Abstract
Posttraumatic stress disorder (PTSD) is common and undertreated among Veterans Affairs (VA) primary care patients. A brief primary care intervention combining clinician support with a self-management mobile app (Clinician-Supported PTSD Coach, CS-PTSD Coach) may improve patient outcomes. This study developed and refined an intervention to provide clinician support to facilitate use of the PTSD Coach app and gathered VA provider and patient qualitative and quantitative feedback on CS-PTSD Coach to investigate preliminary acceptability and implementation barriers/facilitators. VA primary care providers and mental health leadership (N = 9) completed a survey and interview regarding implementation barriers and facilitators structured according to the Consolidated Framework for Implementation Research (CFIR). Clinicians who delivered CS-PTSD Coach (N = 3) and patients (N = 9) who received it provided feedback on the intervention and implementation process. CS-PTSD Coach has high provider and patient acceptability. Important implementation factors included that CS-PTSD Coach be compatible with the clinics’ current practices, have low complexity to implement, be perceived to address patient needs, and have strong support from leadership. Diverse factors related to CS-PTSD Coach delivery facilitate implementation, provide an opportunity to problem-solve barriers, and improve integration of the intervention into primary care.
Keywords: PTSD, Primary care, Technology, Implementation science, Acceptability, Veterans
Posttraumatic stress disorder (PTSD) is a common condition among primary care patients. Research conducted in civilian and US Department of Veterans Affairs (VA) primary care clinics found that 11–12 % of patients have PTSD [1, 2] compared to a 3.5 % prevalence found in the general population [3]. For patients who meet criteria for PTSD and utilize primary care services, PTSD is a chronic condition [4] and is associated with significant functional impairment, higher rates of medical utilization, more intense physical symptoms, poorer health functioning, and a higher suicide risk [2, 5, 6].
Effective, evidence-based psychotherapies for PTSD are widely available for veterans [7]. However, multiple barriers can prevent veterans from receiving adequate PTSD treatment, including negative perceptions of services, stigma, and avoidance associated with PTSD symptoms [8–11]. Offering services for PTSD within primary care could increase access to and engagement in to PTSD treatment. VA has implemented the Primary Care-Mental Health Integration (PC-MHI) initiative in which mental health clinicians work within primary care settings providing brief mental health interventions [12]. Although some PTSD treatments for primary care mental health have preliminary support [13–16], and there is ongoing research in this area, none have found support for their efficacy in a full-scale randomized controlled trial.
A promising way to expand the scope and intensity of brief PC-MHI interventions to match the needs of individuals with PTSD is through the use of technology. Smartphones and other portable electronic devices are frequently utilized by civilians [17] and military personnel [18] alike and provide new opportunities to deliver mobile mental healthcare [19]. Incorporating the use of technology may be especially important for individuals with PTSD because they are more likely to choose to live in remote, rural areas to reduce overstimulation, hyperarousal, and interpersonal conflict [20]. Using a mobile app in primary care may be more appealing, convenient, and less stigmatizing than engaging in traditional psychotherapy [21, 22]. In response to the growing interest in using technology to manage PTSD symptoms, VA’s National Center for PTSD and the Department of Defense’s National Center for Telehealth & Technology jointly developed the PTSD Coach mobile app [23]. PTSD Coach is available at no cost for Apple or Android smart devices. This mobile app incorporates evidence-based assessment, psycho-educational, and cognitive-behavioral strategies [24]. Psycho-educational information includes material on what PTSD is, how it develops, related problems, treatment approaches, and when to seek professional help. In the self-management section of the app, users are asked to identify what symptoms they are experiencing, then the app suggests symptom-specific evidence-based strategies such as pleasant events scheduling, functional analysis of traumatic triggers, and coping self-statements. Additionally, PTSD Coach helps users find support through crisis services, professional services, or their own personal support networks. Preliminary research on veterans’ satisfaction with PTSD Coach produced encouraging results; 89 % were moderately to extremely satisfied with it. Specifically, veterans discussed its usefulness in helping to manage distress, aid with sleep problems, and share psycho-educational information with family and friends [24]. Additionally, preliminary evidence provides initial support for possible efficacy at reducing PTSD symptoms and suggests that regular use of the PTSD Coach app is feasible and acceptable in a sample of community trauma survivors [25].
Nonetheless, a growing body of research suggests that self-management programs (i.e., those that involve little to no therapist contact) are often underutilized. One study found that although a large percentage of individuals indicated interest in mobile health (mHealth) options, only a small group reported use of existing PTSD mHealth programs [21]. In fact, analysis of objective use data for another study utilizing PTSD Coach indicates that although app users report positive feedback on usability and positive impact on symptom distress, only 80 % of first-time users reach the home screen and only 37 % progress to one of the primary content areas [26]. Adding support from a healthcare provider can increase use of mHealth programs. Technology-based interventions that include contact and monitoring from a healthcare provider tend to be utilized more often and lead to better outcomes than self-management only interventions [27, 28]. For example, adding peer support to an online psychoeducational program for bipolar disorder increased treatment adherence, led to improved depression symptoms, and decreased functional impairment compared to the online program alone [29]. Given the need for additional primary care services for veterans with PTSD, the demonstrated acceptability of technology-based mental health interventions, and the benefits of adding clinician support to technology interventions, we sought to develop a primary care-based treatment package that adds clinician support to the PTSD Coach mobile app, called Clinician-Supported PTSD Coach (CS-PTSD Coach). This intervention is meant to be used with any primary care patients who are currently struggling with PTSD symptoms. The clinician-support component is designed to be implemented as a brief intervention and intended to provide structure, guidance, and tailoring to encourage app use.
In order to incorporate veteran and provider acceptability in intervention development, we assessed implementation constructs within the development process from the Consolidated Framework for Implementation Research (CFIR). CFIR was selected to guide our implementation efforts because it is a multidimensional model which accounts for both organizational and patient factors. CFIR is comprised of constructs from a variety of implementation frameworks and models supported in the literature [30–33]. CFIR’s five major organizing domains focus on the intervention, the inner and outer setting, the individuals involved, and the process by which implementation is accomplished. Within these five domains is a comprehensive list of 39 constructs that have support for their influence on implementation effectiveness. CFIR has previously been used to guide both evaluation and implementation efforts through identifying factors affecting implementation of specific interventions (e.g., for stroke rehabilitation and weight management) and best practice guidelines [34–36].
As the first step in our line of research to develop and test CS-PTSD Coach, we sought to gather systematic feedback from VA providers and veterans. We wanted to develop a treatment that was responsive to the needs of providers and veterans and could be smoothly implemented into the existing primary care environments. Therefore, we used the CFIR [37] to elicit provider feedback on feasibility and acceptability of implementing CS-PTSD Coach and to tailor an implementation strategy to maximize potential for a successful implementation. We also gathered veteran satisfaction data as part of a pilot implementation of CS-PTSD Coach. The aims of this study were to: (1) gather preliminary feedback about the feasibility and acceptability of delivering CS-PTSD Coach in primary care, (2) gather information on factors that could support or hinder implementation of CS-PTSD Coach in primary care clinics in order to aid in conducting a future pragmatic clinical trial of the effectiveness of CS-PTSD Coach, and (3) develop and refine a clinician manual for CS-PTSD Coach that is responsive to VA provider and veteran feedback.
METHOD
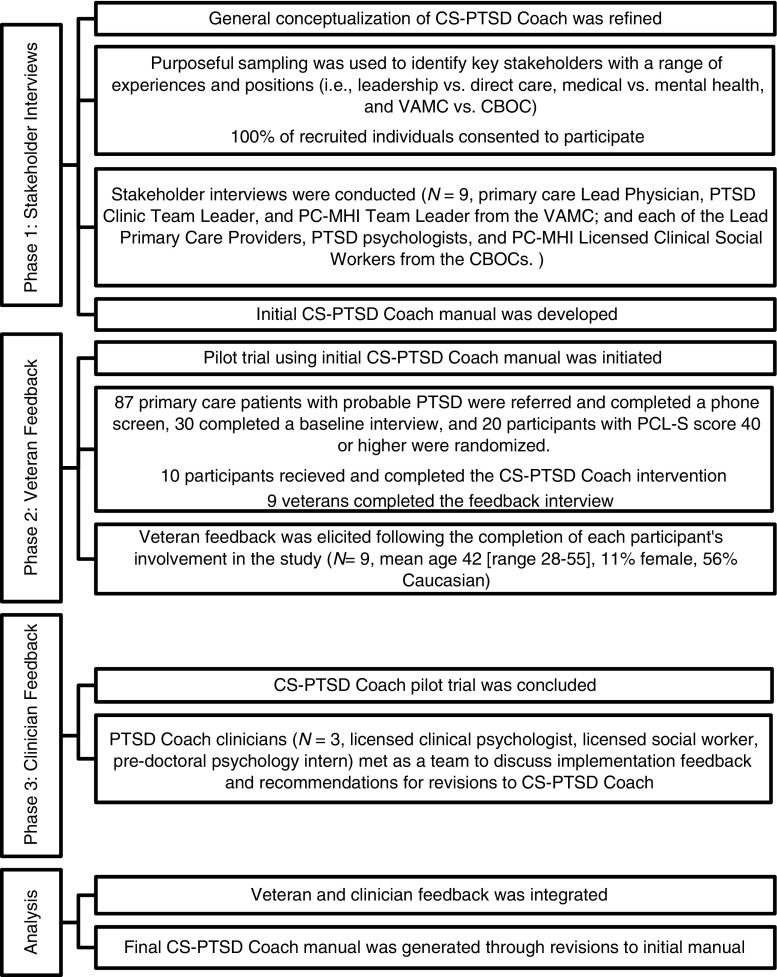
The methodology for this study is divided into three phases: (1) stakeholder interviews regarding implementation constructs, (2) veteran feedback regarding CS-PTSD Coach, and (3) clinician feedback regarding CS-PTSD Coach. These phases were sequential and each phase contributed to the development and refinement process for the CS-PTSD Coach intervention. Specifically, stakeholders were first interviewed on barriers and facilitators to implementation, then the manual was drafted based on their feedback. Next, veterans provided feedback after receiving the CS-PTSD Coach intervention, then clinicians provided feedback after delivering CS-PTSD Coach; both veteran and clinician feedback were incorporated into manual revisions. Figure 1 details the purpose, recruitment rate, and sample characteristics for each phase. This study was approved by the Syracuse VA Institutional Review Board.
Fig 1.
Study Procedures Overview
CS-PTSD Coach intervention
CS-PTSD Coach was developed to fit within standard practice for PC-MHI clinicians; therefore, the intervention needed to be time-limited, problem-focused, patient-centered, and outcome-oriented. The protocol consists of a 4-session (30 min each) cognitive-behavioral intervention for PTSD. The goals of CS-PTSD Coach are to provide psycho-education, develop symptom management skills, provide personalized feedback on symptom severity, and ready patients for additional treatment, if needed. Within sessions, clinicians spend time identifying patients’ PTSD symptoms and discuss with them how to use PTSD Coach to manage their specific PTSD symptoms. Symptom management strategies (e.g., diaphragmatic breathing) from the app are suggested by the clinician and practiced in session. Further, the clinician and patients collaboratively assigned homework to address the patients’ symptoms.
The first session focuses primarily on orienting the patient to the intervention, completing an initial PTSD symptom assessment (i.e., PTSD Checklist), providing instruction in PTSD Coach app use, delivering psychoeducational information, and collaborative goal setting. The second and third sessions involve reviewing progress with using the app to manage symptoms, practicing symptom management skills together, providing feedback to patients regarding implementation of skills, problem solving any barriers to engaging in active symptom management, and instruction and encouragement for continued use. The fourth session focuses on continued instruction and encouragement to use active coping skills, identifying ongoing patient needs, facilitating referrals, if needed, for additional mental healthcare, consolidation of learned skills, and termination. The first session occurs in-person, but subsequent sessions can be either in-person or by telephone, depending on patient preference. The CS-PTSD Coach manual, as just described, was revised to incorporate feedback after study phases 2 and 3.
Participants and procedures
Phase 1: Stakeholder interviews on implementation constructs
VA PC-MHI providers, primary care providers (MDs), and primary care leadership (N = 9) were selected based on their clinical and leadership positions with the goal of gathering data from a variety of individuals in different roles and at different facilities, who all provide direct care or oversight of direct care for primary care patients with PTSD. Please note that, throughout the manuscript, we will refer to participants who provided feedback during the stakeholder interviews as “providers” to differentiate them from those who delivered the CS-PTSD Coach intervention who we refer to as “clinicians.” Staff members from an urban VA Medical Center (VAMC) and two satellite primary care clinics (known in VA as Community Based Outpatient Clinics, CBOCs) that serve more rural areas were included. Staff members from CBOCs were included because these clinics usually have fewer resources to offer to primary care patients with PTSD and, therefore, are in greater need of additional services. Providers in the stakeholder interviews provided informed consent in a group setting with opportunities to ask questions individually. Informed consent included the provision that no identifying information would be made part of the study results or shared with supervisors.
VA provider participants were organized into four 30–60 min discussion sessions based on their location and availability. Sessions consisted of 1–4 participants and were led by the first author. We sought to identify key organization variables from CFIR [37] regarding the implementation of CS-PTSD Coach using two primary methods: a brief survey followed by a semi-structured qualitative interview. Participants were first presented with an overview of the content of CS-PTSD Coach and given a tour of the PTSD Coach app. After completing the CFIR Survey [38], they were asked to comment in a semi-structured qualitative interview on which CFIR constructs they believed would be most important in affecting implementation of the CS-PTSD Coach protocol in primary care. A preliminary draft of the CS-PTSD Coach manual was drafted based on this data.
Phase 2: Veteran feedback on CS-PTSD coach
Veterans with PTSD (N = 9) completed the CS-PTSD Coach protocol as a part of a pilot study (see Fig. 1). Participants were selected for inclusion in the pilot study if they were enrolled in primary care, had a PTSD Checklist [40] score above the recommended clinical cutoff for VA primary care settings (44 or greater), did not demonstrate gross cognitive impairment, had no suicidal intent or attempts in the past 2 months, had not received mental health counseling for PTSD in the last 2 months outside of VA primary care, and had no intent to initiate PTSD treatment in specialty mental health care in the next 2 months. An iPod Touch was lent to participants who did not have their own mobile device that was capable of running PTSD Coach. All participants provided informed consent. Following receipt of 8 weeks of CS-PTSD Coach treatment, Veterans completed the Client Satisfaction Questionnaire [42] and a patient feedback interview. Symptom change results for the pilot trial are reported elsewhere [39].
Phase 3: Clinician feedback on CS-PTSD coach
Three VA clinicians with PC-MHI experience delivered CS-PTSD Coach in the pilot study and provided structured feedback on their experiences and the clinician manual at the end of the study. At the time of the study, two of the three clinicians were working as PC-MHI providers.
MEASURES
CFIR
The CFIR construct survey is based on the CFIR model developed and tested by Damschroder et al. [37] and seeks to identify relevant implementation factors within specific sites. The purpose of using CFIR in designing interventions is to capitalize on existing facilitators and develop strategies to overcome local barriers. The survey provides a brief definition of each construct and was used to gain an initial rating from each participant about the relative importance of the constructs (1—very unimportant to 5—very important).
These semi-structured interviews inquired about the CFIR implementation constructs that participants perceived as most important to CS-PTSD Coach implementation. Participants were also asked to discuss clinic-specific barriers and facilitators for implementing CS-PTSD Coach, how CS-PTSD Coach should be delivered in their clinic, and how best to introduce it to patients. Consistent with a multidisciplinary participatory process described by Curran et al. [32], the hour-long interview prompted participants to explore potential areas of staff resistance, such as concerns that the clinic is already too busy to adopt new practices, and to problem-solve strategies to address concerns that arose during the interview. Participants were also asked to provide their perspectives on both positive and negative aspects of the CS-PTSD Coach protocol.
PTSD checklist
The PTSD Checklist-Specific (PCL-S) is a 17-item self-report measure of PTSD severity based on the DSM-IV [40, 41]. The PTSD Checklist has good psychometric properties and was used as a screener for inclusion criteria for veterans entering the pilot trial and is used within the PTSD Coach app.
Client satisfaction questionnaire
The Client Satisfaction Questionnaire is an 8-item self-report measure that assesses patient satisfaction with treatment [42]. This measure is reliable and higher scores have been shown to relate to treatment completion and symptom reduction.
Feedback interview
The qualitative veteran feedback interview was developed for the current project. It was administered by phone following completion of CS-PTSD Coach intervention. Participants were asked open-ended questions about their impressions of CS-PTSD Coach, what they found helpful, and changes they would recommend (e.g., more or less clinician contact). This interview lasted about 15 min.
Data analysis
Phase 1: Descriptive statistics were used to summarize the CFIR Survey and Client Satisfaction Questionnaire data. Additionally, a series of one-sample t tests were conducted to compare importance ratings for each CFIR construct with a rating of “neutral” importance and to determine which implementation constructs stood out as particularly important. Given the number of analyses, a Bonferroni correction was used to minimize the potential for Type I errors. Thus, only p values of <.002 were considered significant for the purposes of this study.
Qualitative interviews were recorded and transcribed. A structured, content-based deductive, coding system developed based on previous research with the CFIR model was used to code the data from the interviews [37]. The first transcript was independently coded by three investigators using a codebook developed for the current study, then discussed as a team to calibrate ratings. Two investigators then independently coded the rest of the transcripts. Each identified statement was coded on 3 domains: CFIR construct, valence of the comment (i.e., was the comment positive or negative?), and strength of the comment (i.e., was the comment strong or weak?). The importance/strength of the facilitators and barriers were determined based on the emphasis, tone, language, and number of comments within the qualitative interviews. Following the coding process, the coders consolidated their independent ratings. The lead investigator resolved discrepancies between codes and summarized the results. Constructs that were discussed as important (and rated as “strong”) by the most participants were determined to be the most important constructs for CS-PTSD Coach implementation.
Phase 2 and 3: Veteran and clinician feedback data were analyzed by two authors using a general inductive approach [43] by conducting multiple readings of the interview notes, organizing the comments into themes based on the research objectives, identifying specific recommendations for change, summarizing more general feedback comments within major themes, and fitting them into the broader CFIR model.
RESULTS
Phase 1: Stakeholder interviews on implementation constructs
CFIR constructs rated as significantly more important than “neutral” across providers (N = 9) were: relative priority, available resources, compatibility, patient needs and resources, implementation climate, leadership engagement, knowledge and beliefs about PTSD Coach, and planning (see Table 1). Overall, mean ratings suggested that provider stakeholders considered most of the CFIR constructs important for CS-PTSD Coach implementation.
Table 1.
One-sample t test results for stakeholder importance ratings of CFIR constructs
| CFIR construct | M (SD) | t(8)a | p b |
|---|---|---|---|
| Relative priority | 3.89 (0.33) | 8.00 | <0.001* |
| Available resources | 4.00 (0.50) | 6.00 | <0.001* |
| Compatibility | 4.33 (0.71) | 5.66 | <0.001* |
| Patient needs and resources for PTSD | 4.11 (0.60) | 5.55 | 0.001* |
| Implementation climate | 4.11 (0.60) | 5.55 | 0.001* |
| Leadership engagement | 4.11 (0.60) | 5.55 | 0.001* |
| Knowledge and beliefs about PTSD coach | 4.11 (0.60) | 5.55 | 0.001* |
| Planning | 4.11 (0.60) | 5.55 | 0.001* |
| Relative advantage | 3.89 (0.60) | 4.44 | 0.002 |
| Design quality and packaging | 3.89 (0.60) | 4.44 | 0.002 |
| Complexity | 4.11 (0.78) | 4.26 | 0.003 |
| Evidence strength and quality | 4.00 (0.71) | 4.24 | 0.003 |
| Learning climate | 3.78 (0.67) | 3.50 | 0.008 |
| Readiness for implementation | 3.78 (0.67) | 3.50 | 0.008 |
| Access to information | 3.78 (0.67) | 3.50 | 0.008 |
| Adaptability | 3.89 (0.78) | 3.41 | 0.009 |
| Other personal attributes | 3.56 (0.53) | 3.16 | 0.013 |
| Opinion leaders/champions | 3.89 (0.93) | 2.87 | 0.021 |
| External policy and incentives | 3.44 (0.53) | 2.53 | 0.035 |
| Executing | 3.78 (0.97) | 2.40 | 0.043 |
| Self-efficacy | 3.44 (0.73) | 1.84 | 0.104 |
| Formally appointed implementation leaders | 3.67 (1.12) | 1.79 | 0.111 |
| Culture | 3.44 (1.13) | 1.18 | 0.272 |
| Cost | 3.33 (1.23) | 0.82 | 0.438 |
| Tension for change | 3.00 (1.23) | 0.00 | 1.000 |
| Intervention source | 2.67 (1.12) | −0.89 | 0.397 |
| Peer pressure | 2.56 (1.01) | −1.32 | 0.225 |
aThe t tests compared all constructs to a test value of 3 which is equivalent to “neutral” on the rating scale (range = 1–5) in order to evaluate which constructs were significantly more likely to be rated as important or very important
b t tests were evaluated using a Bonferroni correction for 27 comparisons. Only p values of <.002 were considered significant for the purposes of this study
*p < .002
Additionally, we identified CFIR constructs that were identified by at least 2 participants as being among the three “most important” constructs for implementation of CS-PTSD Coach. These constructs were: compatibility, patient needs and resources, leadership engagement, complexity, learning climate, and adaptability. Notably, none of the constructs were rated as being within the top three most important by more than 2 stakeholders.
CFIR constructs emerging as most important from qualitative analysis of provider interviews included: (1) understanding patient needs and resources, (2) compatibility with the primary care setting, (3) having strong leadership engagement, (4) the study and intervention having low complexity, (5) knowledge and beliefs about CS-PTSD Coach, (6) tension for change, (7) patient engagement, and (8) implementation climate. These findings largely mirror the quantitative results described above and emphasize the aspects of implementation viewed as most important by the stakeholder. These constructs were either deemed to be facilitators or barriers based on the valence of the statements as rated by the coders. Table 2 provides a list of the facilitator themes identified, which CFIR construct they represent, and sample quotes supporting them. Table 3 presents identified barrier themes, which CFIR construct they represent, and a plan generated jointly by participants and the lead investigator for resolving each barrier. Facilitators are listed in rank order, with the more important facilitator themes identified first. Similarly, barriers are listed with the strongest barriers to implementation listed first. During the qualitative analyses, the only notable difference in content between the VA medical center and CBOC interviews was that the CBOCs expressed more concerns about technology gaps as a barrier for both veterans and providers. The initial manual described above was prepared for piloting based on these results.
Table 2.
CS-PTSD coach facilitators as identified by the qualitative analyses
| Facilitator theme | CFIR construct | Sample quote demonstrating construct |
|---|---|---|
| Stakeholders | ||
| 1. CS-PTSD Coach will help veterans overcome common barriers to receiving PTSD treatment: | Patient needs and resources | “For younger, working people you can sell it as something that isn’t based on fixed face to face visits with providers. It’s flexible to their lifestyle. For the older folks the hook would really be ‘here’s something new and that’s not the standard PTSD therapy you might have been involved with in the past. It’s not a group, it’s not exposure, it’s self-directed, you can choose what you do.’” |
| 2. CS-PTSD Coach fits well into the primary care setting: | Compatibility | “Primary care integration is so problem solution focused. We try to focus on one issue in terms of the referral. We work in the here and now and try to develop better coping strategies. So this does fit well.” |
| 3. Specific features of CS-PTSD Coach will help engage veterans in care: | Patient engagement | “When you combine technology that looks nice graphically, it pulls you in and makes you want to take advantage of the self-management tools. I think the built-in timers and schedules to remind yourself to do those things are very beneficial.” |
| 4. CS-PTSD Coach fits well with the needs and characteristics of primary care patients with PTSD: | Patient needs and resources | “Some patients don’t necessarily have that official diagnosis but they do have a lot of symptoms. This would be something to help them as a way to remind them to do some of the things I talk about with them about.” |
| 5. CS-PTSD Coach addresses a gap in current primary care services: | Tension for change | “I think it’s good for primary care providers who are very frustrated with PTSD because we recognize how much it impacts on all their other physical health. Unlike depression or anxiety, where we feel like we have some capacity to make interventions in primary care, we feel totally lost when it comes to PTSD. We are not aware of any interventions that are really successful that primary care providers can do. You know we prescribe SSRI’s that maybe have some benefit. I think we are aware that the people who have been successful with PTSD treatment are the ones who are fully engaged in it. And we can’t get people to treatment.” |
| 6. CS-PTSD Coach will help primary care patients transition to PTSD specialty care: | Compatibility | “Using this could make the transition a little smoother when they come into specialty care. In the PTSD specialty clinic, we’re doing PCL’s [PTSD Checklists] regularly and we’ll start with a structuralized interview. If they are already monitoring their symptoms it’s not a new burden.” |
| Veterans | ||
| 1. CS-PTSD Coach has an effective design (e.g., amount of information, tools, session number and format). | Design quality and packaging | “It was the right number of sessions, gives you independence but also doesn’t leave you on your own.” |
| 2. Clinician support was important to engaging with the app. | Patient engagement | Veteran regarding the interaction with the clinician: “I began to seek [the PTSD Coach app] out as treatment as opposed to doing it because I had to.” |
| 3. Flexibility with session format and spacing between sessions facilitated completion. | Patient needs and resources | “It was very helpful that she allowed me to do phone and in person appointments… I was happy to be included even though I couldn’t make it every time… the flexibility allowed me to be in this project.” |
| Clinicians | ||
| 1. Flexibility with the protocol is important. | Patient needs and resources | “One of my patients wouldn’t have been able to participate if we hadn’t included the option for conducting phone sessions.” |
Table 3.
CS-PTSD coach barriers as identified by the qualitative analyses
| Barrier theme | CFIR construct | Initial plan for resolving the barrier |
|---|---|---|
| Stakeholders | ||
| 1. Strong leadership support and clinic champions are needed | Leadership engagement | Elicit strong local primary care and mental health leadership. Find a champion for each primary care clinic. |
| 2. The technology gap experienced by a minority of providers and patients must be addressed | Complexity | The study team will train PC-MHI clinicians to be comfortable with the technology and/or select tech-savvy PC-MHI clinicians. In marketing the study, the CS piece will be emphasized in that even patients who are wary of technology can do this with the help of the clinician. This treatment will not be for everyone, but offered as a novel alternative to traditional treatment. |
| 3. PCPs need education about how to talk to their patients about PTSD and PTSD treatment | Knowledge and beliefs about the intervention | The training will be done immediately before initiating the protocol and will involve education on the effectiveness of PTSD treatments and scripts on how to talk to patients about seeing the PC-MHI clinician. |
| 4. Clinicians will need education about the app and why we are doing the study. | Knowledge and beliefs about the intervention | Clear up any misconceptions about PTSD Coach (e.g., this replaces traditional PTSD treatment). Provide strong rationale for why brief primary care based treatments for PTSD are needed. |
| 5. Primary care clinic staff will need to be open to do new things. | Implementation climate | Need to select PC-MHI clinicians who are willing to do something new. When this is not possible, we need to try to motivate PC-MHI clinicians and provide them with a high level of support. Clinicians reluctant to adopt CS-PTSD Coach may be more motivated if they see their colleagues have early successes. |
| Veterans—none reported | ||
| Clinicians | ||
| 1. The manual did not provide enough instruction on collaborative goal setting | Patient engagement | The manual was revised to include explicit instructions for collaborative goal setting including wording to describe the goal setting process and adding explicitly stated goals for each session for clinicians to tailor to individual patients. |
| 2. The homework assignments were complicated | Complexity of the intervention | The homework assignments included in the manual were simplified so that the revised draft emphasizes only the components of the homework that clinicians perceived as most important. |
| 3. The manual lacked guidance on how to help more complex patients | Patient engagement | Clarification and recommendations were added to the manual regarding how to handle difficult case situations including ambivalent patients, unengaged patients, and patients with significant life stressors. |
| 4. Telephone sessions were difficult but this modality was important to patients | Patient needs and resources | Common difficulties with the telephone modality (e.g., cannot look at the patient’s device together to see the app) were identified in the manual and tips were added to facilitate telephone sessions despite barriers. |
| 5. Parts of the manual were complicated and difficult to read | Complexity | The manual language was simplified and the formatting was streamlined to improve readability and usability. |
Phase 2: Veteran feedback on CS-PTSD coach
Veterans (N = 9) had generally positive feedback regarding the program. On the Client Satisfaction Questionnaire, 100 % (N = 9) of the veterans reported good to excellent satisfaction with intervention characteristics including design quality (the intervention overall and specifically the quality, type, and amount of help they received) and fit to their needs and resources (specifically the usefulness of the intervention). Further, 78 % (n = 8) of the participants indicated that CS-PTSD Coach met all or most of their needs. In the feedback interview, none of the veterans indicated any problems with the program structure, content, sessions, or clinicians. Veterans indicated general satisfaction with the amount of the information presented, the tools, and the 30-min session format. In particular, veterans expressed satisfaction with the support and guidance provided from the clinician to help tailor the use of the app and develop treatment plans (including referrals to additional mental health resources as needed). In addition, feedback about the adaptability of the intervention indicated that the flexibility with in-person and telephone sessions helped participants continue with the intervention who would not otherwise have been able to participate. This feedback informed the decision to maintain the 30-min, 4-session format, and reinforced the premise that clinician-support would help veterans engage more fully in the app materials. In summary, most of the comments fit within the broader CFIR constructs of intervention characteristics, patient needs and resources, and patient engagement.
Phase 3: Clinician feedback on CS-PTSD coach
CS-PTSD Coach clinicians (N = 3) had generally positive feedback about the manual and the protocol. Specific recommendations for improvement included a larger emphasis on collaborative goal setting (patient engagement), simplification of the homework assignments (complexity of the intervention), reduction of homework demands (complexity of the intervention), clarification on how to handle difficult case situations (patient engagement), reminders on how to be flexible with the protocol to meet veterans’ needs (patient needs and resources), inclusion of general tips for more effective sessions when conducted via telephone (patient needs and resources), and re-formatting of the manual to facilitate utilization (complexity of the intervention). Specific adjustments to the protocol structure were also recommended, including moving referral for additional mental health care, maintenance of gains, and relapse prevention to session 3 and changing session 4 to a follow-up appointment to provide ongoing support and check-in regarding follow-through on the treatment plan. These changes are reflected in the revised manual. In summary, most clinician feedback was focused on the broader CFIR themes of patient engagement, patient needs and resources, and intervention complexity.
Final CS-PTSD Coach manual
The initial CS-PTSD Coach manual was revised following incorporation of the feedback from veterans and clinicians. Changes were made to address concerns raised and to highlight the aspects of the program found to be most helpful. The final CS-PTSD Coach protocol consists of three 30-min sessions, spaced 2 weeks apart, and one 30-min 1-month follow-up session. The three initial sessions focus on goal setting, symptom management, and facilitation of the PTSD Coach app, while the follow-up session reinforces the ongoing treatment plan. Following an initial in-person session, CS-PTSD Coach is designed to be implemented in multiple formats including in-person, by telephone, or via videoconferencing. Sessions consist of collaborative goal development, psychoeducation, basic instruction in app use, PTSD symptom assessment, teaching and practicing of skills for symptom management, and homework assignments for further skill development and mastery. Specifically, clinicians guide the patient through setting realistic goals for the brief intervention (e.g., to learn skills to address a symptom domain of PTSD, learn more about PTSD treatment options), developing skills to address treatment goals, and ongoing treatment planning. The resulting intervention is designed to be patient-centered and feasible for implementation in Primary Care Behavioral Health settings.
DISCUSSION
The current study reported the development and preliminary evidence regarding feasibility, acceptability, and implementation of a clinician intervention to facilitate use of the PTSD Coach app in primary care, namely CS-PTSD Coach. Our study demonstrates the development and refinement process for a clinician-supported mobile intervention in primary care. Results indicated that CS-PTSD Coach was a good match to patient needs and resources and to the primary care setting. In addition, primary care medical and mental health professionals, as well as veterans, had favorable experiences with CS-PTSD Coach. Initial implementation findings were used to refine the intervention to better fit the primary care setting and patient needs. The methodology and results regarding the manual development and refinement process from this study are valuable for guiding a large scale test of the effectiveness of CS-PTSD Coach. They can also be generalized to inform the implementation of other clinician guided mHealth treatments.
Phase 1 results suggest that stakeholders believe a number of CFIR constructs are important when considering implementation of CS-PTSD Coach. Specifically, CS-PTSD Coach was perceived as highly compatible with other primary care services and subsequent care veterans receive in the specialty PTSD clinic. The compatibility to both care settings and the ongoing availability of the PTSD Coach app following referral may help patients smoothly transition from primary care to specialty care. The intervention was also seen as meeting the needs of primary care veterans with PTSD in that it was flexible enough to be delivered either face-to-face or remotely, allowed patients to self-direct treatment to focus on their needs/goals, and was appropriate for veterans with a subthreshold PTSD diagnosis. All stakeholders interviewed thought strong leadership engagement and support was necessary for successful implementation, and lack of support would be a major potential barrier for implementation. The training needs of primary care medical providers and PC-MHI clinicians in regards to their knowledge and beliefs about CS-PTSD Coach also emerged as an important construct across all three analyses methods. Specifically, primary care medical providers may need training on how to engage their patients in a discussion about their PTSD symptoms and treatment options, and PC-MHI clinicians need the technical knowledge on mobile app use and to understand how CS-PTSD Coach will be helpful for their patients.
Phase 2 results indicated high acceptability and satisfaction with CS-PTSD Coach among the nine veterans who completed the feedback interviews. Their qualitative feedback complemented the stakeholder feedback regarding CS-PTSD Coach being responsive to patient needs in terms of treatment flexibility and adaptability. Veteran feedback also emphasized that one of the primary benefits of CS PTSD Coach was it helped to engage patients in the treatment process, primarily through interaction with the clinician. Feedback provided by the three PC-MHI clinicians who delivered CS-PTSD Coach during Phase 3 focused on specific alterations to the manual to help the intervention more fully engage patients, meet their needs, and reduce the complexity of treatment delivery. Together, their feedback suggests that veterans and clinicians both value the additional support in engaging with available mobile applications. Further, need for low complexity of the intervention (repeated across all three phases) suggests that basic aspects of clinician support (e.g., coaching to tailor app use to symptoms, goal setting, and homework assignment) might be sufficient to facilitate patient use of similar mobile apps.
The CFIR constructs that emerged as important in this study span across all five CFIR domains. Need for low complexity emerged as an important “intervention characteristic” to consider in future clinician-supported smartphone interventions. Patient needs and resources emerged as an important characteristic of the “outer setting” (external influences such as community, society, and policy acting on the organization) to help identify clinical utility of new technology facilitated primary care interventions. Compatibility, leadership engagement, and implementation climate all emerged as important characteristics of the “inner setting” (local organizational environment) to aid with local implementation. Provider knowledge and beliefs of PTSD Coach emerged as important “individual characteristics” that will be important in training and incorporating technology into practice. Patient engagement emerged as an important “process” characteristic of the implementation. Our findings demonstrate the utility of using a broad framework like CFIR, in that specific, actionable factors were identified across multiple dimensions.
The current research is integral to the growth of the literature within multiple domains in that it (1) initiates investigation into an intervention which would fill a current need for PC-MHI PTSD interventions, (2) provides additional evidence for the acceptability of adding clinician support to technology-based interventions, and (3) demonstrates the use of an implementation science methodology to develop and adapt an intervention for clinical practice. This implementation model enabled the investigators to adapt the protocol for utility in the primary care setting and enhance the likelihood of success for future research and implementation efforts.
The major limitation of this study is that implementation findings can be idiosyncratic to the specific sites where they are collected. This limitation was minimized by gathering input from providers at three sites (one large and two small clinics) to increase the generalizability of our findings to multiple types of primary care settings. Also, VA primary care clinics across the USA share many similarities in terms of organizational structure, the delivery of integrated mental health services, and the high prevalence of patients with PTSD. Our results encourage further research on how knowledge about site-specific implementation facilitators and barriers can be applied to develop successful implementation strategies.
Overall, these findings suggest that a brief PC-MHI intervention that combines clinician support with a mobile app is highly acceptable to VA staff stakeholders responsible for primary care and mental health leadership, PC-MHI clinicians who delivered the intervention, and veterans with PTSD who received the intervention. Our methodology identified a wide variety of implementation constructs that will facilitate future implementation efforts and provided an opportunity to identify and problem-solve potential barriers for future implementation. The CS-PTSD Coach manual resulting from the iterative development process was strengthened by each research phase. Our findings on the importance of specific implementation constructs may generalize to other mental health interventions delivered in the primary care setting and to interventions that combine clinician support with technology-based resources.
Acknowledgments
This manuscript is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Mental Health Quality Enhancement Research Initiative and the Center for Integrated Healthcare.
Compliance with ethical standards
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Implications
Practice: Consideration of implementation factors, specifically compatibility with the treatment setting, the ability of the intervention to address patient needs, leadership engagement, provider knowledge, and beliefs about the intervention, may facilitate implementation of behavioral health interventions.
Policy: Policymakers and administrators should foster environments that encourage implementation of novel approaches and support of interventions that combine clinician support with technology-based resources.
Research: Our results encourage further research on patient and implementation outcomes associated with CS-PTSD Coach and other technology facilitated interventions.
An erratum to this article is available at http://dx.doi.org/10.1007/s13142-016-0415-7.
References
- 1.Magruder KM, Frueh BC, Knapp RG, et al. Prevalence of posttraumatic stress disorder in Veterans Affairs primary care clinics. Gen Hosp Psychiatry. 2005;27(3):169–179. doi: 10.1016/j.genhosppsych.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Stein MB, McQuaid JR, Pedrelli P, Lenox R, McCahill ME. Posttraumatic stress disorder in the primary care medical setting. Gen Hosp Psychiatry. 2000;22(4):261–269. doi: 10.1016/S0163-8343(00)00080-3. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zlotnick C, Rodriguez BF, Weisberg RB, et al. Chronicity in posttraumatic stress disorder and predictors of the course of posttraumatic stress disorder among primary care patients. J Nerv Ment Dis. 2004;192(2):153–159. doi: 10.1097/01.nmd.0000110287.16635.8e. [DOI] [PubMed] [Google Scholar]
- 5.Gillock KL, Zayfert C, Hegel MT, Ferguson RJ. Posttraumatic stress disorder in primary care: prevalence and relationships with physical symptoms and medical utilization. Gen Hosp Psychiatry. 2005;27(6):392–399. doi: 10.1016/j.genhosppsych.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Rauch SA, Morales KH, Zubritsky C, Knott K, Oslin D. Posttraumatic stress, depression, and health among older adults in primary care. Am J of Geriatric Psychiatry. 2006;14(4):316–324. doi: 10.1097/01.JGP.0000199382.96115.86. [DOI] [PubMed] [Google Scholar]
- 7.Karlin BE, Ruzek JI, Chard KM, et al. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. J Trauma Stress. 2010;23(6):663–673. doi: 10.1002/jts.20588. [DOI] [PubMed] [Google Scholar]
- 8.Desai RA, Stefanovics EA, Rosenheck RA. The role of psychiatric diagnosis in satisfaction with primary care: data from the department of veterans affairs. Med Care. 2005;43(12):1208–1216. doi: 10.1097/01.mlr.0000185747.79104.90. [DOI] [PubMed] [Google Scholar]
- 9.Spoont MR, Nelson DB, Murdoch M, et al. Impact of treatment beliefs and social network encouragement on initiation of care by VA service users with PTSD. Psychiatr Serv. 2014;65(5):654–662. doi: 10.1176/appi.ps.201200324. [DOI] [PubMed] [Google Scholar]
- 10.Stecker T, Shiner B, Watts BV, Jones M, Conner KR. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64(3):280–283. doi: 10.1176/appi.ps.001372012. [DOI] [PubMed] [Google Scholar]
- 11.Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72(3):238–255. doi: 10.1521/psyc.2009.72.3.238. [DOI] [PubMed] [Google Scholar]
- 12.Post EP, Metzger M, Dumas P, Lehmann L. Integrating mental health into primary care within the Veterans Health Administration. Fam Syst Health. 2010;28(2):83–90. doi: 10.1037/a0020130. [DOI] [PubMed] [Google Scholar]
- 13.Harmon AL, Goldstein ES, Shiner B, Watts BV. Preliminary findings for a brief posttraumatic stress intervention in primary mental health care. Psychol Serv. 2014;11(3):295–299. doi: 10.1037/a0035846. [DOI] [PubMed] [Google Scholar]
- 14.Cigrang JA, Rauch SA, Avila L, et al. Treatment of active-duty military with PTSD in primary care: early findings. Psychol Serv. 2011;8(2):104–113. doi: 10.1037/a0022740. [DOI] [Google Scholar]
- 15.Engel CC, Bray RM, Jaycox LH, et al. Implementing collaborative primary care for depression and posttraumatic stress disorder: design and sample for a randomized trial in the U.S. military health system. Contemp Clin Trials. 2014;39(2):310–319. doi: 10.1016/j.cct.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18(3):268–280. doi: 10.1007/s10880-011-9237-4. [DOI] [PubMed] [Google Scholar]
- 17.Smith A. The smartphone difference. Pew Research Center. 2015; http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/.
- 18.Bush NE, Wheeler WM. Personal technology use by U.S. military service members and veterans: an update. Telemed J E Health 2015. [DOI] [PubMed]
- 19.Lindhiem O, Bennett CB, Rosen D, Silk J. Mobile technology boosts the effectiveness of psychotherapy and behavioral interventions: a meta-analysis. Behav Modif 2015. [DOI] [PMC free article] [PubMed]
- 20.Morland LA, Frueh C, Pierce K, Miyahira S. PTSD and telemental health: Updates and future directions. National Center for PTSD. Clin Quarterly. 2003;12:1–5. [Google Scholar]
- 21.Erbes CR, Stinson R, Kuhn E, et al. Access, utilization, and interest in mHealth applications among veterans receiving outpatient care for PTSD. Mil Med. 2014;179(11):1218–1222. doi: 10.7205/MILMED-D-14-00014. [DOI] [PubMed] [Google Scholar]
- 22.Price M, Yuen EK, Goetter EM, et al. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychotherapy. 2014;21(5):427–436. doi: 10.1002/cpp.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffman JE, Wald L, Kuhn E, Greene C, Ruzek J, Weingardt K. PTSD Coach Version 1.0.1. [Mobile Application]. 2011; Available at: https://itunes.apple.com/us/app/ptsd-coach/id430646302?mt=8. Accessed Sep 1, 2015.
- 24.Kuhn E, Greene C, Hoffman J, et al. Preliminary evaluation of PTSD Coach, a smartphone app for post-traumatic stress symptoms. Mil Med. 2014;179(1):12–18. doi: 10.7205/MILMED-D-13-00271. [DOI] [PubMed] [Google Scholar]
- 25.Miner A, Kuhn E, Hoffman JE, Owe JE, Ruzek J, Taylor CB. Feasibility, acceptability, and potential efficacy of the PTSD Coach app in a community sample of trauma survivors. Psychol Trauma. In Press. [DOI] [PubMed]
- 26.Owen JE, Jaworski BK, Kuhn E, Makin-Byrd KN, Ramsey KM, Hoffman J. mHealth in the wild: using novel data to examine the reach, use, and impact of PTSD Coach. JMIR Mental Health. 2015;2(1):e7. doi: 10.2196/mental.3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pearson ML, Mattke S, Shaw R, Ridgely MS, Wiseman SH. (RAND Health, Santa Monica, CA). Patient self-management support programs: an evaluation. Final report. Rockville (MD): Agency for Healthcare Research and Quality (US);2007 Nov. Report No.: 08-0011. Contract No.: 282-00-0005.
- 28.Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: is human contact necessary for therapeutic efficacy? Clin Psychol Rev. 2011;31(1):89–103. doi: 10.1016/j.cpr.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 29.Proudfoot J, Parker G, Manicavasagar V, et al. Effects of adjunctive peer support on perceptions of illness control and understanding in an online psychoeducation program for bipolar disorder: a randomised controlled trial. J Affect Disord. 2012;142(1-3):98–105. doi: 10.1016/j.jad.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 30.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care. 1998;7(3):149–158. doi: 10.1136/qshc.7.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Curran GM, Mukherjee S, Allee E, Owen RR. A process for developing an implementation intervention: QUERI Series. Implement Sci. 2008;3:17. doi: 10.1186/1748-5908-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rogers EM. Diffusion of Innovations. 5. New York, NY: Free Press; 2003. [Google Scholar]
- 34.Damschroder LJ, Lowery JC. Evaluation of a large-scale weight management program using the consolidated framework for implementation research (CFIR) Implement Sci. 2013;8:51. doi: 10.1186/1748-5908-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.English M, Nzinga J, Mbindyo P, Ayieko P, Irimu G, Mbaabu L. Explaining the effects of a multifaceted intervention to improve inpatient care in rural Kenyan hospitals—interpretation based on retrospective examination of data from participant observation, quantitative and qualitative studies. Implement Sci. 2011;6:124. doi: 10.1186/1748-5908-6-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Connell LA, McMahon NE, Watkins CL, Eng JJ. Therapists’ use of the Graded Repetitive Arm Supplementary Program (GRASP) intervention: a practice implementation survey study. Phys Ther. 2014;94(5):632–643. doi: 10.2522/ptj.20130240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Damschroder L, Aron D, Keith R, Kirsh S, Alexander J, Lowery J. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science. 2009;4(50). [DOI] [PMC free article] [PubMed]
- 39.Possemato K, Kuhn E, Johnson E, et al. A Pilot Randomized Controlled Trial of Clinician-Supported PTSD Coach: Impact on PTSD and Mental Health Treatment Utilization. Gen Hosp Psychiatry. 2016; 38: 94-98. [DOI] [PubMed]
- 40.Weathers FW, Ford J. Psychometric properties of the PTSD Checklist (PCL-C, PCL-S, PCL-M, PCL-PR) In: Stamm BH, editor. Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press; 1996. [Google Scholar]
- 41.National Center for PTSD. Using the PTSD Checklist for DSM-IV (PCL). U.S. Department of Veterans Affairs. 2014; Available at: http://www.ptsd.va.gov/professional/pages/assessments/assessment-pdf/PCL-handout.pdf. Accessed Sep 1, 2015.
- 42.Attkisson CC, Greenfield TK. The UCSF client satisfaction scales: I. The client satisfaction questionnaire-8. In: Mariush ME, ed. The use of psychological testing for treatment of planning and outcome assessment. Vol 3. 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 2004:799-811.
- 43.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27(2):237–246. doi: 10.1177/1098214005283748. [DOI] [Google Scholar]