Abstract
Ocular yeast infections in diabetics are a therapeutic challenge. Drug resistance and reduced azole susceptibility are major concerns. The case we describe characterizes a Candida albicans strain from a vitrectomy specimen that was susceptible to fluconazole by in vitro testing but recalcitrant to therapy. Molecular studies revealed transient overexpression of CDR1 and ERG11 mRNA in the presence of fluconazole that may have contributed to poor clinical response in this patient.
CASE REPORT
A 48-year-old human immunodeficiency virus-negative woman with a past medical history of insulin-dependent diabetes mellitus, congenital absence of one kidney, recurrent pyelonephritis, and gastric bypass surgery presented to the emergency department with pain and visual loss in her right eye. She responded poorly to treatment with prednisone (60 mg daily) for presumed sarcoid uveitis. A Candida spp. (designated NYP-1) was isolated from a vitrectomy culture. She received an intravitreal injection of amphotericin B and then fluconazole (FLU; 400 mg daily) for 4 months. Her FLU dose was subsequently lowered to 200 mg daily secondary to clinical stability. On follow-up 1 week later, she developed a new choroidal lesion adjacent to the optic disk in her left eye. Treatment was changed to caspofungin and liposomal amphotericin B (5 mg/kg of body weight daily). Although the initial lesions regressed, new satellite lesions appeared during this therapy. Caspofungin was subsequently discontinued secondary to concerns regarding pharmacologic antagonism between the antifungal agents, and the dose of amphotericin B was increased (7.5 mg/kg daily) to maximize penetration into the eye. Her left eye lesions resolved with this treatment, and no further infections were noted in the left eye.
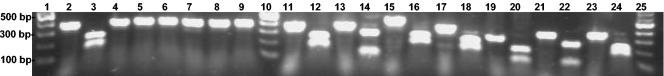
Candida dubliniensis has been reported to respond poorly to azole drugs (7). NYP-1 was characterized by both phenotypic and genotypic methods to definitively differentiate Candida albicans from Candida dubliniensis and to determine drug resistance mechanisms that could account for therapeutic failure. Phenotypically, the isolate was identified as C. albicans by formation of germ tubes at 37°C in horse serum (Life Technologies, Grand Island, N.Y.), production of chlamydospores on cornmeal agar with polysorbate 80 (Becton Dickinson Microbiology Systems, Cockeysville, Md.), substrate assimilation with the API 20C AUX (bioMérieux Inc., Hazelwood, Mo.; bionumber 2174174) and Rapid Yeast Identification Panel (Dade Microscan, Sacramento, Calif; bionumber 745032001), colorimetric growth on CHROMagar Candida plates (DRG International, Mountainside, N.J.), and growth at 42°C. Despite advances in phenotypic detection methods, results can be problematic (1, 8), so molecular evaluation of the ribosomal ITS2 region of the NYP-1 isolate was used to independently verify the species identification. PCR-restriction enzyme analysis (REA) and DNA sequence-based studies were performed utilizing the species-specific ITS2 spacer region of rRNA genes (ribosomal DNA) (5). Fragment analysis showed the NYP-1 ITS2 region to be ∼300 bp, similar in size to control ITS2 DNA of C. albicans, C. dubliniensis, Candida krusei, Candida parapsilosis, and Candida tropicalis. Results showed that only the C. albicans ITS2-specific restriction enzyme AlwI digested the NYP-1 ITS2 region (Fig. 1). All control DNA was appropriately digested by species-specific ITS2 region restriction enzymes. Based on ITS2 region fragment and PCR-REA, the isolate NYP-1 was confirmed as C. albicans (Fig. 1).
FIG. 1.
NYP-1 and reference Candida strain ITS2 region fragment and REA. The ITS2 region was amplified by PCR with universal fungal primers ITS3 and ITS4. Lane 2, NYP-1 ITS2 PCR amplification product. The products were digested with restriction enzymes AlwI (C. albicans specific; lane 3), BsmAI (C. dubliniensis specific; lane 4), HpaI (Candida glabrata specific; lane 5), FspI (C. krusei specific; lane 6), BsmI (Candida lusitaniae specific; lane 7), RsaI (C. parapsilosis specific; lane 8), and SmaI (C. tropicalis specific; lane 9). The REA patterns were compared to those for known control strains. These included ATCC 90028 (C. albicans; ITS2 region only; lane 11), ATCC 90028 (C. albicans; ITS2 region plus AlwI fragment; lane 12), NCPF 3949 (C. dubliniensis; ITS2 region only [lane 13] and ITS2 region plus BsmAI fragment [lane 14]), ATCC 90030 (C. glabrata; ITS2 region only; lane 15), ATCC 90030 (C. glabrata; ITS2 region plus Hpa1 fragment; lane 16), ATCC 6258 (C. krusei; ITS2 region only; lane 17), ATCC 6258 (C. krusei; ITS2 region plus Fsp1 fragment; lane 18), ATCC 200950 (C. lusitaniae; ITS2 region only; lane 19), ATCC 200950 (C. lusitaniae; ITS2 region plus BsmI fragment; lane 20); ATCC 90018 (C. parapsilosis; ITS2 region only; lane 21), ATCC 90018; C. parapsilosis; ITS2 region plus RsaI fragment; lane 22); ATCC 750 (C. tropicalis; ITS2 region only; lane 23), and ATCC 750 (C. tropicalis; ITS2 region plus SmaI fragment; lane 24). Lanes 1, 10, and 25, DNA markers. The ITS2 PCR products and restriction fragments were run on a 1.2% agarose gel and stained with GelStar (FMC Bioproducts).
Susceptibility testing guidelines for broth microdilution were followed according to NCCLS Standard M27-A (4), using the yeast 1 colorimetric panel (Trek Diagnostics, Westlake, Ohio) containing the following antifungal drugs at the indicated MIC ranges: amphotericin B, 0.008 to 16 μg/ml; FLU, 0.125 to 256 μg/ml; itraconazole, 0.008 to 16 μg/ml; ketoconazole, 0.008 to 16 μg/ml; 5-flucytosine (5-FC), 0.03 to 64 μg/ml. C. krusei ATCC 62258 and C. parapsilosis ATCC 22019 were used as quality control strains. Results showed NYP-1 to be susceptible to FLU (MIC, 0.25 μg/ml), itraconazole (MIC, ≤0.008 μg/ml), 5-FC (MIC, 0.24 μg/ml), and amphotericin B (MIC, 0.128 μg/ml). The MIC of voriconazole was reported as ≤0.125 μg/ml (data not shown).
NYP-1 was characterized for known azole resistance mechanisms (2). The ERG11 gene, encoding lanosterol 14-α-demethylase, was amplified by PCR, and the DNA sequence of the ∼1.5-kb coding region was determined to see if point mutations known to cause resistance were present. Azole-susceptible strain C. albicans ATCC 90028 was used as a control (NCCLS Standard M27-A). NYP-1 and the control strain showed a sequence identity of >99% (data not shown). Neither strain contained any point mutations that correlated with azole resistance. Molecular Beacon quantitative reverse transcription-PCR (MB QRT-PCR) was performed to probe for overexpression of ERG11 and drug efflux pump genes CDR1 (ABC transporter class), CDR2, FLU1, and MDR1 as described previously (3). RNA was extracted from NYP-1 and ATCC 90028 cultures grown at 8, 24, and 48 h in the absence and presence of FLU (32 μg/ml) for MB QRT-PCR transcript analysis. Copy numbers of the known drug resistance genes relative to that of PMA1, a highly and constitutively expressed gene encoding the essential plasma membrane proton pump, were measured. Without the addition of FLU, no noticeable differences (defined as greater than fivefold) in CDR1, CDR2, ERG11, FLU1, and MDR1 copies were observed for NYP-1 and ATCC 90028. However, at 8 h of FLU exposure, twofold increases in ERG11 copy numbers were observed for NYP-1. After 24 h of FLU exposure, a 10-fold increase in CDR1, a multidrug efflux pump gene, and a 7-fold increase in ERG11 were observed. At 48 h of FLU exposure, CDR1 mRNA levels were reduced to the pre-drug-induced state, yet higher (approximately an eightfold increase) ERG11 copy numbers were maintained. FLU1 and MDR1, FLU-specific efflux pump genes (multifacilitator class), levels were not changed in both strains.
In conclusion, the patient isolate was genotypically confirmed as C. albicans and not C. dubliniensis. Despite in vitro susceptibility to fluconazole, the initial therapeutic failure with this drug may have resulted from either inadequate drug penetration to the infected eye site or drug-induced overexpression of CDR1 and ERG11 in NYP-1. CDR1 and ERG11 overexpression has been linked to resistance in other clinical strains of C. albicans (2, 6, 7, 9). Further research correlating genetic and phenotypic susceptibility test results with clinical outcomes is warranted.
REFERENCES
- 1.Gales, A. C., M. A. Pfaller, A. K. Houston, S. Joly, D. J. Sullivan, D. C. Coleman, and D. R. Soll. 1999. Identification of Candida dubliniensis based on temperature and utilization of xylose and α-methyl-d-glucoside as determined with the API 20C AUX Vitek YBC systems. J. Clin. Microbiol. 37:3804-3808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maebashi, K., M. Niimi, M. Kudoh, F. J. Fischer, K. Makimura, K. Niimi, R. J. Piper, K. Uchida, M. Arisawa, R. D. Cannon, and H. Yamaguchi. 2001. Mechanisms of fluconazole resistance in Candida albicans isolates from Japanese AIDS patients. J. Antimicrob. Chemother. 47:527-536. [DOI] [PubMed] [Google Scholar]
- 3.Nascimento, A. M, G. H. Goldman, S. Park, S. A. E. Marras, G. Delmas, U. Oza, K. Lolans, and D. S. Perlin. 2003. Differential expression of two novel Aspergillus fumigatus putative efflux pump genes in mutants with high-level resistance to itraconazole. Antimicrob. Agents Chemother. 47:1719-1726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Committee for Clinical Laboratory Standards. 1997. Reference method for broth dilution antifungal susceptibility testing of yeasts. Approved standard M-27-A. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 5.Park, S., M. Wong, S. A. Marras, E. W. Cross, T. E. Kiehn, V. Chaturvedi, S. Tyagi, and D. S. Perlin. 2000. Rapid identification of Candida dubliniensis using a species-specific molecular beacon. J. Clin. Microbiol. 38:2829-2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perea, S., J. L. Lopez-Ribot, W.R. Kirkpatrick, R. K. McAtee, R. A. Santillan, M. Martinez, D. Calabrese, D. Sanglard, and T. F. Patterson. 2001. Prevalence of molecular mechanisms of resistance to azole antifungal agents in Candida albicans strains displaying high-level fluconazole resistance isolated from human immunodeficiency virus-infected patients. Antimicrob. Agents Chemother. 45:2676-2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perea, S., J. L. Lopez-Ribot, B. L. Wickes, W. R. Kirkpatrick, O. P. Dib, S. P. Bachmann, S. M. Keller, M. Martinez, M., and T. F. Patterson. 2002. Molecular mechanisms of fluconazole resistance in Candida dubliniensis isolates from human immunodeficiency virus-infected patients with oropharyngeal candidiasis. Antimicrob. Agents Chemother. 46:1695-1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pincus, D. H., D. C. Coleman, W. R. Pruitt, A. A. Padhye, I. F. Salkin, M. Geimer, A. Bassel, D. J. Sullivan, M. Clarke, and V. Hearn. 1999. Rapid identification of Candida dubliniensis with commercial yeast identification systems. J. Clin. Microbiol. 37:3533-3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White, T. C. 1997. Increased mRNA levels of ERG16, CDR, and MDR1 correlate with increases in azole resistance in Candida albicans isolates from a patient infected with human immunodeficiency virus. Antimicrob. Agents Chemother. 41:1482-1487. [DOI] [PMC free article] [PubMed] [Google Scholar]