Abstract
Free tissue transfer has been increasingly used in clinical practice since the 1970s, allowing reconstruction of complex and otherwise untreatable defects resulting from tumor extirpation, trauma, infections, malformations or burns. Free flaps are particularly useful for reconstructing highly complex anatomical regions, like those of the head and neck, the hand, the foot and the perineum. Moreover, basic and translational research in the area of free tissue transfer is of great clinical potential. Notwithstanding, surgical trainees and researchers are frequently deterred from using microsurgical models of tissue transfer, due to lack of information regarding the technical aspects involved in the operative procedures. The aim of this paper is to present the steps required to transfer a fasciocutaneous epigastric free flap to the neck in the rat.
This flap is based on the superficial epigastric artery and vein, which originates from and drain into the femoral artery and vein, respectively. On average the caliber of the superficial epigastric vein is 0.6 to 0.8 mm, contrasting with the 0.3 to 0.5 mm of the superficial epigastric artery. Histologically, the flap is a composite block of tissues, containing skin (epidermis and dermis), a layer of fat tissue (panniculus adiposus), a layer of striated muscle (panniculus carnosus), and a layer of loose areolar tissue.
Succinctly, the epigastric flap is raised on its pedicle vessels that are then anastomosed to the external jugular vein and to the carotid artery on the ventral surface of the rat's neck. According to our experience, this model guarantees the complete survival of approximately 70 to 80% of epigastric flaps transferred to the neck region. The flap can be evaluated whenever needed by visual inspection. Hence, the authors believe this is a good experimental model for microsurgical research and training.
Keywords: Medicine, Issue 119, Flap, Free Tissue Transfer, Free Flap, Rats, Epigastric Artery, Anatomy, Physiology, Animal Experimentation, Surgical Procedures, Teaching, Learning
Introduction
Free tissue transfer has been increasingly used in clinical practice for reconstructing missing tissues since the 1970s1-5. This has allowed reconstruction of complex and otherwise untreatable defects resulting from tumor extirpation, trauma, infections, malformations or burns1-7. Free flaps of this kind are particularly useful for reconstructing highly complex anatomical regions, like those of the head and neck, the hand, the foot, and the perineum1,4.
However, even today surgical trainees are frequently daunted by the complexity of several steps involved in raising, transferring and insetting a free flap with the use of microsurgical techniques and instruments8,9. In addition, it is widely accepted that to become a proficient microsurgeon, extensive experimental practice in an animal model is mandatory4,8-13.
Moreover, basic and translational research in the area of free tissue transfer is of great clinical potential8,14-16. Notwithstanding, researchers are frequently deterred from using microsurgical models of tissue transfer due to lack of information regarding the technical aspects involved in the operative procedures4,8-14. The rat is a good animal model for microsurgical research and training, as it is relatively inexpensive, easy to keep, and amenable to frequent manipulation8,11,13,14,17,18.
Although several free bone, muscle and skin flaps have been described in the rat18-24, the free epigastric fasciocutaneous flap is the most widely used for teaching purposes9,12,13,18,25. This free flap was first described in 1967 by Strauch and Murray and has gained increasing popularity ever since, due to several factors, namely constant vascular anatomy, relative ease of dissection, sizeable nutrient vessels, and redundancy of skin in the donor zone, which allows primary closure of the defect resulting from flap's elevation4,9-11,13,17,18,25-28.
Flap Anatomy and Histology The epigastric flap is supplied by the superficial epigastric artery and vein (Figure 1). These vessels originate from and drain into the femoral artery and vein, respectively. On average the caliber of the superficial epigastric vein is 0.6 to 0.8 mm, contrasting with the 0.3 to 0.5 mm of the superficial epigastric artery (Figure 2)17,18. The superficial epigastric artery gives off two main branches: a lateral and a medial branch that in turn divide multiple times, originating capillary networks that supply most of the integument of the epigastric region. These capillaries drain into the tributaries of the superficial epigastric veins that have a parallel course to the arterial tree (Figure 2)13,17,18. The diagram in Figure 3 represents the region of the ventrolateral abdominal wall supplied by the superficial epigastric vessels that can be mobilized in the epigastric flap. This flap can be up to 5 cm in length and 3 cm in width13,17,18.
Histologically, the flap is composed of the integument that covers the ventrolateral abdominal wall muscles (Figure 4)13,17,18. It contains a superficial layer of skin, formed by the dermis and epidermis. Beneath the skin there is a layer of fat tissue named panniculus adiposus. Below this layer there is another layer of striated muscle known as panniculus carnosus18,28,29. Below the panniculus carnosus there is loose areolar tissue which is superficial to the deep fascia that covers the larger abdominal muscles. Hence, the flap is a composite block of tissues, containing all these layers, except for the deep muscle fascia (Figure 5)13,17,18,27-31.
Protocol
All procedures involving animal subjects were approved by the Institutional Animal Care and Use Committee and Ethical Committee at Nova University Medical School, Lisbon, Portugal (08/2012/CEFCM).
1. Surgical Procedure Set-up Notes
Use adult Wistar rats weighing 250 to 350 g.
Keep the rats with food and water ad libitum with 12 hr light-dark cycles 7 days prior to surgery.
Weigh the rat in order to determine the amount of anesthetic required.
Autoclave all surgical instruments before surgery.
Layout all the surgical supplies and instruments needed for the procedure (see the Table of Materials).
Perform the surgery under an operating microscope using conventional and microsurgical instruments.
Position the homeothermic blanket, rectal probe, and heat lamp.
Place one 20 ml sterilized vial containing 0.9% saline in a water bath warmed to 37 ºC.
Wear sterilized gloves to disinfect all surfaces of the operating setting with an alcoholic solution. Remove the gloves.
Place a scrub cap and mask.
Disinfect hands with water and soap and wear another pair of sterilized gloves.
Wear a sterile surgical gown.
2. Anesthesia and Skin Preparation
NOTE: Have an assistant help with the following four steps, as a sterile gown and gloves are worn.
Anesthetize the rat with a mixture of Ketamine and Diazepam given intraperitoneally. The dose is 5 mg/kg ketamine and 0.25 mg/kg diazepam. Judge the depth of anesthesia by toe pinch and by observance of respiration rate throughout the entire procedure8,14,15,32.
Apply an ophthalmic gel over the anterior surface of the eyes to avoid corneal abrasion.
Remove the hair over the ventral surface of the abdomen with a depilatory cream. After hair removal, remove the depilatory cream with warm saline.
Spray a substantial amount of alcoholic solution over the operative site. Leave the product on the operative site and do not wipe it off. Wait at least 15 sec. Repeat the application 3 times. Leave a contact time of at least 2 min before proceeding with the surgery. Other research units use other protocols to prevent surgical site infection.
Wearing sterilized gloves, place 2 surgical drapes on both sides of the rat.
3. Donor Site Surgical Procedure
- Set the boundaries of an epigastric flap ranging approximately 5 cm in length and 3 cm width.
- Using a surgical skin marker, draw a line from the xiphoid process of the sternum to the pubic symphysis, in order to mark the midline over the ventral surface of the rat's abdomen.
- On the left side of the rat, using a surgical skin marker, draw two perpendicular lines to the first line: one crossing immediately caudal to the thoracic cage, and another one, parallel to the latter and just cranial to the groin fold (Figures 3 and 6).
- Mark the lateral incision with a surgical skin marker with a line parallel to the midline and around 3 cm apart from it.
- Flap harvesting
- Incise the skin with a number 15 scalpel blade until reaching the panniculus carnosus layer.
- Deeper to the panniculus carnosus plane, make the incision with an electric cautery until reaching the muscle fascia.
- Raise the flap from medial to lateral and from cranial to caudal, exposing the flap's pedicle.
- Carefully ligate and divide the perforating vessels coming up from the deep muscle layer and going into the flap's deep surface.
- Place a retractor in the caudal aspect of the flap and dissect the flap's pedicle cautiously by gently teasing away the loose surrounding tissues (Figure 7).
- Ligate and divide the lateral femoral circumflex artery and vein using 9/0 Nylon for the ligatures.
- Isolate the femoral artery and vein. When present, ligate (using 9/0 Nylon) and divide branches of these vessels to adjacent muscles.
- Firstly, use a double vascular clamp to clamp the proximal aspect of the femoral vein. Subsequently clamp its distal aspect. Then, clamp the distal aspect of the femoral artery and finally its proximal aspect.
- Clamp the distal aspect of the femoral artery and finally its proximal aspect.
- Place a single vascular clamp in the superficial epigastric vein and another one in the superficial epigastric artery. Use a pair of straight microsurgery scissors to cut the superficial epigastric artery and vein at their origin and termination, respectively.
- Copiously irrigate the lumen of these vessels with heparinized normal saline 10 IU/ml, until no blood or debris are seen inside the vessels' lumen33.
- Pull and trim a cuff of adventitia close to the vascular section sites.
- Transfer the epigastric flap to the neck using Addison's forceps (Figure 8).
- Close the donor site with subcuticular interrupted 5/0 absorbable stitches.
- Close the skin with interrupted 5/0 Nylon stitches.
4. Recipient Site Surgical Procedure
- Exposure of Recipient Site Vessels
- Using a surgical skin marker, draw a line over the medial border of the left sternocleidomastoid (SCM) muscle.
- Using a surgical skin marker, draw another line immediately cranial and parallel to the left clavicle. These two lines must converge at the left sternoclavicular joint.
- Incise the skin using a number 15 scalpel blade.
- Use an electric cautery to cut through the subcutaneous tissue.
- Use a pair of dissecting scissors to skeletonize the external jugular vein lateral to the SCM muscle.
- Isolate and ligate the tributaries of the external jugular in this (Figure 9).
- Ligate the external jugular vein just below the mandible with a 9/0 Nylon suture.
- Place a single venous clamp beneath the latter ligation and cut the external jugular vein using a pair of straight microsurgery scissors.
- Wash the lumen of the vein with heparinized normal saline in a concentration of 10 IU/ml.
- Isolate the medial margin of the SCM muscle and retract this muscle laterally, thus exposing the carotid artery and the vagus nerve (Figure 10).
- Make a transverse incision in the middle third of the SCM muscle using the electric cautery.
- Place a retractor between the deep surface of the SCM muscle and the strap muscles.
- Tease away the vagus nerve from the carotid artery, taking care not to damage these structures.
- Vascular anastomoses
- Position a double arterial clamp in the carotid artery.
- Place a 9/0 Nylon stitch in the lateral aspect of the carotid artery, and use this stitch to pull this part of the vessel wall.
- Use a pair of straight microsurgery scissors to produce an opening in this region of vessel wall.
- Using interrupted 10/0 Nylon sutures perform a termino-lateral anastomosis between the superficial epigastric artery of the flap and the carotid artery at the level of the recently created carotid opening.
- Approach the proximal stump of the external jugular vein and the superficial epigastric vein and inspect the caliber of these two veins.
- If the discrepancy in size is slight to moderate, dilate the lumen of the cut end of the superficial epigastric vein using dilation forceps.
- If the caliber difference is very pronounced, in addition to forceps dilation, bevel the end of the superficial epigastric vein in a 30 to 45° angle.
- Perform the venous anastomosis, using interrupted 11/0 Nylon sutures.
- Remove the single clamps placed onto the flap's vessels.
- Remove the double clamp positioned in the femoral vein.
- Remove the double clamp placed in the femoral artery.
- Assess patency and competency of anastomoses
- Verify if the flap's artery and vein are fully dilated and no significant bleeding is observed after 3 min of removing the vascular clamps (Figure 11).
- If there is bleeding during this period place a moist saline gauze over the anastomosis and apply gentle pressure.
- If bleeding from anastomoses does not stop after 3 min, add additional 11/0 Nylon interrupted sutures, after vascular clamp placement, as needed.
- Wait 10 min with the flap connected to the neck vessels and wrapped by a gauze moistened in warm saline.
- Assess flap's perfusion and neck wound hemostasis. Inspect the anastomoses for signs of hemorrhage, thrombosis or excessive traction.
- Secure the flap in the recipient site starting with 5/0 subcuticular interrupted sutures.
- Close the skin with 5/0 Nylon interrupted sutures (Figure 12).
5. Post-operative Care
Leave the rat to recover inside its individual cage in the right lateral decubitus position. Keep the cage warm by placing an electric heat pad set on low beneath. Place a light cloth between the cage and the electric heat pad to avoid hyperthermia.
Watch the animal continuously turning it to the opposite lateral decubitus every 5 min, until it resumes sternal recumbency and it is able to ambulate.
House the rats individually until removing the surgical stitches two weeks after the surgical procedure.
Give an anti-inflammatory drug 1 mg/kg subcutaneously once a day for the 3 days following surgery, for postoperative analgesia.
6. Flap Assessment
Present a food treat over the head of the rat and assess flap's viability by visual inspection.
If exposure is insufficient using the previous step, have an assistant applying gentle touch over the interscapular region of the rat, while examining the flap.
Use digital photography and ImageJ software to quantitatively evaluate the areas of wound dehiscence, flap epidermolysis, hyperemia, congestion and/or necrosis, as explained in detail by Trujillo et al.15.
Representative Results
According to the authors' experience of more than ten years using the epigastric free flap as a model of free tissue transfer both in the context of microsurgery courses and for research purposes, the rate of flap survival depends somewhat on the dexterity and experience of the surgeon. Generally speaking, if the technical aspects described above are taken into consideration, a nearly complete survival rate (<10% of flap necrosis) of around 70% of flaps is to be expected. Around 10% of flaps present partial necrosis (10 to 50%). About 20% of flaps suffer complete necrosis. An 80% nearly complete survival rate was obtained in the last 20 procedures performed by the first author (D.C.) (Figure 13).
During the first two days postoperatively, the free epigastric flap is often edematous and presents some degree of venous congestion. These usually both subside gradually between 3 and 5 days after surgery. Typically, during the first week, the rat removes most external stitches and part of the subcuticular sutures, often resulting in scattered areas of slight wound dehiscence (Figure 14). After day 10, the hair slowly starts to grow on the flap's surface. At the end of the first month after surgery, the flap is usually covered with slightly shorter hair than the adjacent skin. Two months postoperatively, the presence of the flap is heralded by a slight lump, and by a relatively inconspicuous scar around the flap's margins (Figure 14). Auto cannibalism of the flap is an infrequent finding that, in the authors' experience, occurs almost exclusively in cases of total flap necrosis.
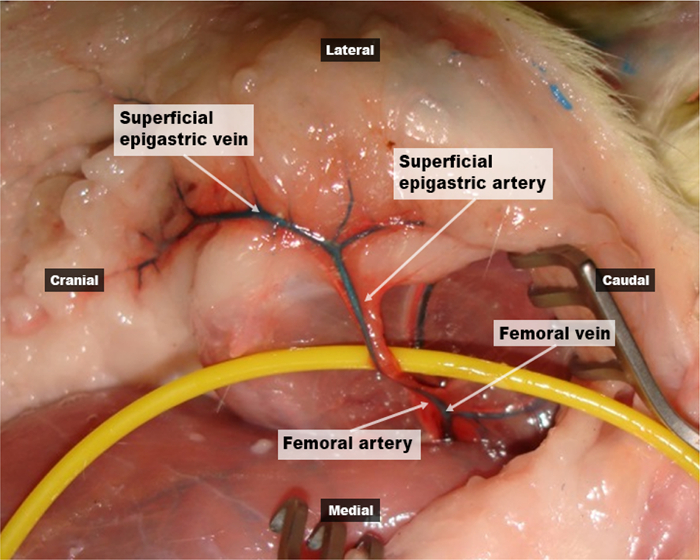 Figure 1:Vascular anatomy of the epigastric free flap. This photograph shows the left epigastric region of a rat previously injected with a red latex solution in the arterial system and with a blue latex solution in the venous system. It is possible to observe that the epigastric region receives an axial blood supply from the superficial epigastric artery and vein. These vessels originate from and drain into the femoral artery and vein, respectively. Please click here to view a larger version of this figure.
Figure 1:Vascular anatomy of the epigastric free flap. This photograph shows the left epigastric region of a rat previously injected with a red latex solution in the arterial system and with a blue latex solution in the venous system. It is possible to observe that the epigastric region receives an axial blood supply from the superficial epigastric artery and vein. These vessels originate from and drain into the femoral artery and vein, respectively. Please click here to view a larger version of this figure.
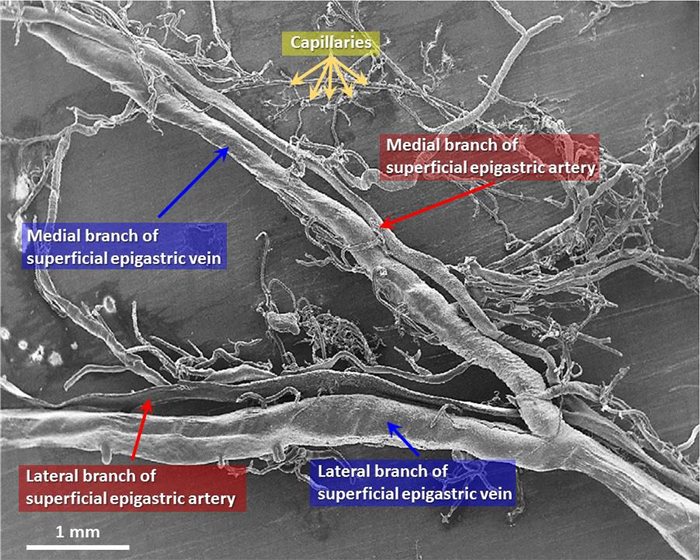 Figure 2:Scanning electron microscopy image of a corrosion cast of the superficial epigastric vessels showing the microscopic vascular blood supply to the epigastric free flap. This scanning electron microscopy image of a corrosion cast of the superficial epigastric vessels of the rat shows that the vein has a larger caliber that the artery. On average the caliber of the superficial epigastric vein is 0.6 to 0.8 mm, compared with the 0.3 to 0.5 mm of the superficial epigastric artery. This image also shows that the superficial epigastric artery originates two main branches: a lateral and a medial branch that in turn divide multiple times, originating capillary networks that supply most of the epigastric region. These capillaries drain into the tributaries of the superficial epigastric vein that have a parallel course to the arterial tree. Please click here to view a larger version of this figure.
Figure 2:Scanning electron microscopy image of a corrosion cast of the superficial epigastric vessels showing the microscopic vascular blood supply to the epigastric free flap. This scanning electron microscopy image of a corrosion cast of the superficial epigastric vessels of the rat shows that the vein has a larger caliber that the artery. On average the caliber of the superficial epigastric vein is 0.6 to 0.8 mm, compared with the 0.3 to 0.5 mm of the superficial epigastric artery. This image also shows that the superficial epigastric artery originates two main branches: a lateral and a medial branch that in turn divide multiple times, originating capillary networks that supply most of the epigastric region. These capillaries drain into the tributaries of the superficial epigastric vein that have a parallel course to the arterial tree. Please click here to view a larger version of this figure.
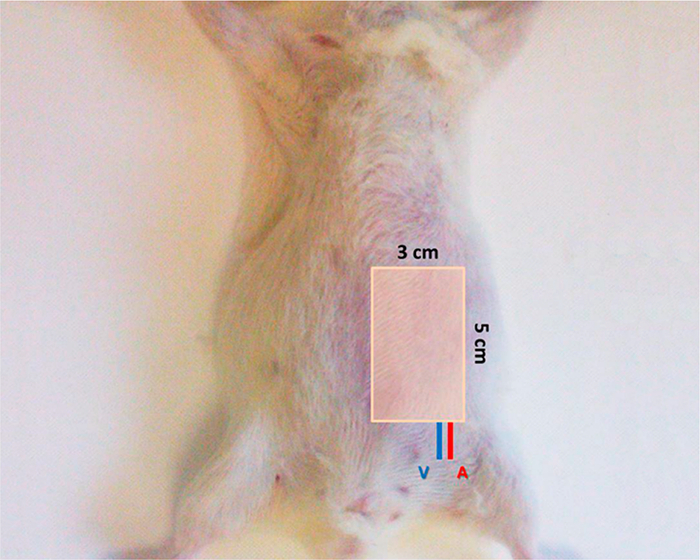 Figure 3: Potential area of a left epigastric free flap in the rat. This diagram represents the region of the abdominal wall supplied by the superficial epigastric vessels and that can be mobilized in the epigastric flap. This flap can be up to 5 cm in length and 3 cm in width. Please click here to view a larger version of this figure.
Figure 3: Potential area of a left epigastric free flap in the rat. This diagram represents the region of the abdominal wall supplied by the superficial epigastric vessels and that can be mobilized in the epigastric flap. This flap can be up to 5 cm in length and 3 cm in width. Please click here to view a larger version of this figure.
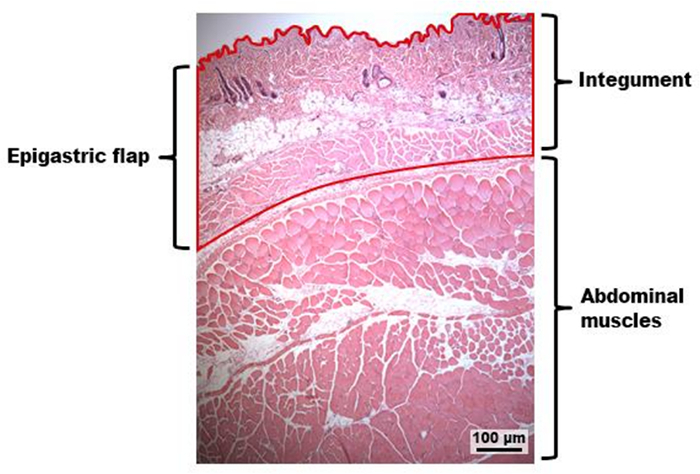 Figure 4:Photograph of a hematoxilin-eosin stained section of the epigastric flap. This hematoxilin-eosin stained section of the epigastric region shows that the epigastric flap is composed of the integument of this region that covers the abdominal wall muscles. Please click here to view a larger version of this figure.
Figure 4:Photograph of a hematoxilin-eosin stained section of the epigastric flap. This hematoxilin-eosin stained section of the epigastric region shows that the epigastric flap is composed of the integument of this region that covers the abdominal wall muscles. Please click here to view a larger version of this figure.
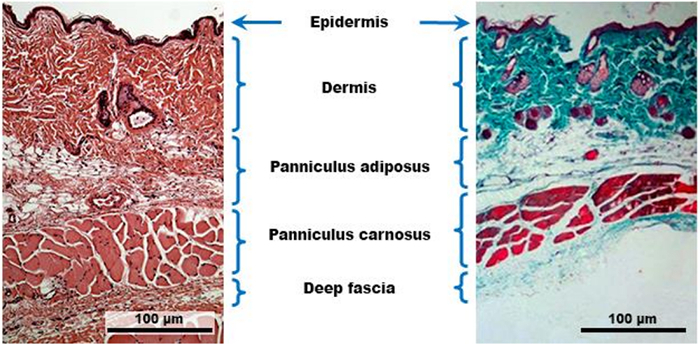 Figure 5:Histological composition of the epigastric flap. The photograph on the left side represents a hematoxilin-eosin stained section of an epigastric flap, whereas the photograph on the right side was obtained from a Masson's trichrome section of this flap. These two pictures illustrate that the epigastric flap of the rat is a composite block of tissues. It contains a superficial layer of skin, formed by the dermis and epidermis. Beneath the skin there is a layer of fat tissue named panniculus adiposus. Below this layer there is layer of striated muscle known as panniculus carnosus. Below the panniculus carnosus there is a deep fascia that covers the larger and deeper abdominal muscles. Please click here to view a larger version of this figure.
Figure 5:Histological composition of the epigastric flap. The photograph on the left side represents a hematoxilin-eosin stained section of an epigastric flap, whereas the photograph on the right side was obtained from a Masson's trichrome section of this flap. These two pictures illustrate that the epigastric flap of the rat is a composite block of tissues. It contains a superficial layer of skin, formed by the dermis and epidermis. Beneath the skin there is a layer of fat tissue named panniculus adiposus. Below this layer there is layer of striated muscle known as panniculus carnosus. Below the panniculus carnosus there is a deep fascia that covers the larger and deeper abdominal muscles. Please click here to view a larger version of this figure.
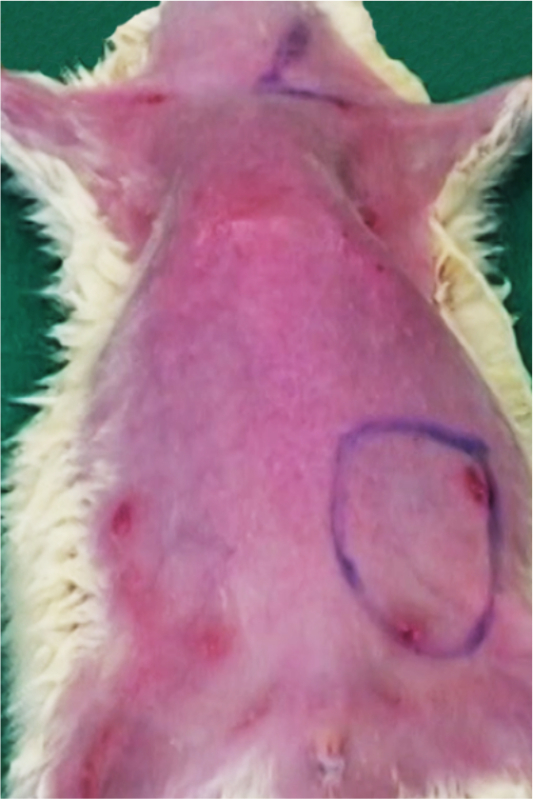 Figure 6. Pre-operative skin markings on the ventral surface of the rat prior to surgery. This photograph illustrates the skin markings for the incisions used to raise the left epigastric flap and subsequently to inset this flap in the ventral aspect of the left cervical region.
Figure 6. Pre-operative skin markings on the ventral surface of the rat prior to surgery. This photograph illustrates the skin markings for the incisions used to raise the left epigastric flap and subsequently to inset this flap in the ventral aspect of the left cervical region.
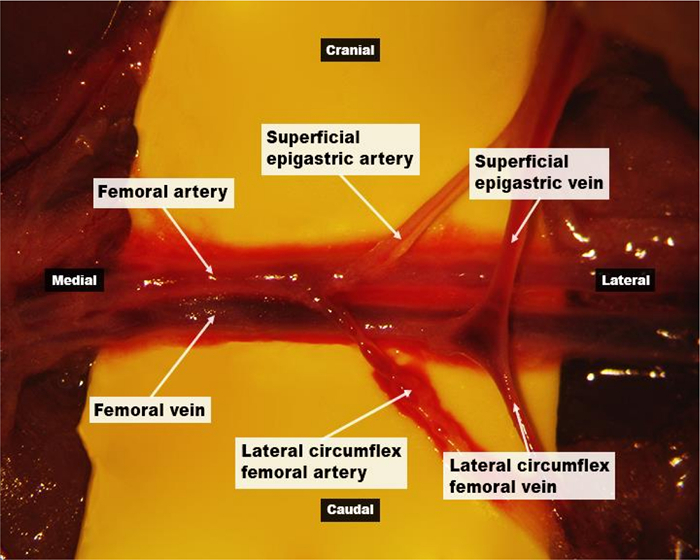 Figure 7.Surgical anatomy of the epigastric flap's nutrient vessels under the operating microscope (10X magnification). This photograph shows the superficial epigastric artery and vein originating from and draining into the femoral artery and vein, respectively. The lateral femoral circumflex artery usually arises from the caudal aspect of the superficial epigastric artery. The lateral femoral circumflex vein has a similar path and usually terminates into the superficial epigastric vein. Please click here to view a larger version of this figure.
Figure 7.Surgical anatomy of the epigastric flap's nutrient vessels under the operating microscope (10X magnification). This photograph shows the superficial epigastric artery and vein originating from and draining into the femoral artery and vein, respectively. The lateral femoral circumflex artery usually arises from the caudal aspect of the superficial epigastric artery. The lateral femoral circumflex vein has a similar path and usually terminates into the superficial epigastric vein. Please click here to view a larger version of this figure.
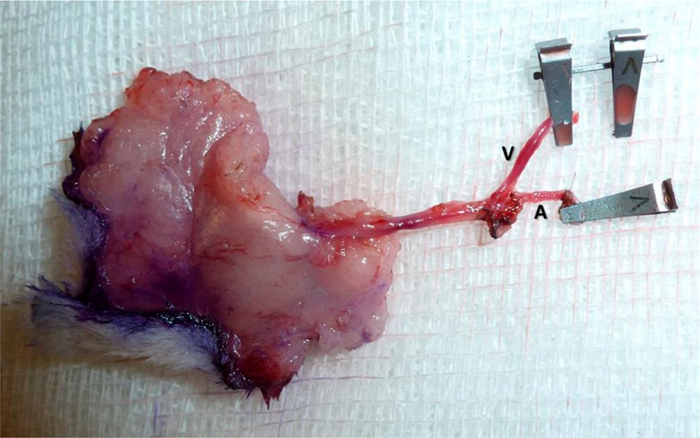 Figure 8.
The epigastric flap
ex vivo
pedicled on its nutrient vessels (the superficial epigastric artery and vein
-
A, V, respectively).
Please click here to view a larger version of this figure.
Figure 8.
The epigastric flap
ex vivo
pedicled on its nutrient vessels (the superficial epigastric artery and vein
-
A, V, respectively).
Please click here to view a larger version of this figure.
 Figure 9. Operating view of the dissection of the recipient vein, i.e., the external jugular vein, on the left side of the neck (6x magnification). It is possible to observe the subcutaneous course of the external jugular vein lateral to the sternocleidomastoid muscle. Please click here to view a larger version of this figure.
Figure 9. Operating view of the dissection of the recipient vein, i.e., the external jugular vein, on the left side of the neck (6x magnification). It is possible to observe the subcutaneous course of the external jugular vein lateral to the sternocleidomastoid muscle. Please click here to view a larger version of this figure.
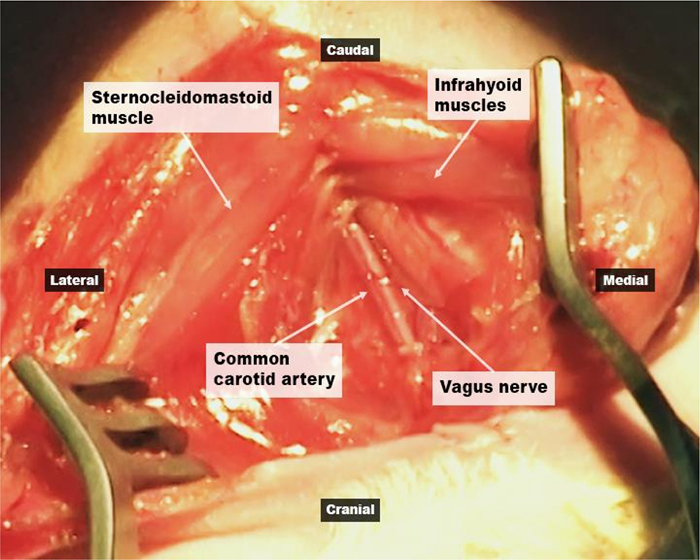 Figure 10. Operating view of the dissection of the donor artery, i.e., the common carotid, on the left side of the neck (10x magnification). The artery and accompanying vagus nerve are exposed after retracting the sternocleidomastoid and the infrahyoid muscles, as shown. Please click here to view a larger version of this figure.
Figure 10. Operating view of the dissection of the donor artery, i.e., the common carotid, on the left side of the neck (10x magnification). The artery and accompanying vagus nerve are exposed after retracting the sternocleidomastoid and the infrahyoid muscles, as shown. Please click here to view a larger version of this figure.
 Figure 11. Photograph of the vascular anastomoses between the flap's vessels and the recipient vessels in the neck, as seen under the operating microscope (10x magnification). This photograph shows the termino-lateral anastomosis between the common carotid and the superficial epigastric arteries. It is also possible to observe the termino-terminal anastomosis between the superficial epigastric and the external jugular veins. Please click here to view a larger version of this figure.
Figure 11. Photograph of the vascular anastomoses between the flap's vessels and the recipient vessels in the neck, as seen under the operating microscope (10x magnification). This photograph shows the termino-lateral anastomosis between the common carotid and the superficial epigastric arteries. It is also possible to observe the termino-terminal anastomosis between the superficial epigastric and the external jugular veins. Please click here to view a larger version of this figure.
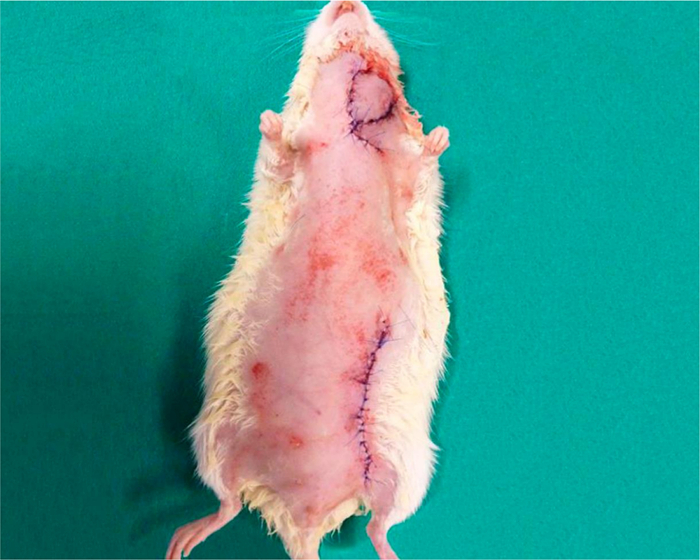 Figure 12. Photograph of ventral aspect of the rat immediately after the surgery. Notice that the donor zone is easily closed primarily. Please click here to view a larger version of this figure.
Figure 12. Photograph of ventral aspect of the rat immediately after the surgery. Notice that the donor zone is easily closed primarily. Please click here to view a larger version of this figure.
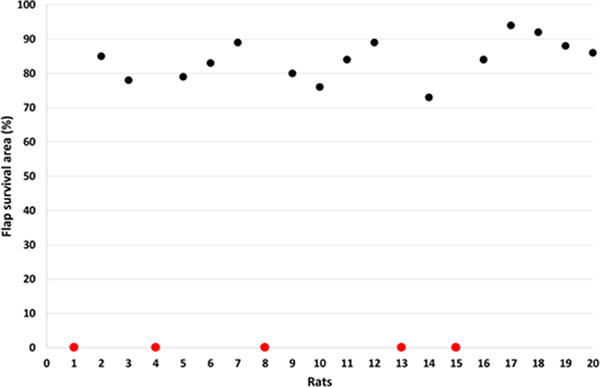 Figure 13.Epigastric free flap survival in 20 consecutive rats operated on by the first author (D.C.). Five rats (20%) presented complete flap necrosis (cases 1, 4, 8, 13 and 15, represented by the red dots). Areas of flap necrosis were determined using the free software ImageJ, as explained in detail by Trujillo et al.15. Please click here to view a larger version of this figure.
Figure 13.Epigastric free flap survival in 20 consecutive rats operated on by the first author (D.C.). Five rats (20%) presented complete flap necrosis (cases 1, 4, 8, 13 and 15, represented by the red dots). Areas of flap necrosis were determined using the free software ImageJ, as explained in detail by Trujillo et al.15. Please click here to view a larger version of this figure.
 Figure 14. Photographs of the epigastric flap placed on the ventral aspect of the neck 4, 14 and 60 days postoperatively. Four days after surgery, there is typically some wound dehiscence, as the rat removes the stitches. However, the flap usually remains in place. It is possible to examine the flap daily by simple visual inspection. Please click here to view a larger version of this figure.
Figure 14. Photographs of the epigastric flap placed on the ventral aspect of the neck 4, 14 and 60 days postoperatively. Four days after surgery, there is typically some wound dehiscence, as the rat removes the stitches. However, the flap usually remains in place. It is possible to examine the flap daily by simple visual inspection. Please click here to view a larger version of this figure.
Discussion
The most important aspect to obtain consistent flap survival is paying attention to detail in various steps of the microsurgical technique. For example, to obtain good visualization of the vessels, of the surgical instruments and of the fine suture lines, it is very helpful to place underneath the vessels, a sterilized colored plastic background. As many researchers, we prefer to use sterilized fragments of yellow or green balloons (Figures 7 and 11). This background provides the additional advantage of minimizing adherence of suture lines to the adjacent structures, which sometimes leads to the need of pulling the suture line with too much tension, which may in turn lead to vascular tearing. Finally, the use of a background has the additional advantage of decreasing the probability of inadvertently dragging potential thrombogenic tissue debris to the anastomosis site.
Considering that the flap's vessels are very fine and fragile, it is important not to pinch the entire width of the vessels, in order to avoid intimal lesion that, in turn, will lead to intravascular thrombosis and flap failure. To prevent inadvertent injury to both the flap's vessels and to the recipient site's vessels, it is safer to liberally ligate and divide neighboring tributaries, which will allow an easier manipulation of these vessels.
Before starting the anastomoses, it is vital to place the vessels in their definitive position, striving to prevent vascular kinking or torsion of the flap's pedicle. Given the small caliber and delicate consistency of the vessels, these are often difficult to exclude unequivocally. One helpful trick is to secure the flap in its final position with 3 stitches placed away from the site of the anastomoses. Next, if in doubt, temporarily open the vascular clamps placed at the flap's pedicle, and fill the vessels' lumen with heparinized normal saline in a concentration of 10 IU/mL until they become engorged. This leads vessels to assume the configuration they will present after being perfused by blood, as when the clamps are removed after anastomoses completion.
Moreover, it is of paramount importance to detect any air bubbles, even if small, inside the vessels during the entire procedure and particularly before tying the final stitches. If these bubbles are distant from the vascular section, the vessels can be milked gently with microsurgical forceps. If they are located close to the anastomotic sites, simple irrigation leads the less dense bubbles to be easily expelled from the vascular lumen. Failure to acknowledge the presence of air bubbles can cause irreversible flap ischemia and necrosis, no doubt due to the fine caliber of the flap vessels.
Additionally, it cannot be overemphasized the need for meticulous care while passing and tying the stitches, in order to: include the three layers of the vessels (intima, media and adventitia); obtain good vessel eversion to ensure adequate intimal contact, which is vital to anastomosis sealing and endothelial regrowth; avoid loose vascular contact, which will result in anastomotic incompetence, i.e., bleeding; and avoid grabbing too much vascular tissue, which will lead to anastomosis stenosis and proclivity to thrombosis, which in turn will result in venous congestion or poor flap perfusion, if the vein or artery are involved, respectively.
Finally, it is essential to ensure perfect hemostasis, during the entire procedure, especially when raising the flap in its deep surface. Otherwise hematoma formation and rat death are likely to ensue.
Modifications and troubleshooting of the technique
The authors observed that making a transverse incision in the middle portion of the SCM using an electric cautery, not only allows a better exposure of the carotid artery, but also minimizes the risk of undue tension over the future arterial anastomosis.
Another important technical tip is to start the anastomosis from the vessels' back wall, in order to minimize the risk of unwillingly catching this wall when placing the stitches in the more easily exposed front wall. If the back wall is sutured to the anterior aspect of the anastomosis, lack of vascular patency will almost invariably result either immediately due to mechanical reasons or after only a few hours as a result of thrombosis8.
If the anastomoses of the epigastric vessels of the rat are considered too technically challenging due to the small caliber of these vessels, the femoral vessels can be ligated distal to the origin of the epigastric vessels and used as the vascular pedicle of the epigastric flap. In this way, larger vessels will be used (the femoral artery has a caliber of 1.0 to 1.2 mm; and the femoral vein has a caliber of 1.2 to 1.5 mm). Moreover, by dissecting and ligating the other tributaries of the femoral vessels, a vascular pedicle length of over 2 cm can be obtained, which will facilitate flap insetting18,34,35.
Reproducibility
Our experience of more than ten years of using this flap for teaching and research purposes strongly suggests that the rat epigastric flap is a reproducible model of free tissue transfer11,13,17,18,26. It can be easily incorporated in microsurgical courses, as it is a good teaching and training model for microsurgery trainees11,13,17,18,26. In our experience, although technically challenging in the beginning for the novice in microsurgery, after some training, the free epigastric flap can be successfully transferred to the neck of the rat with minimal to no subsequent necrosis in 70 to 80% of cases. These results concur with those generally reported in the literature13,18,36.
Significance with respect to existing methods
Numerous free flaps have been described in the rat10,16,18,37-39. The most commonly used for teaching and research purposes have been the transverse rectus abdominis myocutaneous flap, the latissimus dorsi and serratus anterior muscle flaps, the hind limb replantation model, and the epigastric (groin) flap18,35. These flaps have been favored, due to their consistent anatomy and sizeable vascular pedicle. The epigastric flap is arguably the one associated with lesser donor site morbidity, as it dissected above the muscle fascia18. Moreover, the epigastric flap, described in 1967, was the first flap to be described in rats34,35. This occurred only 4 years after the first description of an experimental flap in an animal by Goldwyn. Interestingly, this flap was a groin flap in the dog34.
Limitations of the technique
The two main limitations of this model are the need for microsurgical skills in order to carry out the surgery, and the presence of significant necrosis in 20 to 25% of cases, according to different authors13,18,36. Another potential limitation of the model herein presented is the auto cannibalism of the flap. However, as the authors above, this is an infrequent finding that almost only occurs in cases of total flap necrosis.
Future applications of the technique
The rat epigastric free flap can be used in experimental studies of tissue perfusion, tissue repair and surgical wound infection40,41. Its nutrient vessels are particularly suitable for intravascular injection of solutions containing substances of interest, namely drugs, viral vectors or liposomes, that will mostly produce a local or regional effect30,31. In addition, beneath the flap, pathogens, foreign bodies, radioactive seeds or chemicals can also be placed, mimicking several disease processes and potential treatments30,31.
Disclosures
The authors have nothing to disclose.
Acknowledgments
One of the authors (Diogo Casal) received a grant from The Program for Advanced Medical Education, which is sponsored by Fundação Calouste Gulbenkian, Fundação Champalimaud, Ministério da Saúde e Fundação para a Ciência e Tecnologia, Portugal.
The authors would like to thank the technical help of Mr. Alberto Severino in filming and editing the video. The authors are also grateful to Mr. Octávio Chaveiro, Mr. Marco Costa and Mr. Carlos Lopes for their help in preparing the animal specimens presented in this paper.
Finally, the authors would like to thank Ms. Gracinda Menezes for her help in all the logistical aspects pertaining to animal acquisition and maintenance.
References
- Morain WD. In: Plastic Surgery. Mathes SJ, editor. Vol. 1. Saunders; 2006. pp. 27–34. [Google Scholar]
- Christoforou D, Alaia M, Craig-Scott S. Microsurgical management of acute traumatic injuries of the hand and fingers. Bull Hosp Jt Dis. 2013;71(1):6–16. [PubMed] [Google Scholar]
- Santoni-Rugiu P, Sykes PJ. In: A History of Plastic Surgery. Santoni-Rugiu P, Sykes PJ, editors. Springer; 2007. pp. 79–119. 3. [Google Scholar]
- Tamai S. In: Experimental and Clinical Reconstructive Microsurgery. Tamai S, Usui M, Yoshizu T, editors. Springer-Verlag; 2003. pp. 3–24. Ch. 1. [Google Scholar]
- Bettencourt-Pires MA, et al. Anatomy and grafts - From Ancient Myths, to Modern Reality. Arch Anat. 2014;2(1):88–107. [Google Scholar]
- Casal D, Gomez MM, Antunes P, Candeias H, Almeida MA. Defying standard criteria for digital replantation: A case series. Int J Surg Case Rep. 2013;4(7):597–602. doi: 10.1016/j.ijscr.2013.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez MM, Casal D. Reconstruction of large defect of foot with extensive bone loss exclusively using a latissimus dorsi muscle free flap: a potential new indication for this flap. J Foot Ankle Surg. 2012;51(2):215–217. doi: 10.1053/j.jfas.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Plenter RJ, Grazia TJ. Murine heterotopic heart transplant technique. J Vis Exp. 2014. [DOI] [PMC free article] [PubMed]
- Pichierri A, et al. How to set up a microsurgical laboratory on small animal models: organization, techniques, and impact on residency training. Neurosurg Rev. 2009;32(1):101–110. doi: 10.1007/s10143-008-0154-4. [DOI] [PubMed] [Google Scholar]
- Klein I, Steger U, Timmermann W, Thiede A, Gassel HJ. Microsurgical training course for clinicians and scientists at a German University hospital: a 10-year experience. Microsurgery. 2003;23(5):461–465. doi: 10.1002/micr.10180. [DOI] [PubMed] [Google Scholar]
- Fukui A. In: Experimental and Clinical Reconstructive Microsurgery. Tamai S, Usui M, Yoshizu T, editors. Springer-Verlag; 2004. pp. 35–43. Ch. 1. [Google Scholar]
- Ad-El DD, Harper A, Hoffman LA. Digital replantation teaching model in rats. Microsurgery. 2000;20(1):42–44. doi: 10.1002/(sici)1098-2752(2000)20:1<42::aid-micr8>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Ruby LK, Greene M, Risitano G, Torrejon R, Belsky MR. Experience with epigastric free flap transfer in the rat: technique and results. Microsurgery. 1984;5(2):102–104. doi: 10.1002/micr.1920050211. [DOI] [PubMed] [Google Scholar]
- Edmunds MC, Wigmore S, Kluth D. In situ transverse rectus abdominis myocutaneous flap: a rat model of myocutaneous ischemia reperfusion injury. J Vis Exp. 2013. [DOI] [PMC free article] [PubMed]
- Trujillo AN, Kesl SL, Sherwood J, Wu M, Gould LJ. Demonstration of the rat ischemic skin wound model. J Vis Exp. 2015. [DOI] [PMC free article] [PubMed]
- Siemionow MZ. In: Plastic and Reconstructive Surgery: Experimental models and research designs. Siemionow MZ, editor. Springer - Verlag; 2015. pp. 3–67. Ch. 1-7. [Google Scholar]
- Petry JJ, Wortham KA. The anatomy of the epigastric flap in the experimental rat. Plast Reconstr Surg. 1984;74(3):410–413. doi: 10.1097/00006534-198409000-00014. [DOI] [PubMed] [Google Scholar]
- Hirase Y. Tamai S, Usui M, Yoshizu T. Experimental and Clinical Reconstructive Microsurgery. Vol. 6. Springer-Verlag; 2004. pp. 111–114. Ch. 6. [Google Scholar]
- Zhang F, et al. Microvascular transfer of the rectus abdominis muscle and myocutaneous flap in rats. Microsurgery. 1993;14(6):420–423. doi: 10.1002/micr.1920140614. [DOI] [PubMed] [Google Scholar]
- Tonken HP, et al. Microvascular transplant of the gastrocnemius muscle in rats. Microsurgery. 1993;14(2):120–124. doi: 10.1002/micr.1920140207. [DOI] [PubMed] [Google Scholar]
- Miyamoto S, et al. Free pectoral skin flap in the rat based on the long thoracic vessels: a new flap model for experimental study and microsurgical training. Ann Plast Surg. 2008;61(2):209–214. doi: 10.1097/SAP.0b013e318157a6ea. [DOI] [PubMed] [Google Scholar]
- Nasir S, Aydin A, Kayikcioglu A, Sokmensuer C, Cobaner A. New experimental composite flap model in rats: gluteus maximus-tensor fascia lata osteomuscle flap. Microsurgery. 2003;23(6):582–588. doi: 10.1002/micr.10212. [DOI] [PubMed] [Google Scholar]
- Coskunfirat OK, Islamoglu K, Ozgentas HE. Posterior thigh perforator-based flap: a new experimental model in rats. Ann Plast Surg. 2002;48(3):286–291. doi: 10.1097/00000637-200203000-00010. [DOI] [PubMed] [Google Scholar]
- Ozkan O, et al. A new flap model in rats: iliac osteomusculocutaneous flap. Ann Plast Surg. 2001;47(2):161–167. doi: 10.1097/00000637-200108000-00009. [DOI] [PubMed] [Google Scholar]
- Padubidri AN, Browne E. Modification in flap design of the epigastric artery flap in rats--a new experimental flap model. Ann Plast Surg. 1997;39(5):500–504. doi: 10.1097/00000637-199711000-00010. [DOI] [PubMed] [Google Scholar]
- Strauch B, Murray DE. Transfer of composite graft with immediate suture anastomosis of its vascular pedicle measuring less than 1 mm. in external diameter using microsurgical techniques. Plast Reconstr Surg. 1967;40(4):325–329. doi: 10.1097/00006534-196710000-00002. [DOI] [PubMed] [Google Scholar]
- Green CE. Anatomy of the Rat. First edn. Hafner Publishing Company; 1968. pp. 124–153. [Google Scholar]
- Greene EC. Anatomy of the rat. New York: Hafner; 1959. [Google Scholar]
- Langworthy OR. A morphological study of the panniculus carnosus and its genetical relationship to the pectoral musculature in rodents. Am J Anat. 1925;35(2):283–302. [Google Scholar]
- Popesko P, Ratjová V, Horák J. A Colour Atlas of the Anatomy of Small Laboratory Animals. Vol. 2. Saunders; 1992. pp. 13–104. [Google Scholar]
- Brown SH, Banuelos K, Ward SR, Lieber RL. Architectural and morphological assessment of rat abdominal wall muscles: comparison for use as a human model. J Anat. 2010;217(3):196–202. doi: 10.1111/j.1469-7580.2010.01271.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harder Y, et al. Ischemic tissue injury in the dorsal skinfold chamber of the mouse: a skin flap model to investigate acute persistent ischemia. J Vis Exp. 2014. p. e51900. [DOI] [PMC free article] [PubMed]
- Cox GW, Runnels S, Hsu HS, Das SK. A comparison of heparinised saline irrigation solutions in a model of microvascular thrombosis. Br J Plast Surg. 1992;45(5):345–348. doi: 10.1016/0007-1226(92)90002-f. [DOI] [PubMed] [Google Scholar]
- Gurunluoglu R, Siemionow MZ. In: Plastic and Reconstructive Surgery: Experimental models and research designs. Siemionow MZ, editor. Spronger; 2015. pp. 53–62. Ch. 6. [Google Scholar]
- Nasir S. Plast Reconstr Surg. Springer; 2015. pp. 227–236. [Google Scholar]
- Parsa FD, Spira M. Evaluation of anastomotic techniques in the experimental transfer of free skin flaps. Plast Reconstr Surg. 1979;63(5):696–699. doi: 10.1097/00006534-197905000-00014. [DOI] [PubMed] [Google Scholar]
- Dunn RM, Huff W, Mancoll J. The Rat Rectus Abdominis Myocutaneous Flap: A True Myocutaneous Flap Model. Ann Plast Surg. 1993;31(4):352–357. doi: 10.1097/00000637-199310000-00012. [DOI] [PubMed] [Google Scholar]
- Özkan Ö, et al. A new flap model in rats: iliac osteomusculocutaneous flap. Ann Plast Surg. 2001;47(2):161–167. doi: 10.1097/00000637-200108000-00009. [DOI] [PubMed] [Google Scholar]
- Ozkan O, Koshima I, Gonda K. A supermicrosurgical flap model in the rat: a free true abdominal perforator flap with a short pedicle. Plast Reconstr Surg. 2006;117(2):479–485. doi: 10.1097/01.prs.0000197215.94170.b8. [DOI] [PubMed] [Google Scholar]
- Dorsett-Martin WA. Rat models of skin wound healing: a review. Wound Repair Regen. 2004;12(6):591–599. doi: 10.1111/j.1067-1927.2004.12601.x. [DOI] [PubMed] [Google Scholar]
- Ghali S, et al. Treating chronic wound infections with genetically modified free flaps. Plast Reconstr Surg. 2009;123(4):1157–1168. doi: 10.1097/PRS.0b013e31819f25a4. [DOI] [PubMed] [Google Scholar]


