Abstract
In spite of the well-known benefits of physical activity, the vast majority of children in North America do not meet current international guidelines for accumulating sufficient health-enhancing physical activity. Indeed, despite considerable attention to this population health crisis, the current prevalence of inactivity, along with its concomitant health consequences, shows little sign of abating. In this paper, we identify acknowledged barriers to wide scale physical activity adoption and maintenance at the population level among children and propose a viable tripartite framework (albeit one that would require political support) that we hope will provide the basis for debate and implementation. We emphasize that each of these considerations, in isolation, would be insufficient to substantively address the problem, but when combined would ensure that all elementary school children (without any medical contraindication) are sufficiently active, rather than the minority of this population.
Keywords: Physical activity, Children, Population health, Policy
In North America, the vast majority of children do not meet current guidelines of 60 min of daily moderate to vigorous physical activity (MVPA) [1, 2]. Specifically, in the USA, 42 % of children aged 6–11 are estimated to meet these recommendations, while only 8 % of adolescents are sufficiently active [1]. The picture is equally bleak in Canada, with less than 10 % of children and youth meeting these guidelines [2]. In light of compelling medical and epidemiologic evidence concerning both the physiological and psychological benefits of physical activity [3], as well as the prevalence and risks of inactivity (e.g., reduced risk of diabetes, obesity, cardiovascular disease, most cancers, depression) [3], a wide-range of behavior-change interventions and initiatives have been developed and implemented over the past few decades to encourage children to adopt and sustain active lifestyles. These initiatives have been tested using increasingly robust research designs. Unfortunately, however, the accumulated evidence to date suggests that the effectiveness of these interventions have been limited. To illustrate, in a recent meta-analysis that examined the effects of interventions that were tested using controlled trials in relation to objective measures of physical activity among children, the overall effect of the interventions was very small and equated to an average increase of just 4 min more of walking or running per day on children’s overall activity levels [4].
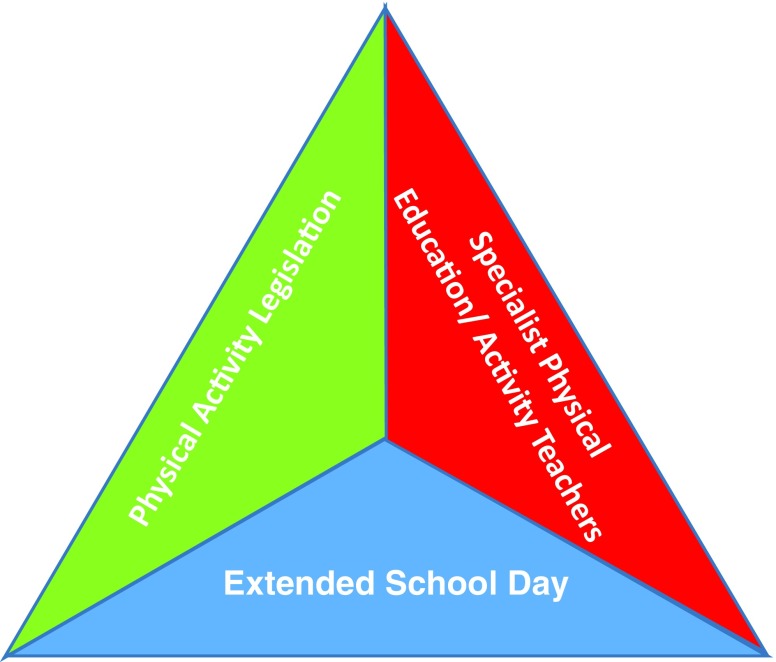
Given the current evidence regarding (a) the small effects that the best pediatric physical activity interventions can deliver, (b) the pervasive levels of inactivity that exist among children, and (c) the considerable health-related and developmental costs associated with inactivity among this population, we propose that it is time for a substantive rethink about our options to redress this public health crisis. In this paper, we highlight evidence concerning some of the most substantive barriers to wide scale physical activity adoption and maintenance (at the population level) and articulate a viable tripartite (see Fig. 1) health-policy approach (one that would require political support) that would ensure that most North American children meet international physical activity guidelines. Each of these three considerations, in isolation, would be insufficient to impart substantial change but, as we explain later in the paper, when combined would ensure that all elementary school children are sufficiently active, rather than the minority.
Fig 1.
Tripartite model for physical activity provision in North American elementary schools
The first consideration relates to the potential utility of legislation with regard to the implementation of physical education and physical activity. In the USA, the Centers for Disease Control (CDC) currently recommends that elementary school students participate in 150 min of physical education (PE) per week [5] (i.e., 30 min/day), with the expectation being that students accumulate additional physical activity outside of school hours [5, 6]. Although many states (n = 38, 78 %) and school districts in the USA have implemented minimum PE requirements, even among those schools that have (by virtue of ‘codified laws’) specific time requirements for PE tend not to meet the CDC guidelines. For example, in a recent study by Perna and colleagues [6], elementary schools in the USA that were subjected to state requirements accumulated an average of 104.76 min/week of PE, whereas among those elementary schools without such a requirement, the mean time spent in PE was markedly lower (64.58 min/week). Based on these findings, three points are worthy of note. First, time spent in PE was assessed in this research by virtue of the amount of time that schools self-reported scheduling PE during the school year (assessed via the CDC School Health Policies and Programs Survey), and so likely represents an overestimation of the actual amount of time spent in PE. Second, although it is conceivable that schools subject to state requirement may have further inflated their self-report measures to some extent (due to normative pressures tied to legislation), it is noteworthy that elementary schools in those states that were subject to specific PE requirement laws participated in substantively more PE (on average, 40 min more per week) than those without such laws. Third, the majority of schools, regardless of whether they were subjected to state legislation, still did not meet the CDC guidelines for PE described above. When taken together, the results of this work suggest that legislation surrounding minimum physical activity levels in schools appears to be effective (when compared to no legislation). However, on the basis of this evidence, current legislative measures seem to be insufficient. So what else needs to be considered?
The second consideration relates to the barrier of time. One of the most frequently reported barriers to improving the amount of physical activity in elementary schools corresponds to competing demands on curriculum time [7]. Within our proposed framework, we propose extending the school day by 30–60 min and legislating that all elementary school-aged children (without medical contraindication) participate in at least 60 min of daily health-enhancing (i.e., moderate-to-vigorous) physical activity. Currently, the vast majority of adults in North America are also insufficiently active [1, 8], and as such it would seem unrealistic to expect inactive parents to ensure that their own children are sufficiently active (i.e., meet international guidelines) outside of school hours. Indeed, the accumulated evidence to date suggests that interventions that target parents to enhance child physical activity have demonstrated very limited success [9]. Schools have been widely identified as a viable context to promote health-enhancing physical activity [10]; however, for this potential to be realized, it is important that they also have sufficient ‘time’ during the school day to provide opportunities for children to adopt and sustain active lifestyles.
So how would this be done and what would be the costs of implementing such legislation? These are certainly not trivial questions; however, if we are serious about redressing this substantive public health problem, we believe that answers to these questions be considered. At present, the average child in North America goes to school for about 6 and a half hours a day for 180 days a year. Driven by a political agenda for the USA to be more competitive on a global stage, there have been growing calls from President Barack Obama for children to spend more time in schools [11]. Some initiatives already exist in the USA that have embraced a longer school day. Massachusetts, for example, became the first state (in 2005) to embrace an extended working day on a large scale basis through an Expanded Learning Time initiative [12]. The state currently provides an additional $1300 per child to cover an additional 300 h of time in school per year [12]. It should be noted, however, that the focus of that initiative is/was to extend the amount of time in the classroom and was not designed as a (physical activity) health promotion initiative. As a point of comparison, in the UK, the former Chancellor of the Exchequer, George Osborne, recently announced plans to increase the duration of the school day by an hour to accommodate additional extracurricular activities, including school sports, and built this into the UK government’s March 2016 budget [13]. When taken together, there appears to be a political will to consider extending school days in North America, and we would certainly echo such sentiments; however, we would suggest that such an extended school day should be used to implement increased (i.e., daily) health-enhancing physical activity, in much the same way as is currently being pursued within the UK. Parenthetically, in response to those who might be concerned that additional time spent in physical activity might detract from academic success, it is noteworthy that greater participation in physical activity appears to be prospectively related to improved academic performance among children [14].
The third consideration within our proposed framework relates to the recruitment and training of teachers with specialist training in physical education and physical activity provision (e.g., coaching) in elementary schools. This already happens in most secondary schools in North America, so why should elementary schools be devoid of this provision? There is now considerable evidence to suggest that elementary school teachers (who are often required to teach a broad range of subjects) often lack the confidence and competencies to teach physical education [15], and so it should not be seen as a surprise that children in such settings do not receive sufficient support for accruing optimal levels of health-enhancing physical activity. With regard to the training of elementary school teachers, two points are worthy of note. First, we envision that the training of teachers could be accomplished within the context of existing teacher training frameworks/institutions (parallel to the training of secondary school physical education teachers). Similarly, experienced teachers are typically required to undertake (one-day) professional development workshops over the course of the school year, and so greater opportunities could/should be made available to ‘upskilling’ experienced elementary school teachers with competencies to teach physical activities/education within these workshops. When taken together, from a fiscal perspective, if such training opportunities are embedded within these existing frameworks, the increased costs associated with such training would be (relatively) limited. The second point is that, within the context of this additional physical activity provision within elementary schools, contemporary knowledge from educational psychology and motivation science [16] should be harnessed to ensure that time involved in such activities is optimally spent. For example, there is now compelling evidence that when teachers deliver physical education through ‘autonomy-supportive’ approaches (actions designed to foster student volition and choice), this tends to result in greater psychological need satisfaction, along with meaningful gains in classroom engagement, skill development, future intentions, and course achievement [17]. We also recognize that within the context of an extended school day, for those schools with limited space for physical activity, simply offering physical activities as an after-school provision might not be possible, and that for such schools (physical) activities might be scheduled throughout the course of the school day. However, if one accepts the premise that we, as a society, have a duty of care to support the healthy development of school-aged children, we feel that a paradigm shift is required in the way physical activity is supported.
When taken together, we believe that each of the considerations highlighted in the tripartite framework described in this paper require implementation, and that on their own they would be insufficient to bring about sufficient/substantive change. Specifically, while legislation surrounding time spent in physical education/activity clearly works to some extent (when compared to no legislation), if elementary schools do not have sufficient time to ensure children are engaged in physical activity, then it would be unrealistic to expect that all/most students will meet current guidelines. Similarly, even if the school day is expanded by 30–60 min and schools are legislated (by codified laws) to expand their offering of health-enhancing physical activity, this will not be sufficient unless schools possess the capacity—sufficient numbers of trained/qualified teachers—to ensure this expanded physical activity provision is implemented properly (i.e., high fidelity). Parenthetically, research from a prominent tracking study, conducted over 21 years, that assessed physical activity from childhood through to adulthood found that high levels of continuous physical activity among youth predicted a high level of physical activity in adulthood [18]. As such, by establishing regular physical activity during the formative years of childhood appears to have downstream effects on physical activity later in life; with physical activity in adulthood not only related to improvements in psychological and physical health [19], but also reduced health care costs (recent estimates indicate that physical inactivity in adulthood accounts for 11.1 % ($117 billion) of aggregate health care expenditure per year in the USA) [20].
Balanced against the public policy and professional practice implications presented above that accompany the tripartite model highlighted in this paper, there are several pressing research opportunities. For example, and as highlighted above, much of the accumulated data surrounding physical activity participation in schools subject to legislation versus those not subject to those requirements are based on self-report data [6]. Although opportunities to utilize highly controlled designs (e.g., randomized controlled trials) may be limited in examining the effectiveness of legislating physical activity on a large-scale basis, further work should certainly look to utilize more objective measures (e.g., accelerometry, pedometers) or even blinded third-party assessments (e.g., independent expert observations). Another important direction for research, corresponds to the implementation of rigorous policy/program evaluation tied to the dissemination of each/all of the proposed tripartite components, should they be taken up by school districts (or States/Provinces, should they be adopted on a large scale basis). From a validity theory perspective [21], this would not only include examination of potential adaptive outcomes touched upon in this paper (e.g., physical activity participation, academic achievement outcomes, socio-emotional growth and development), but also unanticipated consequences that might arise. For example, although an extension of the school day tied to providing added extra-curricular/physical activities would simply represent the provision of structure in the form of a reconstituted curriculum, if this is conveyed and implemented with a punitive emphasis (emphasis on threats or penalties from senior administrators), this would likely undermine teachers’ motivation as well as the quality of curriculum delivery [22]. In short, should the proposed tripartite recommendation presented in this paper gain traction, research should be implemented that examines both targeted outcomes, as well as highlighting potentially unanticipated consequences.
In conclusion, we realize, as with other large scale public-health change initiatives, such as that on tobacco control, that legislating for various health-enhancing or against health-compromising behaviors is not without controversy, and will be resisted by some. However, to use the old adage ‘if we do what we’ve always done we’ll get what we’ve always got’; and unless we take substantive action regarding the current levels of inactivity among children, this will continue to have major debilitative effect for the health and well-being of children as well as society at large. It is our hope that the proposed tripartite framework (see Fig. 1) be debated by those concerned with public health policy and, in time, implemented.
Acknowledgments
The authors can confirm that the manuscript has not been previously published and is not being simultaneously submitted elsewhere. As the submission is a commentary paper, no primary data were collected and so no statements are necessary with regard to previous reporting of data, control of primary data, human rights and informed consent related to study participants, the Declaration of Helsinki, and IRB approval. Mark R. Beauchamp is supported by a Michael Smith Foundation for Health Research Scholar Award as well as through funds from the Canadian Institutes of Health Research. Ryan E. Rhodes is supported by a Canadian Cancer Society Senior Scientist Award and the Give to Live organization as well as through funds from the Canadian Cancer Society, the Canadian Institutes of Health Research and the Social Sciences and Humanities Research Council of Canada. Claudio N. Nigg is supported by funds from the National Institutes of Health, the United States Department of Agriculture, and the Hawaii Medical Services Association Foundation.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 2.Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Catalogue no. 82-003-XPE. Health Rep. 2011;22(1):15–23. [PubMed] [Google Scholar]
- 3.Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phy Act. 2010;7:40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Metcalfe, B., Henley, W., & Wilkin, T. (2012). Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). Brit Med J, 345, e5888. doi:10.1136/bmj.e5888. [DOI] [PubMed]
- 5.U.S. Department of Health and Human Services (2010). (Accessed May 24, 2015, at http://www.cdc.gov/physicalactivity/downloads/PA_State_Indicator_Report_2010.pdf) State indicator report on physical activity. Washington, DC: U.S. Department of Health and Human Services.
- 6.Perna FM, A O, JF C, et al. The association of State law to physical education time association in US public schools. Am J Public Health. 2012;102(8):1594–1599. doi: 10.2105/AJPH.2011.300587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morgan PJ, Hansen V. Classroom teachers’ perceptions of the impact of barriers to teaching physical education on the quality of physical education programs. Res Quart Exerc Sport. 2008;79(4):506–517. doi: 10.1080/02701367.2008.10599517. [DOI] [PubMed] [Google Scholar]
- 8.Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Catalogue no. 82-003-XPE. Health Rep. 2011;(1):7–14. [PubMed]
- 9.O'Connor TM, Jago R, Baranowski T. Engaging parents to increase youth physical activity: a systematic review. Am J Prev Med. 2009;37:141–149. doi: 10.1016/j.amepre.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 10.Pate RR, Davis MG, Robinson TN, Stone EJ, McKenzie TL, Young JC. Promoting physical activity in children and youth: a leadership role for schools: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Physical Activity Committee) in collaboration with the Councils on Cardiovascular Disease in the Young and Cardiovascular Nursing. Circulation. 2006;114(11):1214–1224. doi: 10.1161/CIRCULATIONAHA.106.177052. [DOI] [PubMed] [Google Scholar]
- 11.Contreras, R. Obama pushes longer school days, shorter breaks. Washington Times. Sept 29, 2009. (Accessed May 24, 2015, at http://www.washingtontimes.com/news/2009/sep/29/obama-pushes-longer-school-days-shorter-breaks/?page=all).
- 12.Massachusetts Department of Elementary and Secondary Education. School Redesign: MA Expanded Learning Time (ELT). (Accessed May 24, 2015, at http://www.doe.mass.edu/redesign/elt/).
- 13.Sellgren K. Budget sets out academies plan and longer school day. British Broadcasting Corporation March 16, 2016. (Accessed April 15, 2016, at http://www.bbc.com/news/education-35815023).
- 14.Singh A, Uijtdewilligen L, Twisk JW, van Mechelen W, Chinapaw MJ. Physical activity and performance at school: a systematic review of the literature including a methodological quality assessment. Arch Pediat Adol Med. 2012;166(1):49–55. doi: 10.1001/archpediatrics.2011.716. [DOI] [PubMed] [Google Scholar]
- 15.Faulkner G, Reeves C. Primary school student teachers’ physical self-perceptions and attitudes toward teaching physical education. J Teach Phys Educ. 2000;19:311–324. doi: 10.1123/jtpe.19.3.311. [DOI] [Google Scholar]
- 16.Ryan RM, Deci EL. An overview of self-determination theory. In: Deci EL, Ryan RM, editors. Handbook of self-determination research. University of Rochester Press: Rochester (NY); 2002. pp. 3–33. [Google Scholar]
- 17.Cheon SH, Reeve J, Moon IS. Experimentally based, longitudinally designed, teacher-focused intervention to help physical education teachers be more autonomy supportive toward their students. J Sport Exerc Psychol. 2012;34(3):365–396. doi: 10.1123/jsep.34.3.365. [DOI] [PubMed] [Google Scholar]
- 18.Telama R, Yang X, Viikari J, Välimäki I, Wanne O, Raitakari O. Physical activity from childhood to adulthood: a 21-year tracking study. Am J Prev Med. 2005;28(3):267–273. doi: 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. Can Med Assoc J. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carlson, S. A., Fulton, J. E., Pratt, M., et al. (2014). Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis, 57(4), 315–323. doi:10.1016/j.pcad.2014.08.002. [DOI] [PMC free article] [PubMed]
- 21.Messick S. Validity of psychological assessment: validation of inferences from persons’ responses and performances as scientific inquiry into score meaning. Am Psychol. 1995;50:741–749. doi: 10.1037/0003-066X.50.9.741. [DOI] [Google Scholar]
- 22.Schwartz B. Why we work. NY: Simon and Schuster; 2015. [Google Scholar]