Abstract
Introduction
Many studies have demonstrated that patients with bipolar disorder (BD) suffer from significant functional impairment, even during remission periods. This study aimed to assess the levels of overall functioning and specific areas of functioning in remitted patients with BD compared with those in healthy controls.
Methods
Eighty completely remitted patients with BD and 80 healthy controls were included in the study. The Bipolar Disorder Functioning Questionnaire (BDFQ), Young Mania Rating Scale, and Beck Depression Inventory were used.
Results
There were fewer married and employed cohorts in the BD group than in the control group. Compared with healthy controls, patients with BD exhibited a worse functioning in terms of intellectual and sexual functioning, feelings of stigmatization, social withdrawal, household relationships, relationships with friends, and participation in social activities. There was no difference between the groups in terms of emotional functioning, daily activities and hobbies, taking initiative and self-sufficiency, and occupation. The total BDFQ scores of patients were lower than those of healthy controls. A better functionality was observed in patients using only a mood stabilizer than in patients using three or more drugs.
Conclusion
Remarkably, remitted patients with BD tended to perform daily activities well when these activities were not in a social context. Stigma-oriented interpersonal approaches can be particularly beneficial for these patients.
Keywords: Bipolar disorder, functioning, stigmatization, combination therapy
INTRODUCTION
Bipolar disorder (BD) causes substantial psychosocial morbidity by affecting the independent living and occupational and social activities of patients (1). MacQueen et al. (2) demonstrated that 30%–60 % of patients have psychosocial dysfunctions as measured by the impairment in employment and social functioning. Patients with BD suffer from significant functional impairment even during interepisode intervals and after recovery from an acute episode of illness (3,4,5,6,7). This is true even when the traditionally defined syndromal or clinical diagnoses are no longer met (8). Hence, recovery of patients with BD is multidimensional and should include symptomatic (remission) and functional recoveries. Symptomatic recovery is the resolution of symptoms, while functional recovery is the ability to return to an adequate level of functioning (9). In a prospective study conducted by Tohen et al. (10), the symptomatic recovery rate was 72%, while the functional recovery rate was 43% at 2 years after the first episode of mania. This is an indication that within a set of patients presenting with symptomatic remission, some patients continue to suffer from a considerable degree of impairment (7).
Risk factors associated with poor functioning in patients with BD have been widely studied. The most reported predictors of functional impairment are psychiatric and medical comorbidity and persistent interepisode subsyndromal symptoms (11). In particular, interepisode subsyndromal depressive symptoms are a consistent predictor of poor functioning in most studies (1,12,13,14,15). A 20-year prospective study revealed that depressive and manic/hypomanic symptoms are equally disabling in psychosocial functioning; moreover, subsyndromal depressive symptoms, but not subsyndromal manic or hypomanic symptoms, are associated with significant psychosocial impairment in patients with BD (16). The relationship between functioning and medication is also worth considering. While medication improves functioning by healing the disease, its side effects, particularly regarding cognition, have a negative impact on functioning in patients with BD (17).
Studies on functioning in patients with BD are more likely to assess the risk factors of poor functioning and generally assess “overall functioning.” This causes poor evaluation of specific functioning areas (18). Furthermore, most studies have examined the current mood symptoms of patients and may be biased toward a poor outcome (19). The main aim of this study was to assess the levels of overall functioning and specific areas of functioning in a remitted BD population compare with those in healthy controls using a comprehensive questionnaire. Furthermore, the relationship between medication and functioning was investigated.
METHODS
Study Design
This study is a part of our ongoing research on the “Aspects of functionality in remitted bipolar patients.” Our previously published article, which is a part of this research, examined the predictors of functioning (12). Patients with a diagnosis of “bipolar disorder, complete remission” according to the Diagnostic and Statistical Manuel of Mental Disorders, fourth edition were included in the study. Patients with a diagnosis of mental retardation, chronic physical disease, substance use disorder, and pregnant or puerperant patients were excluded from the study. None of the patients underwent electro convulsive therapy in the last 2 months. Ninety-one patients were included in the study during a period of 4 months, and 11 were excluded (five patients declined to participate in the study, two did not complete the scales, one had alcohol abuse, and three had a chronic physical disease). Therefore, 80 patients were included the final assessment. The healthy controls included volunteers from the blood transfusion center of the institute. Volunteers were included if they had no history of psychiatric, neurological, and chronic physical diseases. Healthy individuals in the control group were matched (for every 10 individuals) for age, gender, and educational level to patients with BD in the BD group. Informed consent was obtained from the patients and healthy controls. The ethical committee approval was obtained from the Ethical Committee of the Haydarpaşa Numune Training and Research Hospital.
Materials
Demographic and clinical information form
This form contained information regarding age, gender, education level, marital status, occupation, and recently used drugs.
Bipolar Disorder Functioning Questionnaire (BDFQ)
It was developed by the Scientific Section for Mood Disorders of the Psychiatric Association of Turkey (20). The questionnaire contains 58 items and 11 subscales: emotional functioning, intellectual functioning, sexual functioning, feelings of stigmatization, social withdrawal, household relationships, relationships with friends, participation in social activities, daily activities and hobbies, taking initiative, self-sufficiency, and occupation. In the reliability analyses, after excluding six items with low reliability coefficients, Cronbach’s alpha coefficient was calculated to be 0.91. The item-total scale correlations were between 0.22 and 0.86. In the test–retest reliability analyses, the correlation between the two ratings was high (r=0.82, p<0.0001). In the validity analyses, 13 factors were obtained, representing 65.1% of the total variance in the exploratory factor analysis. BDFQ revealed significantly negative correlation with HAM-D (r=−0.541, p<0.0001) and YMRS (r=−0.365, p<0.0001) and discriminated patients (mean score=111.8±15.2) from healthy controls (mean score=121.4±10.4) (t=−2.300, p=0.038). With the six items excluded, it is suggested that the 52-item BDFQ is a reliable and valid instrument in assessing functioning in patients with BD (20).
Beck Depression Inventory (BDI)
BDI (21) was adapted by Hisli (22) for use in Turkey and was reported to be reliable and valid. BDI contains 21 items, each of which has four potential answers. Respondents choose the most appropriate answer for their condition during the last 7 days. Each item is scored from 0 to 3; higher scores indicate more severe depression.
Young Mania Rating Scale (YMRS)
YMRS comprises 11 items, each of which measures five severity levels (from mild to serious symptoms) of the core symptoms in the manic phase of BD (23). The internal consistency coefficient was found to be 0.79 in the Turkish reliability and validity study of the scale (24). The consensus level of the researchers on the items of YMRS ranged between 63.3% and 95.5%, with κ values of 0.114–0.849.
Statistical Analyses
The statistical analyses were assessed using the Statistical Package for the Social Sciences (SPSS Inc; Chicago, IL, USA) 16.0 program. The independent sample t test was used for comparing the continuous variables. The chi-square test was used for comparing the categorical variables. The Pearson chi-square, continuity correction, or Fisher’s exact test was used if required. One way ANOVA was used for multiple group comparisons. The post hoc Tukey test was used to demonstrate the differences between groups. Statistical significance was accepted as p<0.05.
RESULTS
The comparison of demographic and clinical variables between the patients and healthy controls is presented in Table 1. There was no statistically significant difference between the groups in terms of age, sex, and duration of education. There were fewer married and employed individuals in the BD group than in the control group. Subthreshold depressive and manic symptoms were more frequent in patients with BD.
Table 1.
Comparison of demographic and clinical variables between patients with BD and healthy controls
| BD group (n=80) | Control group (n=80) | Statistics | |
|---|---|---|---|
| Age (years, mean±SD) | 37.57±10.37 | 35.73±7.67 | t test p=0.20 |
| Sex (n, %) | |||
| Male | 15 (18.7%) | 20 (25%) | χ2 test |
| Female | 65 (81.3%) | 60 (75%) | p=0.44 |
| Duration of education (years, mean±SD) | 8.65±3.52 | 9.63±3.26 | t test p=0.07 |
| Marital status | |||
| Married | 38 (22.5%) | 54 (67.5%) | χ2 test |
| Not married | 42 (77.5%) | 26 (32.5%) | p=0.01 |
| Occupation | |||
| Employed | 21 (26.3%) | 57 (71.3%) | χ2 test |
| Unemployed | 59 (73.7%) | 23 (28.7%) | p<0.01 |
| BDI (mean±SD) | 9.20±7.88 | 5.31±6.96 | t test p<0.01 |
| YMRS (mean±SD) | 0.70±2.07 | 0.11±0.39 | t test p=0.01 |
BD: Bipolar Disorder; SD: standard deviation; BDI: Beck Depression Inventory; YMRS: Young Mania Rating Scale
The comparison of total and subscale scores of BDFQ between the patients with BD and healthy controls is presented in Figure 1. Compared with healthy controls, patients with BD exhibited worse functioning in terms of intellectual and sexual functioning, feelings of stigmatization, social withdrawal, household relationships, relationships with friends, and participation in social activities. There was no difference between the groups in terms of emotional functioning, daily activities and hobbies, taking initiative and self-sufficiency, and occupation. The total BDFQ scores of patients with BD were lower than those of healthy controls.
Figure 1.
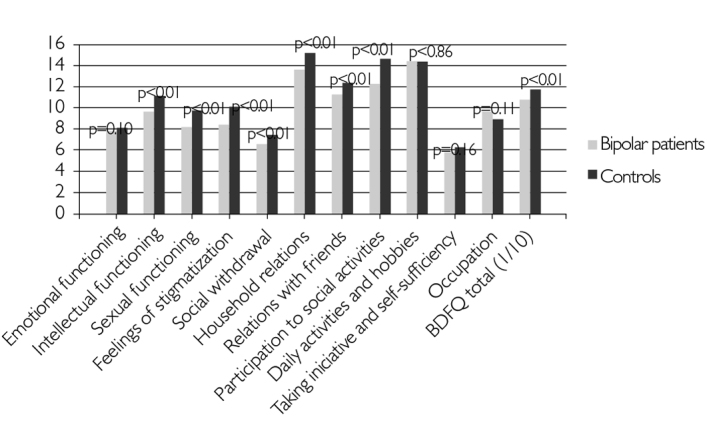
Comparison of BDFQ scores between patients with BD and healthy controls
BD: Bipolar Disorder; BDFQ: Bipolar Disorder Functioning Questionnaire
Furthermore, we assessed the relationship between medication and functioning in the BD group (Table 2). We divided the BD group in terms of their most used drug types; 14 (17.5%) patients were using only a mood stabilizer, 34 (42.5%) were using a mood stabilizer along with an antipsychotic drug, and 24 (30%) were using three or more drugs (any of the mood stabilizers, antipsychotic drugs, or antidepressant drugs). A total of eight patients from the three drug group [an antidepressant drug and an antipsychotic drug (n=2), a mood stabilizer and an antidepressant drug (n=3), and only an antipsychotic drug (n=3)] were excluded from the assessment as these groups were small in number.
Table 2.
Relationship between medication group and functioning among patients with bipolar disorder
| 1 (n=14) | 2 (n=34) | 3 (n=24) | Statistics | |
|---|---|---|---|---|
| BDFQ total | 112.24±12.71 | 110.79±10.09 | 101.71±16.89 | One way ANOVA, df=71, F=4.317, p=0.02 Post hoc Tukey analysis: 1=2 (p=0.94) 1>3 (p=0.02) 2=3 (p=0.13) |
1. Patients using only a mood stabilizer.
2. Patients using a mood stabilizer and an antipsychotic.
3. Patients using three or more drugs (any of mood stabilizers, antipsychotic drugs, or antidepressant drugs). BDFQ: Bipolar Disorder Functioning Questionnaire
We found that there were differences between these three drug groups in terms of total functioning (total BDFQ score). Post hoc analyses basically revealed that patients using only a mood stabilizer had better functioning than patients using three or more drugs (Table 2).
DISCUSSION
This study mainly focused on investigating the deteriorated areas of functioning in patients with BD compared with healthy controls. BDFQ is a comprehensive questionnaire that assesses functionality among 11 domains in remitted patients with BP. Furthermore, in our opinion, investigating functionality in a remitted population provides more reliable information than investigating patients in acute states. The study results are discussed in three parts: demographic and clinical variables and functioning, specific domains of functioning, and relationship between medication and functioning.
Demographic and Clinical Variables and Functioning
The patient and control groups were matched for age, gender, and education level to compare between similar groups in terms of demographical and sociocultural aspects. In this study, as in most studies, we found that fewer patients with BD were married (7,16,18) and employed (25,26,27) compared with healthy controls. In this study, the proportion of unemployed patients with BD (73%) was striking compared with healthy controls (29%). Moreover, the proportion of unemployed patients varies between 50% and 70% in most studies (25,27,28).
Specific Domains of Functioning
Findings regarding specific domains of functioning are listed in Table 3.
Table 3.
List of findings for specific domains of functioning
| Patients with BD showed worse functioning | No significant difference between patients with BD and healthy controls |
| Intellectual functioning | Emotional functioning |
| Sexual functioning | Daily activities and hobbies |
| Feelings of stigmatization | Taking initiative and self sufficiency |
| Social withdrawal | Occupation |
| Household relationships | |
| Relationships with friends | |
| Participation in social activities | |
| Total functioning |
BD: Bipolar Disorder
As expected, in this study, the total functioning scores of patients with BD were significantly lower than those of healthy controls; however, this difference was not consistent in all subscales.
Intellectual functioning mainly refers to attention, concentration, and memory functions in this study. Cognitive functioning has been widely studied in patients with BD. Two large meta-analyses demonstrated the considerable differences between patients with BD and healthy controls (29,30). Another meta-analysis revealed a strong relationship between cognitive deficits and functioning (31). Our finding of deteriorated intellectual functioning in patients with BD was consistent with these studies.
There are few studies on the sexual functioning among euthymic patients with BD in the literature. In this study, the sexual functioning scores (representing mainly sexual desire, arousal, and satisfaction) were lower in patients with BD than in healthy controls. Dell’Osso et al. (32) revealed that impairment in sexual desire, excitement, and ability to achieve orgasm was significantly more common in patients with mood disorders than in healthy controls. Another study conducted by Zuncheddu and Carpiniello (33) revealed that fewer sexual fantasies and less sexual intercourse, desire, pleasure, and satisfaction were observed in euthymic patients with BD than in healthy controls. The consequences of illness (e.g., having less sexual intercourse) should be accounted together with the known adverse effects of medication (e.g., decrease in sexual desire) when considering sexual disability in patients with BD.
Feelings of stigmatization and the relationship of these feelings with functioning have been attracting attention in recent years. Studies have demonstrated a correlation between stigma and poor functioning in patients with BD (34,35). Moreover, our previous study revealed that stigma played a core role in predicting poor functioning in patients with BD (12). Another study conducted by Sarısoy et al. (36) demonstrated that internalized stigma was correlated with intimate relationships in patients with BD. It can be interpreted that studying the thoughts of patients regarding the manner in which they experience their illness is important for achieving better functioning.
As expected, domains of functioning reflecting family and social functioning (social withdrawal, household relationships, relationships with friends, and participation in social activities) were found to be worse in patients with BD when compared to controls. Interestingly, there was no difference between the groups in terms of daily activities/hobbies and taking initiative/self-sufficiency. These two findings appear to be in conflict. However, the items of daily activities/hobbies and taking initiative/self-sufficiency mostly examine individually performed activities (e.g., paying bills, shopping, applying for a job) rather than socially performed activities. This is a remarkable finding of this study, reflecting that remitted patients with BD tend to perform daily activities well when these activities are not in a social context. This finding can also be interpreted as an unfavorable result of self-stigmatization. Self-stigmatization may embarrass patients when performing socially. To the best of our knowledge, this is the first study distinguishing social and individual functioning by discovering such a distinction in daily life conditions in patients with BD.
It was surprising that there was no difference between the groups in emotional and occupational functioning. Emotional functioning mainly expresses emotional reactions to daily circumstances and how the patient finds his/her emotional participation. Occupational functioning mainly examines how the patient finds himself/herself when working (recently or in the past). These two findings were unexpected because most patients with BD complain of diminished emotions and occupational performance.
Medication and Functioning
The main finding regarding medication was that bipolar patients using only a mood stabilizer have better functionality than patients using 3 or more drugs. Furthermore, total functioning scores were found to decrease as the number of drugs increased, although this finding was not statistically significant. This finding is consistent with the findings of the study conducted by Martinez-Aran et al. (37), which revealed that number of drugs was related with functional impairment in patients with BD. Another study found significant differences in overall functioning between drug groups in patients with BD. According to this longitudinal, open-label study, the lowest impairment was found among patients on lithium monotherapy, followed by untreated individuals, those on antipsychotic monotherapy, and those on combination therapy (lithium and antipsychotic drugs) (38). In general, antipsychotics are estimated to be responsible for deteriorated functioning in terms of their unfavorable effects on cognition. In a study conducted by Arts et al. (17), it was found that the use of second-generation antipsychotics was associated with the largest negative effects on cognition, which were evident in the areas of motor speed and basic information processing. Although there is evidence for the unfavorable effect of the number of drugs on functioning, the deteriorated functioning should not be attributed only to the number of drugs. It is unclear whether the number of drugs has a direct impact on functioning or whether patients requiring multiple psychotropic drugs are clinically more severe than others.
Study Limitations
The cross-sectional design and the known limitations of self-perceived scales are the limitations of this study. The healthy controls may have performed a standardized evaluation in order to evaluate their current psychiatric, neurologic, and physical state. They were only evaluated using BDI and YMRS and asked if they had a psychiatric, neurological, and chronic physical problem currently or previously. In addition, there were significant differences between patients with BD and healthy controls in terms of BDI and YMRS scores, which might be considered while comparing these two groups; however, our main focus was to compare the remitted patients with the control group, so we disregarded this difference.
In conclusion, clinicians should not assume that patients with BD are sufficiently healed when they meet conventional “complete remission” criteria. Interepisode mild depressive symptoms are an important starting point leading to struggles with poor functioning. Clinicians may hesitate to prescribe antidepressant therapy in terms of precipitating a manic switch when a bipolar patient with depressive symptoms is consulted (1). The very low incidence of antidepressant use in our study is concordant with that opinion. Although medication can improve psychosocial functioning by ameliorating affective symptoms (39), the number of medications used should be considered in terms of its possible unfavorable effect on functioning.
Regarding the results of individual and social functioning in this study, psychosocial interventions, particularly in a context of interpersonal relationships and stigma, should be beneficial for patients with BD. With the aid of these interventions, patients can experience acceptance, appreciation, and meaningful interpersonal connections (40). Group psychoeducation (41) and interpersonal and social rhythm therapy (42) are models with evidence of favorable outcomes.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Kauer-Sant’Anna M, Bond DJ, Lam RW, Yatham LN. Functional outcomes in first-episode patients with bipolar disorder: a prospective study from the Systematic Treatment Optimization Program for Early Mania project. Compr Psychiat. 2009;50:1–8. doi: 10.1016/j.comppsych.2008.05.013. http://dx.doi.org/10.1016/j.comppsych.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 2.MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiat Scand. 2001;103:163–170. doi: 10.1034/j.1600-0447.2001.00059.x. http://dx.doi.org/10.1034/j.1600-0447.2001.00059.x. [DOI] [PubMed] [Google Scholar]
- 3.Goetz I, Tohen M, Reed C, Lorenzo M, Vieta E. Functional impairment in patients with mania: baseline results of the EMBLEM study. Bipolar Disord. 2007;9:45–52. doi: 10.1111/j.1399-5618.2007.00325.x. http://dx.doi.org/10.1111/j.1399-5618.2007.00325.x. [DOI] [PubMed] [Google Scholar]
- 4.Coryell W, Scheftner W, Keller M, Endicott J, Maser J, Klerman GL. The enduring psychosocial consequences of mania and depression. Am J Psychiat. 1993;150:720–727. doi: 10.1176/ajp.150.5.720. http://dx.doi.org/10.1176/ajp.150.5.720. [DOI] [PubMed] [Google Scholar]
- 5.Kasper SF. Living with bipolar disorder. Expert Rev Neurother. 2004;4:9–15. doi: 10.1586/14737175.4.6.S9. http://dx.doi.org/10.1586/14737175.4.6.S9. [DOI] [PubMed] [Google Scholar]
- 6.Robb JC, Cooke RG, Devins GM, Young LT, Joffe RT. Quality of life and lifestyle disruption in euthymic bipolar disorder. J Psychiat Res. 1997;31:509–517. doi: 10.1016/s0022-3956(97)00030-7. http://dx.doi.org/10.1016/S0022-3956(97)00030-7. [DOI] [PubMed] [Google Scholar]
- 7.Montoya A, Tohen M, Vieta E, Casillas M, Chacón F, Polavieja P, Gilaberte I. Functioning and symptomatic outcomes in patients with bipolar I disorder in syndromal remission: a 1-year, prospective, observational cohort study. J Affect Disorders. 2010;127:50–57. doi: 10.1016/j.jad.2010.04.026. http://dx.doi.org/10.1016/j.jad.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 8.Goodwin GM, Anderson I, Arango C, Bowden CL, Henry C, Mitchell PB, Nolen WA, Vieta E, Wittchen HU. ECNP consensus meeting. Bipolar depression. Eur Neuropsychopharm. 2008;18:535–549. doi: 10.1016/j.euroneuro.2008.03.003. http://dx.doi.org/10.1016/j.euroneuro.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Haro JM, Reed C, Gonzalez-Pinto A, Novick D, Bertsch J, Vieta E. 2-Year course of bipolar disorder type I patients in outpatient care: factors associated with remission and functional recovery. Eur Neuropsychopharm. 2011;21:287–293. doi: 10.1016/j.euroneuro.2010.08.001. http://dx.doi.org/10.1016/j.euroneuro.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 10.Tohen M, Zarate CA, Jr, Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, salvatore P, Baldessarini RJ. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiat. 2003;160:2099–2107. doi: 10.1176/appi.ajp.160.12.2099. http://dx.doi.org/10.1176/appi.ajp.160.12.2099. [DOI] [PubMed] [Google Scholar]
- 11.Keck PE. Long-term management strategies to achieve optimal function in patients with bipolar disorder. J Clin Psychiat. 2006;67:17. http://dx.doi.org/10.4088/JCP.1206e17. [PubMed] [Google Scholar]
- 12.Cerit C, Filizer A, Tural Ü, Tufan AE. Stigma: a core factor on predicting functionality in bipolar disorder. Compr Psychiat. 2012;53:484–489. doi: 10.1016/j.comppsych.2011.08.010. http://dx.doi.org/10.1016/j.comppsych.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Altshuler LL, Post RM, Black DO, Keck PE, Jr, Nolen WA, Frye MA, Suppes T, Grunze H, Kupka RW, Leverich GS, McElroy SL, Walden J, Mintz J. Subsyndromal depressive symptoms are associated with functional impairment in patients with bipolar disorder: results of a large, multisite study. J Clin Psychiat. 2006;67:1551–1560. doi: 10.4088/jcp.v67n1009. http://dx.doi.org/10.4088/JCP.v67n1009. [DOI] [PubMed] [Google Scholar]
- 14.Bonnín CM, Martínez-Arán A, Torrent C, Pacchiarotti I, Rosa AR, Franco C, Murru A, Sanchez-Moreno J, Vieta E. Clinical and neurocognitive predictors of functional outcome in bipolar euthymic patients: a long-term, follow-up study. J Affect Disorders. 2010;121:156–160. doi: 10.1016/j.jad.2009.05.014. http://dx.doi.org/10.1016/j.jad.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Gitlin MJ, Mintz J, Sokolski K, Hammen C, Altshuler LL. Subsyndromal depressive symptoms after symptomatic recovery from mania are associated with delayed functional recovery. J Clin Psychiat. 2011;72:692–697. doi: 10.4088/JCP.09m05291gre. http://dx.doi.org/10.4088/JCP.09m05291gre. [DOI] [PubMed] [Google Scholar]
- 16.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA, Coryell W, Maser JD, Keller MB. Psychosocial disability in the course of bipolar I and II disorders: a prospective, comparative, longitudinal study. Arch Gen Psychiat. 2005;62:1322–1330. doi: 10.1001/archpsyc.62.12.1322. http://dx.doi.org/10.1001/archpsyc.62.12.1322. [DOI] [PubMed] [Google Scholar]
- 17.Arts B, Jabben N, Krabbendam L, van Os J. A 2-year naturalistic study on cognitive functioning in bipolar disorder. Acta Psychiat Scand. 2011;123:190–205. doi: 10.1111/j.1600-0447.2010.01601.x. http://dx.doi.org/10.1111/j.1600-0447.2010.01601.x. [DOI] [PubMed] [Google Scholar]
- 18.MacQueen GM, Young LT, Robb JC, Marriott M, Cooke RG, Joffe RT. Effect of number of episodes on well being and functioning of patients with bipolar disorder. Acta Psychiat Scand. 2000;101:374–381. doi: 10.1034/j.1600-0447.2000.101005374.x. http://dx.doi.org/10.1034/j.1600-0447.2000.101005374.x. [DOI] [PubMed] [Google Scholar]
- 19.Rosa AR, Reinares M, Franco C, Comes M, Torrent C, Sánchez-Moreno J, Martínez-Arán A, Salamero M, Kapczinski F, Vieta E. Clinical predictors of functional outcome of bipolar patients in remission. Bipolar Disord. 2009;11:401–409. doi: 10.1111/j.1399-5618.2009.00698.x. http://dx.doi.org/10.1111/j.1399-5618.2009.00698.x. [DOI] [PubMed] [Google Scholar]
- 20.Aydemir Ö, Eren İ, Savaş H, Oğuzhanoğlu NK, Koçal N, Özgüven HD, Akkaya C, Devrim Başterzi A, Karlidağ R, Yenilmez C, Ozerdem A, Kora K, Tamam L, Gülseren S, Oral ET, Vahip S. Development of a Questionnaire to Assess Inter-Episode Functioning in Bipolar Disorder: Bipolar Disorder Functioning Questionnaire. Turk Psikiyatr Derg. 2007;18:344–352. [PubMed] [Google Scholar]
- 21.Beck AT. An inventory for measuring depression. Arch Gen Psychiat. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. http://dx.doi.org/10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 22.Hisli N. Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji Dergisi. 1989;7:3–13. [Google Scholar]
- 23.Young RC, Biggs JT, Ziegler, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Brit J Psychiat. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. http://dx.doi.org/10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 24.Karadağ F, Oral ET, Aran Yalçın F, Erten E. Young Mani Derecelendirme Ölçeğinin Türkiye’de geçerlik ve güvenilirliği. Turk Psikiyatr Derg. 2002;13:107–114. [PubMed] [Google Scholar]
- 25.Morriss R, Scott J, Paykel E, Bentall R, Hayhurst H, Johnson T. Social adjustment based on reported behaviour in bipolar affective disorder. Bipolar Disord. 2007;9:53–62. doi: 10.1111/j.1399-5618.2007.00343.x. http://dx.doi.org/10.1111/j.1399-5618.2007.00343.x. [DOI] [PubMed] [Google Scholar]
- 26.Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiat. 2003;64:161–174. http://dx.doi.org/10.4088/JCP.v64n0209. [PubMed] [Google Scholar]
- 27.Kupfer DJ, Frank E, Grochocinski VJ, Cluss PA, Houck PR, Stapf DA. Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiat. 2002;63:120–125. doi: 10.4088/jcp.v63n0206. http://dx.doi.org/10.4088/JCP.v63n0206. [DOI] [PubMed] [Google Scholar]
- 28.Gutiérrez-Rojas L, Gurpegui M, Ayuso-Mateos JL, Gutiérrez-Ariza JA, Ruiz-Veguilla M, Jurado D. Quality of life in bipolar disorder patients: a comparison with a general population sample. Bipolar Disord. 2008;10:625–634. doi: 10.1111/j.1399-5618.2008.00604.x. http://dx.doi.org/10.1111/j.1399-5618.2008.00604.x. [DOI] [PubMed] [Google Scholar]
- 29.Arts B, Jabben N, Krabbendam L, van Os J. Meta-analyses of cognitive functioning in euthymic bipolar patients and their first-degree relatives. Psychol Med. 2008;38:771–785. doi: 10.1017/S0033291707001675. http://dx.doi.org/10.1017/S0033291707001675. [DOI] [PubMed] [Google Scholar]
- 30.Torres IJ, Boudreau VG, Yatham LN. Neuropsychological functioning in euthymic bipolar disorder: a meta-analysis. Acta Psychiat Scand. 2007;434:17–26. doi: 10.1111/j.1600-0447.2007.01055.x. http://dx.doi.org/10.1111/j.1600-0447.2007.01055.x. [DOI] [PubMed] [Google Scholar]
- 31.Depp CA, Mausbach BT, Harmell AL, Savla GN, Bowie CR, Harvey PD, Patterson TL. Meta-analysis of the association between cognitive abilities and everyday functioning in bipolar disorder. Bipolar Disord. 2012;3:217–226. doi: 10.1111/j.1399-5618.2012.01011.x. http://dx.doi.org/10.1111/j.1399-5618.2012.01011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dell’Osso L, Carmassi C, Carlini M, Rucci P, Torri P, Cesari D, Landi P, Ciapparelli A, Maggi M. Sexual dysfunctions and suicidality in patients with bipolar disorder and unipolar depression. J Sex Med. 2009;6:3063–3070. doi: 10.1111/j.1743-6109.2009.01455.x. http://dx.doi.org/10.1111/j.1743-6109.2009.01455.x. [DOI] [PubMed] [Google Scholar]
- 33.Zuncheddu C, Carpiniello B. Sexual dysfunctions and bipolar disorder: a study of patients submitted to a long-term lithium treatment. Clin Ther. 2006;157:419–424. [PubMed] [Google Scholar]
- 34.Thomé ES, Dargél AA, Migliavacca FM, Potter WA, Jappur DM, Kapczinski F, Ceresér KM. Stigma experiences in bipolar patients: the impact upon functioning. J Psychiat Ment Hlt. 2012;19:665–671. doi: 10.1111/j.1365-2850.2011.01849.x. http://dx.doi.org/10.1111/j.1365-2850.2011.01849.x. [DOI] [PubMed] [Google Scholar]
- 35.Vázquez GH, Kapczinski F, Magalhaes PV, Córdoba R, Lopez Jaramillo C, Rosa AR, Sanchez de Carmona M, Tohen M. Stigma and functioning in patients with bipolar disorder. J Affect Disord. 2011;130:323–327. doi: 10.1016/j.jad.2010.10.012. http://dx.doi.org/10.1016/j.jad.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 36.Sarısoy G, Kaçar OF, Pazvantoğlu O, Korkmaz IZ, Oztürk A, Akkaya D, Yılmaz S, Böke Ö, Sahin AR. Internalized stigma and intimate relations in bipolar and schizophrenic patients: A comparative study. Compr Psychiat. 2013;54:665–672. doi: 10.1016/j.comppsych.2013.02.002. http://dx.doi.org/10.1016/j.comppsych.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 37.Martinez-Aran A, Vieta E, Torrent C, Sanchez-Moreno J, Goikolea JM, Salamero M, Malhi GS, Gonzalez-Pinto A, Daban C, Alvarez-Grandi S, Fountoulakis K, Kaprinis G, Tabares-Seisdedos R, Ayuso-Mateos JL. Functional outcome in bipolar disorder: the role of clinical and cognitive factors. Bipolar Disord. 2007;9:103–113. doi: 10.1111/j.1399-5618.2007.00327.x. http://dx.doi.org/10.1111/j.1399-5618.2007.00327.x. [DOI] [PubMed] [Google Scholar]
- 38.Goldberg JF, Harrow M, Leon AC. Lithium treatment of bipolar affective disorders under naturalistic followup conditions. Psychopharmacol Bull. 1996;32:47–54. [PubMed] [Google Scholar]
- 39.Balanzá-Martínez V, Selva G, Martínez-Arán A, Prickaerts J, Salazar J, González-Pinto A, Vieta E, Tabarés-Seisdedos R. Neurocognition in bipolar disorders--a closer look at comorbidities and medications. Eur J Pharmacol. 2010;626:87–96. doi: 10.1016/j.ejphar.2009.10.018. http://dx.doi.org/10.1016/j.ejphar.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 40.Levy B, Manove E. Functional outcome in bipolar disorder: the big picture. Depress Res Treat. 2012;2012:949248. doi: 10.1155/2012/949248. http://dx.doi.org/10.1155/2012/949248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Colom F, Vieta E, Sánchez-Moreno J, Palomino-Otiniano R, Reinares M, Goikolea JM, Benabarre A, Martínez-Arán A. Group psychoeducation for stabilised bipolar disorders: 5-year outcome of a randomised clinical trial. Brit J Psychiat. 2009;194:260–265. doi: 10.1192/bjp.bp.107.040485. http://dx.doi.org/10.1192/bjp.bp.107.040485. [DOI] [PubMed] [Google Scholar]
- 42.Frank E, Soreca I, Swartz HA, Fagiolini AM, Mallinger AG, Thase ME, Grochocinski VJ, Houck PR, Kupfer DJ. The role of interpersonal and social rhythm therapy in improving occupational functioning in patients with bipolar I disorder. Am J Psychiat. 2008;165:1559–1565. doi: 10.1176/appi.ajp.2008.07121953. http://dx.doi.org/10.1176/appi.ajp.2008.07121953. [DOI] [PMC free article] [PubMed] [Google Scholar]


