Abstract
OBJECTIVE
To quantify the contribution of acute versus post-acute care factors to survival and functional outcomes after hip fracture.
DESIGN, SETTING, AND PARTICIPANTS
Retrospective cohort study using Medicare data; subjects included previously ambulatory nursing home residents hospitalized for hip fracture between 2005 and 2009.
METHODS
We used logistic regression to measure the associations of hospital and nursing home factors with functional and survival outcomes at 30 and 180 days among patients discharged to a nursing facility; we quantified the contribution of hospital versus nursing home factors to outcomes via the omega statistic.
RESULTS
Among 45,996 hospitalized patients, 1,814 (3.9%) died during hospitalization. 42,781 (93%) were discharged alive to a nursing home. Of these, 12,126 (28%) died within 180 days and 20,479 (48%) died or were newly unable to walk within 180 days. Hospital characteristics were not consistently associated with outcomes. Multiple nursing home characteristics predicted 30- and 180-day outcomes, including bed count, chain membership, and performance on selected quality measures. Nursing home factors explained three times more variation in the odds of 30-day mortality than did hospital factors (omega, hospital versus nursing home: 0.32, 95% confidence interval (CI) 0.11, 0.96), seven times more variation in the odds of 180-day mortality (omega: 0.15, 95% CI 0.04, 0.61), and eight times more variation in the odds of 180-day death or new dependence in locomotion (omega: 0.12, 95% CI 0.05, 0.31).
CONCLUSIONS
Nursing home factor sex plain a larger proportion of the variation in clinical outcomes following hip fracture than do hospital factors.
Keywords: Hip fracture, post-acute care, patient-centered outcomes
INTRODUCTION
Post-acute care represents a large and growing source of US healthcare spending. Medicare spending for post-acute care exceeded $62 billion in 2012,(1) with evidence that spending on post-acute care has increased far out of proportion to total Medicare spending for patients hospitalized with common conditions.(2)
Nonetheless, little is known regarding the relative impact of variations in the quality of care across acute versus post-acute settings on survival and functional outcomes after an inpatient care episode. Such information may help health systems determine how to best direct resources under bundled payment models,(3) assist policy makers in selecting targets for quality improvement initiatives, and guide patients’ care choices.
We examined the relative contribution of acute- and post-acute care facility factors to clinical outcomes among fee-for-service Medicare beneficiaries treated for acute hip fracture, a common and highly morbid event.(4, 5) Employing a large national cohort of previously ambulatory nursing home residents hospitalized with hip fracture, we quantified the contribution of selected acute and post-acute care facility factors to explaining variations in the probability of dying or developing new total dependence in locomotion at up to 180 days after hospital discharge, and to explaining the probability of death at 30 and 180 days after discharge. We hypothesized that, taken together, nursing home characteristics would explain a greater share of the variation in outcomes than would hospital characteristics.
METHODS
Study design
Comparing the contribution of acute and post-acute care facility factors to a patient’s outcome requires that the patient in question received both acute and post-acute care. The relative contribution of acute care versus post-acute care factors to outcomes cannot be calculated for patients who do not receive post-acute care, such as those who die in-hospital.
At the same time, an analysis restricted to those patients who survive hospitalization may yield misleading findings since it censors in-hospital deaths. If inpatient mortality is higher in certain hospitals, an analysis limited to hospital survivors may underestimate the importance of hospital factors to patient outcomes by ignoring the potential contribution of such characteristics to survival.
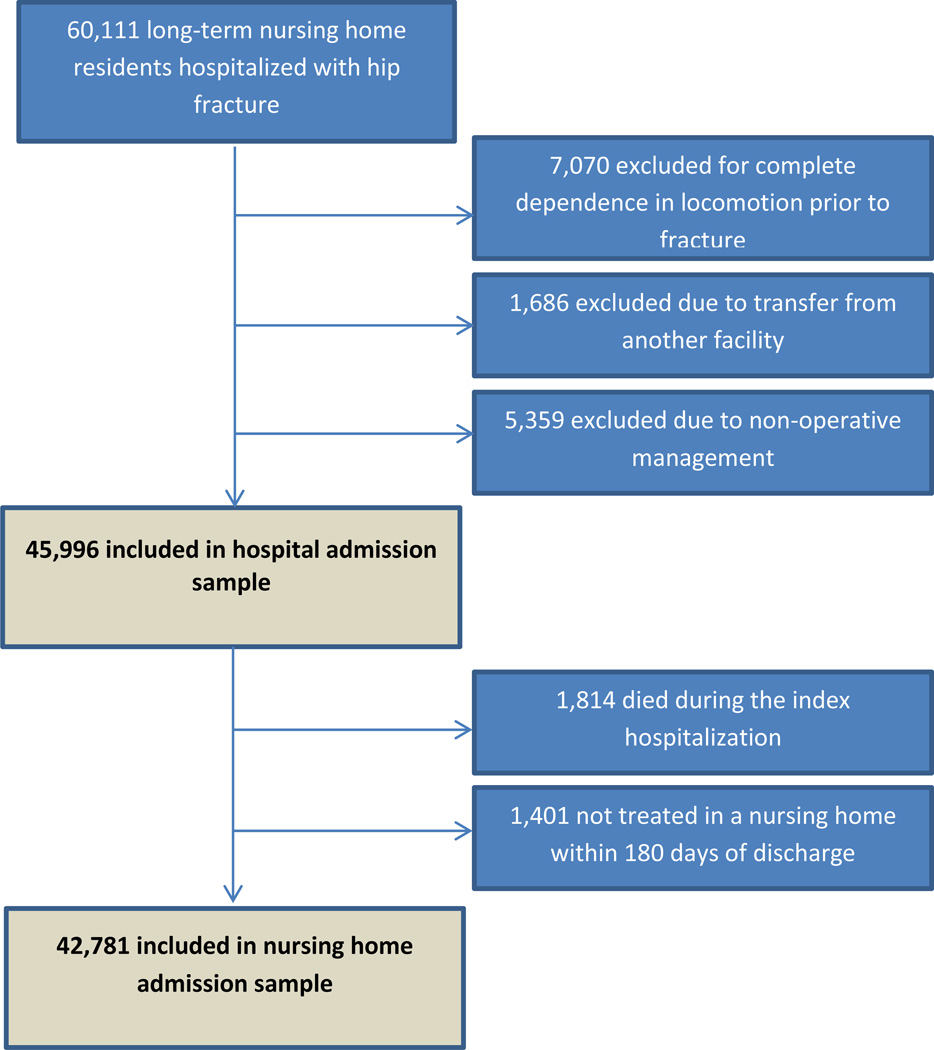
To address this issue, we present two complementary analyses (Figure 1) using a pair of overlapping samples. The “hospital admission sample” includes all patients in our cohort hospitalized with hip fracture. The “nursing home admission sample” examines those patients from the first sample who survived hospitalization and received nursing home care within 180 days of hospital discharge.
Figure 1. Development of the study samples.
Development of the hospital admission and nursing home admission samples
We first measure the association of selected hospital factors with an endpoint of inpatient mortality within the hospital admission sample to characterize the contribution of hospital factors to the probability of surviving to discharge. Next, we compare the contribution of nursing facility factors versus hospital factors to the primary study outcome, namely the development of new total dependence in locomotion or death at 180 days after hospital discharge among patients in the nursing home admission sample. This endpoint was selected as the primary study outcome because the restoration of ambulatory ability represents the primary goal of acute and post-acute care for hip fracture patients, and because hip fracture patients view the preservation of independence as an endpoint of primary importance.(7, 8)
We also compare the contribution of nursing facility versus hospital factors to two secondary outcomes within nursing home admission sample: death prior to 30 days after discharge and death prior to 180 days after discharge.
Data sources and study sample
Our study sample came from a previously characterized cohort of Medicare fee-for-service beneficiaries hospitalized with hip fracture between January 1, 2005 and June 30, 2009 who resided in a nursing facility during the 180 days prior to hip fracture and who could ambulate without human assistance prior to fracture.(9) We focused on nursing home residents with hip fracture because they are at high risk of poor short- and long-term outcomes after fracture(9) and because they are commonly discharged after to nursing facilities versus other settings for post-acute care, reducing the potential influence on outcomes of selection of individual patients into different post-acute care settings.(10)
Data came from: (1) Medicare Provider Analysis and Review (MedPAR) files, which contain hospital discharge abstracts for fee-for services Medicare beneficiaries; (2) the Medicare Beneficiary Summary File, which contains vital status and HMO enrollment data; (3) the Medicare Provider of Services (POS) and the Online Survey Certification and Reporting (OSCAR) databases, which contain information on hospital and nursing home facility characteristics; (4) the Medicare Long-Term Care Minimum Data Set, which contains clinical assessment data collected at admission and every 92 days for long-stay nursing home residents; and (5) the Medicare Nursing Home Compare website.(11)
Hip fracture admissions and surgical procedures were identified using ICD-9-CM diagnosis and procedure codes,(12) which are highly sensitive and specific for hip fracture diagnoses and treatments.(13) We identified individuals who were residing in a nursing home during the 180 days prior to fracture based on the presence of two or more admission or quarterly MDS assessments in the 180 days prior to the hip fracture admission date as in prior work.(9) For patients with more than one hip fracture admission over this period, only the first admission was used in our analysis. We excluded patients who were admitted directly from another acute-care hospital. Because our goal was to examine recovery of independence in locomotion as a study outcome, we restricted our analysis to those patients who were able to ambulate with or without human assistance prior to fracture, as recorded in the last MDS assessment before fracture.
Independent variables
Acute and post-acute care facility factors
We obtained data on the following hospital characteristics: (1) nurse-to-bed ratio;(14) (2) nurse skill mix, calculated as the number of full-time registered nurses and licensed practical nurses divided by the total number of nursing staff; (3) resident-to-bed ratio;(15) (4) non-profit versus for-profit ownership status; (5) bed count (fewer than 200 beds; 200–399 beds; 400 or more beds); and (6) hospital referral region-level hospital market concentration, as measured by the Herfindahl-Hirschman index (HHI)(16)
To obtain a measure of past hospital performance for hip fracture care, we calculated observed-to-expected (O:E) ratios for 30-day hip fracture mortality based on data from January 1, 2003 through December 31, 2003 as described elsewhere;(17) hospitals with 50 or more hip fractures per year or more were classified into one of four quartiles of historical risk-adjusted mortality (high, high-moderate, low-moderate, and low) based on O:E ratio. As O:E ratios may be unreliable for low-volume facilities,(18) we did not calculate them for facilities with fewer than 50 cases per year; instead, these facilities were grouped into a fifth category of “low volume” facilities for purposes of comparison.
We obtained data on the following nursing home factors: (1) ownership status (for-profit, non-profit, government);(19, 20) (2) hospital-based versus non-hospital based location;(21) (3) use of advance practice nurses;(22) (4) (5) chain membership;(19, 23, 24) (6) presence of a full-time director of nursing;(25) (7) bed count (fewer than 100 beds; 100–149 beds; 150 or more beds);(21, 26) (8) payer mix; (9) occupancy rate;(27) (10) staff hours per resident per day for registered nurses, licensed practical nurses, and nurse aides;(28) and (11) hospital referral region-level nursing home market concentration, as measured by the HHI.
We obtained information on 7 publicly reported nursing home quality measures from the Nursing Home Compare website, which each were available for at least 95% of patients in the study sample; missing values for these items were handled via mean imputation. Data was linked to the study dataset for the quarter corresponding to each patient’s hospital discharge; measures assessed related to the percent of long-stay residents whose need for help with ADLs has increased; who spend most of their time in bed or in a chair; who have/had a catheter inserted and left in their bladder; who have depressive symptoms; who self-report moderate to severe pain; who were physically restrained; and who had a urinary tract infection.(29)
For patients who received care at multiple nursing facilities before and after their index hospitalization, or who received care at multiple nursing homes following discharge, we used data on the first nursing home where the patient received treatment after discharge.
Patient covariates
We used MedPAR data to characterize patient age, sex, and race. Hip fracture types were classified as femoral neck, intertrochanteric, subtrochanteric, or multiple locations based on ICD-9-CM diagnosis codes.(12) For each patient, we calculated the Charlson comorbidity index based on ICD-9-CM diagnosis codes from the index hospitalization and all hospitalizations over the preceding 180 days using validated algorithms.(30)
We used data from the last MDS assessment prior to fracture to calculate summary scores for baseline self-performance in activities of daily living (ADLs) and cognitive performance. ADL independence was summarized using the MDS-ADL score of Morris and colleagues.(31) The MDS-ADL score ranges from 0 to 28 and sums scores for MDS assessments of each of seven ADLs seven activities of daily living (locomotion; dressing; personal hygiene; toilet use; transferring; getting in and out of bed; eating) from 0 (“independence”) to 4 (“total dependence”) over a 7 day assessment window.
Pre-fracture cognitive function was characterized using the MDS Cognitive Performance Scale (CPS), which grades cognition on a 7-point scale ranging from “intact” to “very severe impairment.”(32) As with the MDS-ADL score, CPS scores were calculated using data from the last MDS assessment available prior to fracture.
Dependent variables
Within the hospital admission sample, we examined an outcome of death during hospitalization; within the nursing home admission sample, we examined a primary study outcome of new total dependence in locomotion or death within 180 days after hospital discharge. The presence of new total dependence in locomotion was assessed based on the last available MDS assessment within 180 days after discharge. We included death in this outcome since failure to account fully for decedents in analyses of functional outcomes can lead to spurious results due to survivorship bias; as longitudinal studies of functional outcomes that do not account for death (i.e. “complete-case analyses”) can produce misleading results, we did not carry out a comparison of functional outcomes restricted only to survivors.(33, 34) We also examined two secondary outcomes within the nursing home admission sample, namely death within 30 days of hospital discharge and death within 180 days of hospital discharge.
Statistical analysis
Initial analyses characterized the distribution of patient and facility factors and study outcomes in each of the study samples. Within the hospital admission sample, we used logistic regression to measure the association between hospital factors and the odds of in-hospital mortality. Within the nursing home admission sample, we fit separate logistic regression models to measure the association between selected hospital and nursing home factors and each of the outcomes named above while also adjusting for patient characteristics and admission year. Models employed robust standard errors that adjusted for clustering at the level of the hospital.(35, 36) We used the margins command in Stata to obtain marginal effects estimates for all model covariates.
Omega analysis
To measure the relative contribution of hospital versus nursing home factors to outcomes, we used the ω (omega) statistic,(37–39) a ratio which measures the relative contribution of different sets of predictors to the overall variance of a logistic regression model. In the present context, ω is used to compare the variance contributed by hospital factors relative to nursing home factors for each of the three study outcomes based on a logistic regression model that includes covariates corresponding to hospital factors, nursing home factors, and patient factors.
With hospital characteristics in the numerator and nursing home characteristics in the denominator, ω = 2 would mean that hospital characteristics explain twice the variation in the log odds of the outcome predicted by the logistic regression model than do nursing home characteristics; if ω = 1, hospital and nursing home characteristics explain equivalent amounts of variation. For comparison, we also present information on two other ω calculations. For both the hospital admission sample and the nursing home admission sample, we calculated a ω value comparing the contribution of patient versus hospital characteristics for in-hospital mortality (within the hospital admission sample) and for post-discharge outcomes (within the nursing home admission sample). Within the nursing home admission sample, we calculated an ω value to compare the contribution of patient versus nursing home factors to post-discharge outcomes. A detailed description of the ω calculation appears in the Supplemental Digital Content. For each ω calculation, we tested the hypothesis that ω differed from 1 using the 95% confidence interval of Silber, Rosenbaum, and Ross.(37, 38)
Analyses were carried out using SAS version 9.3 (SAS institute, Cary, NC, 2010) and Stata version 14 (StataCorp, College Station, TX, 2015). The Perelman School of Medicine IRB approved this study and waived the requirement for informed consent.
RESULTS
We identified 60,111 Medicare beneficiaries who were treated at a US hospital for an acute hip fracture over the study period and who resided in a nursing facility within the 180 days prior to fracture. We excluded 7,070 patients who were totally dependent in locomotion prior to fracture, 5,359 patients who did not have surgery, and 1,686 patients who were transferred from another hospital. This resulted in a hospital admission sample of 45,996 patients.
We next excluded 1,814 (3.9%) patients who died during hospitalization and 1,401 (3.0%) patients who survived to discharge but did not receive care in a nursing facility within 180 days, yielding a nursing home admission sample of 42,781 patients, 91.7% of whom (39,249 patients) received care at the same nursing facility prior to and following their hospitalization. Within this sample, 3,757 (8.8%) died within 30 days of discharge, 12,126 (28%) died within 180 days of discharge and 20,479 (48%) either died or developed new total dependence in locomotion within 180 days (Figure 1). 14,819 (34.6%) were readmitted to an acute care hospital within 180 days of discharge. Table 1 shows the characteristics of these two samples.
Table 1.
Characteristics of patients included in the hospital admission sample and the nursing home admission samples
| Hospital admission sample, N=45,996 |
Nursing home admission sample, N=42,781 |
|
|---|---|---|
| Patient characteristics | ||
| Gender (%) | ||
| Female | 34,641 (75.3) | 32,551 (76.1) |
| Male | 11,355 (24.7) | 10,230 (23.9) |
| Race (%) | ||
| White | 42,583 (92.6) | 39,581 (92.5) |
| Black | 2,296 (5.0) | 2,147 (5.0) |
| Other | 1,117 (2.4) | 1,053 (2.5) |
| Age category (%) | ||
| <75 | 4,980 (10.8) | 4,673 (10.9) |
| 75–80 | 6,413 (13.9) | 6,044 (14.1) |
| 81–85 | 11,164 (24.3) | 10,480 (24.5) |
| 86–90 | 12,355 (26.9) | 11,476 (26.8) |
| >=91 | 11,084 (24.1) | 10,108 (23.6) |
| Mean Charlson comorbidity score (SD) | 2.55 (2.0) | 2.51 (1.97) |
| Baseline MDS Cognitive Performance Scale score (%) |
||
| 0 (intact) | 4,484 (9.8) | 4,093 (9.6) |
| 1 (borderline intact) | 4,443 (9.7) | 4,116 (9.6) |
| 2 (mild impairment) | 8,181 (17.8) | 7,599 (17.8) |
| 3 (moderate impairment) | 19,671 (42.8) | 18,310 (42.8) |
| 4 (moderate-severe impairment) | 4,552 (9.9) | 4,271 (10.0) |
| 5 (severe impairment) | 4,306 (9.4) | 4,053 (9.5) |
| 6 (very severe impairment) | 359 (0.8) | 339 (0.8) |
| Mean baseline MDS ADL score (SD)a | 11.32 (6.37) | 11.29 (6.38) |
| Fracture location (%) | ||
| Femoral neck | 21,914 (47.6) | 20,366 (47.6) |
| Multiple locations | 1,927 (4.2) | 1,757 (4.1) |
| Intertrochanteric | 20,566 (44.7) | 19,200 (44.9) |
| Subtrochanteric | 1,589 (3.5) | 1,458 (3.4) |
| Year (%) | ||
| 2005 | 6,212 (13.5) | 5,795 (13.6) |
| 2006 | 11,852 (25.8) | 11,021 (25.8) |
| 2007 | 11,248 (24.5) | 10,462 (24.5) |
| 2008 | 11,223 (24.4) | 10,415 (24.3) |
| 2009 | 5,461 (11.9) | 5,088 (11.9) |
| Hospital facility characteristics | ||
| Mean hospital nurse-to-bed ratio (SD) | 1.26 (0.91) | 1.27 (0.93) |
| Mean hospital nurse skill mix (SD) | 0.86 (0.13) | 0.86 (0.13) |
| Mean hospital resident-to-bed ratio (SD) | 0.04 (0.11) | 0.04 (0.11) |
| Mean hospital market concentration, HHI (SD) | 0.17 (0.15) | 0.17 (0.15) |
| Hospital for-profit status (%) | ||
| No | 40,669 (88.4) | 37,841 (88.5) |
| Yes | 5,327 (11.6) | 4,940 (11.6) |
| Hospital size (%) | ||
| Fewer than 200 beds | 16,666 (36.2) | 15,506 (36.3) |
| 200–399 beds | 15,988 (34.8) | 14,893 (34.8) |
| ≥400 beds | 13,342 (29.0) | 12,382 (28.9) |
| Hospital performance indicatorsb (%) | ||
| High volume facility, low historical risk adjusted mortality |
7,696 (16.7) | 7,221 (16.9) |
| High volume facility, low-moderate historical risk adjusted mortality |
9,091 (19.8) | 8,457 (19.8) |
| High volume facility, high-moderate historical risk adjusted mortality |
9,054 (19.7) | 8,424 (19.7) |
| High volume facility, high historical risk adjusted mortality |
7,843 (17.1) | 7,256 (17.0) |
| Low volume facility | 12,312 (26.8) | 11,423 (26.7) |
| Nursing home facility characteristics | ||
| Nursing home ownership (%) | ||
| For-profit | N/A | 28353 (66.4) |
| Non-profit | N/A | 11,616 (27.2) |
| Government | N/A | 2,718 (6.4) |
| Nursing home location in a hospital (%) | ||
| No | N/A | 41,355 (96.7) |
| Yes | N/A | 1,398 (3.3) |
| Nursing home number of full time physician extenders (SD) |
N/A | 0.04 (0.34) |
| Nursing home chain membership (%) | ||
| No | N/A | 20,003 (46.8) |
| Yes | N/A | 22,750 (53.2) |
| Nursing home availability of a full-time director of nursing (%) |
||
| No | N/A | 794 (1.9) |
| Yes | N/A | 41,959 (98.1) |
| Nursing home size (%) | ||
| < 100 beds | N/A | 12,845 (30.0) |
| 100–150 beds | N/A | 16,130 (37.7) |
| >= 150 beds | N/A | 13,806 (32.3) |
| Mean occupancy rate (SD) | N/A | 86.87 (12.16) |
| Mean registered nurse hours per resident day (SD) |
N/A | 0.29 (0.27) |
| Mean licensed practical nurse hours per resident day (SD) |
N/A | 0.77 (0.44) |
| Mean nurse aide hours per resident day (SD) | N/A | 2.13 (0.72) |
| Mean percentage of residents with Medicare as primary payer (SD) |
N/A | 13.11 (9.37) |
| Mean percentage of residents with Medicaid as primary payer (SD) |
N/A | 62.98 (17.79) |
| Mean nursing home market concentration, HHI (SD) |
N/A | 0.03 (0.03) |
| Nursing home performance indicators | ||
| Mean percentage of residents whose need for help with ADLs has increased (SD) |
N/A | 15.86 (6.43) |
| Mean percentage of residents confined to bed (SD) |
N/A | 3.87 (4.57) |
| Mean percentage of residents who have/had a catheter inserted and left in their bladder (SD) |
N/A | 5.59 (3.24) |
| Mean percentage of residents who have depressive symptoms (SD) |
N/A | 14.52 (7.63) |
| Mean percentage of residents who self-report moderate to severe pain (SD) |
N/A | 4.39 (4.03) |
| Mean percentage of residents who were physically restrained (SD) |
N/A | 4.96 (5.76) |
| Mean percentage of residents with a urinary tract infection (SD) |
N/A | 8.99 (4.31) |
Notes
MDS-ADL scales self-performance in seven activities of daily living (locomotion; dressing; personal hygiene; toilet use; transferring; getting in and out of bed; and eating) on a 0–28 scale, with higher values indicating greater degrees of disability.
Hospitals were classified as high vs low volume facilities based on treatment of 50 or more hip fracture cases January 1 and December 31, 2003. High-volume facilities were classified into performance categories based on quartiles of observed-to-expected 30 day mortality ratios for hip fracture cases treated between January 1 and December 31, 2003.
SD: Standard deviation; MDS: Minimum Data Set; ADL: Activities of Daily Living.
Within the hospital admission sample, patients admitted to hospitals in the lowest quartile of historical performance, as measured by observed-to-expected 30 day mortality ratio, had an increased probability of in-hospital death compared to patients in the highest-performing quartile (marginal effect: 0.0078, p=0.019; see Table 2) in adjusted models.
Table 2.
Logistic regression results for death in hospital among patients in the nursing home admission sample (N=42,781); marginal effects shown.
| Death in hospital | ||
|---|---|---|
| dy/dx | P | |
| Patient characteristics | ||
| Sex | ||
| Female (reference) | ||
| Male | 0.0240 | <0.001 |
| Race | ||
| White (reference) | ||
| Black | −0.0096 | 0.001 |
| Other | −0.0100 | 0.028 |
| Age category | ||
| 65–74 (reference) | ||
| 75–80 | 0.0007 | 0.858 |
| 81–85 | 0.0126 | 0.001 |
| 86–90 | 0.0212 | <0.001 |
| ≥91 | 0.0384 | <0.001 |
| Charlson Comorbidity Index score | 0.0044 | <0.001 |
| Baseline MDS Cognitive Performance Scale score | ||
| 0 (intact; reference) | ||
| 1 (borderline intact) | −0.0064 | 0.027 |
| 2 (mild impairment) | −0.0038 | 0.163 |
| 3 (moderate impairment) | −0.0064 | 0.015 |
| 4 (moderate-severe impairment) | −0.0117 | <0.001 |
| 5 (severe impairment) | −0.0121 | <0.001 |
| 6 (very severe impairment) | −0.0160 | 0.022 |
| Baseline MDS-ADL Scorea | 0.0001 | 0.308 |
| Fracture location | ||
| Femoral neck (reference) | ||
| Multiple locations | 0.0093 | 0.042 |
| Intertrochanteric | −0.0009 | 0.619 |
| Subtrochanteric | 0.0113 | 0.03 |
| Admission year | ||
| 2005 (reference) | ||
| 2006 | −0.0034 | 0.217 |
| 2007 | −0.0035 | 0.181 |
| 2008 | −0.0041 | 0.116 |
| 2009 | −0.0068 | 0.018 |
| Hospital facility characteristics | ||
| Nurse to bed ratio | −0.0001 | 0.848 |
| Nurse skill mix | −0.0044 | 0.483 |
| Resident to bed ratio | 0.0146 | 0.083 |
| For-profit status | −0.0031 | 0.209 |
| Hospital market concentration (Herfindahl-Hirschman Index) | 0.0082 | 0.107 |
| Hospital size | ||
| Less than 200 beds | ||
| 200–399 beds | −0.0007 | 0.759 |
| ≥400 beds | −0.0019 | 0.437 |
| Hospital performance indicatorsb | ||
| High volume, low risk adjusted mortality (reference) | ||
| High volume, low-moderate risk adjusted mortality | 0.0035 | 0.267 |
| High volume, high-moderate risk adjusted mortality | 0.0036 | 0.265 |
| High volume, high risk adjusted mortality | 0.0078 | 0.019 |
| Low volume facility | 0.0062 | 0.052 |
Notes: C-statistic: 0.648.
MDS-ADL scales self-performance in seven activities of daily living (locomotion; dressing; personal hygiene; toilet use; transferring; getting in and out of bed; and eating) on a 0–28 scale, with higher values indicating greater degrees of disability.
Hospitals were classified as high vs low volume facilities based on treatment of 50 or more hip fracture cases January 1 and December 31, 2003. High-volume facilities were classified into performance categories based on quartiles of observed-to-expected 30 day mortality ratios for hip fracture cases treated between January 1 and December 31, 2003.
MDS: Minimum Data Set; ADL: Activities of Daily Living.
Within the nursing home admission sample, hospital resident-to-bed ratio and hospital market concentration were associated with differences in our composite outcome of death or new disability in locomotion at 180 days in adjusted models (marginal effect, resident-to-bed ratio: 0.0471, p=0.048; market concentration: −0.0614, P=0.01, Table 3); adjusted 30-day mortality was greater at patients treated at facilities with higher versus lower historical risk-adjusted mortality (marginal effect, highest versus lowest quartile: 0.0105, p=0.030). Other hospital characteristics were not significantly associated with study outcomes.
Table 3.
Adjusted regression results for death at 180 days after discharge (nursing home admission sample, N=42,781); marginal effects shown
| Death within 30 days | Death within 180 days | Death or new locomotion dependence at 180 days |
||||
|---|---|---|---|---|---|---|
| dy/dx | P | dy/dx | P | dy/dx | P | |
| Patient characteristics | ||||||
| Sex | ||||||
| Female (reference) | ||||||
| Male | 0.0581 | <0.001 | 0.1255 | <0.001 | 0.0569 | <0.001 |
| Race | ||||||
| White (reference) | ||||||
| Black | −0.0331 | <0.001 | −0.0418 | <0.001 | 0.0270 | 0.019 |
| Other | −0.0361 | <0.001 | −0.0751 | <0.001 | −0.0333 | 0.051 |
| Age category | ||||||
| 65–74 (reference) | ||||||
| 75–80 | 0.0161 | 0.020 | 0.0466 | <0.001 | 0.0443 | <0.001 |
| 81–85 | 0.0387 | <0.001 | 0.0916 | <0.001 | 0.0868 | <0.001 |
| 86–90 | 0.0585 | <0.001 | 0.1389 | <0.001 | 0.1199 | <0.001 |
| ≥91 | 0.1084 | <0.001 | 0.2271 | <0.001 | 0.1838 | <0.001 |
| Charlson Comorbidity Index score | 0.0055 | <0.001 | 0.0205 | <0.001 | 0.0128 | <0.001 |
| Baseline MDS Cognitive Performance Scale score | ||||||
| 0 (intact; reference) | ||||||
| 1 (borderline intact) | −0.0008 | 0.897 | −0.0043 | 0.688 | 0.0070 | 0.537 |
| 2 (mild impairment) | 0.0144 | 0.018 | 0.0258 | 0.008 | 0.0407 | <0.001 |
| 3 (moderate impairment) | 0.0223 | <0.001 | 0.0437 | <0.001 | 0.0945 | <0.001 |
| 4 (moderate-severe impairment) | 0.0429 | <0.001 | 0.0726 | <0.001 | 0.1653 | <0.001 |
| 5 (severe impairment) | 0.0398 | <0.001 | 0.0815 | <0.001 | 0.2004 | <0.001 |
| 6 (very severe impairment) | 0.0168 | 0.363 | 0.0314 | 0.26 | 0.2727 | <0.001 |
| Baseline MDS-ADL Score | 0.0013 | <0.001 | 0.0038 | <0.001 | 0.0105 | <0.001 |
| Fracture type | ||||||
| Femoral neck (ref) | ||||||
| Multiple locations | 0.0301 | <0.001 | 0.0553 | <0.001 | 0.0684 | <0.001 |
| Intertrochanteric | 0.0047 | 0.078 | 0.0016 | 0.742 | 0.0084 | 0.103 |
| Subtrochanteric | −0.0024 | 0.737 | −0.0047 | 0.694 | 0.0416 | 0.003 |
| Admission year | ||||||
| 2005 (reference) | ||||||
| 2006 | 0.0059 | 0.175 | −0.0083 | 0.245 | −0.0149 | 0.074 |
| 2007 | 0.0042 | 0.343 | −0.0057 | 0.436 | −0.0306 | <0.001 |
| 2008 | 0.0004 | 0.931 | −0.0158 | 0.032 | −0.0460 | <0.001 |
| 2009 | −0.0068 | 0.169 | −0.0404 | <0.001 | −0.0644 | <0.001 |
| Hospital facility characteristics | ||||||
| Nurse to bed ratio | 0.0002 | 0.915 | −0.0016 | 0.442 | −0.0041 | 0.318 |
| Nurse skill mix | 0.0066 | 0.563 | −0.0015 | 0.929 | −0.0348 | 0.147 |
| Resident to bed ratio | −0.0083 | 0.516 | −0.0152 | 0.492 | 0.0471 | 0.048 |
| For-profit status | −0.0034 | 0.395 | 0.0020 | 0.788 | 0.0041 | 0.621 |
| Hospital market concentration (HHI) | −0.0129 | 0.293 | −0.0232 | 0.265 | −0.0614 | 0.01 |
| Hospital size | ||||||
| Less than 200 beds | ||||||
| 200–399 beds | −0.0062 | 0.069 | −0.0045 | 0.466 | 0.0005 | 0.949 |
| ≥400 beds | −0.0074 | 0.069 | −0.0049 | 0.484 | 0.0050 | 0.556 |
| Hospital performance indicatorsb | ||||||
| High volume, low risk adjusted mortality (Reference) | ||||||
| High volume, low-moderate risk adjusted mortality | 0.0020 | 0.644 | −0.0043 | 0.553 | 0.0058 | 0.492 |
| High volume, high-moderate risk adjusted mortality | 0.0083 | 0.064 | 0.0022 | 0.774 | −0.0052 | 0.532 |
| High volume, high risk adjusted mortality | 0.0104 | 0.030 | 0.0098 | 0.199 | 0.0129 | 0.154 |
| Low volume facility | 0.0018 | 0.690 | 0.0038 | 0.612 | 0.0065 | 0.466 |
| Nursing home facility characteristics | ||||||
| Ownership | ||||||
| For-profit (Reference) | ||||||
| Non-profit | −0.0029 | 0.366 | −0.0061 | 0.288 | 0.0019 | 0.767 |
| Government | −0.0054 | 0.326 | −0.0152 | 0.113 | −0.0096 | 0.422 |
| Based in a hospital | −0.0137 | 0.044 | −0.0316 | 0.013 | 0.0102 | 0.519 |
| Number of full time physician extenders | 0.0064 | 0.149 | 0.0008 | 0.913 | 0.0148 | 0.041 |
| Ownership by a multi-facility organization | 0.0012 | 0.671 | 0.0021 | 0.669 | −0.0304 | <0.001 |
| Full-time nursing director | 0.0059 | 0.484 | 0.0339 | 0.019 | 0.0505 | 0.007 |
| Nursing home size | ||||||
| Less than 100 beds | ||||||
| 100–149 beds | 0.0015 | 0.639 | 0.0103 | 0.078 | 0.0137 | 0.038 |
| ≥ 150 beds | 0.0011 | 0.762 | 0.0169 | 0.007 | 0.0334 | <0.001 |
| Occupancy rate | −0.0001 | 0.264 | −0.0005 | 0.007 | −0.0006 | 0.016 |
| Registered nurse hours per resident day | 0.0014 | 0.748 | −0.0108 | 0.239 | −0.0007 | 0.953 |
| Licensed practical nurse hours per resident day | −0.0003 | 0.928 | 0.0067 | 0.150 | 0.0061 | 0.341 |
| Nurse aide hours per resident day | −0.0005 | 0.779 | −0.0065 | 0.034 | 0.0011 | 0.782 |
| Percentage of residents with Medicare as primary payer | −0.00003 | 0.854 | 0.0005 | 0.101 | 0.0004 | 0.203 |
| Percentage of residents with Medicaid as primary payer | −0.0001 | 0.538 | −0.0002 | 0.271 | 0.0004 | 0.053 |
| Nursing home market concentration (HHI) | 0.1153 | 0.033 | 0.0825 | 0.425 | 0.0216 | 0.858 |
| Nursing home performance indicators | ||||||
| Percent of Residents Whose Need for Help with Activities of Daily Living Has Increased |
0.0002 | 0.345 | 0.0004 | 0.302 | 0.0017 | <0.001 |
| Percent of Residents Who Were Confined to Bed | −0.0002 | 0.532 | 0.0001 | 0.801 | 0.0025 | <0.001 |
| Percent of Residents Who Have/Had a Catheter Inserted and Left in Their Bladder |
0.0008 | 0.048 | −0.0005 | 0.504 | −0.0027 | 0.001 |
| Percent of Residents Who Have Depressive Symptoms | 0.0006 | 0.001 | 0.0005 | 0.111 | −0.0026 | <0.001 |
| Percent of Residents who Self-Report Moderate to Severe Pain | −0.0002 | 0.492 | −0.0008 | 0.183 | −0.0016 | 0.014 |
| Percent of Residents Who Were Physically Restrained | −0.0007 | 0.003 | −0.0004 | 0.343 | −0.0010 | 0.036 |
| Percent of Residents with a Urinary Tract Infection | −0.0003 | 0.418 | 0.0001 | 0.873 | −0.0002 | 0.755 |
Notes: C-statistics: 0.655 (30-day mortality); 0.635 (180-daymortality); 0.641 (180-day composite outcome)
MDS-ADL scales self-performance in seven activities of daily living (locomotion; dressing; personal hygiene; toilet use; transferring; getting in and out of bed; and eating) on a 0–28 scale, with higher values indicating greater degrees of disability.
Hospitals were classified as high vs low volume facilities based on treatment of 50 or more hip fracture cases January 1 and December 31, 2003. High-volume facilities were classified into performance categories based on quartiles of observed-to-expected 30 day mortality ratios for hip fracture cases treated between January 1 and December 31, 2003.
MDS: Minimum Data Set; ADL: Activities of Daily Living.
Multiple nursing home factors were associated with the study outcomes (Table 3); we observed modest associations between the primary study endpoint and nursing home chain ownership (marginal effect: −0.0304, P <0.001); presence of a full-time director of nursing (marginal effect: 0.0505, P=0.007) and treatment in a nursing home with 150 beds or more versus a facility with fewer than 100 beds (marginal effect: 0.0334, P<0.001). All nursing home performance indicators demonstrated associations of small magnitude with the composite outcome, though the direction of these effects varied across measures. Hospital location (marginal effect: −0.0316, P=0.013) and presence of a full-time director of nursing (marginal effect: 0.0339, P=0.019) were each associated with modest differences in 180-day mortality; nursing home market concentration was modestly associated with 30-day mortality (marginal effect: 0.1143, P=0.033).
In omega analyses, patient factors contributed substantially more than either nursing home or hospital factors to the overall variance in all study outcomes (Table 4). Compared to nursing home factors, however, hospital factors accounted for a substantially lower amount of the overall variation observed in the odds of either of the post-discharge outcomes. Within the nursing home admission sample, the omega value comparing the contribution of hospital to nursing home factors to the variation in the odds of new total dependence in locomotion or death was 0.12 (95% CI 0.05, 0.31). For 30 day mortality, this value was 0.32 (95% CI 0.11, 0.96); for 180 day mortality, it was 0.15 (95% CI 0.04, 0.61).
Table 4.
Omega analysis: relative contribution of patient, hospital, and nursing home factors to study outcomes
| Hospital Admission Sample (N = 45,996) |
Nursing Home Admission Sample (N= 42,781) | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome: Death during hospitalizationa |
Outcome: Death at 30 daysb |
Outcome: Death at 180 daysb | Outcome: Death or new total dependence in locomotion at 180 daysb |
|||||
| Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | |
| Patient factors vs. hospital factors |
26.63 | 9.84, 72.05 | 53.19 | 19.53, 144.86 | 183.00 | 47.71, 701.96 | 92.88 | 37.53, 229.85 |
| Patient factors vs. nursing home factors |
N/A | 17.07 | 9.51, 30.64 | 27.86 | 17.00, 45.67 | 10.99 | 8.40, 14.38 | |
| Hospital factors vs. nursing home factors |
N/A | 0.32 | 0.11, 0.96 | 0.15 | 0.04, 0.61 | 0.12 | 0.05, 0.31 | |
Notes.
Patient factors included in model: age, sex, race, Charlson comorbidity score, pre-fracture ADL self-performance (MDS-ADL score), pre-fracture cognitive impairment (MDS-CPS score), fracture location; hospital factors included in model: observed-to-expected 30-day mortality quartile, nurse to bed ratio, nurse skill mix, resident to bed ratio, for-profit status, hospital market concentration, and hospital size (see Table 2);
Patient factors included in model: age, sex, race, Charlson comorbidity score, pre-fracture ADL self-performance (MDS-ADL score), pre-fracture cognitive impairment (MDS-CPS score), fracture location; hospital factors included in model: observed-to-expected 30-day mortality quartile, nurse to bed ratio, nurse skill mix, resident to bed ratio, for-profit status, hospital market concentration, and hospital size; nursing home factors included in model: ownership type (for-profit, non-profit, government), location in a hospital, number of full time physician extenders on staff, ownership by a multi-facility organization, availability of a full-time RN director of nursing, facility bed count, occupancy rate, staff hours per resident day (registered nurses, licensed practical nurses, nurse aides), percentage of residents with Medicare as primary payer; percentage of residents with Medicaid as primary payer, nursing home market concentration, and facility performance on 7 nursing home compare measures (see Table 3).
DISCUSSION
Among previously ambulatory hip fracture patients who were residing in a nursing home in the 180 days before fracture, 4% died during hospitalization and 93% were discharged alive and received post-acute care in a nursing home. Among the latter group of patients, one-third died within 180 days of discharge and half either died or developed new total dependence in locomotion within 180 days.
While patient characteristics represented the principal determinants of outcomes after hip fracture, selected hospital and post-acute care facility characteristics were associated with short and long-term outcomes. Among those patients discharged alive to a nursing facility, the characteristics of the index hospital explained a substantially smaller part of the variation in outcomes than did the characteristics of the nursing home. Compared to hospital factors, nursing home factors explained over 8 times more variation in a patient’s probability of dying or being newly unable to walk at 180 days; approximately 7 times more variation in a patient’s probability of dying at 180 days; and over 3 times more variation in a patients’ probability of dying at 30 days.
Our analysis identified modest associations between several individual hospital and post-acute care facility factors and clinical outcomes. For several of the hospital and nursing home factors considered here, such as historical hospital risk-adjusted mortality,(17) nursing home size,(26) and nursing home occupancy,(27) observed associations were consistent with past research findings. Nonetheless, our findings of worsened 180-day outcomes at facilities employing more physician extenders and those staffed by a full time director of nursing run counter to prior findings in this area.(22) Further research may investigate whether these paradoxical findings may relate to differences in care processes across facilities that may employ different staffing models, such as those that are and are not exempt from current nurse staffing regulations.(40)
This work should be interpreted in the context of limitations. Our comparison of the contribution of hospital versus nursing home factors to variations in outcomes sample was restricted to patients who survived to hospital discharge. Nonetheless, since the vast majority of deaths in the first 180 days after hip fracture occurred after hospital discharge, our findings offer important insights into the relative contributions of acute care and post-acute care facility factors to hip fracture outcomes overall. Since we restricted our analysis to patients treated in nursing facilities after hospital discharge, our results do not speak to patients treated in other post-acute care settings, such as home health care or acute inpatient rehabilitation.
Since we focused on ambulatory patients, our findings may not be applicable to all hip fracture patients. Our sample included patients with varying durations of residence in nursing facilities in the 180 days prior to fracture, and did not examine specifically whether the associations we identified may have varied across patient groups that differed in terms of the duration of their nursing home residence prior to fracture. Our analyses incorporated a wide range of nursing facility and hospital level variables to characterize institutions in which patients received care, including hospital performance rankings based on previously validated risk-adjusted mortality rates. Nonetheless, it is possible that additional information on processes of care, such as the average time spent by patients in skilled nursing for patients treated at a particular nursing home after fracture, could provide further insight on the relative contribution of hospitals versus nursing homes to outcomes. While our models adjusted for a wide array of patient-level characteristics, including detailed information on pre-fracture functional and cognitive status, patients treated in different facilities may have differed in terms of baseline illness severity in ways not captured in our data, since sicker or healthier patients may be selected into certain nursing facilities or hospitals. As such, our analysis should not be taken to imply causality due our inability to rule out the possibility of residual confounding due to unmeasured differences in patient illness across facilities.
Despite these limitations, our work has important implications for both policy and practice. Policy initiatives such as bundled payments for acute and post-acute care, seek to improve the outcomes and efficiency of medical care by considering the care provided across different settings. Rahman, McHugh, and others have recently demonstrated that, among Medicare patients discharged to a skilled nursing facility for post-acute care, the skilled nursing facility’s rehospitalization rate has greater influence on patients’ risk of rehospitalization than does the discharging hospital.(41) Alongside this work, our quantitative estimates of the relative contribution of care provided within individual settings to functional and survival outcomes can provide input to policy-makers and health care providers to help identify targets for quality improvement and inform strategies and to allocate resources within health systems to maximize the value of care that they provide.
CONCLUSION
Compared to hospital factors, nursing home characteristics explain a larger proportion of the variation in outcomes after hip fracture. Further quantitative and qualitative work may explore the impact of such factors on outcomes for older adults hospitalized for conditions other than hip fracture, as well as the processes within facilities that may help to explain the variations in outcomes observed here.
Supplementary Material
Acknowledgments
Funding: Funding was provided by the National Institute on Aging (K08AG043548, to Dr. Neuman and K24AG047908 to Dr. Werner)
Acknowledgements: None
Footnotes
Disclosures: The authors declare no potential conflicts of interest.
REFERENCES
- 1.Mechanic R. Post-acute care--the next frontier for controlling Medicare spending. N Engl J Med. 2014;370:692–694. doi: 10.1056/NEJMp1315607. [DOI] [PubMed] [Google Scholar]
- 2.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Aff (Millwood) 2013;32:864–872. doi: 10.1377/hlthaff.2012.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sood N, Huckfeldt PJ, Escarce JJ, et al. Medicare's bundled payment pilot for acute and postacute care: analysis and recommendations on where to begin. Health Aff (Millwood) 2011;30:1708–1717. doi: 10.1377/hlthaff.2010.0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55:M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 6.Buntin MB, Colla CH, Deb P, et al. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010;48:776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borkan JM, Quirk M, Sullivan M. Finding meaning after the fall: injury narratives from elderly hip fracture patients. Soc Sci Med. 1991;33:947–957. doi: 10.1016/0277-9536(91)90265-e. [DOI] [PubMed] [Google Scholar]
- 8.Salkeld G, Cameron ID, Cumming RG, et al. Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ. 2000;320:341–346. doi: 10.1136/bmj.320.7231.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neuman MD, Silber JH, Magaziner JS, et al. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med. 2014;174:1273–1280. doi: 10.1001/jamainternmed.2014.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoverman C, Shugarman LR, Saliba D, et al. Use of Postacute Care by Nursing Home Residents Hospitalized for Stroke or Hip Fracture: How Prevalent and to What End? J Am Geriatr Soc. 2008 doi: 10.1111/j.1532-5415.2008.01824.x. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Department of Health and Human Services Center for Medicare and Medicaid Services. Data.Medicare.gov: Nursing Home Compare Datasets. [Accessed September 2, 2016];2016 Available at: https://data.medicare.gov/data/nursing-home-compare.
- 12.Elkassabany NM, Passarella MA, Mehta S, et al. Journal of the American Geriatrics Society. 2016. Hospital characteristics, inpatient processes of care, and readmissions among older adults with hip fractures. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fisher ES, Whaley FS, Krushat WM, et al. The accuracy of Medicare's hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992;82:243–248. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spetz J, Donaldson N, Aydin C, et al. How many nurses per patient? Measurements of nurse staffing in health services research. Health Serv Res. 2008;43:1674–1692. doi: 10.1111/j.1475-6773.2008.00850.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silber JH, Rosenbaum PR, Romano PS, et al. Hospital teaching intensity, patient race, and surgical outcomes. Arch Surg. 2009;144:113–120. doi: 10.1001/archsurg.2008.569. discussion 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirschman AO. The Paternity of an Index. American Economic Review. 1964;54:761–762. [Google Scholar]
- 17.Neuman MD, Passarella MA, Werner RM. Healthcare: the Journal of Delivery Science and Innovation. 2016. The relationship between historical risk-adjusted 30-day mortality and subsequent hip fracture outcomes: retrospective cohort study. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dimick JB, Staiger DO, Birkmeyer JD. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res. 2010;45:1614–1629. doi: 10.1111/j.1475-6773.2010.01158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harrington C, Olney B, Carrillo H, et al. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Serv Res. 2012;47:106–128. doi: 10.1111/j.1475-6773.2011.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrington C, Woolhandler S, Mullan J, et al. Does investor ownership of nursing homes compromise the quality of care? Am J Public Health. 2001;91:1452–1455. doi: 10.2105/ajph.91.9.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harrington C, Mullan JT, Carrillo H. State nursing home enforcement systems. J Health Polit Policy Law. 2004;29:43–73. doi: 10.1215/03616878-29-1-43. [DOI] [PubMed] [Google Scholar]
- 22.Bostick JE, Rantz MJ, Flesner MK, et al. Systematic review of studies of staffing and quality in nursing homes. J Am Med Dir Assoc. 2006;7:366–376. doi: 10.1016/j.jamda.2006.01.024. [DOI] [PubMed] [Google Scholar]
- 23.Kim H, Harrington C, Greene WH. Registered nurse staffing mix and quality of care in nursing homes: a longitudinal analysis. Gerontologist. 2009;49:81–90. doi: 10.1093/geront/gnp014. [DOI] [PubMed] [Google Scholar]
- 24.Kim H, Kovner C, Harrington C, et al. A panel data analysis of the relationships of nursing home staffing levels and standards to regulatory deficiencies. J Gerontol B Psychol Sci Soc Sci. 2009;64:269–278. doi: 10.1093/geronb/gbn019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rantz MJ, Hicks L, Grando V, et al. Nursing home quality, cost, staffing, and staff mix. Gerontologist. 2004;44:24–38. doi: 10.1093/geront/44.1.24. [DOI] [PubMed] [Google Scholar]
- 26.Harrington C, Zimmerman D, Karon SL, et al. Nursing home staffing and its relationship to deficiencies. J Gerontol B Psychol Sci Soc Sci. 2000;55:S278–S287. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- 27.Castle NG, Liu D, Engberg J. The association of Nursing Home Compare quality measures with market competition and occupancy rates. J Healthc Qual. 2008;30:4–14. doi: 10.1111/j.1945-1474.2008.tb01129.x. [DOI] [PubMed] [Google Scholar]
- 28.Park J, Stearns SC. Effects of state minimum staffing standards on nursing home staffing and quality of care. Health Serv Res. 2009;44:56–78. doi: 10.1111/j.1475-6773.2008.00906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.U.S. Centers for Medicare and Medicaid Services. Baltimore, MD: U.S. Center for Medicare and Medicaid Services; 2016. Design for Nursing Home Compare Five-Star Quality Rating System: Technical User's Guide. [Google Scholar]
- 30.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 31.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54:M546–M553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 32.Morris JN, Fries BE, Mehr DR, et al. MDS Cognitive Performance Scale. J Gerontol. 1994;49:M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 33.Diehr P, Johnson LL, Patrick DL, et al. Methods for incorporating death into health-related variables in longitudinal studies. J Clin Epidemiol. 2005;58:1115–1124. doi: 10.1016/j.jclinepi.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 34.Diehr P, Patrick DL. Trajectories of health for older adults over time: accounting fully for death. Ann Intern Med. 2003;139:416–420. doi: 10.7326/0003-4819-139-5_part_2-200309021-00007. [DOI] [PubMed] [Google Scholar]
- 35.White H. A Heteroskedasticity-Consistent Covariance-Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica. 1980;48:817–838. [Google Scholar]
- 36.Moulton BR. An Illustration of a Pitfall in Estimating the Effects of Aggregate Variables on Micro Units. Review of Economics and Statistics. 1990;72:334–338. [Google Scholar]
- 37.Silber JH, Rosenbaum PR, Ross RN. Comparing the Contributions of Groups of Predictors - Which Outcomes Vary with Hospital Rather Than Patient Characteristics. Journal of the American Statistical Association. 1995;90:7–18. [Google Scholar]
- 38.Polsky D, Armstrong KA, Randall TC, et al. Variation in chemotherapy utilization in ovarian cancer: the relative contribution of geography. Health Serv Res. 2006;41:2201–2218. doi: 10.1111/j.1475-6773.2006.00596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown SE, Ratcliffe SJ, Halpern SD. An empirical comparison of key statistical attributes among potential ICU quality indicators. Crit Care Med. 2014;42:1821–1831. doi: 10.1097/CCM.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.U.S. Department of Health and Human Services Center for Medicare and Medicaid Services. State Operations Manual, Appendix PP - Guidance to Surveyors for, Long Term Care Facilities. [Accessed September, 2, 2016];2016 Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_pp_guidelines_ltcf.pdf. 2016.
- 41.Rahman M, McHugh J, Gozalo PL, et al. The Contribution of Skilled Nursing Facilities to Hospitals' Readmission Rate. Health Serv Res. 2016 doi: 10.1111/1475-6773.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.