Abstract
Fabry disease is a hereditary, X-linked lysosomal storage disease due to a deficiency of the alpha galactosidase A enzyme. Globotriaosylceramide accumulates in tissues and results in multiorgan dysfunction. The most common ocular finding in Fabry disease is cornea verticillata. Increase in conjunctival vascular tortuosity, and cataract may also be seen. Herein, we demonstrate the in vivo confocal microscopic findings of a genetically proven Fabry disease patient with a novel hemizygous R112L mutation in GLA gene.
Keywords: Cornea verticillata, Fabry disease, GLA gene, In vivo confocal microscopy, Mutation, R112L
Introduction
Fabry disease is a hereditary, X-linked disease caused by a deficiency in lysosomal hydrolase α-galactosidase A (α-Gal A). The disease begins in childhood and globotriaosylceramide accumulates in tissues. Overall rate of the disease is 1/40,000 to 1/117,000 in men. Women are heterozygous carriers, and may develop some symptoms.1
Globotriaosylceramide accumulates in the vascular endothelium of skin, kidneys, nervous system and heart, thereby leading to inflammation and fibrosis. Eventually this leads to multiorgan dysfunction and even death.2 Early manifestations of Fabry disease include cutaneous and peripheral neurological manifestations; cutaneous vascular lesions, such as angiokeratoma, angioma, and telangiectasia; lymphedema; sweating abnormalities; and acroparesthesis. Ophthalmologic findings are also important to clinically diagnose the disease.3
The most common ocular finding in Fabry disease is cornea verticillata. It is characterized by palm leaf pattern corneal deposits and is visible only by slit-lamp examination. Other common ocular findings are increased tortuosity and aneurysmal dilatation in conjunctival vessels.3
In vivo scanning laser confocal microscopy (IVCM) is an useful modern technique in diagnosis and follow-up of many corneal diseases. This noninvasive device provides high resolution and high contrast real-time images and gives details of ocular structures on the cellular level. It uses a monochrome laser radiation source; thus, chromatic aberrations may be eliminated and very sharp images may be obtained.4
Herein, we aimed to report IVCM findings of a patient with Fabry disease who was unaware of his illness until 69 years of age.
Case report
A 69 year old male was referred to Ophthalmology Department from Cardiology Department for Fabry disease investigation. Upon medical history it was learned that his elder brother died due to a heart attack a few months after being diagnosed as Fabry disease.
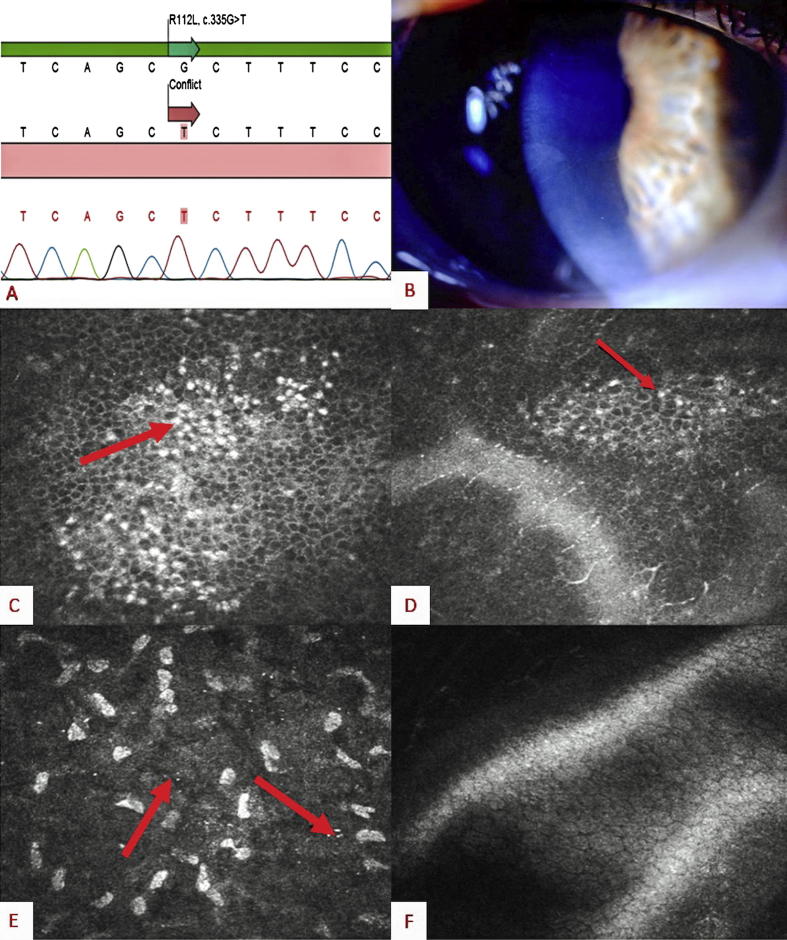
A complete cardiological examination including echocardiography and cardiac perfusion MRI revealed myocardial hypertrophy and hypokinesia at basal and midventricular levels – which were interpreted in favor of a storage disease. Medical Genetics Department confirmed the Fabry disease diagnose and found a novel hemizygous R112L mutation which was predicted to be deleterious by in silico analysis in GLA gene by sequencing (Fig. 1A). There was no acroparesthesia, hypohidrosis, angiokeratoma, and renal or cerebral involvement detected on the patient.
Fig. 1.
(A) Electropherogram of the novel R112L mutation. (B) Slit-lamp picture of cornea verticillata. (C and D) Intracellular inclusion in basal epithelium cells. (E) Microdots and impaired transparency of anterior stroma. (F) No involvement is detected in the endothelium.
A detailed ophthalmologic examination was performed. Best corrected visual acuity was 20/20 in both eyes and intraocular pressures were within normal limits. Slit-lamp examination indicated cornea verticillata in both eyes (Fig. 1B). No vascular tortuosity or anomaly was detected in conjunctival vessels. Cornea verticillata was grade 2 and grade 1, on the right and left eyes respectively, according to grading system suggested by Orlando et al.5 IVCM (HRT II Rostock Cornea Module, Heidelberg Engineering GmnH, Heidelberg, Germany) demonstrates that the corneal changes revealed hyperreflective intracellular inclusions in epithelial layer especially in basal epithelial cells (Fig. 1C and D). Also microdots were observed in stroma. No endothelial inclusions were detected (Fig. 1E and F).
Discussion
Fabry disease is a X-linked hereditary disease emerged from a lysosomal enzyme deficiency α-Gal A. The disease is usually seen in young males; however, the females might be asymptomatic carriers or severely affected. The onset is in childhood. Moderate forms of the disease have been defined in elderly individuals in whom an asymptomatic period might be seen up to 40 years of age. Until 2001, treatment in Fabry disease only aimed to alleviate symptoms. But after then, enzyme replacement therapy was provided and with this treatment symptomatic control was succeeded, and complication rate decreased. At the present time, suggestion is that the sooner the enzyme replacement therapy begins, the better results are achieved.3, 6 Herein, we present a 69 years old male who was unaware of his disease up to this age.
The hallmark of Fabry disease is ocular findings cornea verticillata being the most frequent one. By slit-lamp examination cornea verticillata is defined as white to brown colored, whorl-like opacities that generally do not impair vision. This corneal lesion is seen in 76.9% of female carriers and 73.1% of males according to Fabry Outcome Survey registry. These opacities arise from accumulation of glycosphingolipids in corneal layers.1, 3
However, cornea verticillata is not pathognomonic for Fabry disease. The most common cause of cornea verticillata is intake of amphiphilic drugs, especially amiodarone. As the verticillata appearance in these disorders is similar on slit-lamp examination, the exact cause cannot be discriminated with routine ophthalmologic examination alone. At this point, IVCM enables the ophthalmologist to demonstrate the nature of the corneal involvement that causes cornea verticillata. In Fabry patients diffuse and uniform intraepithelial inclusions, also intrastromal microdots may be seen as in our case. Endothelial microdots are not a feature of Fabry patients.3 In amiodarone induced cornea verticillata the deposits are more hyperreflectant with various dimensions and the pattern of the deposition is less organized. Moreover, contrary to Fabry induced cornea verticillata the accumulated material might be detected in subepithelial nerve plexus and the endothelium as well.7
In conclusion, cornea verticillata is a common finding of Fabry disease and usually does not affect vision. In young patients with cornea verticillata, Fabry disease can be considered as a preliminary diagnosis. However, it should be kept in mind that moderate form Fabry patients with cornea verticillata might as well stop by in older ages, and the discrimination of these corneal lesions might easily be made with IVCM.
Financial disclosure
None.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Sodi A., Ioannidis A.S., Mehta A., Davey C., Beck M., Pitz S. Ocular manifestations of Fabry's disease: data from the Fabry Outcome Survey. Br J Ophthalmol. 2007 February;91:210–214. doi: 10.1136/bjo.2006.100602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuttolomondo A., Pecoraro R., Simonetta I., Miceli S., Pinto A., Licata G. Anderson-Fabry disease: a multiorgan disease. Curr Pharm Des. 2013;19:5974–5996. doi: 10.2174/13816128113199990352. [DOI] [PubMed] [Google Scholar]
- 3.Falke K., Buttner A., Schittkowski M., Stachs O., Kraak R., Zhivov A. The microstructure of cornea verticillata in Fabry disease and amiodarone-induced keratopathy: a confocal laser-scanning microscopy study. Graefes Arch Clin Exp Ophthalmol. 2009 April;247:523–534. doi: 10.1007/s00417-008-0962-9. [DOI] [PubMed] [Google Scholar]
- 4.Bochert R., Zhivov A., Kraak R., Stave J., Guthoff R.F. Contribution to comprehension of image formation in confocal microscopy of cornea with Rostock cornea module. Br J Ophthalmol. 2005 October;89:1351–1355. doi: 10.1136/bjo.2004.063743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orlando R.G., Dangel M.E., Schaal S.F. Clinical experience and grading of amiodarone keratopathy. Ophthalmology. 1984 October;91:1184–1187. doi: 10.1016/s0161-6420(84)34165-3. [DOI] [PubMed] [Google Scholar]
- 6.Yonamine F.Y., Arantes T.E., Muccioli C. Fabry disease – importance of screening in cornea verticillata: case report. Arq Bras Oftalmol. 2011;74:447–448. doi: 10.1590/s0004-27492011000600014. November-December. [DOI] [PubMed] [Google Scholar]
- 7.Wasielica-Poslednik J., Pfeiffer N., Reinke J., Pitz S. Confocal laser-scanning microscopy allows differentiation between Fabry disease and amiodarone-induced keratopathy. Graefes Arch Clin Exp Ophthalmol. 2011 November;249:1689–1696. doi: 10.1007/s00417-011-1726-5. [DOI] [PubMed] [Google Scholar]