Abstract
Background
Care quality continues to be a focal point within US health care. One quality innovation is the Magnet recognition program for hospitals, which is a nurse-driven initiative emphasizing care and patient safety improvements. To date, Magnet hospitals have been associated with better outcomes, but their distribution is highly uneven. Relatedly, little research has characterized what factors drive Magnet adoption (e.g., competitive pressure from other hospitals).
Objective
To examine if hospitals respond to more competing hospitals becoming Magnets by also becoming Magnet institutions.
Research Design
We use longitudinal data from the American Hospital Association, 1997 – 2012, and estimate hospital-level fixed effect regressions to capture the association between Magnet adoption among competitors and a hospital’s own likelihood of becoming a Magnet. We also explore heterogeneity in the relationships according to a hospital’s standing within its market.
Results
Having more competitors become Magnets strongly predicts that a given hospital seeks Magnet recognition; yet, a hospital’s market position and prevailing competition levels are moderating influences.
Conclusions
A large literature links Magnet hospitals with better outcomes for patients and nurses, and more recent evidence suggests a business case for becoming a Magnet. We find evidence that hospitals appear motivated by competitive pressure, which suggests economic considerations in the decision to invest in costly care improvements.
Keywords: Magnet hospital recognition, hospital competition, nursing workforce, health care quality
Introduction
Care quality continues to be a focal point within the US health care system in an effort to deliver high value services while simultaneously containing costs.1 Advancements in this area include new financial incentives for providers as well as innovative models for care delivery. An example of a quality-driven initiative with a long history, but recently growing popularity, is Magnet hospital recognition. The Magnet hospital concept emerged in the 1980s when it became evident that some hospitals had “magnet-like” properties enabling them to better recruit and retain nurses and deliver superior patient care.2,3. In 1994, the American Nurse Credentialing Center (ANCC) formally established the Magnet Recognition Program as a nurse-driven initiative emphasizing care quality and patient safety improvements.4 More than 400 hospitals have achieved Magnet recognition across the US,4 and importantly, Magnet recognition has been associated with positive care delivery outcomes – such as lower mortality rates and higher patient satisfaction.5–13
For these reasons, hospitals could presumably use Magnet recognition as a signal of quality when competing within two related markets: the market for nursing staff and the market for patients. Prior work shows that inter-organizational competition can drive health care innovation diffusion, which is partly attributable to the desire for attracting new business and staff.14 But pursuing and obtaining Magnet recognition is not a costless activity. Hospitals may have to undertake significant investments to meet Magnet standards and also accept a recurring renewal fee and review process after receiving their initial recognition.15 The related direct costs for a typical 500-bed hospital can range between $46,000 and $251,000.16 Jayawardhana and colleagues (2014) recently argued in favor of a “business case” for Magnet adoption;17 however, such a case is likely to be weaker or stronger depending on local factors – but this remains virtually unexplored. In fact, limited empirical work has tried to characterize the underlying drivers of Magnet adoption, despite the long interest in Magnet recognition’s effects on clinical quality. This is a nontrivial gap in the literature since the growth in Magnets across the US has been uneven, with certain areas having far greater Magnet penetration than others.
One potential reason for widely varying adoption rates is competitive pressure. In other contexts, competing health care organizations are known to more readily embrace service innovation and new technologies, such as advanced imaging equipment and invasive procedures for cardiac care,18,19 via a “medical arms race”. If Magnet recognition is perceived to confer an edge in attracting patients and/or clinical staff, market conditions could shape the willingness to invest in the quality signal. Specifically, as a hospital faces more competing Magnets (i.e., more rival hospitals that have achieved Magnet recognition), it may find the pursuit of its own Magnet recognition more compelling. However, local market characteristics vary, so it is also possible that Magnet uptake differs across markets as well as across hospitals within the same market (e.g., those with and without existing market power). These theoretical possibilities motivate our empirics.
Our aim is to then explore one factor (i.e., competitive pressure) that may influence Magnet adoption and be partly responsible for some of the disparate take-up of Magnet recognition across the US. We first construct measures of Magnet competition from the perspective of an individual hospital and then estimate the relationship between the degree of Magnet competition and a given hospital’s likelihood of becoming a Magnet over time. We also perform sub-analyses to assess how a hospital’s existing position within its market moderates any competitive influence. While our results are descriptive in nature, they are a novel contribution that lends itself to a conceptually consistent interpretation. If competitive pressures do matter, then our findings have implications for how we think about the selection into Magnet and the importance of economic factors in the decision to pursue activities geared toward improving population health and health system performance.
Methods
We used the annual surveys from the American Hospital Association (AHA) spanning 1997 – 2012. We restricted to hospitals that provide adult acute-care services and that were not federal facilities – 5,191 unique hospitals, with 85% of the hospitals present for the full 16 years. As our study was longitudinal in nature, we dropped hospitals that were only present for three waves or less (0.8% of the data) due to their limited analytic information. We relied on a binary variable for Magnet recognition as our hospital-level outcome of interest throughout our analyses.
We then required a measure of local Magnet competition from the perspective of an individual hospital that reflected the degree of Magnet adoption among the hospital’s competitors. Common to the hospital literature, we treated the Hospital Referral Region (HRR) as a hospital’s geographic market. HRRs are provided by the Dartmouth Atlas and are derived from utilization patterns belonging to Medicare beneficiaries. Importantly, we first grouped affiliated hospitals in the same HRR into a single entity so that they were counted as one system (or entity). For example, an HRR with 10 individual hospitals – three of which share the same owner – would be classified as having 7 unique entities in the market. The number of competitors facing any single entity in this market would be 6 (i.e., the total number of hospital entities – accounting for horizontal integration – minus the individual entity). This procedure improved upon simple counts of hospitals as it better reflected the actual market structure and strategic considerations facing local market participants. Moreover, in related work,20 we have shown considerable Magnet adoption behavior within individual health care systems – including affiliates located in the same market – which we did not want to conflate with adoption responses to competitor (i.e., non-affiliate) behavior. We created a total count of competitors for every HRR by year. We did likewise for the total number of Magnet hospitals in a given market and year – again treating integrated hospitals as a single entity. In this way, the summation of Magnets in a local market-year captured the number of competitors with at least one Magnet in the system, with non-integrated (i.e., standalone) hospitals counting as their own system. We then divided the total number of Magnet hospital competitors by the total number of competitors to recover the fraction of competitors that had received Magnet recognition in a given market-year, or said differently, to capture the degree of Magnet penetration among competing hospitals. This fraction (or degree of Magnet penetration) operated as our key measure of competitive pressure on a hospital to invest in achieving Magnet recognition. Of note, in sensitivity analyses, we employed progressively more restrictive definitions of Magnet recognition for hospital systems (i.e., requiring higher fractions of local system affiliates to hold Magnet recognition to then classify the system as a Magnet competitor). As seen in Appendix Tables 4 – 6, our analytic choices for the main analyses appear conservative.
To capture the degree of competition prevailing in the market, we constructed a standard Herfindahl-Hirschman Index (HHI) using hospital size (i.e., total beds). We again accounted for horizontal integration so that affiliated hospitals within the same market had their bed quantities summed together into a composite total. We used standard Department of Justice definitions of market concentration and considered markets with HHI values between 1500 and 2500 to be moderately concentrated and those with values greater than 2500 to be very concentrated markets. We also created a “market leader” indicator variable equal to one when a given hospital’s (or entity in the case of locally integrated hospitals) share of beds was greater than or equal to 25% of all beds in the market. We then constructed a simple set of time-varying hospital characteristic covariates. We first categorized the teaching level of a given hospital by the ratio of FTE post-graduate residents/fellows to patient beds. Hospitals with a ratio above zero but less than or equal to 0.25 received a binary indicator equal to one for “minor” teaching status. Hospitals with a ratio above 0.25 received a one for a separate, “major” teaching status categorical variable. We then used binary indicators for non-profit ownership status and being a hospital with advanced treatment technology. The latter is equal to one when a hospital reports having the capability to perform open-heart surgery, organ transplantation, or both.
Statistical Analyses
Our regression analyses exploited the multiyear panel to conduct longitudinal analyses with hospital fixed effects (FE). In this way, we specifically captured within-hospital changes in Magnet recognition over time. The key right-hand side variable of interest was our measure of Magnet adoption among a hospital’s local competitors – as previously described. The primary linear estimating equation for each hospital ‘i’ at time ‘t’ was:
The linear model was also well-suited for FE estimation and preferred for comparing coefficients across models as well as direct interpretations of interaction coefficients.21–23 The equation included hospital-level time-varying characteristics (X), a vector of year dummies (τ), and individual hospitals fixed effects (η). The ‘CompAdopt’ variable captures the time-varying Magnet adoption behavior of local competitors. Appendix Table 1 summarizes the Magnet penetration variable for the analytic sample. The distribution is non-normal, with a long right tail. Thus, we did not rely on the continuous measure but instead used an indicator variable equal to one when 10% or more of a hospital’s competitors were Magnets in a given year (roughly the top quintile of Magnet penetration within a market). In sensitivity analyses, we lowered the indicator variable threshold to ensure that the pattern of results was not overly influenced by the chosen cutoff. Of note, while the measures of Magnet competition in the market incorporate hospital system affiliations, the estimating equation – and hence included covariates and outcome measure – are at the individual hospital level (i.e., not aggregated into a larger entity).
We implemented our primary regression model in a stepwise fashion. First, we showed the bivariate relationship between Magnet competition and a hospital’s likelihood of becoming a Magnet in a given year. Then, we introduced our set of year indicators, followed by our set of covariates for local HHI, individual hospital characteristics, and number of competitors in the market. The latter variable ensured that our key variation was driven by Magnet adoption by competitors, rather than fluctuations in the number of competitors in a given HRR. Appendix Figure 1 shows the substantial increase in the total number of Magnets during our study period. Our final specification incorporated 1- and 2-year lags and leads of the Magnet competition measure to more flexibly reflect the multiyear process in achieving Magnet recognition (i.e., a lagged response to competing with new Magnets) as well as the role of forecasting in hospital’s strategic decisions – for example, if a hospital observed a competitor undergoing the Magnet recognition process.
In a second set of analyses, we allowed for an interactive relationship between the degree of Magnet competition and a hospital’s position as a “market leader” – as defined above. Hospitals with a more dominant position in their local market may have behaved differently than those at a competitive disadvantage, so we wished to reflect this possible heterogeneity across hospitals within a market. The regression model and variables were identical to those used in the prior specifications, with the exception that we included a “market leader” dummy variable (‘Leader’), along with its Magnet competition interaction (‘Comp × Lead’).
We also re-ran the model for subsets of the analytic sample – stratified by the level of competition in the market (HRR) at baseline (i.e., the 1997 data wave) – to explore potential variation across market structures.
We concluded our empirics with a supplementary analysis to check for logical consistency. This final analytic exercise closely followed the prior setup; however, instead of focusing on the degree of Magnet competition facing a given hospital, we turned our attention to a decrease in local competition (i.e., a “shock” to the market due to exit by one or more local competitors since the prior survey year). If having more competitors as Magnets encourages hospitals to seek Magnet recognition via market forces (i.e., a “medical arms race”), then a reduction in prevailing competition should lower the incentive to undertake recognition (i.e., the associations should run in the opposite directions). To implement this analysis, we generated a binary (market “shock”) variable equal to one if a hospital’s number of competitors decreased relative to the preceding year. While the data did not detail the reason for a given hospital’s exit from the market, comparing changes seen in the AHA data for the state of Pennsylvania (PA) with public reports on PA hospital closures and mergers revealed that nearly all observed “exits” in the data fell into one of these two groups (roughly an even split between mergers and closures) – rather than missing data or bad reporting. Despite not being able to separate out closures from mergers, both phenomena affect local competition in the same direction (i.e., reduce the number of hospitals with which the reference hospital must compete), which was sufficient for our purposes. All other covariates remained the same – except for the number of competitors, which was removed from this portion of our analyses. We also paralleled the above analytic structure by including additional specifications with “market leader” interactions as well as subsample estimations according to market structure. We used robust standard errors in all regression models since our outcome variable (Magnet recognition) was binary.
Results
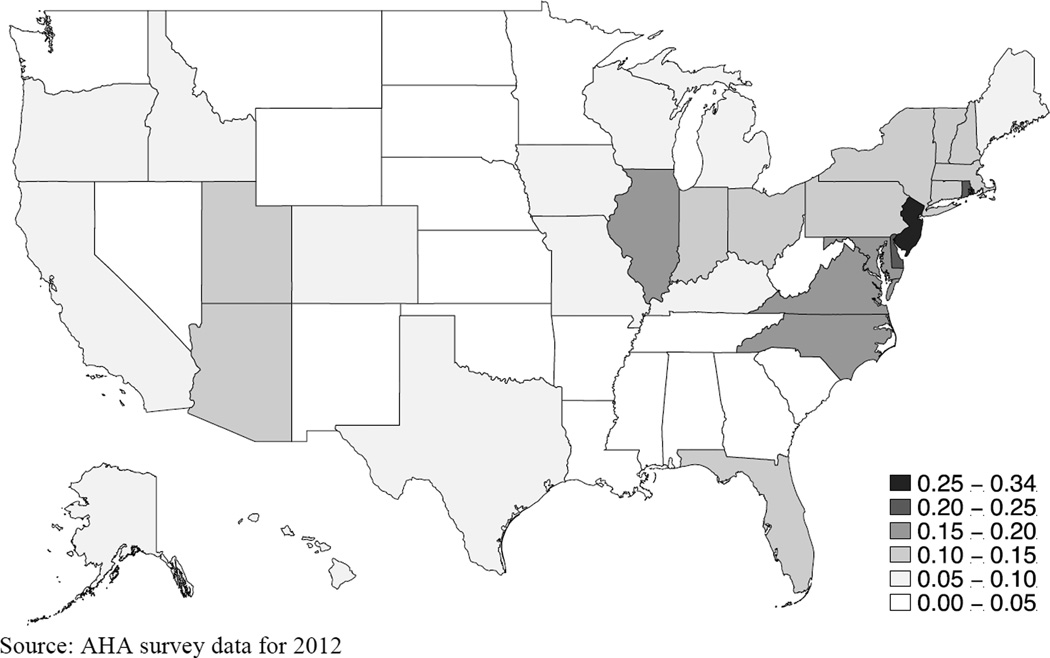
While the increase in Magnets is nearly linear from 2002 onward (see Appendix Figure 1), the geographic distribution of Magnets in 2012 is uneven – as evident in Figure 1, which displays the fraction of all hospitals within a state that are Magnets. States with smaller geographies (and potentially closer hospital proximity) often have the highest concentration of Magnets – e.g., Delaware, Maryland, and Rhode Island – with New Jersey as the leading state with roughly a third of all hospitals classified as Magnets in 2012. Although multiple factors could account for the Magnet dispersion patterns seen in Figure 1, the concentration of Magnets is at least consistent with a role for competitive pressure. Appendix Figure 2 shows the absolute number of Magnets by state.
Figure 1.
Fraction of All Hospitals Within a State That Are Magnets in 2012
Source: AHA survey data for 2012
We summarize our analytic sample across all years (1997 – 2012) in Table 1. The majority of hospitals are non-teaching and not-for-profit, and the average market size is just under 20 hospitals. A typical hospital market in our data is also moderately concentrated according to Department of Justice definitions, and finally 6.6% of our sample achieves Magnet recognition.
Table 1.
Summary Statistics for Analytic Sample of US Hospitals 1997 – 2012
| Become Magnet Hospitals | 6.6% |
|---|---|
| Baseline Characteristics | |
| Major or Minor Teaching Hospital | 24.5% |
| Not-for-Profit Hospital | 84.3% |
| Advanced Tech Hospital | 0.03% |
| No. Competing Hospitals within HRR | 18.5 |
| HHI within HRR | 1694.9 |
Source: AHA data from 1997 to 2012 (5191 unique hospitals)
Baseline characteristics summarize features of our included hospitals and their local markets during their initial survey wave (i.e., the first time they are present in the data)
HRR stands for Dartmouth constructed Hospital Referral Region
HHI stands for Herfindahl-Hirschman Index for market concentration
Table 2 presents our core results from the hospital fixed effects regression models. The specification for column 1 is the simple bivariate correlation. The estimate suggests that as more competitors become Magnets, a hospital is more likely to invest in its own Magnet recognition. The magnitude of the coefficient is expectedly reduced once we include the set of year dummies (since the growth in Magnets has increased over time); however, the estimate remains stable in columns 2 – 5, despite the introduction of additional time-varying control variables. The coefficients across these four columns imply that having 10% or more competitors becoming Magnets is associated with a 2-percentage point increase in the probability of a hospital becoming a Magnet itself. The estimates are all highly significant. Column 6 in Table 2 captures some of the dynamic process involved in a hospital’s strategic response to others’ Magnet adoption. The strongest correlations are in the contemporaneous year and the immediately preceding year. The estimates are weaker and less precise when moving farther from the current year. There is also some suggestive evidence of hospital forecasting in column 6, whereby having more competing Magnets in the future year (“t + 1”) positively predicts a hospital becoming a Magnet in the current year. Appendix Table 2 displays the coefficients for the other covariates, and Appendix Table 3 re-estimates all specifications from Table 2 with a lower threshold for the Magnet competition indicator (i.e., 5% instead of 10% market penetration). The pattern of results is identical, with only the correlation magnitudes reduced. This is unsurprising since the alternative cutoff represents a weaker change in the degree of Magnet competition.
Table 2.
Association Between Magnet Recognition and Competing Hospitals’ Degree of Magnet Adoption
| Hospital Fixed Effects | ||||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Mag Density (t+2) | -- | -- | -- | -- | -- | 0.003 (0.003) |
| Mag Density (t+1) | -- | -- | -- | -- | -- | 0.005* (0.003) |
| At Least 10% Magnet Density Among Competitors (t) |
0.063*** (0.005) |
0.024*** (0.005) |
0.024*** (0.005) |
0.023*** (0.005) |
0.022*** (0.005) |
0.010*** (0.004) |
| Mag Density (t−1) | -- | -- | -- | -- | -- | 0.008*** (0.003) |
| Mag Density (t−2) | -- | -- | -- | -- | -- | 0.005 (0.005) |
| Covariates | ||||||
| Year Dummies | Yes | Yes | Yes | Yes | Yes | |
| HHI | Yes | Yes | Yes | Yes | ||
| Hospital Char. | Yes | Yes | Yes | |||
| No. Competitors | Yes | Yes | ||||
| Observations | 5191 | 5191 | 5191 | 5191 | 5191 | 5113 |
P value at 0.01
P value at 0.05
P value at 0.10, Huber-White robust standard errors
Magnet recognition is a binary outcome equal to ‘1’ when a given hospital is a Magnet in a given year
All models are “within-in” estimators (hospital-level fixed effects)
At Least 10% Magnet Density Among Competitors is a binary indicator variable, column 6 includes two leads and two lags of this variable
Table 3 introduces our interactive models between Magnet competition and a hospital’s status as a local market leader. The positive correlation remains in this modified specification (column 1, Table 3), but we can see the strongest association is concentrated among the more dominant hospitals (in terms of size and relative to their local market conditions). The differential behavior of market leaders holds when the number of competitors is modest to small (column 2) but is not evident when the number of competitors is larger (column 3). An interpretation consistent with columns 1 and 2 (Table 3) is that dominant hospitals wish to maintain their market advantage by also acquiring the quality signal (i.e., Magnet recognition) – so long as the signal is clearly visible in the market. Stratifying the sample by HHI levels (columns 4 – 6 in Table 3) offers some interesting patterns as well. The market leader interaction coefficient remains positive, substantive, and statistically significant across all models; however, the behavior of non-market leaders (i.e., relatively smaller hospitals) diverges based on market structure. In competitive markets (column 6), these hospitals are more likely to invest in Magnet adoption as they face more competition from other Magnets, but the opposite is found in very concentrated markets (column 4). Smaller hospitals competing with other powerful institutions are much less likely to seek Magnet recognition when more of their competitors become Magnets – perhaps because any eventual payoff is perceived to be too low to justify the costs of recognition.
Table 3.
Association Between Magnet Recognition and Competing Hospitals’ Degree of Magnet Adoption with an Interaction for Local Market Leader
| Hospital Fixed Effects | ||||||
|---|---|---|---|---|---|---|
| All | 25 or Less Competitors at Baseline |
More Than 25 at Baseline |
HHI Over 2500 at Baseline |
HHI Between 1500 and 2500 at Baseline |
HHI Under 1500 at Baseline |
|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| At Least 10% Magnet Density Among Competitors |
0.011** (0.005) |
0.008 (0.006) |
0.018* (0.010) |
−0.040*** (0.009) |
0.013 (0.010) |
0.026*** (0.008) |
| Market Leader | 0.004 (0.005) |
0.003 (0.005) |
0.003 (0.011) |
−0.013* (0.008) |
0.003 (0.008) |
0.007 (0.007) |
| Mag Density × Market Leader |
0.054*** (0.015) |
0.060*** (0.016) |
0.006 (0.037) |
0.075** (0.035) |
0.049** (0.021) |
0.058** (0.026) |
| Covariates | ||||||
| Year Dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| HHI | Yes | Yes | Yes | Yes | Yes | Yes |
| Hospital Char. | Yes | Yes | Yes | Yes | Yes | Yes |
| No. Competitors | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 5191 | 3708 | 1483 | 835 | 1560 | 2796 |
P value at 0.01
P value at 0.05
P value at 0.10, Huber-White robust standard errors
Magnet recognition is a binary outcome equal to ‘1’ when a given hospital is a Magnet in a given year
All models are “within-in” estimators (hospital-level fixed effects)
At Least 10% Magnet Density Among Competitors is a binary indicator variable
Market Leader is equal to ‘1’ when the local hospital/system has 25% or more of HRR bed capacity in a given year
Table 4 provides an alternative angle on the role of competition and Magnet adoption. Rather than focus on the degree of Magnet competition, we shift our emphasis to changes in the prevailing amount of competition. Looking across columns 1 – 7 (Table 4), we can see a negative ‘shock’ to the level of competition in the market is negatively correlated with the likelihood a hospital invests in becoming a Magnet – especially among smaller hospitals. Market leaders show little or no relationship with lower competition on net since the negative constitutive term (“Shock for Lower Comp”) is generally offset by the positive interaction term. The negative association among non-market leader hospitals also persists across all market structures and is always highly significant (columns 5 – 7, Table 4). The data patterns and intuition belonging to Table 4 are congruent with what is found in Tables 2 and 3. Taken together, the willingness to invest in becoming a Magnet hospital seems responsive to competitive pressure, and in turn, the potential benefits a hospital expects in the market after acquiring the costly quality signal.
Table 4.
Association Between Magnet Recognition and a Market ‘Shock’ Due to Competitor Exit with an Interaction for Local Market Leader
| Hospital Fixed Effects | |||||||
|---|---|---|---|---|---|---|---|
| All | All | 25 or Less Competitors at Baseline |
More Than 25 at Baseline |
HHI Over 2500 at Baseline |
HHI Between 1500 and 2500 at Baseline |
HHI Under 1500 at Baseline |
|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| ‘Shock’ for Lower Comp |
−0.003*** (0.001) |
−0.006*** (0.001) |
−0.009*** (0.002) |
0.0004 (0.002) |
−0.009** (0.005) |
−0.007*** (0.002) |
−0.005*** (0.002) |
| Market Leader | -- | 0.008 (0.005) |
0.008* (0.005) |
0.002 (0.012) |
−0.003 (0.009) |
0.008 (0.008) |
0.010 (0.007) |
| Lower Comp × Market Leader |
-- | 0.010*** (0.003) |
0.011*** (0.004) |
0.010 (0.007) |
0.005 (0.007) |
0.013** (0.006) |
0.011** (0.005) |
| Covariates | |||||||
| Year Dummies | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| HHI | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hospital Char. | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Observations | 5191 | 5191 | 3708 | 1483 | 835 | 1560 | 2796 |
P value at 0.01
P value at 0.05
P value at 0.10, Huber-White robust standard errors
Magnet recognition is a binary outcome equal to ‘1’ when a given hospital is a Magnet in a given year
‘Shock’ for Lower Comp. is a binary variable equal to ‘1’ if the number of competitors facing a given hospital in an HRR has been reduced from the year prior and ‘0’ otherwise
All models are “within-in” estimators (hospital-level fixed effects)
Market Leader is equal to ‘1’ when the local hospital/system has 25% or more of HRR bed capacity in a given year
Discussion
Magnet recognition is a growing, but unevenly distributed, trend among US hospitals. Our findings suggest that the skewed concentration of Magnets could be attributed in part to local market environments and the competitive pressure to become a Magnet. We specifically find that hospitals’ own Magnet recognition is positively associated with more competitors becoming Magnets over time, and a reduction in prevailing market competition seems to discourage Magnet pursuit – at least among smaller hospitals. The former relationship also accords with Abraham and colleagues’ (2011) cross-sectional look at Magnet adoption.26 We also see that investing in Magnet recognition is a strategic process that evolves in response to the dynamic behavior of local competitors, and our results reveal differences in behavior based on a hospital’s standing within its market. Magnet recognition and maintaining Magnet standing constitute significant financial investments for hospitals that must be weighed against the uncertain future financial benefits. Thus, the perceived potential payoff – and hence decision to adopt – may be heavily influenced by a hospital’s current market conditions.
At this time, mounting evidence underscores the quality benefits of being a Magnet hospital, including: better outcomes at lower or similar costs,24 lower mortality,5,6,8,9,11,12 fewer in-hospital falls,7 fewer pressure ulcers,25 and greater patient satisfaction.10,13 Yet, efforts to improve care quality through Magnet adoption may heavily depend on economic factors rather than institutional commitments to clinical quality, which can challenge more widespread Magnet adoption.
Overall, our unique study offers an economic perspective on Magnet adoption behavior across hospital settings. We find suggestive evidence that market forces play an important role in either accelerating or attenuating Magnet adoption. These findings fill an important gap in the literature and have implications for researchers considering the selection process into Magnet as well as policy initiatives aimed a greater diffusion of care quality innovations. However, the analyses may not account for any time-varying omitted variables – though we did test the results’ sensitivity to controlling for changes in the local economic conditions (i.e., the unemployment rate), which had no impact on the estimates (available by request). We also recognize that the decision to pursue Magnet recognition includes balancing various trade-offs and other complex factors, which cannot be fully addressed in our data. Instead, we narrowly focus on how local competitors’ Magnet adoption behavior influences a given hospital’s decision to pursue Magnet recognition.
Policy efforts to promote population health and health system performance will need to be mindful of economic considerations weighing on hospitals’ decisions to pursue this and other quality signals. Expected returns on investments may significantly shape the willingness of a given hospital to participate.
Supplementary Material
Acknowledgments
The authors wish to thank the American Nurses Foundation Nursing Research Grants Program for supporting this research. All views and remaining errors belong solely to the authors.
Footnotes
Author Declaration
The authors have no conflicts of interest to disclose.
Contributor Information
M. Richards, Department of Health Policy, Vanderbilt University, 2525 West End Ave, Suite 1206, Nashville, TN 37203, Phone: 615-875-9642, michael.r.richards@vanderbilt.edu.
K. Lasater, Center for Health Outcomes and Policy Research, School of Nursing, University of Pennsylvania, karenlb@nursing.upenn.edu.
M. McHugh, Center for Health Outcomes and Policy Research, School of Nursing, University of Pennsylvania, Phone: 215-746-0205, mchughm@nursing.upenn.edu.
References
- 1.Burwell SM. Setting value-based payment goals — HHS efforts to improve U.S. health care. New Eng J Med. 2015;372:897–899. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 2.McClure M, Poulin M, Sovie M, et al. Magnet Hospitals: Attraction and Retention of Professional Nurses. Kansas City, MO: American Nurses Association; 1983. [Google Scholar]
- 3.McClure M. Magnet hospitals: Insights and issues. Nurs Adm Q. 2005;29:198–201. doi: 10.1097/00006216-200507000-00003. [DOI] [PubMed] [Google Scholar]
- 4.American Nurses Credentialing Center. Magnet Recognition Program Overview. [Accessed November 2, 2015];2015 Available at: http://www.nursecredentialing.org/Magnet/ProgramOverview. [Google Scholar]
- 5.Aiken LH, Smith HL, Lake ET. Lower Medicare mortality among a set of hospitals known for good nursing care. Med Care. 1994;32:771–787. doi: 10.1097/00005650-199408000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell PH, Shortell SM. Adverse outcomes and variations in organization of care delivery. Med Care. 1997;35:NS19–NS32. doi: 10.1097/00005650-199711001-00003. [DOI] [PubMed] [Google Scholar]
- 7.Lake ET, Shang J, Klaus S, et al. Patient falls: association with hospital magnet status and nursing unit staffing. Res Nurs Health. 2010;33:413–425. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lake ET, Staiger D, Horbar J, et al. Association between hospital recognition for nursing excellence and outcomes of very low-birth-weight infants. JAMA. 2012;307:1709–1716. doi: 10.1001/jama.2012.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McHugh MD, Kelly LA, Smith HL, et al. Lower mortality in magnet hospitals. Med Care. 2013;51:382–388. doi: 10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith SA. Magnet hospitals: higher rates of patient satisfaction. Policy Polit Nurs Pract. 2014;15:30–41. doi: 10.1177/1527154414538102. [DOI] [PubMed] [Google Scholar]
- 11.Friese CR, Xia R, Ghaferi A, et al. Hospitals in 'Magnet' Program show better patient outcomes on mortality measures compared to non-'Magnet' hospitals. Health Aff (Millwood) 2015;34:986–992. doi: 10.1377/hlthaff.2014.0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kutney-Lee A, Stimpfel AW, Sloane DM, et al. Changes in patient and nurse outcomes associated with magnet hospital recognition. Med Care. 2015;53:550–557. doi: 10.1097/MLR.0000000000000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stimpfel AW, Sloane DM, McHugh MD, et al. Hospitals known for nursing excellence associated with better hospital experience for patients. Health Serv Res. 2015 doi: 10.1111/1475-6773.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenhalgh T, Robert G, MacFarlan F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russell J. Journey to magnet: cost vs. benefits. Nurs Econ. 2010;28:340–342. [PubMed] [Google Scholar]
- 16.Drenkard K. The business case for Magnet. J Nurs Adm. 2010;40:263–271. doi: 10.1097/NNA.0b013e3181df0fd6. [DOI] [PubMed] [Google Scholar]
- 17.Jayawardhana J, Welton JM, Lindrooth RC. Is there a business case for magnet hospitals? Estimates of the cost and revenue implications of becoming a magnet. Med Care. 2014;52:400–406. doi: 10.1097/MLR.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 18.Cutler DM, McClellan C. The determinants of technological change in heart attack treatment. National Bureau of Economic Research 1996, Working Paper [Google Scholar]
- 19.Baker LC. Managed care and technology adoption in health care: evidence from magnetic resonance imaging. J Health Econ. 2001;20:395–421. doi: 10.1016/s0167-6296(01)00072-8. [DOI] [PubMed] [Google Scholar]
- 20.Richards MR, Lasater KB, McHugh MD. Organizational momentum and Magnet adoption among integrated hospitals. Unpublished manuscript. [Google Scholar]
- 21.Ai C, Norton EC. Interaction terms in logit and probit models. Economic Letters. 2003;80:123–129. [Google Scholar]
- 22.Mood C. Logistic regression: Why we cannot do what we think we can do, and what we can do about it. Eur Sociol Rev. 2010;26:67–82. [Google Scholar]
- 23.Allison PD. Comparing logit and probit coefficients across groups. Sociol Method Res. 1999;28:186–208. [Google Scholar]
- 24.Silber JH, McHugh MD, Rosenbaum PR, et al. Comparing the value of better nursing work environments across different levels of patient risk. JAMA Surg. 2016 doi: 10.1001/jamasurg.2015.4908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goode CJ, Blegen MA, Park SH, et al. Comparison of patient outcomes in Magnet® and non-Magnet hospitals. J Nurs Adm. 2011;41:517–523. doi: 10.1097/NNA.0b013e3182378b7c. [DOI] [PubMed] [Google Scholar]
- 26.Abraham J, Jerome-D’Emilia D, Begun JW. The diffusion of Magnet hospital recognition. Health Care Manag Rev. 2011;36:306–314. doi: 10.1097/HMR.0b013e318219cd27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.