Abstract
“First-trial effect” characterizes the rapid adaptive behavior that changes the performance outcome (from fall to non-fall) after merely a single exposure to postural disturbance. The purpose of this study was to investigate how long the first-trial effect could last. Seventy-five (≥ 65 years) community-dwelling older adults, who were protected by an overhead full body harness system, were retested for a single slip 6–12 months after their initial exposure to a single gait-slip. Subjects’ body kinematics that was used to compute their proactive (feedforward) and reactive (feedback) control of stability was recorded by an eight-camera motion analysis system. We found the laboratory falls of subjects on their retest slip were significantly lower than that on the novel initial slip, and the reactive stability of these subjects was also significantly improved. However, the proactive stability of subjects remains unchanged between their initial slip and retest slip. The fall rates and stability control had no difference among the 6-, 9-, and 12-month retest groups, which indicated a maximum retention on 12 months after a single slip in the laboratory. These results highlighted the importance of the “first-trial effect” and suggested that perturbation training is effective for fall prevention, with lower trial doses for a long period (up to 1 year). Therefore, single slip training might benefit those older adults who could not tolerate larger doses in reality.
Keywords: Perturbation training, Motor memory, Stability, Adaptive control
Introduction
Falls could be precipitated by both intrinsic (physiologic origin) and extrinsic (environmental or other hazards) factors (Currie 2008). Falling is a common cause of injury and death (Hayes et al. 1996; Morley 2002), even for those healthiest and most active older adults (Rubenstein 2006). Intervention paradigms that can inoculate older adults against falls would be highly desirable.
Exercises aimed at increasing one’s strength and balance has been shown effective (Lord et al. 1995; Wolf et al. 1996). Recently, perturbation training (Parijat and Lockhart 2012; Pai et al. 2014a) has also emerged as an alternative approach to harness and improve a person’s natural responses in everyday living (Pai et al. 2014a). In perturbation training, the external factor (slip or trip for example) disrupts the regular gait pattern in locomotion and alters the relationship between one’s center-of-mass (COM) and base-of-support (BOS). The perturbation-induced kinematic error stimulates the central nervous system (CNS) to make adaptive improvements to regain balance from the destabilization (Pai et al. 2014b). This process is probably akin to the “learning from falling” observed among toddlers in early childhood (Joh and Adolph 2006), which indicates humans can learn implicitly to resist falls from physically experiencing falls. In other words, the CNS can better internalize and represent the error-correction pathway through repeated exposures. The formation of such representation can shift the reliance from online reactive (feedback) control to a predicable proactive (feedforward) control (Atkeson 1989; Owings et al. 2001; Pavol et al. 2004; Pai and Bhatt 2007). In the case of fall prevention, proactive control of stability represents a first line of defense, and reactive control of stability is the only other line of defense to prevent a fall (Pai et al. 2003).
Previous studies examining mechanisms of adaptation to overground slips have demonstrated that a feedforward change in proactive stability resulting from changes in step length, and in knee and foot angles at pre-slip touchdown can influence the reactive stability by altering the braking impulse which subsequently reduces the slip intensity (its displacement and velocity) (Bhatt et al. 2006b; Cham and Redfern 2001). Further within a single-session training, when the adaptive changes are reinforced by repeated, unannounced perturbations, such implicit learning (learned without instructions) can be retained over 6 or even 12 months (Pai et al. 2014b).
Remarkably, such kind of error-driven learning of postural control can take place immediately to yield the “first-trial effect,” which characterizes the rapid adaptive behavior that changes the performance outcome after merely a single exposure to postural disturbance (Adkin et al. 2000; Mcllroy and Maki 1995; Marigold and Patla 2002). Previous studies indicated that older adults can reduce their fall incidence by more than half with a mere single exposure to a real-life like slip (Pai et al. 2010). In this instance, more than half of the older adult fallers no longer fell after being exposed to a novel slip (Pai et al. 2010), resulting from the rapid improvements in the control of stability that can be accounted for by the recalibration and update on the limits of stability (Wang et al. 2011).
It can be questioned if such a potentially beneficial first-trial effect can be functionally meaningful and be retained over a substantial period of time, such as a winter season, 6 months, or even longer? Though the robust effects obtained from repeated exposure to perturbation in a single-session training already simplifies the need for multisession training (Pai et al. 2010; Pai et al. 2014a), it is highly desirable that we can further shorten the already highly efficient single-session training to a single exposure—a condition conducive to application among frail aging adults.
Thus, the purpose of the study was to determine the effective retention duration of any postural control improvement obtained from a single slip exposure to gait-slip among community-living older adults. A three-stage, sequential, initial-retest design (Pai et al. 2014b) was applied in the present study to test the hypothesis that these subjects would exhibit long-term improvements in both proactive and reactive control of the COM stability for 6, 9, or even 12 months in comparison to that displayed during the initial single exposure to an unannounced gait-slip. In addition, to understand how the COM stability was controlled at the whole body and at the segmental level, we would explore the secondary causal factors (such as relative COM position and its velocity, maximum BOS velocity, knee angle, and step length) contributing to the changes from the initial exposure to the retest.
Methods
Subjects
One hundred twenty community-dwelling older adults (≥ 65 years) were initially recruited from exercise or community centers, independent senior living facilities, the Aging Research Registry of the Buehler Center on Aging at Northwestern University, and affiliates of the City of Chicago Department on Aging. These people followed a standard protocol and criteria (Pai et al. 2010; Pai et al. 2014a; Pai et al. 2014b) to be screened for the current use of selected drugs that may alter their control of stability, cognitive impairment (Folstein Mini Mental Status Exam score < 25) (Folstein et al. 1975), or poor mobility (> 13.5 s on the Timed-Up-and-Go test) (Podsiadlo and Richardson 1991). All of them had given written informed consent in this study approved by the Institutional Review Board in the University of Illinois at Chicago.
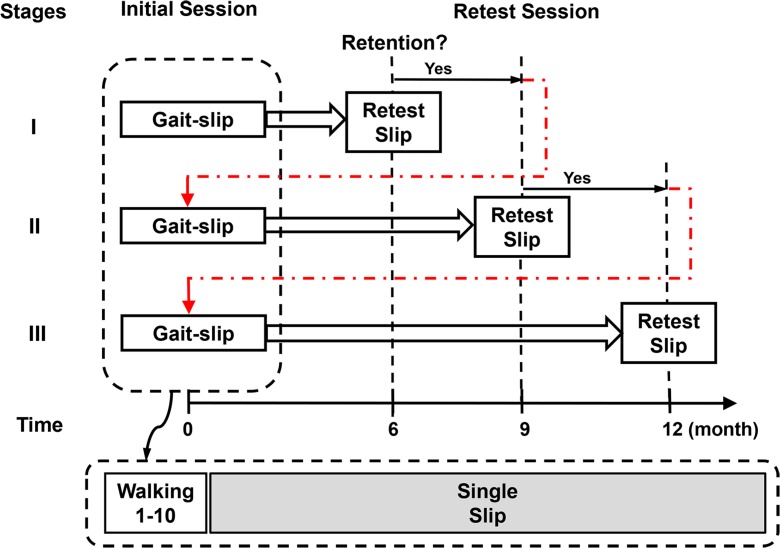
In order to eliminate any likelihood that the single slip introduced in a retest session in itself can produce a training effect for the subsequent retest, and hence contaminate the results, each subject only participated in one retest session. Therefore, a three-stage, sequential, initial-retest design (Fig. 1) similar to that of the previous study (Pai et al. 2014b) was applied. The retest for the group in the first stage was set at 6 months after their initial training, and the span of time for the retest of the subsequent two stages was contingent upon the results of the previous group. Whether or not the participants in the first or the second given stage successfully retained their training would then determine the timing for the retest in the next stage (the second or the third stage, respectively, Fig. 1). Successful retention observed in a given group was defined by the significant improvements in all of the outcome variables in the retest than results that were taken upon the novel slip trial. In the end, 25 of 49 in the first stage returned for their retest; 25 of 35 participants in the second and 25 of 36 subjects in the third stage returned. Thus, 75 out of those 120 subjects were included in the final analysis (Table 1).
Fig. 1.
Schematic of the three-stage, sequential, initial-retest design and protocol. The gait-slip design consisted of a single slip, which was unannounced
Table 1.
Means (standard deviations) and comparisons of subject demographics and training parameters for the three independent retest cohorts
| 6-month subgroup (n = 25) | 9-month subgroup (n = 25) | 12-month subgroup (n = 25) | p value | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 74.4 (5.8) | 73.0 (4.9) | 72.2 (6.3) | 0.39 |
| Gender (female) | 22 (88%) | 18 (72%) | 17 (68%) | 0.22 |
| Body mass index | 27.0 (4.6) | 27.4 (5.6) | 29.3 (6.6) | 0.33 |
| Perturbation training | ||||
| Falls upon novel slip | 10 (40%) | 12 (48%) | 12 (48%) | 0.81 |
| Proactive stability | −0.14 (0.04) | −0.16 (0.05) | −0.13 (0.04) | 0.10 |
| Reactive stability | −0.28 (0.15) | −0.31 (0.16) | −0.31 (0.18) | 0.83 |
| Falls upon retest slip | 6 (24%) | 7 (28%) | 9 (36%) | 0.65 |
| Proactive stability | −0.14 (0.06) | −0.14 (0.07) | −0.12 (0.08) | 0.38 |
| Reactive stability | −0.14 (0.20) | −0.14 (0.22) | −0.19 (0.17) | 0.62 |
Experimental setup
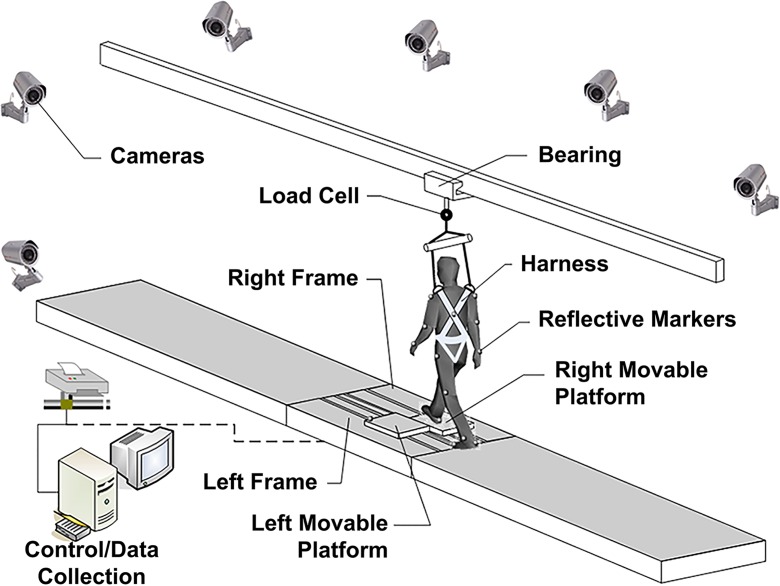
All the subjects were instructed to walk on a 7-meter walkway (Fig. 2) at their preferred speed and manner. Subjects were informed that they “may or may not be slipped” at any time and that, if a slip occurred, they should “try to recover” and “continue to walk.” None of them were told when, where, or how they might slip. All slips were unannounced in order to mimic real-life slips. The first slip was induced unexpectedly after ten walking trials. The initial session ended after this slip (Fig. 1). The retest session used an identical setup and protocol as the initial session. The slip was induced by releasing of a pair of side-by-side, low-friction, movable platforms embedded near the middle of the walkway (Fig. 2). The platforms were firmly locked in those first ten walking trials. During a slip trial, the released platforms could slide freely in the anteroposterior direction for up to 90 cm on the right and 75 cm on the left, but cannot move in the medial-lateral direction. Upon detection of a subject’s step by force plates (AMTI, Newton, MA) installed beneath the platforms, a computer-controlled triggering mechanism would release the electronic mechanical lock that held the platform firmly in place. A full-body harness, connected with shock-absorbing ropes to a load cell (Transcell Technology Inc., Buffalo Grove, IL) mounted to an overhead trolley on a track over the walkway, enabled subjects to walk freely while providing protection against body impact with the floor surface (Fig. 2). Kinematics was recorded by an eight-camera motion capture system (Motion Analysis Corporation, Santa Rosa, CA) and a full body marker set composed of 28 retro-reflective markers. Kinematics was sampled at 120 Hz and synchronized with the force plate and load cell data which were collected at 600 Hz.
Fig. 2.
The overground walkway with embedded movable platforms. The simulated slip was triggered by the release of two side-by-side low-friction moveable platforms
Outcome variables
The novel slip trial in the initial session and the retest slip trial were analyzed. The laboratory falls were recorded for the two slips. A fall was determined when the peak force recorded by the load cell in the harness system exceeded 30% of body weight (Yang and Pai 2011). Kinematic variables at right (leading) foot touchdown (RTD) can reveal training-induced alterations in proactive (feedforward) control immediately preceded slip onset in slip trials. The variables at left (recovery) foot lift off (LLO) and the following touchdown (LTD) can detect any perturbation training effect on the reactive (feedback) control after slip onset. The instants of RTD, LLO, and LTD were identified from the synchronized vertical ground reaction force (GRF) and motion analysis data. Four outcome variables (the stability, the relative COM position, the relative COM velocity, and the knee angle) were calculated at both RTD and LLO to investigate the change from novel to retest slips.
The COM state (that is, the COM position and velocity relative to the BOS) was used to measure a person’s instantaneous dynamic stability (Pai and Patton 1997; Pai and Iqbal 1999; Yang et al. 2007; Yang et al. 2008). First, full-body COM kinematics were calculated using a 13-segment rigid body model with gender-dependent segmental inertial parameters (de Leva 1996). Then, the COM position and velocity was expressed in its relative state using the rear edge of the BOS (i.e., the right heel) as the reference. The relative position was normalized by the foot length (lBOS), and the relative velocity was normalized by the quantity , where g is the gravitational acceleration and bh represents the body height. Finally, the COM stability was computed as the shortest distance from the COM motion state to the dynamic feasible stability boundary against backward loss of balance under slip conditions. When stability values are less than 0, a backward loss of balance must take place, and greater values mean greater stability against backward loss of balance (Pai et al. 2003). The maximum BOS velocity was determined as the maximum velocity of the right movable platform from RTD to lift off the leading foot. Other secondary causal factors were inspected on the lower limb joint angles and step length. Knee joint angle was the one formed by thigh segment and the extension line of leg segment with flexion as positive. The knee angle was calculated for the leading leg. The step length was normalized by body height and was represented by the anteroposterior distance from the heel of stance leg to the heel of swing leg at the time of touchdown of the swing leg. This made the forward direction always as positive which could then clearly differentiate a backward recovery step (the step after slip onset) with a regular walking (or forward recovery) step. The step length was calculated at the pre-slip instance of RTD and post-slip instance of LTD (recovery step) to reflect the proactive and reactive control respectively.
Statistical analysis
To test whether the laboratory fall outcome was different among three retest subgroups and between first and retest slips, the generalized estimating equation statistical model was used. Main effects were then resolved by chi-squared (χ 2) tests for the between subject factor (three retest groups: 6 vs. 9 vs. 12 months) and McNemar’s test for within subject factor (two time levels: initial vs. retest slip). To test whether the retention in proactive and reactive stability was different among three retest subgroups and between first and retest slips, a mixed factor ANOVA for repeated measures was used. Significant main effects were resolved by Tukey’s post hoc analysis for the between subject factor (three retest groups) and paired-sample t tests for the within-subject factor (two time levels). One-way ANOVA was used to compare the demographics including age, gender, and body mass index among three retest subgroups. Paired-sample t tests were used to determine the role of the knee angle, maximum BOS velocity, relative COM position, relative COM velocity, step length, and stability between the novel slip and retest slip (in the control of proactive and reactive control separately except the maximum BOS velocity). All statistical analyses were performed using SPSS 22 (IBM Corp, Armonk, NY).
Results
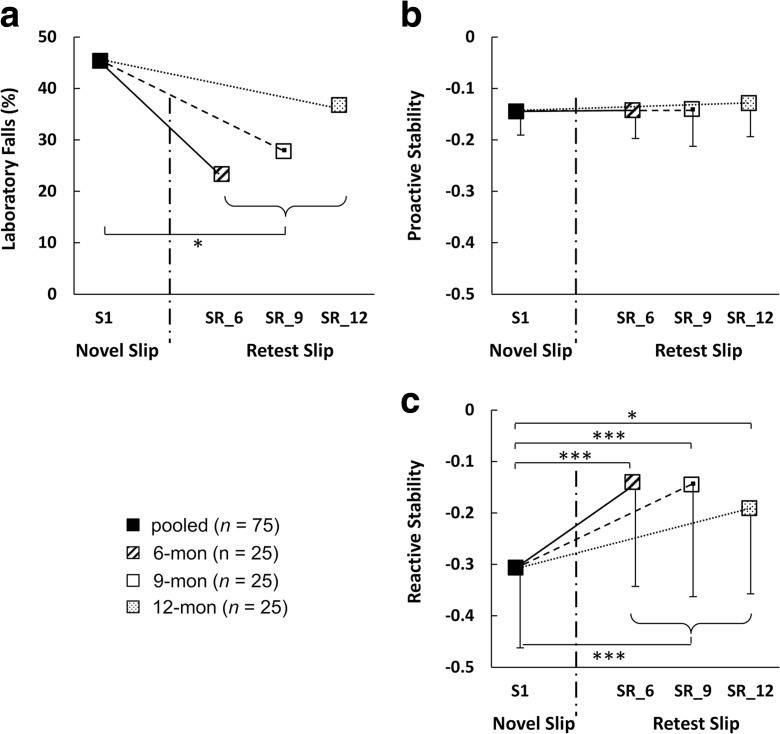
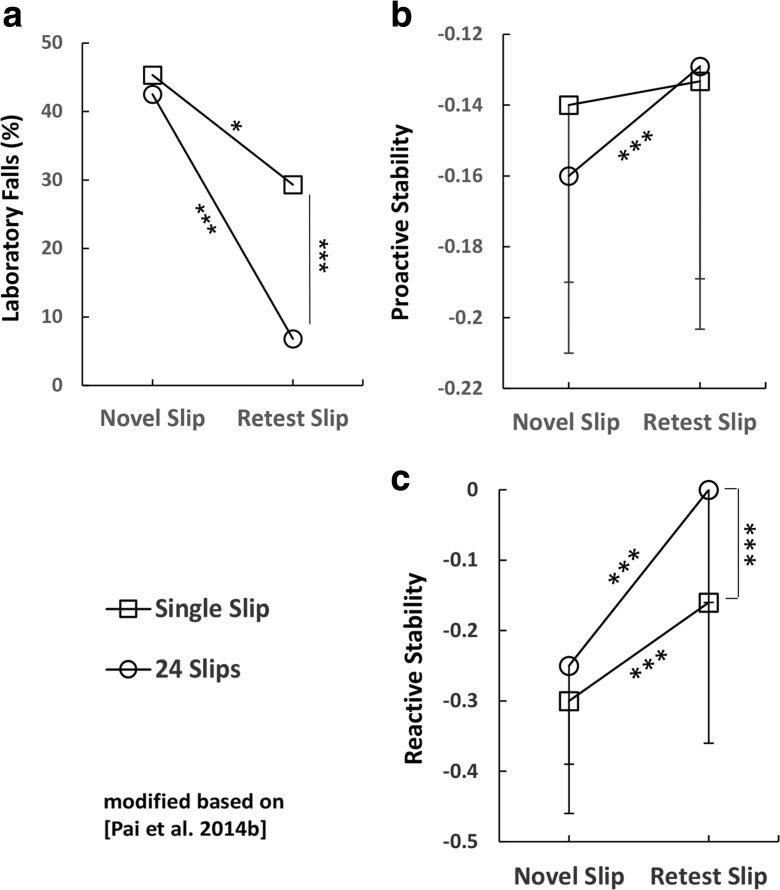
The laboratory fall incidence was significantly lower in the retest slip than the novel slip (main effect: χ 2 = 6, p = 0.014, Fig. 3a). However, no significant difference was found in laboratory fall incidence between the retest slip in each subgroup and the novel slip (p > 0.05 for all, Fig. 3a). The proactive stability was not significantly different between the novel and retest slips (main effect: F (1, 72) = 1.625, p = 0.207, Fig. 3b). The reactive stability was significantly higher in the retest slip compared to that in the novel slip (main effect: F (1, 72) = 35.18, p < 0.001, Fig. 3c). Post hoc paired t test also showed significant difference in reactive stability between the retest slip in each subgroup and the novel slip (Fig. 3c): 6-month subgroup (p < 0.001), 9-month subgroup (p < 0.001), and 12-month subgroup (p = 0.011). No significant difference was found among the three retest subgroups in laboratory falls, proactive and reactive stability (Fig. 3). The subjects in each cohort (6-, 9-, or 12-month retest stage) had comparable demographic characteristics, perturbation training performance in both initial and retest sessions (p > 0.05 for all, Table 1).
Fig. 3.
a Reduction in laboratory falls (%) and the retention in b proactive and c reactive control of stability. Measurements were taken from the novel slip (S1, filled squares) of the initial session and the retest slip, which took place 6 months (SR_6, diagonal squares), 9 months (SR_9, open squares), or 12 months (SR_12, dotted squares) after the initial session. For S1, the values were pooled from all three cohorts. *p < 0.05; ***p < 0.001
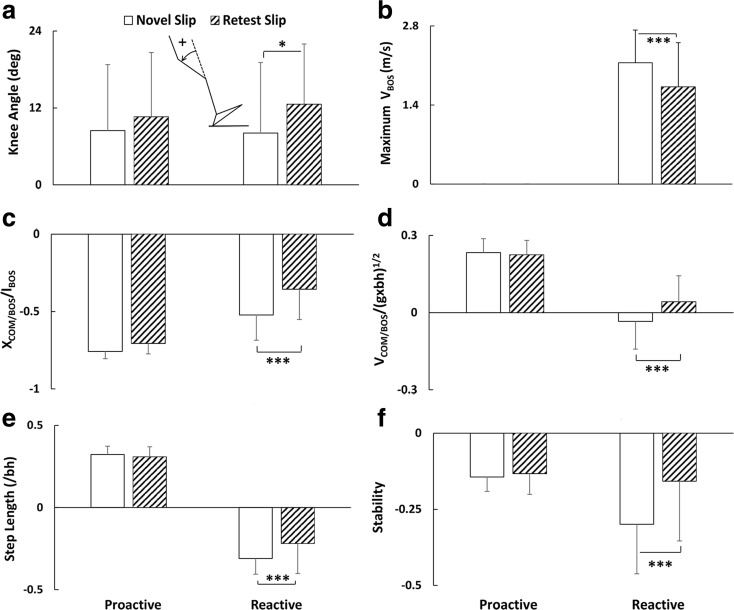
No significance was found in the knee angle, relative COM position, relative COM velocity, step length, and stability between the novel slip and retest slip in proactive control (Fig. 4). While in reactive control, the significant improvement in stability from the novel slip to the retest slip (p < 0.001, Fig. 4f) was accompanied by more flexion in the knee joint (p = 0.01, Fig. 4a), a decrease in the maximum BOS velocity (p < 0.001, Fig. 4b), a forward shift in the relative COM position (p < 0.001, Fig. 4c), an increase in the relative COM velocity (p < 0.001, Fig. 4d), and a decrease in the step length of the recovery step that landed posteriorly (p < 0.001, Fig. 4e).
Fig. 4.
Comparisons of the proactive and reactive a knee angle, b maximum BOS velocity, c relative COM position, d relative COM velocity, e step length, and f stability during the first and retest slips for all three cohorts. Knee joint angle was the one formed by thigh segment and the extension line of leg segment with flexion as positive. The knee angle was calculated for the leading leg. The step length was defined by the distance between left and right heels normalized by the body height with the forward direction as positive. *p < 0.05; ***p < 0.001
Discussion
In this study, our results demonstrated that older adults could successfully retain the learning obtained from a single slip to a maximum duration of 12 months to reduce the rate of laboratory-induced falls. This improvement obtained from the so-called first-trial effect could be extraordinarily valuable for older adults to improve their reactive (feedback) control of stability (Fig. 4f).
These older adults improved their reactive stability control (Fig. 4f) by a forward shift in the COM position (Fig. 4c) and/or an increase in the COM velocity (Fig. 4d) relative to the BOS (Pai and Patton 1997). The recovery step length was shortened (Fig. 4e) resulting in the modification of the COM position (Fig. 4c). The increased knee flexion on the leading foot (Fig. 4a) has been found to be associated with subsequent reduction of the peak slip velocity (maximum BOS velocity, Fig. 4b) and increase of the relative COM velocity (Fig. 4d) (Bhatt et al. 2006b; Cham and Redfern 2001).
Because traditional balance training paradigms usually require multiple (more than two) sessions over weeks or months to obtain sufficient training effect (Rubenstein and Josephson 2006; Shumway-Cook et al. 2007; Tinetti et al. 1994; Wolf et al. 2003), the first-trial effect emerged from perturbation training becomes especially noteworthy (Bhatt et al. 2005; Mansfield et al. 2007; Pavol et al. 2004). Unlike traditional training that focuses on enhancing volitional and self-motivated performance, perturbation training forces the CNS to react to a sudden alteration of the environment. Such adaptation happens quickly after the novel perturbation, which is called the first-trial effect (Adkin et al. 2000; Mcllroy and Maki 1995; Marigold and Patla 2002; Pai et al. 2003; Pai et al. 2010), a process during which the CNS proportionately matches corrective responses with the motor errors resulting from a slip perturbation. We reported that most subjects who fell in a novel trial were often able to rapidly avoid another fall in the second exposure (Pai et al. 2003; Pai et al. 2010). Such a quick learning effect was acquired probably by the update and recalibration of the internal representation of the stability limits, rather than by the alteration of a person’s physical conditions, such as strength, flexibility, or agility (Wang et al. 2011). Thus, the control of stability would be recalled when identical disturbance arises many months later.
While the improvements in the control of stability achieved after a single exposure were significant and robust that can be retained after 12 months, they were only a fraction of those that can be achieved after repeated exposure with standard block-and-mixed design for motor training (Fig. 5c). In the laboratory test conducted 6–12 months later, such improvements made after the single exposure indeed resulted in a significant reduction of the rate of falls (Fig. 3a). Nevertheless, such reduction was still far inferior to the reduction achieved following the single session of repeated slips (Fig. 5a). For example, with only one slip, the reduction in laboratory falls (reduced by only 16% from 45.3% on novel slip to 29.3% on the retest) was only half of that following the repeated slips (reduced by 35.7% from 42.5% on novel slip to 6.8% on the retest, Fig. 5a). The single slip perturbation also could not significantly improve the proactive control of stability (Figs. 3b and 5b), suggesting that the CNS was not yet to get sufficient incentive to modify regular gait pattern after merely a single exposure to disturbance. The scale in the reactive changes was five times greater than the proactive ones (cf. the scale in Fig. 5b, c) indicative of a prominent and perhaps dominant role played by the reactive response.
Fig. 5.
a Laboratory falls (%), b proactive stability, and c reactive stability during the novel slip and retest slip for single slip group (open squares) and 24 slips group (open circles). The scale in c is five times of the scale in b. *p < 0.05; ***p < 0.001
Clearly, these differences exhibited in laboratory were associated with, and may even account for the differences in the reduction of falls in everyday living, which requires the carryover of the laboratory learned effects to real world. The generalization of slip-perturbation adaptation has been observed after repeated slips on moveable platform and carried over to novel contexts such as vinyl (Bhatt and Pai 2009) and other tasks such as sit-to-stand slips (Wang et al. 2011) in laboratory environment. These results indicated the importance of training intensity in order to carry over the learned effects to the real world. One confirmation came recently where such 24 slips training paradigm was able to successfully reduce community-living older adults’ annual risk falls by more than 50% in the real world (Pai et al. 2014a). From this perspective, these results suggested that a person’s ability to generalize the learning obtained in the laboratory to everyday living is dictated by the amount of learning achieved in the laboratory. It is likely that the improvements must exceed certain threshold, below which this generalization (carryover) may not materialize.
Therefore, repeated-slip training sufficiently assured an improvement of proactive and reactive stability above the threshold that can significantly reduce not only the likelihood of laboratory falls but also the risk of falls in these subjects everyday living 12 months after this single-session intervention (Pai et al. 2014a). The better performance in repeated-slip training group could be attributed to a greater dosage induced overlearning (Bhatt et al. 2006a; Hart et al. 1997; Markowitsch et al. 1985; Pai et al. 2014b). However, training strategies need to compromise the practical needs. For example, the ideal training programs for those older adults who may lack the physical capacity to undergo the repeated slips should also be accessible. Fortunately, stability measurements are so sensitive that they can still detect and quantify the subpar improvements resulting from the single-trial effect, while on a whole such improvements still could not be sufficiently robust to reach the necessary level in order to reduce the likelihood of falls in real-life daily living (reduced only by 17% from 39 to 32%, p > 0.05) (Pai et al. 2014a) as the intensified 24 slips did (reduced by 56% from 34% pre-training to 15% post-training, p < 0.01) (Pai et al. 2014a).
This study has limitations. The older adults in this study were healthy ones without cognitive and/or balance control problems. Future studies are needed to investigate the effect of perturbation training on participants who were most vulnerable to falls (i.e., patients who are frail or cognitively impaired). Also, we did not quantify but only assumed that there was learning effect immediately after the single slip exposure. Precisely because of this single-trial effect, it is difficult to directly detect the immediate training effect as well as its retention. Any repeated trial (i.e., the second slip in this case), whether it is conducted on the same day or months later during the retest, is highly likely to produce its own training effect. That presents an insurmountable obstacle for applying a repeated-measures design. In the present study, this limitation that we chose to investigate the retention without being able to quantify the same person’s actual immediate learning effect or quantify the same person’s memory decay over 6, 9, and 12 months is a reflection of this dilemma. However, should the retest slip induce any effect, it would affect all three groups equivalently given the experimental design of this study.
In conclusion, undergoing perturbation training might benefit a broad population of older adults to induce long-term retention of fall resisting skills, and the amount of gain might depend on the dosage of training.
Acknowledgments
This study was supported by the National Institutes of Health (RO1-AG029616, RO1-AG044364). The authors would like to thank Dr. Edward Wang for providing consultation in statistical analysis.
References
- Adkin AL, Frank JS, Carpenter MG, Peysar GW. Postural control is scaled to level of postural threat. Gait Posture. 2000;12:87–93. doi: 10.1016/S0966-6362(00)00057-6. [DOI] [PubMed] [Google Scholar]
- Atkeson CG. Learning arm kinematics and dynamics. Annu Rev Neurosci. 1989;12:157–183. doi: 10.1146/annurev.ne.12.030189.001105. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Pai YC. Generalization of gait adaptation for fall prevention: from moveable platform to slippery floor. J Neurophysiol. 2009;101:948–957. doi: 10.1152/jn.91004.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatt T, Wang E, Pai YC. Retention of adaptive control over varying intervals: prevention of slip- induced backward balance loss during gait. J Neurophysiol. 2006;95:2913–2922. doi: 10.1152/jn.01211.2005. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Wening JD, Pai YC. Adaptive control of gait stability in reducing slip-related backward loss of balance. Exp Brain Res. 2006;170:61–73. doi: 10.1007/s00221-005-0189-5. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Wening JD, Pai YC. Influence of gait speed on stability: recovery from anterior slips and compensatory stepping. Gait Posture. 2005;21:146–156. doi: 10.1016/j.gaitpost.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Cham R, Redfern MS. Lower extremity corrective reactions to slip events. J Biomech. 2001;34:1439–1445. doi: 10.1016/S0021-9290(01)00116-6. [DOI] [PubMed] [Google Scholar]
- Currie L. Fall and injury prevention. Hughes R. Patient safety and quality: an evidence-based handbook for nurses. Rockville (MD) US: Agency for Healthcare Research and Quality; 2008. pp. 195–229. [PubMed] [Google Scholar]
- de Leva P. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. J Biomech. 1996;29:1223–1230. doi: 10.1016/0021-9290(95)00178-6. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Hart M, Poremba A, Gabriel M. The nomadic engram: overtraining eliminates the impairment of discriminative avoidance behavior produced by limbic thalamic lesions. Behav Brain Res. 1997;82:169–177. doi: 10.1016/S0166-4328(97)80986-2. [DOI] [PubMed] [Google Scholar]
- Hayes WC, Myers ER, Robinovitch SN, Van Den Kroonenberg A, Courtney AC, McMahon TA. Etiology and prevention of age-related hip fractures. Bone. 1996;18:77S–86S. doi: 10.1016/8756-3282(95)00383-5. [DOI] [PubMed] [Google Scholar]
- Joh AS, Adolph KE. Learning from falling. Child Dev. 2006;77:89–102. doi: 10.1111/j.1467-8624.2006.00858.x. [DOI] [PubMed] [Google Scholar]
- Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12-month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. J Am Geriatr Soc. 1995;43:1198–1206. doi: 10.1111/j.1532-5415.1995.tb07394.x. [DOI] [PubMed] [Google Scholar]
- Mansfield A, Peters AL, Liu BA, Maki BE. A perturbation-based balance training program for older adults: study protocol for a randomised controlled trial. BMC Geriatr. 2007;7:12. doi: 10.1186/1471-2318-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marigold DS, Patla AE. Strategies for dynamic stability during locomotion on a slippery surface: effects of prior experience and knowledge. J Neurophysiol. 2002;88:339–353. doi: 10.1152/jn.00691.2001. [DOI] [PubMed] [Google Scholar]
- Markowitsch HJ, Kessler J, Streicher M. Consequences of serial cortical, hippocampal, and thalamic lesions and of different lengths of overtraining on the acquisition and retention of learning tasks. Behav Neurosci. 1985;99:233–256. doi: 10.1037/0735-7044.99.2.233. [DOI] [PubMed] [Google Scholar]
- Mcllroy W, Maki B. Adaptive changes to compensatory stepping responses. Gait Posture. 1995;3:43–50. doi: 10.1016/0966-6362(95)90808-6. [DOI] [Google Scholar]
- Morley JE. A fall is a major event in the life of an older person. J Gerontol Ser A Biol Sci Med Sci. 2002;57:M492–M495. doi: 10.1093/gerona/57.8.M492. [DOI] [PubMed] [Google Scholar]
- Owings TM, Pavol MJ, Grabiner MD. Mechanisms of failed recovery following postural perturbations on a motorized treadmill mimic those associated with an actual forward trip. Clin Biomech (Bristol, Avon) 2001;16:813–819. doi: 10.1016/S0268-0033(01)00077-8. [DOI] [PubMed] [Google Scholar]
- Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Arch Phys Med Rehabil. 2010;91:452–459. doi: 10.1016/j.apmr.2009.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69:1586–1594. doi: 10.1093/gerona/glu087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Yang F, Bhatt T, Wang E (2014b) Learning from laboratory-induced falling: long-term motor retention among older adults. Age (Dordr) 36:9640–014–9640-5. Epub 2014 Mar 26. doi: 10.1007/s11357-014-9640-5 [DOI] [PMC free article] [PubMed]
- Pai YC, Bhatt TS. Repeated-slip training: an emerging paradigm for prevention of slip-related falls among older adults. Phys Ther. 2007;87:1478–1491. doi: 10.2522/ptj.20060326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Iqbal K. Simulated movement termination for balance recovery: can movement strategies be sought to maintain stability in the presence of slipping or forced sliding? J Biomech. 1999;32:779–786. doi: 10.1016/S0021-9290(99)00074-3. [DOI] [PubMed] [Google Scholar]
- Pai YC, Patton J. Center of mass velocity-position predictions for balance control. J Biomech. 1997;30:347–354. doi: 10.1016/S0021-9290(96)00165-0. [DOI] [PubMed] [Google Scholar]
- Pai YC, Wening JD, Runtz EF, Iqbal K, Pavol MJ. Role of feedforward control of movement stability in reducing slip-related balance loss and falls among older adults. J Neurophysiol. 2003;90:755–762. doi: 10.1152/jn.01118.2002. [DOI] [PubMed] [Google Scholar]
- Parijat P, Lockhart TE. Effects of moveable platform training in preventing slip-induced falls in older adults. Ann Biomed Eng. 2012;40:1111–1121. doi: 10.1007/s10439-011-0477-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavol MJ, Runtz EF, Pai YC. Young and older adults exhibit proactive and reactive adaptations to repeated slip exposure. J Gerontol A Biol Sci Med Sci. 2004;59:494–502. doi: 10.1093/gerona/59.5.M494. [DOI] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show. Med Clin North Am. 2006;90:807–824. doi: 10.1016/j.mcna.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Silver IF, LeMier M, York S, Cummings P, Koepsell TD. Effectiveness of a community-based multifactorial intervention on falls and fall risk factors in community-living older adults: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2007;62:1420–1427. doi: 10.1093/gerona/62.12.1420. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, Koch ML, Trainor K, Horwitz RI. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331:821–827. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- Wang TY, Bhatt T, Yang F, Pai YC. Generalization of motor adaptation to repeated-slip perturbation across tasks. Neuroscience. 2011;180:85–95. doi: 10.1016/j.neuroscience.2011.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and injuries: cooperative studies of intervention techniques. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Sattin RW, Kutner M, O’Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51:1693–1701. doi: 10.1046/j.1532-5415.2003.51552.x. [DOI] [PubMed] [Google Scholar]
- Yang F, Anderson FC, Pai YC. Predicted threshold against backward balance loss following a slip in gait. J Biomech. 2008;41:1823–1831. doi: 10.1016/j.jbiomech.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Anderson FC, Pai YC. Predicted threshold against backward balance loss in gait. J Biomech. 2007;40:804–811. doi: 10.1016/j.jbiomech.2006.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Pai YC. Automatic recognition of falls in gait-slip training: harness load cell based criteria. J Biomech. 2011;44:2243–2249. doi: 10.1016/j.jbiomech.2011.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]