associated with urine-based assays is the reduced urine collection observed as orthotopic tumors grow in the bladder. While urine can be easily collected from mice during the first few weeks after implantation, with time, the volume of urine collected may not be sufficient for PSA and creatinine measurements. The minimum volume of urine needed is 110 µL, but more is better. Thus, PSA readings may not be available for all mice at later time points. Also, lysis of red blood cells in urine gives falsely high reading on the PSA ELISA. A non-urine-based assay could overcome this problem. Unfortunately, though fluorescence imaging is simple to use, we found that the mouse feed had red fluorescence as well. This gave a high background against which the bladder could not be easily seen. It is possible that using a green fluorescent dye or protein may overcome this problem, as described by Sweeney et al.10 For both fluorescence and ultrasound, mice need to be shaved on the ventral surface.
Ultrasound images appear to be as good as PSA gene expression in locating tumors. However, the disadvantage of ultrasound imaging is that the bladder must be distended during imaging to get good tumor visualization. While the images are clear when the bladder tumor is large, it is hard to differentiate small tumors in mice from the absence of tumors. It has been reported that ultrasound can detect tumors around 1.5 mm in diameter22, but on day 4 after implantation, tumors are much smaller than this. Thus, this method may not be good for the detection of tumors on day 4. Table 1 compares the 3 different tumor monitoring systems; the PSA ELISA is the simplest to use and does not require small-animal imaging systems, which may not be available at all animal facilities.
Given the greater sensitivity of real-time PCR analysis of PSA gene expression, it can be used in the place of immunohistochemistry to confirm whether mice were cured when the experiment was terminated. With immunohistochemistry, a tumor of 0.2 - 0.3 mm is detectable by day 4 after implantation15. However, this is an end-point analysis method that cannot be used to monitor tumor implantation. In this study, MRI was not evaluated, but it has been reported to be able to identify the presence of tumors by day 10 after implantation8. By modifying cells to express the green florescent protein (GFP), it is possible to confirm tumor implantation by day 7. A combination of early urinary PSA to detect tumor implantation and real-time PCR analysis at termination provides confirmation of tumor implantation and therapeutic efficacy between different treatment groups.
A drawback of our protocol is mainly that the ELISA assay cannot confirm the presence of tumors when the number of cells present is less than 105 cells. Thus more sensitive assays need to be developed as well as faster assays to reduce the time needed for PSA detection. ELISA takes several hours to perform. A quick method such as the creatinine assay which is based on the Jaffe method23 and takes about 5 min to perform would greatly simplify monitoring of tumor growth. To this end, an enzyme-based method to detect PSA activity was evaluated, but it was not successful. The use of colloidal gold and nanoparticle based assay systems could reduce the time taken to perform the assay and increase the sensitivity24. In this regard, electrode based sensors and electrochemical based sensors using nanoparticles have been developed to assay human PSA25-27 and if the cost is reasonable may be applicable to the animal model. The assay system could also be improved by using a different protein secretion system such as GFP or luciferase where the assay is performed under optimal conditions in vitro rather than depending on in vivo imaging which is dependent on tissue oxygenation.
While chemical carcinogenesis in mice generates tumors with similarity to human cancers in terms of mutations28, they take longer to produce and are not as comparable in size between animals, requiring larger numbers of mice which increases the cost of experimentation. When targeting agents recognizing human proteins are to be evaluated, human xenografts implanted subcutaneously in nude or Severe combined immunodeficiency (SCID) mice is the only option. Though these models provide proof of concept of antibody recognition, the lack of an intact immune system hinders assessment of immune activation. The recent development of a humanized mouse model for bladder cancer using human xenografts29, does provide some immune insights, but as cells are implanted subcutaneously it does not actually recapitulate the human disease environment. It is technically difficult to produce orthotopic tumors in immune deficient mice. Thus the syngeneic orthotopic model despite its limitations is still a good model for the assessment and development of therapy for bladder cancer as it provides the correct tissue location enabling controlled exposure to therapy modelling the clinical situation and the ability to evaluate the impact of host immune cells during cancer therapy. All this combined with rapid tumor development in mice and the ability to monitor tumor growth results in a cost-effective model.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This work was funded by a grant from the National Medical Research Council of Singapore (NMRC/CIRG/1335/2012) awarded to Professor Kesavan Esuvaranathan.
References
- Gunther JH, et al. Optimizing syngeneic orthotopic murine bladder cancer (MB49) Cancer Res. 1999;59:2834–2837. [PubMed] [Google Scholar]
- Dobek GL, Godbey WT. An orthotopic model of murine bladder cancer. Journal of visualized experiments : JoVE. 2011. [DOI] [PMC free article] [PubMed]
- Chade DC, et al. Histopathological characterization of a syngeneic orthotopic murine bladder cancer model. Int Braz J Urol. 2008;34:220–226. doi: 10.1590/s1677-55382008000200013. [DOI] [PubMed] [Google Scholar]
- Chan ES, et al. Optimizing orthotopic bladder tumor implantation in a syngeneic mouse model. J Urol. 2009;182:2926–2931. doi: 10.1016/j.juro.2009.08.020. [DOI] [PubMed] [Google Scholar]
- Kasman L, Voelkel-Johnson C. An orthotopic bladder cancer model for gene delivery studies. Journal of visualized experiments : JoVE. 2013. p. e50181. [DOI] [PMC free article] [PubMed]
- Ninalga C, Loskog A, Klevenfeldt M, Essand M, Totterman TH. CpG oligonucleotide therapy cures subcutaneous and orthotopic tumors and evokes protective immunity in murine bladder cancer. J Immunother. 2005;28:20–27. doi: 10.1097/00002371-200501000-00003. [DOI] [PubMed] [Google Scholar]
- Tham SM, Ng KH, Pook SH, Esuvaranathan K, Mahendran R. Tumor and Microenvironment Modification during Progression of Murine Orthotopic Bladder Cancer. Clin Dev Immunol. 2011. p. 865684. [DOI] [PMC free article] [PubMed]
- Chin J, Kadhim S, Garcia B, Kim YS, Karlik S. Magnetic resonance imaging for detecting and treatment monitoring of orthotopic murine bladder tumor implants. J Urol. 1991;145:1297–1301. doi: 10.1016/s0022-5347(17)38618-4. [DOI] [PubMed] [Google Scholar]
- Kikuchi E, et al. Detection and quantitative analysis of early stage orthotopic murine bladder tumor using in vivo magnetic resonance imaging. J Urol. 2003;170:1375–1378. doi: 10.1097/01.ju.0000075504.13456.41. [DOI] [PubMed] [Google Scholar]
- Sweeney SK, Luo Y, O'Donnell MA, Assouline J. Nanotechnology and cancer: improving real-time monitoring and staging of bladder cancer with multimodal mesoporous silica nanoparticles. Cancer nanotechnology. 2016;7:3. doi: 10.1186/s12645-016-0015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M, et al. Noninvasive detection of bladder cancer in an orthotopic murine model with green fluorescence protein cytology. J Urol. 2003;170:975–978. doi: 10.1097/01.ju.0000073209.65128.c1. [DOI] [PubMed] [Google Scholar]
- Jurczok A, Fornara P, Soling A. Bioluminescence imaging to monitor bladder cancer cell adhesion in vivo: a new approach to optimize a syngeneic, orthotopic, murine bladder cancer model. BJU Int. 2008;101:120–124. doi: 10.1111/j.1464-410X.2007.07193.x. [DOI] [PubMed] [Google Scholar]
- Newton MR, et al. Anti-interleukin-10R1 monoclonal antibody in combination with bacillus Calmette--Guerin is protective against bladder cancer metastasis in a murine orthotopic tumour model and demonstrates systemic specific anti-tumour immunity. Clin Exp Immunol. 2014;177:261–268. doi: 10.1111/cei.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel AR, et al. Transabdominal micro-ultrasound imaging of bladder cancer in a mouse model: a validation study. Urology. 2010;75:799–804. doi: 10.1016/j.urology.2009.06.047. [DOI] [PubMed] [Google Scholar]
- Wu Q, Esuvaranathan K, Mahendran R. Monitoring the response of orthotopic bladder tumors to granulocyte macrophage colony-stimulating factor therapy using the prostate-specific antigen gene as a reporter. Clin Cancer Res. 2004;10:6977–6984. doi: 10.1158/1078-0432.CCR-04-0605. [DOI] [PubMed] [Google Scholar]
- Luo Y, Chen X, O'Donnell MA. Use of prostate specific antigen to measure bladder tumor growth in a mouse orthotopic model. J Urol. 2004;172:2414–2420. doi: 10.1097/01.ju.0000143860.50878.b1. [DOI] [PubMed] [Google Scholar]
- Coralli C, Cemazar M, Kanthou C, Tozer GM, Dachs GU. Limitations of the reporter green fluorescent protein under simulated tumor conditions. Cancer Res. 2001;61:4784–4790. [PubMed] [Google Scholar]
- Biot C, et al. Preexisting BCG-specific T cells improve intravesical immunotherapy for bladder cancer. Sci Transl Med. 2012;4(137):137ra172. doi: 10.1126/scitranslmed.3003586. [DOI] [PubMed] [Google Scholar]
- Swirski FK, et al. A near-infrared cell tracker reagent for multiscopic in vivo imaging and quantification of leukocyte immune responses. PLoS One. 2007;2:1075. doi: 10.1371/journal.pone.0001075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jozwicki W, Brozyna AA, Siekiera J, Slominski AT. Frequency of CD4+CD25+Foxp3+ cells in peripheral blood in relation to urinary bladder cancer malignancy indicators before and after surgical removal. Oncotarget. 2016. [DOI] [PMC free article] [PubMed]
- Walk EL, McLaughlin SL, Weed SA. High-frequency Ultrasound Imaging of Mouse Cervical Lymph Nodes. J Vis Exp. 2015. p. e52718. [DOI] [PMC free article] [PubMed]
- Rooks V, Beecken WD, Iordanescu I, Taylor GA. Sonographic evaluation of orthotopic bladder tumors in mice treated with TNP-470, an angiogenic inhibitor. Academic radiology. 2001;8:121–127. doi: 10.1016/s1076-6332(01)90038-8. [DOI] [PubMed] [Google Scholar]
- Folin O, Morris JL. On the determination of creatinine and creatine in urine. JBC. 1914;17:469–473. [Google Scholar]
- Dykman LA, Bogatyrev VA, Khlebtsov BN, Khlebtsov NG. A protein assay based on colloidal gold conjugates with trypsin. Anal Biochem. 2005;341:16–21. doi: 10.1016/j.ab.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Shi HW, et al. Joint enhancement strategy applied in ECL biosensor based on closed bipolar electrodes for the detection of PSA. Talanta. 2016;154:169–174. doi: 10.1016/j.talanta.2016.03.059. [DOI] [PubMed] [Google Scholar]
- Ma H, et al. Electrochemiluminescent immunosensing of prostate-specific antigen based on silver nanoparticles-doped Pb (II) metal-organic framework. Biosensors & bioelectronics. 2016;79:379–385. doi: 10.1016/j.bios.2015.12.080. [DOI] [PubMed] [Google Scholar]
- Kavosi B, Salimi A, Hallaj R, Moradi F. Ultrasensitive electrochemical immunosensor for PSA biomarker detection in prostate cancer cells using gold nanoparticles/PAMAM dendrimer loaded with enzyme linked aptamer as integrated triple signal amplification strategy. Biosensors & bioelectronics. 2015;74:915–923. doi: 10.1016/j.bios.2015.07.064. [DOI] [PubMed] [Google Scholar]
- Lu Y, et al. Cross-species comparison of orthologous gene expression in human bladder cancer and carcinogen-induced rodent models. Am J Transl Res. 2010;3:8–27. [PMC free article] [PubMed] [Google Scholar]
- Gong Z, et al. Establishment of a Novel Bladder Cancer Xenograft Model in Humanized Immunodeficient Mice. Cellular physiology and biochemistry : international journal of experimental cellular physiology, biochemistry, and pharmacology. 2015;37:1355–1368. doi: 10.1159/000430401. [DOI] [PubMed] [Google Scholar]


