Abstract
The lungs are constantly exposed to the external environment, which in addition to harmless particles, also contains pathogens, allergens, and toxins. In order to maintain tolerance or to induce an immune response, the immune system must appropriately handle inhaled antigens. Lung dendritic cells (DCs) are essential in maintaining a delicate balance to initiate immunity when required without causing collateral damage to the lungs due to an exaggerated inflammatory response. While there is a detailed understanding of the phenotype and function of immune cells such as DCs in human blood, the knowledge of these cells in less accessible tissues, such as the lungs, is much more limited, since studies of human lung tissue samples, especially from healthy individuals, are scarce. This work presents a strategy to generate detailed spatial and phenotypic characterization of lung tissue resident DCs in healthy humans that undergo a bronchoscopy for the sampling of endobronchial biopsies. Several small biopsies can be collected from each individual and can be subsequently embedded for ultrafine sectioning or enzymatically digested for advanced flow cytometric analysis. The outlined protocols have been optimized to yield maximum information from small tissue samples that, under steady-state conditions, contain only a low frequency of DCs. While the present work focuses on DCs, the methods described can directly be expanded to include other (immune) cells of interest found in mucosal lung tissue. Furthermore, the protocols are also directly applicable to samples obtained from patients suffering from pulmonary diseases where bronchoscopy is part of establishing the diagnosis, such as chronic obstructive pulmonary disease (COPD), sarcoidosis, or lung cancer.
Keywords: Immunology, Issue 119, bronchoscopy, monocyte, dendritic cell, tissue digestion, immunohistochemistry, flow cytometry.
Introduction
The lungs are in continuous contact with the external environment and are highly exposed to both harmless particles and microbes with the capacity to cause disease. Therefore, it is critical for the immune system to mount potent immune responses against invading pathogens, but it is equally important to maintain tolerance to inhaled antigens that do not cause disease. To provide potent immune surveillance, the respiratory system is lined with a network of immune cells, including dendritic cells (DCs). DCs are professional antigen-presenting cells with the unique capacity to activate naive T cells. In human lungs, resident DCs encounter an antigen and then process and transport it to the lung-draining lymph nodes for presentation to and activation of T cells1,2,3.
In the human immune system, DCs can be divided into several subsets, with distinct but overlapping functions: CD1c+ and CD141+ myeloid DCs (MDCs) and CD123+ plasmacytoid DCs (PDCs)4,5. While most detailed knowledge on human DCs stems from studies in blood, it is now evident that the human lungs also harbor rare populations of DC subsets with T-cell stimulatory capacity6,7,8,9. However, accumulating data show that immune cells, including DCs, differ in their frequency, phenotype, and function depending on their anatomical location10. Thus, it is important to study immune cells from the relevant tissue to understand their contribution to local immunity and tolerance. Taken together, this underlines the need to study lung-resident DCs when addressing lung diseases, despite blood DCs being more readily available and accessible in humans.
The first studies that investigated lung-resident DCs in humans primarily relied on morphology and the expression of single markers, such as HLA-DR and CD11c, in tissue sections using immunohistochemistry11,12,13. In contrast, more recent studies have typically relied on flow cytometric analyses to study different immune cell subsets. However, since it is difficult to find a single cell-surface marker that uniquely identifies a specific DC subset, the potential limitation of studies applying only four-color flow cytometry is the risk of including cell populations with similar phenotypic markers as DCs. For example, CD11c is expressed on all myeloid DCs and the vast majority of monocytes. On the other hand, in studies applying more advanced flow cytometry panels, non-cancerous lung tissue from surgical resections of patients were typically used10,14,15,16, although it is unclear whether these rare populations are truly representative of DCs present in healthy subjects. Overall, studies are limited largely due to the fact that surgically removed or whole human lung tissue is scarce.
To overcome some of these limitations, this work describes how to perform a detailed analysis of spatial distribution and a phenotypic identification of DCs in mucosal endobronchial biopsies obtained from healthy volunteers who undergo a bronchoscopy. Several small biopsies can be collected from each individual and can subsequently be embedded for sectioning and analysis using immunohistochemistry or enzymatically digested for advanced flow cytometric analysis. Using lung tissue in the form of endobronchial biopsies obtained from bronchoscopies confers the advantage of making it possible to perform the study on healthy volunteers, unlike open surgery of the lungs that, for obvious reasons, is limited to patients that require thoracic surgery. Furthermore, the tissue that is sampled during a bronchoscopy from healthy volunteers is physiologically normal, in contrast to a non-affected area of lung tissue in patients with a pulmonary disease. On the other hand, the biopsies are small and the number of cells retrieved, even when pooling several biopsies, limits the type of analyses that can be performed.
While the present work focuses on DCs, the methods described can be directly expanded to include other (immune) cells of interest that reside in human mucosal lung tissue. Furthermore, the protocols are also directly applicable to samples obtained from patients suffering from pulmonary diseases where bronchoscopy is part of establishing the diagnosis, such as chronic obstructive pulmonary disease (COPD), sarcoidosis, or lung cancer.
Protocol
NOTE: This research was approved by the regional Ethical Review Board in Umeå, Sweden.
1. Bronchoscopy for Sampling Endobronchial Biopsies from Human Subjects
Obtain informed consent from all participants.
Treat subjects with oral midazolam (4-8 mg) and intravenous glycopyrronium (0.2-04 mg) 30 min before the bronchoscopy. Apply topical anesthesia with lidocaine in the larynx and bronchi. Let the subject gargle with ~3 ml of lidocaine 4% and apply 3 ml to the tongue base and into the larynx via a larynx syringe. Optimize the topical anesthesia with 8-10 doses of lidocaine spray. Carry out this step with the subject sitting.
Insert a flexible video bronchoscope through the mouth via a plastic mouthpiece with the subject in the supine position. Use a purpose-made spray catheter to complete the topical anesthesia of the distal trachea and bronchi via the bronchoscope. Here, use a dose of approximately 5-10 ml of lidocaine 2%.
Take 6-9 endobronchial mucosal biopsies from the main carina and the main bronchial divisions using fenestrated forceps (Figure 1). Following the bronchoscopy and before leaving the hospital, let the subject rest for 2-4 hr and provide him/her with a light meal.
2. Embedding the Biopsies in Glycol Methylacrylate (GMA) Resin
NOTE: The GMA immunostaining protocol was originally developed at Southampton University, Histochemistry Research Unit17.
Fixation: For immunohistochemistry, remove the biopsies from the forceps and place them directly into glass vials containing 3 ml of ice-cold dehydrated acetone and protease inhibitors (phenylmethylsulfonyl fluoride (35 mg/100 ml acetone) and iodoacetamide (370 mg/100 ml acetone)). Fix the tissue overnight at -20 °C (Figure 2). NOTE: The following steps should be performed in a fume hood with appropriate nitrile gloves. The embedding kit contains components that can cause sensitization, irritation, and/or allergic skin reactions. All waste must be disposed of as hazardous waste.
Dehydration: Remove the acetone with inhibitors and replace with fresh dehydrated acetone (without inhibitors) for 15 min at room temperature (RT). Remove the acetone and replace it with methyl benzoate for 15 min.
Infiltration: Prepare a processing solution of 5% methyl benzoate solution in glycol methacrylate monomer; 10 ml is sufficient for one vial. Using plastic Pasteur pipettes, suction off the methyl benzoate solution and replace with 3 ml of processing solution. Incubate the biopsies and excess processing solution at 4 °C for 2 hr; Pasteur pipettes can be used for all subsequent solution changes, including embedding solution.
Exchange the processing solution every 2 hr (3x 2 hr incubations), so the total infiltration time of the biopsies in the processing solution is at least 6 hr. Insert paper labels into the top end of the embedding capsules to identify the biopsies.
Prepare an embedding solution of 75 mg benzoyl peroxide in 10 ml of glycol methacrylate monomer. Add 0.25 ml of N,N-dimethylaniline poly(ethylene oxide) (accelerator) to the embedding solution to begin the polymerization reaction. Remove the processing solution and place one biopsy into the relevant embedding capsule using forceps.
Slowly fill the embedding capsule to the top with embedding solution and close the cap. Avoid disturbing the biopsy and creating large air bubbles. Incubate the capsules at 4 °C until the resin has completely polymerized.
Store the embedded biopsies at -20 °C in a 50 ml tube containing approximately 5 g of silica gel.
3. Sectioning of GMA-embedded Endobronchial Biopsies
Microscope slide coating: Wash the microscope slides in a dishwasher on a normal cycle. Cover the slides and allow them to air dry.
Prepare a coating solution of 10% poly-L-lysine (PLL) solution in distilled water. Submerge the slides in coating solution for 5 min, and then let them air dry. Store dry PLL-coated slides in their original boxes.
Wash sheet glass strips with 0.1% Tween 20 in distilled water. Rinse the glass with 70% ethanol and dry with paper towels. Cut glass blades from the glass strip using a knife maker. Store the blades in a container that prevents movement to ensure that the cutting edge does not get damaged or nicked.
Biopsy trimming: Place the biopsy capsule in a capsule splitter and cut down each side using a carbon-steel single-edge blade. Remove the GMA-embedded biopsy and place it firmly in a vice. Trim excess GMA from around the biopsy using the steel blade.
- GMA sectioning.
- Prepare 0.05% ammonia solution with distilled water. Place the glass knife and biopsy in the microtome. Carefully align the biopsy block with the blade by adjusting the knife holder and the angle of the biopsy block so that the blade rests flat against the surface of the block.
- Cut 2 µm thick sections using the microtome on a slow cutting speed and use forceps to transfer and float out sections on the ammonia water. Float the sections for 45-90 sec, allowing gentle antigen retrieval and unfolding of the section.
- Pick up sections with microscope slide. Check the biopsy histology by quickly staining with toluidine blue.
- Dry the slides on a hot plate set to 50 °C and apply 500 µl of filtered toluidine blue stain to a section using a plastic Pasteur pipette. Warm the section on the hot plate until a green ring begins to emerge at the edge of the stain, and then wash it off with water.
- Using a light microscope, check the biopsy histology. Sections used for immunohistochemistry should contain good areas of undamaged lamina propria and epithelium, with as few glands and as little smooth muscle as possible.
- As in section 3.4.2, cut sections that have good histology and pick them up with PLL-coated microscope slides for immunohistochemical staining. Cut at least two sections from each biopsy for analysis. Dry slides for at least 1 hr. After drying, sections can be wrapped in tin foil and stored at -20 °C for up to 2 weeks, or they can be immediately immunostained.
4. Immunohistochemical Staining of GMA-embedded Endobronchial Biopsies
NOTE: Sodium azide is toxic. Prepare the 0.1% sodium azide solution within a fume hood and away from acids. Contact with acids liberates toxic gas.
Draw around sections using a diamond-tipped pen and arrange the slides onto a staining rack.
Perform a Peroxidase block. Prepare a peroxidase block solution of 0.3% hydrogen peroxide in 0.1% sodium azide solution. Apply 1 ml of the peroxidase block to sections and incubate for 30 min.
Prepare a wash solution of 0.05 M Tris-buffered saline (TBS), pH 7.6. Wash the slides in TBS, 3x 5 min.
Prepare a 1% BSA block solution in DMEM. Do this in advance and in large volumes, aliquot and freeze it until needed. Drain the slides and incubate the sections in block solution for 30 min to block unspecific antibody binding. If unspecific binding still occurs, include a 30 min incubation step with 5% serum block from the same species as the secondary antibody.
Dilute primary antibody (CD45 or CD1a) in TBS to the desired concentration (CD45 diluted at 1:1,000; CD1a diluted at 1:1,00) and apply it to slides. Coverslip the sections and incubate overnight at RT.
Wash slides in TBS three times. Dilute biotinylated secondary antibody (directed against the primary antibody host species, in this case rabbit anti-mouse F(ab'2)) in TBS to the desired concentration (1:300 dilution) and apply it to slides. Incubate for 2 hr at RT.
Prepare a streptavidin biotin-peroxidase complex at least 30 min before use. Ensure that there is enough to cover all slides. Wash the slides in TBS three times. Apply the solution to the slides and incubate for 2 hr at RT.
Wash the slides in TBS three times. Prepare 3-amino-9-ethylcarbazole (AEC) peroxidase substrate solution (made per the manufacturer's instructions). Apply it to the slides and incubate for 20-30 min or until the desired stain intensity develops.
Rinse the slides in running tap water for 5 min. Counterstain the sections with filtered Mayer's haematoxylin solution for 2 min. Wash the slides in running tap water for 5 min.
Drain the slides and cover the sections with permanent aqueous mounting medium. Dry the slides at 80 °C in a drying oven. Allow the slides to cool, and then mount them with DPX and place a coverslip.
5. Staining Analysis
Analyze the sections at 40X magnification using a light microscope with a mounted camera connected to a computer. NOTE: For cellular analysis, count positively stained, nucleated cells within the bronchial lamina propria and intact epithelium, excluding areas of smooth muscle, glands, large blood vessels, and mismatched or damaged tissue.
Average the cell counts and correct the average cell count for the area of the lamina propria and the length of the epithelium. The area of the lamina propria and the length of the epithelium can be calculated using an image analysis program.
6. Enzymatic Digestion of Endobronchial Biopsies
Washing biopsies: Using sterile forceps, place intact biopsies in a 15 ml conical tube containing 10 ml of Hank's buffered saline solution (HBSS) (Figure 3). Incubate for 5 min at RT on a rocking platform at 30 rpm. Transfer the biopsies to a sterile dish by decanting the content of the 15 ml tube with HBSS.
Disrupting mucus with DTT: Replace the HBSS in the tube with 10 ml of HBSS containing 5 mM 1,4-dithiothreitol (DTT). Transfer the biopsies back into the 15 ml tube using sterile forceps. Incubate for 15 min at RT on a rocking platform at 30 rpm.
Vortex the tube gently for 15 sec. Transfer the biopsies onto a sterile dish by decanting the content of the 15 ml tube with HBSS and DTT.
Transferring the biopsies to the culture medium: Replace the HBSS and DTT in the tube with 10 ml of RPMI 1640 culture medium. Transfer the biopsies back into the 15 ml tube using sterile forceps. Incubate for 10 min at RT on a rocking platform at 30 rpm.
- Digesting biopsies with collagenase and DNase.
- Prepare a digestion solution of collagenase II (0.25 mg/ml) and DNase (0.2 mg/ml) in pre-warmed RPMI containing 1 M HEPES solution. Add 500 µL of digestion solution per well in a 48-well tissue culture plate.
- Place 1 biopsy per well in digestion solution. Incubate the plate on a shaking platform for 60 min at 37 °C at 220 rpm. Pipette up and down after 30 min to re-disperse the biopsies, and after 60 min, to completely disaggregate the tissue.
- Preparing single cell suspensions.
- Pool together the digested biopsies from the wells into a 50 ml tube by passing it through a 40 µm cell strainer. Collect the remaining cells by washing the wells with ice-cold FACS buffer (phosphate-buffered saline (PBS) containing 2% fetal bovine serum).
- Squeeze the remaining tissue on the cell strainer using the back of the plunger of a syringe. Centrifuge the digested cells at 400 x g for 5 min at 4 °C. Carefully remove the supernatant and resuspend the pellet in 5 ml of ice-cold FACS buffer. Count the cells manually using a hemocytometer and Trypan blue stain to assess the viability of the cells.
7. Flow Cytometric Analysis of Single Cells of Endobronchial Biopsies after Enzymatic Digestion
Resuspend the cell pellet to approximately 1 x 106 cells in 200 µl of FACS buffer.
Add a cell viability dye for dead cell exclusion according to the manufacturer's protocol.
Add 5 µl of FcR blocking reagent and incubate for 5 min at 4 °C.
Add cell surface antibodies against CD45 (2 µl), lineage (CD3, CD20, CD56, CD66abce, and CD14; 2 µl each), CD16 (0.5 µl), HLA-DR (3 µl), CD11c (5 µl), CD123 (5 µl), CD1c (3 µl), and CD103 (2 µl) and incubate for 15 min at 4 °C. Details on antibodies can be found in the methods section, but titrate and optimize the antibodies to the precise flow cytometer in use. Wash off excess antibodies with PBS for 5 min at 400 x g. Acquire the samples fresh on a flow cytometer or fix the cells in 1% paraformaldehyde prior to later acquisition.
Identify human DCs in lung biopsies using a flow cytometry assay18 (Figure 4). NOTE: Using a flow cytometry analysis software, immune cells are distinguished from other lung cells by gating on CD45. Dead cells can be excluded as cells that are positive for the LIVE/DEAD dye. Of all live CD45+ cells, lineage cells (B cells, T cells, NK cells, neutrophils, and monocytes) can be excluded using a cocktail of antibodies against CD20, CD3, CD56, CD66abce, CD14, and CD16 in one channel. Following that, HLA-DR+ cells will allow the identification of all human DCs. MDCs can be distinguished from PDCs based on the expression of CD11c or the lack of CD11c, respectively. MDCs can be further divided into CD1c+ MDCs or CD141+.
Representative Results
Studies characterizing human respiratory tissue-resident immune cells, including DCs, are limited, largely due to the fact that surgically removed or whole human lung tissue is scarce. Here, a less invasive method of obtaining lung tissue from endobronchial biopsies (EBB) of healthy volunteers and developed protocols to study the immune cells in the tissue using immunohistochemistry or flow cytometry are outlined.
Healthy volunteers underwent bronchoscopy, as previously described19,20. Six to nine 1-2 mm3 endobronchial mucosal biopsies were taken from the main carina and the main bronchial divisions of each subject using fenestrated forceps (Figure 1A). Two biopsies were embedded in GMA and subsequently used for immunohistochemistry to provide spatial information. The remaining biopsies were enzymatically digested, and the single-cell suspensions were analyzed using multi-color flow cytometry, which allowed careful characterization of rare cell subsets (Figure 1B).
To obtain as much spatial information as possible from the small tissue pieces, the biopsies were embedded in GMA that allows for ultrathin μm sections (Figure 2A-B). As expected, CD45-expressing immune cells were relatively rare-on average, 125 CD45+ cells per mm2 were present in mucosal lung tissue during steady-state conditions, as assessed by immunohistochemistry (Figure 2C). The IgG1 isotype control resulted in no positive staining, indicating high specificity of the primary antibody. The number of positive cells in both the lung epithelium and the underlying lamina propria were quantified and showed that CD45+ immune cells were more abundant in the lamina propria than in the epithelium (Figure 2D). Furthermore, CD1a-expressing cells were identified and enumerated, and they most likely represent DCs (Figure 2E). On average, fewer than one CD1a+ cell per mm2 was identified in the lung lamina propria at steady state (Figure 2F).
Immunohistochemistry provides information on the anatomical distribution of cells in intact tissue, but it is typically limited in its ability to define the cells using multiple cell-surface markers. Multi-color flow cytometry, depending on the instrument, has the advantage of providing more information per cell, and it can be used in small samples. Up to nine mucosal lung biopsies were pooled, washed, and incubated to disrupt the mucus. Each biopsy was then digested by collagenase and DNase in individual wells of a 48 well-plate, resulting in a single-cell suspension (Figures 3A-3B). On average, 1.5 x 106 endobronchial cells per subject were obtained, and a positive correlation between the cell yield and viability was observed (Figure 3C). The reduced cell viability observed with lower cell numbers could potentially be explained by a higher enzyme concentration per cell that was suboptimal for the cells. This is a challenge with biopsies varying both in size and in cell density, with some biopsies sampling more of the superficial mucosa than others. As expected, flow cytometric analysis of the single-cell suspension revealed that, on average, 12% of the cells were CD45+ leukocytes, while the majority of cells in the lung mucosal tissue under steady-state conditions were not immune cells (Figure 3D). The flow cytometric and IHC data correlated, which highlights the strength of employing both techniques in parallel.
Utilizing the enzymatic digestion protocol, cell suspensions from the endobronchial biopsies were stained with a panel of fluorescently labeled antibodies. The frequency of different DC subsets in lung tissue and their expression of CD103 compared to cells in bronchoalveolar lavage or peripheral blood from the same subject were analyzed. Myeloid cells were identified using a gate on live CD45+ leukocytes that expressed HLA-DR but were negative for the lineage markers CD3, CD20, CD56, CD66abce, CD14, and CD16 (Figure 4A). In this small population of cells, plasmacytoid DCs (PDCs) were identified based on their lack of CD11c expression and their high expression of CD123 and HLA-DR (teal). Among the CD11c+ HLA-DR+ lineage-negative cells, both CD1c+ (coral) and CD141+ (maroon) myeloid DCs were identified (Figure 4A). To further characterize these cell subsets, their expression of the integrin CD103 that binds to E-cadherin, important in tissue anchoring, was evaluated. While all DC subsets, as well as T cells circulating in peripheral blood, were low or negative for CD103, a distinct proportion of DCs and T cells found in the lungs of the same individual expressed CD103. This was true of cells found both in bronchoalveolar lavage as well as in lung tissue (Figure 4B).
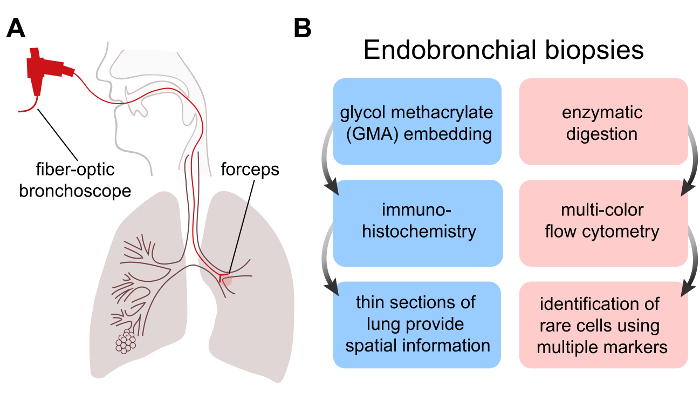 Figure 1: Sampling of human lung mucosal tissue. (A) Bronchoscopies were performed on subjects to obtain endobronchial biopsies from the main bronchial divisions of one lung using forceps. (B) Biopsies were either embedded in GMA for tissue sectioning and immunohistochemistry (blue diagram) or enzymatically digested to obtain single-cell suspensions for flow cytometry (pink diagram). Please click here to view a larger version of this figure.
Figure 1: Sampling of human lung mucosal tissue. (A) Bronchoscopies were performed on subjects to obtain endobronchial biopsies from the main bronchial divisions of one lung using forceps. (B) Biopsies were either embedded in GMA for tissue sectioning and immunohistochemistry (blue diagram) or enzymatically digested to obtain single-cell suspensions for flow cytometry (pink diagram). Please click here to view a larger version of this figure.
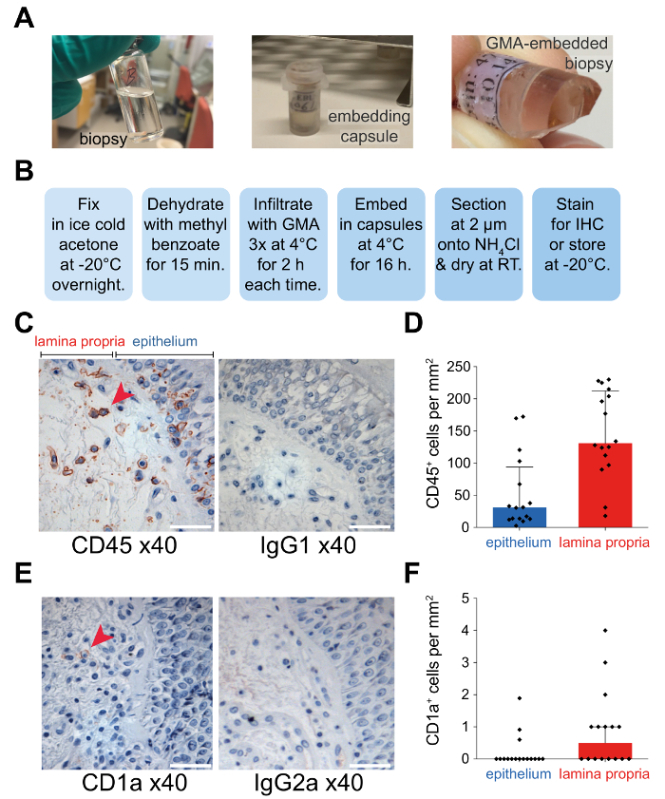 Figure 2: Embedding the biopsies in GMA resin. (A)Biopsies taken from bronchoscopies were immediately transferred to glass vials containing ice-cold dehydrated acetone (left panel). Following overnight fixation, the biopsies were infiltrated with methyl benzoate solution. Biopsies were placed in embedding capsules filled with embedding solution to begin polymerization (middle panel). Embedded biopsies can be stored at -20 °C or can be sectioned for immunohistochemistry staining (right panel). (B) The schematic highlights key steps in the process of embedding biopsies using GMA. Representative images of sectioned biopsies showing the presence of CD45+ cells (C) or CD1a+ cells (E) are shown compared to the respective isotype controls (right panels). Specific staining is shown in red, and cell nuclei counterstained with hematoxylin are in blue. Scale bar = 50 µm. Bar graphs show the median ± interquartile range of CD45+ (D) or CD1a+ (F) cells per mm2 in the epithelium or lamina propria (n = 20). Please click here to view a larger version of this figure.
Figure 2: Embedding the biopsies in GMA resin. (A)Biopsies taken from bronchoscopies were immediately transferred to glass vials containing ice-cold dehydrated acetone (left panel). Following overnight fixation, the biopsies were infiltrated with methyl benzoate solution. Biopsies were placed in embedding capsules filled with embedding solution to begin polymerization (middle panel). Embedded biopsies can be stored at -20 °C or can be sectioned for immunohistochemistry staining (right panel). (B) The schematic highlights key steps in the process of embedding biopsies using GMA. Representative images of sectioned biopsies showing the presence of CD45+ cells (C) or CD1a+ cells (E) are shown compared to the respective isotype controls (right panels). Specific staining is shown in red, and cell nuclei counterstained with hematoxylin are in blue. Scale bar = 50 µm. Bar graphs show the median ± interquartile range of CD45+ (D) or CD1a+ (F) cells per mm2 in the epithelium or lamina propria (n = 20). Please click here to view a larger version of this figure.
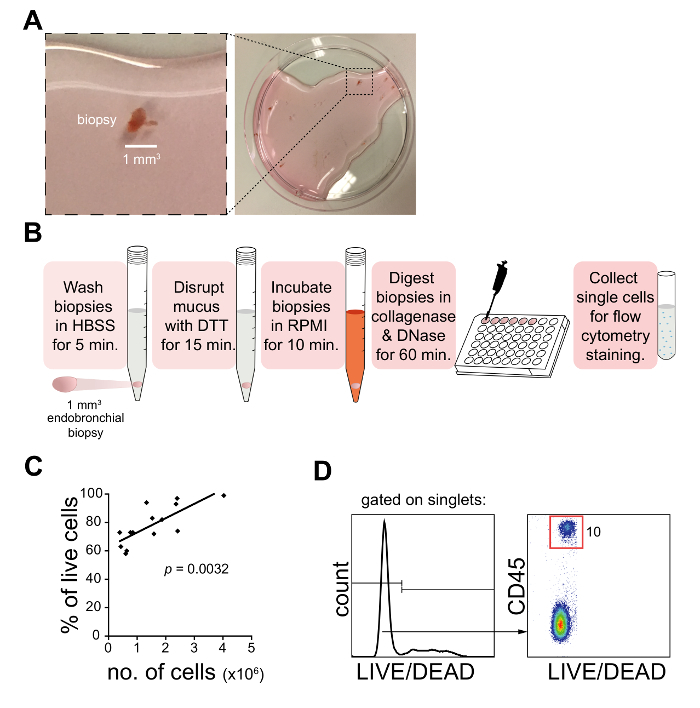 Figure 3: Enzymatic digestion of biopsies for flow cytometry. (A) An endobronchial biopsy taken from a bronchoscopy in a Petri dish. The biopsies were washed in HBSS, treated with DTT to remove mucus, and digested with collagenase and DNase prior to the collection of single cells for flow cytometric analysis. (B) The schematic summarizes the main procedures for digesting biopsies for flow cytometry. (C) The graph shows the correlation in cell yield and viability, as assessed by manual counting and Trypan blue exclusion (n = 20). (D) Single-cell suspensions from the digested biopsy were analyzed by flow cytometry and assessed for viability and the expression of CD45 (leukocyte common antigen). The flow cytometry plot shows one representative donor out of 20 healthy subjects. Please click here to view a larger version of this figure.
Figure 3: Enzymatic digestion of biopsies for flow cytometry. (A) An endobronchial biopsy taken from a bronchoscopy in a Petri dish. The biopsies were washed in HBSS, treated with DTT to remove mucus, and digested with collagenase and DNase prior to the collection of single cells for flow cytometric analysis. (B) The schematic summarizes the main procedures for digesting biopsies for flow cytometry. (C) The graph shows the correlation in cell yield and viability, as assessed by manual counting and Trypan blue exclusion (n = 20). (D) Single-cell suspensions from the digested biopsy were analyzed by flow cytometry and assessed for viability and the expression of CD45 (leukocyte common antigen). The flow cytometry plot shows one representative donor out of 20 healthy subjects. Please click here to view a larger version of this figure.
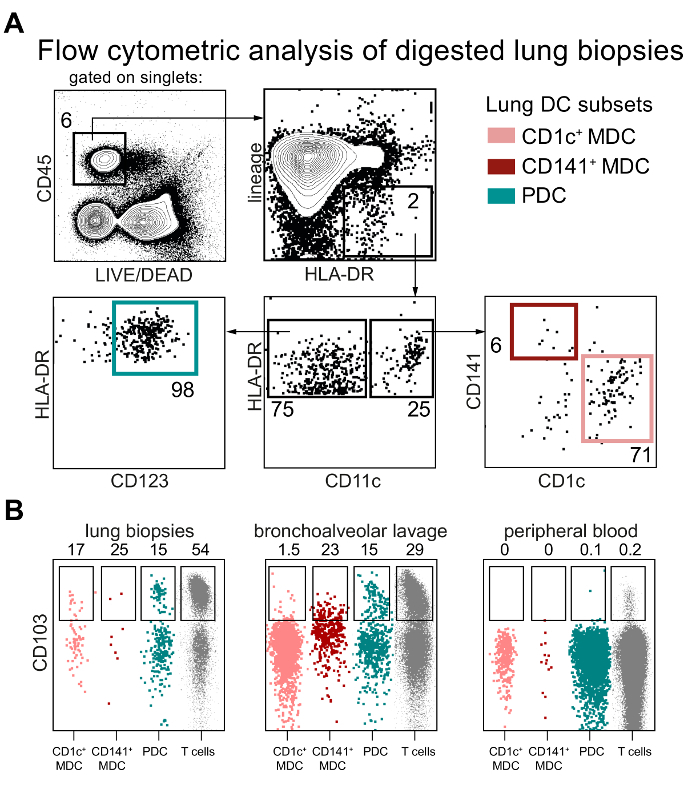 Figure 4: Identification of lung dendritic cell subsets in digested biopsies. (A) Gating strategy for the identification of CD1c+ and CD141+ myeloid DCs (MDCs) and plasmacytoid DCs (PDCs) in lung mucosal tissue. The flow cytometry plots from one representative subject are shown. (B) The dot plots show the expression of the integrin CD103 on populations of DCs in lung biopsies (left panel), bronchoalveolar lavage (middle panel), and peripheral blood (right panel). Please click here to view a larger version of this figure.
Figure 4: Identification of lung dendritic cell subsets in digested biopsies. (A) Gating strategy for the identification of CD1c+ and CD141+ myeloid DCs (MDCs) and plasmacytoid DCs (PDCs) in lung mucosal tissue. The flow cytometry plots from one representative subject are shown. (B) The dot plots show the expression of the integrin CD103 on populations of DCs in lung biopsies (left panel), bronchoalveolar lavage (middle panel), and peripheral blood (right panel). Please click here to view a larger version of this figure.
Discussion
This paper describes how to generate a detailed spatial and phenotypical characterization of lung tissue-resident DCs in healthy humans using immunohistochemistry and flow cytometry on endobronchial mucosal biopsies collected during bronchoscopy. In the following paragraphs critical steps in the protocol are discussed in detail.
Critical Steps with the Protocol
Sectioning and immunohistochemistry: It is critical to keep the biopsy blocks at -20 °C when not using them (step 2.5). Warm blocks can sometimes become soft and will not section as well. Additionally, keeping the blocks at -20 °C will preserve antigen sites and result in better staining using immunohistochemistry.
Sectioning and immunohistochemistry: When sectioning the GMA-embedded biopsies, it is convenient to have 3-4 containers of ammonia water available to float the sections on. When a section is picked up, make sure to replace it with a fresh section (step 3.4). This ensures that, by the time that section is handled again, it will have been floating on the ammonia water for approximately the correct length of time (45-90 sec), which aids in antigen presentation and the subsequent immunohistochemistry. Cutting 2 µm sections in this fashion also allows for consecutive sectioning, which means that the same cell can potentially be stained with different cell-surface or intracellular markers. It is important not to touch the cutting edge of the glass blade when sectioning, as it is easily damaged. If there is any debris from the blade that needs to be removed, always brush away from the cutting edge.
Enzymatic digestion and flow cytometry: In tissue samples where immune cells are rare, it is critical to include CD45 in the flow staining panel to first identify leukocytes (in minority) before further identifying DCs or other immune cells of interest. Also, "fluorescence minus one" or isotype controls are critical to include while validating the antibody panels used to ensure that rare events are true signal over noise.
Modifications and Troubleshooting
Sectioning and immunohistochemistry: For most cellular markers expressed by immune cells, tonsil tissue can be used as a good positive control and to titrate antibodies for immunohistochemistry in order to avoid wasting limited endobronchial biopsy material (step 4). To visualize the dendritic processes of DCs, tissues can be sectioned parallel to the epithelium, rather than perpendicularly through the mucosa21. Other peroxidase substrates can be used in addition to AEC, such as DAB, if the user requires a different substrate color. The avidin/biotin enzyme complex can also be substituted, for example, with alkaline phosphatase.
Enzymatic digestion and flow cytometry: Although the endobronchial biopsies are small, the tissue-resident cells survive the enzymatic digestion and processing into a single-cell suspension for flow cytometric analysis (Figure 3). However, it is important to assess the potential impact of the enzymes on the stains used in the flow cytometry antibody panel. To test whether the enzymatic digestion protocol cleaves off, alters, or interferes with the antibody staining, more easily accessible cells expressing similar markers, such as peripheral blood mononuclear cells, can be treated with the digestive enzymes (step 6) or not, and they can subsequently by stained with fluorescently labeled antibodies and analyzed by flow cytometry (step 7). If the collagenase and DNase do not interfere with the antigen availability, the stains with or without treatment of the cells with enzymes should look similar. Furthermore, this can be verified using both flow cytometry, as well as intact tissue sections and immunohistochemistry (Figures 2-3)19.
Limitations of the Technique
Bronchoscopy: Most healthy individuals tolerate a bronchoscopy well, and it is a method routinely used to examine and sample the lungs, including to collect endobronchial mucosal biopsies, as described here (step 1). However, bronchoscopy is typically not a suitable method to perform for longitudinal sampling, since it is often perceived as uncomfortable, and it is also a time- and resource-demanding procedure. Therefore, endobronchial biopsies provide only a snapshot of the immune cells present in the mucosal lung tissue at a given time, rather than a long-term study of changes in dynamics or kinetics.
Significance of the Technique with Respect to Existing/Alternative Methods
Sectioning and immunohistochemistry: The advantage of embedding in GMA rather than paraffin or by cryopreservation is the superior preservation of morphology and antigens, and greater number of sections from the small biopsies, due to the thin sections that can be obtained17.
Enzymatic digestion and flow cytometry. By obtaining single cells from small biopsies, much more information can be attained by multi-color flow cytometry.
Future Applications or Directions after Mastering This Technique
This protocol described two parallel methods for maximizing the information that can be obtained from small endobronchial biopsies by combining immunohistochemistry and flow cytometry. To characterize the spatial distribution of rare immune cells such as DCs, biopsies can be embedded in GMA to obtain thin sections for immunohistochemistry, whereas to distinguish DCs from other immune cells with similar markers, the enzymatic digestion of the biopsies allows multi-color flow cytometry to be performed. To enable the unbiased identification of novel characteristics of DCs during inflammation or disease, the automated analysis of flow cytometric data can be performed by applying feature extraction algorithms22. Future applications include using these single cells for cell sorting to collect specific cell populations that can be used for RNA sequencing or transcriptomic profiling. The identification of DCs residing in the lungs may be important for understanding the changes in the immune landscape during health and disease.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgments
The authors would like to thank the volunteers who have contributed clinical material to this study. We are also thankful to the staff at the Department of Public Health and Clinical Medicine, Division of Medicine/Respiratory Medicine, University Hospital, Umeå (Norrlands universitetssjukhus) for the collection of all clinical material.
This work was supported by grants to AS-S from the Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Foundation for Strategic Research, and the Karolinska Institutet.
References
- Kopf M, Schneider C, Nobs SP. The development and function of lung-resident macrophages and dendritic cells. Nat Immunol. 2015;16(1):36–44. doi: 10.1038/ni.3052. [DOI] [PubMed] [Google Scholar]
- Condon TV, Sawyer RT, Fenton MJ, Riches DW. Lung dendritic cells at the innate-adaptive immune interface. J Leukoc Biol. 2011;90(5):883–895. doi: 10.1189/jlb.0311134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambrecht BN, Hammad H. Biology of lung dendritic cells at the origin of asthma. Immunity. 2009;31(3):412–424. doi: 10.1016/j.immuni.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Schlitzer A, McGovern N, Ginhoux F. Dendritic cells and monocyte-derived cells: Two complementary and integrated functional systems. Semin Cell Dev Biol. 2015;41:9–22. doi: 10.1016/j.semcdb.2015.03.011. [DOI] [PubMed] [Google Scholar]
- Ziegler-Heitbrock L, et al. Nomenclature of monocytes and dendritic cells in blood. Blood. 2010;116(16):e74–e80. doi: 10.1182/blood-2010-02-258558. [DOI] [PubMed] [Google Scholar]
- Demedts IK, Brusselle GG, Vermaelen KY, Pauwels RA. Identification and characterization of human pulmonary dendritic cells. Am J Respir Cell Mol Biol. 2005;32(3):177–184. doi: 10.1165/rcmb.2004-0279OC. [DOI] [PubMed] [Google Scholar]
- Donnenberg VS, Donnenberg AD. Identification rare-event detection and analysis of dendritic cell subsets in broncho-alveolar lavage fluid and peripheral blood by flow cytometry. Front Biosci. 2003;8:s1175–s1180. doi: 10.2741/1185. [DOI] [PubMed] [Google Scholar]
- Masten BJ, et al. Characterization of myeloid and plasmacytoid dendritic cells in human lung. J Immunol. 2006;177(11):7784–7793. doi: 10.4049/jimmunol.177.11.7784. [DOI] [PubMed] [Google Scholar]
- Ten Berge B, et al. A novel method for isolating dendritic cells from human bronchoalveolar lavage fluid. J Immunol Methods. 2009;351(1-2):13–23. doi: 10.1016/j.jim.2009.09.009. [DOI] [PubMed] [Google Scholar]
- Yu CI, et al. Human CD1c+ dendritic cells drive the differentiation of CD103+ CD8+ mucosal effector T cells via the cytokine TGF-beta. Immunity. 2013;38(4):818–830. doi: 10.1016/j.immuni.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicod LP, Lipscomb MF, Toews GB, Weissler JC. Separation of potent and poorly functional human lung accessory cells based on autofluorescence. J Leukoc Biol. 1989;45(5):458–465. doi: 10.1002/jlb.45.5.458. [DOI] [PubMed] [Google Scholar]
- Sertl K, et al. Dendritic cells with antigen-presenting capability reside in airway epithelium, lung parenchyma, and visceral pleura. J Exp Med. 1986;163(2):436–451. doi: 10.1084/jem.163.2.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Haarst JM, de Wit HJ, Drexhage HA, Hoogsteden HC. Distribution and immunophenotype of mononuclear phagocytes and dendritic cells in the human lung. Am J Respir Cell Mol Biol. 1994;10(5):487–492. doi: 10.1165/ajrcmb.10.5.8179911. [DOI] [PubMed] [Google Scholar]
- Schlitzer A, et al. IRF4 transcription factor-dependent CD11b+ dendritic cells in human and mouse control mucosal IL-17 cytokine responses. Immunity. 2013;38(5):970–983. doi: 10.1016/j.immuni.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu YA, et al. Flow Cytometric Analysis of Myeloid Cells in Human Blood, Bronchoalveolar Lavage, and Lung Tissues. Am J Respir Cell Mol Biol. 2015. [DOI] [PMC free article] [PubMed]
- Haniffa M, et al. Human tissues contain CD141hi cross-presenting dendritic cells with functional homology to mouse CD103+ nonlymphoid dendritic cells. Immunity. 2012;37(1):60–73. doi: 10.1016/j.immuni.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britten KM, Howarth PH, Roche WR. Immunohistochemistry on resin sections: a comparison of resin embedding techniques for small mucosal biopsies. Biotech Histochem. 1993;68(5):271–280. doi: 10.3109/10520299309105629. [DOI] [PubMed] [Google Scholar]
- Perfetto SP, Chattopadhyay PK, Roederer M. Seventeen-colour flow cytometry: unravelling the immune system. Nat Rev Immunol. 2004;4(8):648–655. doi: 10.1038/nri1416. [DOI] [PubMed] [Google Scholar]
- Baharom F, et al. Dendritic Cells and Monocytes with Distinct Inflammatory Responses Reside in Lung Mucosa of Healthy Humans. J Immunol. 2016;196(11):4498–4509. doi: 10.4049/jimmunol.1600071. [DOI] [PubMed] [Google Scholar]
- Salvi S, et al. Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. Am J Respir Crit Care Med. 1999;159(3):702–709. doi: 10.1164/ajrccm.159.3.9709083. [DOI] [PubMed] [Google Scholar]
- Schon-Hegrad MA, Oliver J, McMenamin PG, Holt PG. Studies on the density, distribution, and surface phenotype of intraepithelial class II major histocompatibility complex antigen (Ia)-bearing dendritic cells (DC) in the conducting airways. J Exp Med. 1991;173(6):1345–1356. doi: 10.1084/jem.173.6.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeys Y, Gassen SV, Lambrecht BN. Computational flow cytometry: helping to make sense of high-dimensional immunology data. Nat Rev Immunol. 2016;16(7):449–462. doi: 10.1038/nri.2016.56. [DOI] [PubMed] [Google Scholar]


