Abstract
Collecting reliable behavioral data from toddlers and preschoolers is challenging. As a result, there are significant gaps in our understanding of human auditory development for these age groups. This paper describes an observer-based procedure for measuring hearing sensitivity with a two-interval, two-alternative forced-choice paradigm. Young children are trained to perform a play-based, motor response (e.g., putting a block in a bucket) whenever they hear a target signal. An experimenter observes the child's behavior and makes a judgment about whether the signal was presented during the first or second observation interval; the experimenter is blinded to the true signal interval, so this judgment is based solely on the child's behavior. These procedures were used to test 2 to 4 year-olds (n = 33) with no known hearing problems. The signal was a 1,000 Hz warble tone presented in quiet, and the signal level was adjusted to estimate a threshold corresponding to 71%-correct detection. A valid threshold was obtained for 82% of children. These results indicate that the two-interval procedure is both feasible and reliable for use with toddlers and preschoolers. The two-interval, observer-based procedure described in this paper is a powerful tool for evaluating hearing in young children because it guards against response bias on the part of the experimenter.
Keywords: Behavior, Issue 119, Hearing, children, auditory development, audiology, preschooler, tone detection, psychophysics, perception, behavioral assessments
Introduction
It is difficult to obtain reliable estimates of behavioral hearing thresholds for toddlers and preschoolers. The operant techniques used to test infants in the clinic and the laboratory do not generally work well with children in this age range because toddlers and preschoolers tend to habituate faster than infants1,2. On the other hand, toddlers and preschoolers often lack the cognitive maturity required to complete standard forced-choice behavioral testing procedures that are used to evaluate children 4 years of age and older3,4. Consequently, there are significant gaps in our understanding of human auditory development between infancy and early school age.
A single-interval, adaptive procedure called Conditioned Play Audiometry5 (CPA) is routinely used in the audiology clinic to assess hearing sensitivity for children with a developmental age falling between about 2.5 and 5 years6. CPA relies on the use of a play-based motor activity (e.g., stacking blocks) to establish a time-locked conditioned response to an auditory signal. A test assistant provides the child with positive social reinforcement, further shaping the response behavior. Results from several studies have shown that the use of CPA yields a conventional clinical audiogram for more than 90% of typically developing 3 year-olds7,8. Substantially lower yield rates have been reported for younger children. For example, Thompson et al.9 reported that a conditioned response to sound could be established using CPA in 68% of 2 year-olds.
Despite the widespread use of CPA in the audiology clinic, it is not well suited for most laboratory-based investigations of auditory behavior. CPA is a single-interval adaptive procedure designed to maximize both efficiency and patient acceptance, but it is susceptible to observer and listener response bias. The observer in the CPA procedure initiates signal presentations, and may thus be influenced by factors such as a priori expectations regarding the child's hearing sensitivity or their propensity to respond10. The inclusion of "catch" trials – trials in which no sound is presented - is sometimes used to quantify and accommodate examiner response bias11.
The overall goal of the method described in the present report is to efficiently estimate hearing thresholds in toddlers and preschoolers using a play-based, two-interval, forced-choice behavioral testing procedure. The rationale for using a forced-choice paradigm is that it guards against some forms of response bias10, thus permitting more direct comparisons across different ages and/or stimuli using an efficient adaptive procedure. Conventional two- and three-interval, forced-choice methods require a specific, prescribed response (e.g., pushing one of several buttons) on the part of the listener, to indicate which interval contains the signal. Children as young as 4 to 5 years of age can perform this task12, but the demands of the procedure make these methods unsuitable for younger listeners and for many listeners with developmental delays.
The method described here builds on the work of Browning et al.13, which evaluated the feasibility and efficiency of estimating infant behavioral thresholds using a two-interval, forced-choice adaptation of the observer-based psychophysical procedure14. In this method, the signal is presented during one of two observation intervals. Each interval is indicated to the observer in real time both visually and acoustically, but the observer is not told which interval contains the signal. The infant, on the other hand, is not given any indication of the occurrence of an observation interval apart from the presentation of a signal. After each trial, the observer selects the interval containing the signal based on the infant's behavior. The results reported by Browning et al.13 demonstrated that this procedure is both feasible and efficient for use with 7 to 9 month-old infants. The method for testing toddlers and preschoolers closely follows procedures for testing infants, with the caveat that children's responses to sound are shaped using methods common with CPA.
For this article, a simple experiment was designed to measure children's tone detection in quiet. The signal was a 500 msec, 1,000 Hz warble tone presented through an insert earphone. Note that we have also successfully used this protocol to assess performance in more complex listening tasks, such as speech detection in a noise masker15. In the protocol described below, children are taught to perform a play-based conditioned motor response when a signal is heard. However, any behavioral response can be used, provided it is time-locked to the presentation of the stimulus and can be reliably judged. As demonstrated here, this task is appropriate for testing typically developing children as young as 2 years of age.
Protocol
The Institutional Review Board at The University of North Carolina at Chapel Hill approved this research.
1. Personnel and Space Requirements
Perform testing in a sound-isolating room. Configure the room with a table and chairs, as shown in Figure 1.
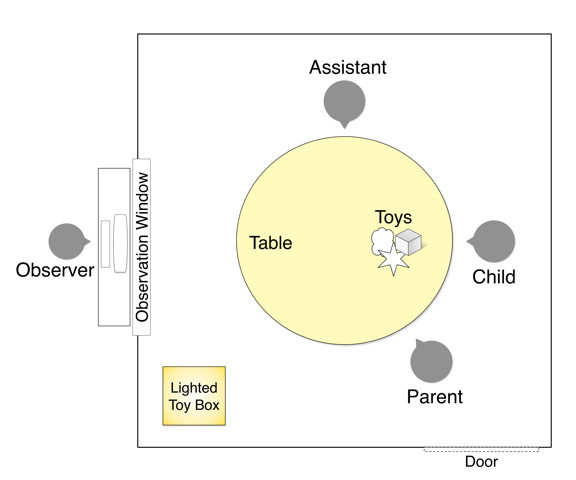 Figure 1: Test environment. The assistant and the listener are seated at a table inside the sound booth. The child's parent may elect to sit inside or outside the booth. The observer sits outside the booth, positioned in front of the window for good visibility of the assistant and the child. The computer screen and keyboard controlling the run-time computer are accessible to the observer, allowing him/her to initiate trials and enter responses. Please click here to view a larger version of this figure.
Figure 1: Test environment. The assistant and the listener are seated at a table inside the sound booth. The child's parent may elect to sit inside or outside the booth. The observer sits outside the booth, positioned in front of the window for good visibility of the assistant and the child. The computer screen and keyboard controlling the run-time computer are accessible to the observer, allowing him/her to initiate trials and enter responses. Please click here to view a larger version of this figure.
Use two experimenters to test toddlers and preschoolers; an "assistant" who sits inside the booth with the child and an "observer" who is in the adjacent control room. NOTE: The role of the assistant inside the booth is to: (1) train the child to perform a simple play-based motor response (e.g., stacking blocks) whenever the target signal is heard; (2) provide reinstruction whenever necessary; (3) socially engage the child throughout the testing session; (4) change the game the child is playing based on the child's level of interest; and (5) provide social reinforcement (e.g., clapping or cheering) following trials in which the child performs the targeted motor response. NOTE: The role of the observer seated outside of the booth is to: (1) observe the child and assistant inside the booth through a window; (2) initiate test trials when the child is quiet and in a "ready" position; and (3) indicate whether the child heard the sound in the 1st or 2nd interval following each test trial by clicking on the corresponding response button in the computer software user interface. This decision is based solely on the child's response. NOTE: The experience level of the experimenters will affect the yield rate and data obtained. In this experiment, all observers and assistants had at least two years of experience testing toddlers and preschoolers in the audiology clinic and/or research laboratory.
Locate the computer and hardware in the control room. Position the computer monitor so the observer can view the monitor as well as the child and the assistant inside the booth.
Equip the testing space with a two-way communication system between the observer and the assistant. NOTE: This system allows the two testers to work together to ensure trials are initiated when the child is alert and oriented to the task.
2. Hardware and Software Configuration
In this example, custom software controls a real-time processor, which routes the sound to an insert earphone. Alternatively, a soundcard system with precise control of stimulus timing can be used.
Select a target signal. In this example, the signal is a 500 msec, 1,000 Hz warble tone.
Present the stimuli through an earphone that is appropriately calibrated to ensure the sound levels presented to the listener are accurate and safe.
Program the custom software to control the timing of the two observation intervals for each trial. NOTE: In this example, each observation interval is 1,065 msec in duration, and intervals are separated by a 300 msec inter-stimulus interval. Thus, the total duration of each trial is 2,430 msec.
Collect pilot data to help select appropriate durations for the signal, the observation intervals and inter-stimulus interval. Optimal durations may vary depending on the stimulus and the population and/or age of children being tested.
Program the software to provide an audio and visual prompt to mark the two intervals. In this example, an audio prompt is a voice recording of a female talker saying "one" and "two." Both the observer and the assistant hear the audio prompt. The visual prompt appears as a flashing black circle on the monitor screen. Only the observer sees the visual display. NOTE: The observer uses these time-locked auditory and visual interval indicators, in conjunction with observations of the listener's behavior, to determine which interval contained the target signal.
Program the software to indicate which interval contains the signal only after the observer has entered a response.
- Program the custom software to execute the three stages of the testing protocol. The purpose and main features of each stage are as follows:
- In Stage 1, present the signal at a fixed and clearly audible level, always in interval 2. Select the training level intensity based on pilot data. After three trials in Stage 1, program the software to prompt the observer to either repeat Stage 1 or initiate Stage 2. NOTE: The purpose of Stage 1, the operant conditioning stage, is to teach the listener to perform a play-based, motor response as soon as he/she hears the signal.
- In Stage 2, program the software to allow the signal to occur in either interval 1 or interval 2, with equal a priori probability. Present the signal at the same audible level used in Stage 1. Program Stage 2 to continue until the observer correctly judges the observation interval containing the signal on 4 out of 5 consecutive trials. NOTE: The purpose of Stage 2, the verification stage, is to ensure the observer can reliably judge the interval containing the signal based solely on the child's behavior.
- Program Stage 3 to collect experimental data. In this example, the software is program to run an adaptive track procedure in Stage 3. The signal occurs in either interval 1 or interval 2, with equal a priori probability. NOTE: The present example uses a 2-down, 1-up adaptive tracking procedure to estimate the signal level associated with 71% correct detection16. The track continues for 8 reversals, and threshold is based on the last 6 reversals.
- Program the software to also present probe trials in Stage 3. Responses on probe trials reflect consistency of responses to supra-threshold signals across the testing session. During a probe trial, present the signal at the same clearly audible level used in the two training stages (Stage 1 and Stage 2). Randomly present probe trials twice out of every 12 trials. Consider a track invalid if the average probe hit rate is <80%.
For all three stages, program the software to require the observer to initiate a trial by clicking on a response box in the user interface.
Program the user interface to allow the observer to click on a box to indicate which interval contained the signal. After the response is entered, provide feedback to the observer indicating the interval that contained the signal.
- Program the software to activate two mechanical toys with lights that are located in dark Plexiglas boxes in the testing room.
- Use mechanical toys as reinforcements, in addition to an assistant providing social reinforcement in the test booth.
- Design the program to maintain a consistent delay between the signal and the activation of the toy, regardless of whether the signal occurs in interval 1 or 2. If the signal occurs in interval 1, the mechanical toy is activated immediately following the observer's response. If the signal occurs in interval 2, the mechanical toy activation is delayed by the interval duration plus the inter-stimulus interval (1,365 msec in this example).
- Activate the mechanical toy only if the observer correctly judges the interval that contained the signal.
3. Data Collection
Prepare the environment before the child arrives to the laboratory, as detailed in Figure 1.
Select 4 to 6 games for the test session based on the child's age, motor control, and interests. Examples include placing pegs into a board, putting blocks into a bucket, completing a puzzle, and placing felt pieces onto a board to make a scene.
Complete a listening check of the experimental stimuli and the observer-assistant communication system.
As soon as the child and parent arrive at the laboratory, obtain informed consent for participation in the study.
Instruct the child and parent to enter the booth. Children typically prefer that a parent sits next to them inside of the booth, and in some cases the child sits on the parent's lap.
Using child-friendly language, give the child and parent an overview of the task. Describe the sound(s) that the child will hear and model the targeted motor response.
- Have the experimenter or the assistant place the insert earphone or supra-aural headphones on the child.
- Position the child at eye-level, and allow the child to see and feel the insert earphone or headphone prior to placement.
- Provide the child with a sense of control by allowing him/her to choose where to clip the transducer or by having the child assist the experimenter in placing the headphones.
- If the child is reluctant to wear headphones, place the transducer on the parent or a doll to model the procedure.
- Terminate the testing session if in the unlikely event that the child is unwilling to wear the transducer or becomes distressed.
If the parent prefers to be in the control room during testing, have the observer escort the parent to the control room. Allow the parent to hear and see the child from the control room.
Have the assistant verify that the booth door(s) are closed.
Have the assistant place headphones on his/her ears in order to hear the observer in the control room, as well as the audio prompt marking each interval.
Have the assistant give the child a toy (e.g., a block) and instruct the child to place the object against his/her torso or cheek. This placement of the toy is called the "ready" position; the child uses this position throughout testing.
Require the observer to initiate a trial only if the child is in the ready position.
Have the observer initiate the conditioning stage (Stage 1). The goal of this Stage 1 is to condition the child to make a clear, time-locked motor response when he/she hears the target signal.
- To facilitate learning the task, have the assistant and child initially "listen together" using a hand-over-hand technique.
- Have the assistant place his/her hand on the child's hand. Have the assistant move the child's hand when the assistant hears the auditory interval marker for the second interval in his/her headset, because the signal is always present in interval 2 during Stage 1.
- Alternatively, have the assistant perform the task in parallel with the child.
- Have the assistant reduce the level of assistance with subsequent trials.
- If the child is slow to respond, encourage the child to respond as soon as he/she hears the target signal or ask the child to "race" the assistant.
- Continue presenting trials in Stage 1 until the observer is confident the child's responses are under stimulus control.
- Have the observer make this decision based on (1) whether the child is able to perform the motor task without assistance, and (2) whether the child is able to make a fast, time-locked response to the signal that the observer can judge.
- Require a minimum of 3 trials in this stage.
Have the observer initiate Stage 2 of testing. NOTE: In this stage, neither the observer nor the assistant know which test interval contains the signal. The observer must accurately judge 4 out of 5 sequential trials to successfully complete this stage. NOTE: The child is considered trained with the successful completion of Stages 1 and 2. If more than one session is needed, suspend the testing session at this point. It is recommended that testing resumes within two weeks. At the second visit, present a few reminder trials (using Stage 1) prior to initiating Stage 3 of testing.
Initiate Stage 3 to collect experimental data. As in Stage 2, have the observer closely watch the listener and judge which interval contains the signal. In addition to the motor-based play response, have the observer watch for subtle behaviors.
NOTE: Children often exhibit subtle behaviors to sound, including eye or head movement, changes in facial expression, and quieting of activity17,18. Have the observer use these subtle behaviors to judge which interval contained the signal when the signal level is near a child's threshold.
Have the assistant switch the game every 10-15 trials to maximize the child's interest and reduce the risk of habituation9. Have the assistant provide frequent social reinforcement to the child to engage the child and to shape and maintain the child's behavior.
- If the child stops responding in a consistent manner, the child may have "forgotten" what the signal sounds like or may have habituated to the play-based task. Employ the following strategies to increase the child's participation:
- Have the assistant reinstruct the child and model the response for the child. Have the assistant introduce a new game.
- Provide more reinforcement, either by increasing social reinforcement from the assistant or activating the mechanical toys controlled by the custom software.
For 2 and 3 year-olds, terminate testing after the completion of Stage 3. For children who are 4 years or older, run a second adaptive track if desired. Prior to starting a second track, give children a short break (5-10 min) to play.
At the conclusion of testing, complete a screening tympanogram to evaluate middle ear functioning. Perform the screening at the end of the visit because some children are more receptive to this procedure after spending time in the test environment and becoming familiar with the testers.
Compensate the participant and schedule a follow-up visit, if needed.
4. Data Analysis
Average the signal level at the last 6 reversals of the adaptive track to calculate the detection threshold.
Compute the standard deviation of the last 6 reversal levels. In order for a threshold to be considered valid, the standard deviation must be below a criterion established based on pilot data. A high standard deviation indicates that the reversal levels were widely spaced, possibly due to inconsistencies in the observer's judgements or listeners factors such as training effects, fatigue, or off-task behaviors.
Calculate the hit rate for probe trials by determining the proportion of probe signal trials that were correctly judged by the observer during Stage 3 of testing. In order for a threshold to be considered valid, the probe hit rate must meet the minimum criterion of 0.80. Failure to meet this criterion is because of inconsistent responses to supra-threshold signals, which may indicate fatigue, off-task behavior, or inadequate training for the listener and/or the observer.
Representative Results
Thirty-three children were recruited from a database of children who are typically-developing, based on parental report. Inclusion criteria included no known history of hearing loss, no more than three episodes of otitis media, and no episodes of otitis media in the month prior to testing. Eight 2 year-olds, eighteen 3 year-olds, and seven 4 year-olds met these inclusion criteria. Of the children recruited, three would not tolerate the insert earphone and testing was not attempted.
Of the remaining 30 children, all but one child (a 2 year-old) successfully completed both training stages (Stage 1 and Stage 2). On average, children required 4.8 trials (SD = 2.4; max = 12) in Stage 1 and 4.1 trials (SD = 0.3; max = 5) in Stage 2. Two 2 year-olds and one 3 year-old were only able to complete training during the first visit; two of these children returned for a second visit and successfully completed Stage 3. All remaining children completed the protocol in a single session. On average, children required 40.0 trials to complete Stage 3 (SD = 7.9; min = 27; max = 57). All 28 children who completed Stage 3 of testing met the probe rate criterion of ≥0.80; all probe signal trials were correctly identified in 75% of testing sessions. Only one child's data were excluded based on excessive variability; in this case, the standard deviation of reversal values exceeded the criterion of 4.4 dB.
Figure 2 shows individual children's thresholds as a function of age. Thresholds for all children with normal middle ear functioning, based on tympanometry on the day of testing, are shown by the open circles. Six additional children (21%) had abnormal tympanograms, indicating possible middle ear dysfunction (e.g., middle ear fluid). Data shown with filled symbols indicate abnormal middle ear function based on tympanometry: reduced compliance (Type B; square) or excessive negative pressure (Type C; triangle). One additional child would not tolerate the test procedure for screening tympanometry, so his middle ear status is unknown (diamond). Interpret threshold values from children with abnormal middle ear function cautiously because abnormal middle ear status is associated with elevated thresholds19. Thresholds obtained from children are broadly consistent with previous data on this age group. For example, Schneider at al.20 estimated psychometric functions for detecting an octave-wide band of noise at 1,000 Hz in preschoolers. Defining threshold as the level associated with 65% correct, the mean threshold was approximately 21 dB SPL for 3 year-olds and 14 dB SPL for 4 year-olds.
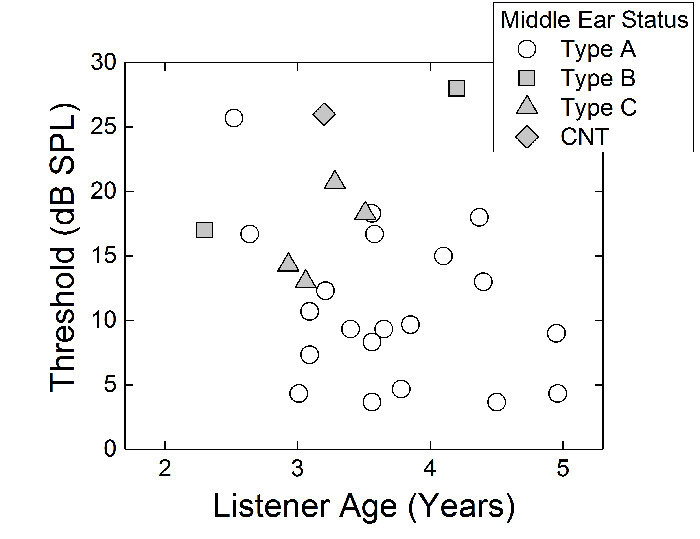 Figure 2: Warble-tone detection thresholds. Detection thresholds are plotted as a function of child age. Only the first threshold obtained from each listener is shown. Symbol shape reflects the middle ear status of the listener: Type A (circle), Type B (square), Type C (triangle), or could not test (CNT; diamond). Whereas Type A indicates normal middle ear admittance, Type B (flat) and Type C (negative pressure) are typically associated with reduced middle ear function due to fluid, congestion, or ear infection. Please click here to view a larger version of this figure.
Figure 2: Warble-tone detection thresholds. Detection thresholds are plotted as a function of child age. Only the first threshold obtained from each listener is shown. Symbol shape reflects the middle ear status of the listener: Type A (circle), Type B (square), Type C (triangle), or could not test (CNT; diamond). Whereas Type A indicates normal middle ear admittance, Type B (flat) and Type C (negative pressure) are typically associated with reduced middle ear function due to fluid, congestion, or ear infection. Please click here to view a larger version of this figure.
Thresholds were also measured for a group of young adults with normal hearing sensitivity and middle ear status on the day of testing (n = 8; 20-25 years). Due to procedural modifications between the two age groups, caution is warranted when comparing the child and adult data. The primary protocol difference between the two age groups was that an assistant inside of the booth was not present when testing adults. In contrast to children who were provided reinforcement through social engagement with the assistant, adults were provided only with trial-by-trial feedback through the activation of mechanical toys. Adults completed two consecutive adaptive tracks in a single testing session. However, only the threshold from the first adaptive track run was considered here. The mean adult threshold for the warble stimulus was 2.4 dB SPL (SD = 1.7 dB). In the present study, the group difference in threshold between adults and the 3 year-olds, with normal middle ear function, was 7.2 dB. This observed child-adult difference is smaller than has been reported in some studies20. However, the magnitude of the child-adult difference is likely influenced by both the overall procedure and any procedural modifications implemented between children and adults. Further research is needed to better understand how children's and adults' sensitivity to the stimulus is affected by modifications to the two-interval, observer-based procedure described in this paper.
Discussion
This paper described a two-interval, forced-choice behavioral procedure for measuring hearing abilities in 2 to 4 year old children. In this procedure, an observer judges whether the signal is presented in interval 1 or interval 2 based solely on the listener's behavior. Children's behavior is shaped to be time-locked to the presentation of the signal by training them to perform a play-based response to the sound. Our preliminary results indicate this method is feasible and reliable for testing the hearing sensitivity of 2 to 4 year-olds.
Significance of the Procedure
There are several advantages associated with this method. The first advantage is that it can be used to test children as young as 2.0 years developmental age. Thresholds were successfully measured for 5 out of the 8 2-year-olds. A similar yield rate (~60-70%) has been reported in the literature for the measurement of hearing sensitivity in 2-year-olds using conditioned-play audiometry in the soundfield9,21. As with conditioned-play audiometry7,8, thresholds were successfully measured for all but one of the 3 year-olds, and all 4 year-olds. The second advantage of this method is that it guards against observer response bias. The observer must base his/her judgments solely on the child's behavior, so prior expectations regarding the child's sensitivity or behavior do not affect the results. The third advantage of this method is that it may be easier for the observer to judge which interval contains the signal than to make a yes-no decision regarding the presence or absence of a signal. In the present two-interval task, the observer is able to compare the child's behavior across the two intervals rather than comparing behavior across multiple trials, as is required in the single-interval task. Thus, the memory load on the observer may be smaller for the two-interval relative to the single-interval task. Moreover, looking for time-locked changes in behavior may allow the observer to adapt to changes in the child's behavior that occur during the testing session.
Limitations
There are a few limitations to consider when applying this method. First, pilot data are required to determine the appropriate parameters – training criteria, starting level, inter-stimulus interval value, and transducer – to use for different age groups and stimuli. In particular, adjusting testing parameters may affect the number of 2 year-olds who can successfully do the task and provide useable experimental data. Yield rate for 2 year-olds may be improved by presenting stimuli through the soundfield or headphones rather than an insert earphone. However, precautions must be taken when performing testing in the soundfield to prevent the assistant and parent from hearing the signal (see Leibold et al.22 for specifics.) A longer inter-stimulus interval may be required for younger children than for older children, if younger listeners take longer to complete the play-based response. Also, 2 year-olds may require greater training and may fatigue faster than older children. In order to guard against fatigue, it is recommended to change toys frequently9 and provide frequent breaks in testing. Recall that we tested three of the youngest children over two visits, rather than one. Second, it is not clear how much experience is required for observers and assistants to obtain reliable results using this procedure. In this example, all observers and assistants had at least two years of experience testing toddlers and preschoolers in the audiology clinic using play-based audiometry, as well as at least one additional year of experience in the laboratory testing infants and/or school-aged children. It is recommended to establish protocols for training new observers and to ensure consistent performance for trained observers. Further research is needed to determine the reliability of this method across observers and laboratories.
Future Applications
It may be possible to modify this procedure to test children who are unable to perform conventional motor responses. For example, the conditioned response could be an eye movement, head turn, or a change in activity level14. Previous work has shown that trained observers can reliably use these alternative behaviors to test infants as young as 1 month of age using a single-interval, observer-based method23. Furthermore, the single-interval, observer-based method has been used to measure hearing sensitivity in special populations, including 2 to 12 month-olds with Down Syndrome24 and 26 to 36 month-olds with cochlear implants25. Results from these previous studies support the feasibility of testing children who cannot produce a play-based, motor response with a two-interval paradigm.
Whereas the current study evaluated detection thresholds in quiet, this procedure can also be used to evaluate masked detection or discrimination. In the case of masking noise, previous studies of infants tested with the single-interval, observer-based procedure suggest that the masker be played continuously over the course of an adaptive track in order to avoid responses to masker onsets and/or offsets26. Similarly, to evaluate discrimination abilities, a standard sound is presented repeatedly apart from the signal interval, during which the signal stimulus would be presented27. For all stimulus conditions, the listener would be conditioned to respond when he/she detects a change in the stimulus, whether that change is the addition of a sound (detection) or a change in the sound (discrimination). While the current study used an adaptive procedure to estimate threshold, the same procedures could be used to evaluate percent correct performance at a fixed signal and/or masker level. Another possible modification is that the stimuli can be presented through other transducers, including the soundfield13,22.
In summary, the play-based, two-interval procedure described here provides reliable behavioral data on the hearing abilities of toddlers and preschoolers. Using this method, researchers will be able to study how the auditory system changes during the toddler and preschooler years – a time period where we know little about auditory behavior.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgments
Research reported in this publication was supported by the National Institute on Deafness and Other Communication Disorders of the National Institutes of Health under award number R01DC014460. Video production and editing was carried out by Robert Ladd and Barbara Rochen Renner of the Health Sciences Library at The University of North Carolina at Chapel Hill, with support from a National Library of Medicine of the National Institutes of Health Administrative Supplement for Informationist Services in NIH-funded Research Projects under award number R01DC011038. Children were recruited through the Research Participant Registries of the IDDRC at The University of North Carolina at Chapel Hill (NIH-NICHD award number U54HD079124). We appreciate Emily Buss' comments on this procedure and a previous version of this article. The authors would also like to thank Steve Lockhart for programming support and members of the Human Auditory Development Laboratory for testing assistance: Jenna Browning, Lauren Charles, Nicole Corbin, Molly Drescher, Hannah Hodson McLean, Heather Porter and Dani Warmund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Eisenberg LS, Martinez AS, Boothroyd A. Assessing auditory capabilities in young children. Int J Pediatr Otorhinolaryngol. 2007;71(9):1339–1350. doi: 10.1016/j.ijporl.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primus MA, Thompson G. Response strength of young children in operant audiometry. J. Speech Hear. Res. 1985;28(4):539–547. doi: 10.1044/jshr.2804.539. [DOI] [PubMed] [Google Scholar]
- Allen P, Wightman F. Spectral pattern discrimination by children. J. Speech Hear. Res. 1992;35(1):222–233. doi: 10.1044/jshr.3501.222. [DOI] [PubMed] [Google Scholar]
- Jensen JK, Neff DL. Development of basic auditory discrimination in preschool children. Psychol. Sci. 1993;4(2):104–107. [Google Scholar]
- Thompson M, Thompson G. Response of infants and young children as a function of auditory stimuli and test methods. J. Speech Hear. Res. 1972;15(4):699–707. doi: 10.1044/jshr.1504.699. [DOI] [PubMed] [Google Scholar]
- Diefendorf AO. Hearing Impairment in Children. New York Press; 1988. Behavioral evaulation of hearing impaired children; pp. 133–151. [Google Scholar]
- Barr B. Pure tone audiometry for preschool children; a clinical study with particular reference to children with severely impaired hearing. Acta Otolaryngol Suppl. 1955;121:1–84. [PubMed] [Google Scholar]
- Thompson G, Weber BA. Responses of infants and young children to behavior observation audiometry (BOA) J Speech Hear Disord. 1974;39(2):140–147. doi: 10.1044/jshd.3902.140. [DOI] [PubMed] [Google Scholar]
- Thompson M, Thompson G, Vethivelu S. A comparison of audiometric test methods for 2-year-old children. J Speech Hear Disord. 1989;54(2):174–179. doi: 10.1044/jshd.5402.174. [DOI] [PubMed] [Google Scholar]
- Green DM, Swets JA. Signal detection theory and psychophysics. John Wiley & Sons, Inc; 1966. [Google Scholar]
- Widen JE, O'Grady GM. Using visual reinforcement audiometry in the assessment of hearing in infants. Hear J. 2002;55(11):28–36. [Google Scholar]
- Wightman F, Allen P, Dolan T, Kistler D, Jamieson D. Temporal resolution in children. Child Dev. 1989;60(3):611–624. [PubMed] [Google Scholar]
- Browning J, Buss E, Leibold LJ. Preliminary evaluation of a two-interval, two-alternative infant behavioral testing procedure. J. Acoust. Soc. Am. 2014;136(3):EL236–EL241. doi: 10.1121/1.4893333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsho LW, Koch EG, Halpin CF, Carter EA. An observer-based psychoacoustic procedure for use with young infants. Dev. Psychol. 1987;23(5):627–640. [Google Scholar]
- Bonino AY, Corbin N, Leibold LJ. Preliminary evaluation of target/masker sex mismatch for preschoolers' speech-on-speech detection. American Speech-Language Hearing Association Conference; Denver, CO. 2015. [Google Scholar]
- Levitt H. Transformed up-down methods in psychoacoustics. J. Acoust. Soc. Am. 1971;49(2B):467–477. [PubMed] [Google Scholar]
- Bargones JY, Werner LA, Marean GC. Infant psychometric functions for detection: Mechanisms of immature sensitivity. J. Acoust. Soc. Am. 1995;98(1):99–111. doi: 10.1121/1.414446. [DOI] [PubMed] [Google Scholar]
- Watrous BS, McConnell F, Sitton AB, Fleet WF. Auditory responses of infants. J Speech Hear Disord. 1975;40(3):357–366. doi: 10.1044/jshd.4003.357. [DOI] [PubMed] [Google Scholar]
- MRC Multi-Centre Otitis Media Study Group. Sensitivity, specificity and predictive value of tympanometry in predicting a hearing impairment in otitis media with effusion. Clin Otolaryngol Allied Sci. 1999;24(4):294–300. doi: 10.1046/j.1365-2273.1999.00259.x. [DOI] [PubMed] [Google Scholar]
- Schneider BA, Trehub SE, Morrongiello BA, Thorpe LA. Auditory sensitivity in preschool children. J. Acoust. Soc. Am. 1986;79(2):447–452. doi: 10.1121/1.393532. [DOI] [PubMed] [Google Scholar]
- Nielsen SE, Olsen SO. Validation of play-conditioned audiometry in a clinical setting. Scand. Audiol. 1997;26(3):187–191. doi: 10.3109/01050399709074992. [DOI] [PubMed] [Google Scholar]
- Leibold LJ, Taylor CN, Hillock-Dunn A, Buss E. Effect of talker sex on infants' detection of spondee words in a two-talker or a speech-shaped noise masker. Proc. Mtgs. Acoust. 2013;19:060074. [Google Scholar]
- Werner LA, Gillenwater JM. Pure-tone sensitivity of 2- to 5-week-old infants. Infant Behav. Dev. 1990;13(2):355–375. [Google Scholar]
- Werner LA, Mancl LR, Folsom RC. Preliminary observations on the development of auditory sensitivity in infants with Down syndrome. Ear Hear. 1996;17(6):455–468. doi: 10.1097/00003446-199612000-00002. [DOI] [PubMed] [Google Scholar]
- Grieco-Calub TM, Litovsky RY, Werner LA. Using the observer-based psychophysical procedure to assess localization acuity in toddlers who use bilateral cochlear implants. Otol. Neurotol. 2008;29(2):235–239. doi: 10.1097/mao.0b013e31816250fe. [DOI] [PubMed] [Google Scholar]
- Leibold LJ, Werner LA. Effect of masker-frequency variability on the detection performance of infants and adults. J. Acoust. Soc. Am. 2006;119(6):3960–3970. doi: 10.1121/1.2200150. [DOI] [PubMed] [Google Scholar]
- Werner LA. Infants' detection and discrimination of sounds in modulated maskers. J. Acoust. Soc. Am. 2013;133(6):4156–4167. doi: 10.1121/1.4803903. [DOI] [PMC free article] [PubMed] [Google Scholar]


