Abstract
Introduction
Fatigue is a subjective and non-specific symptom; therefore, evaluation of fatigue is quite difficult. Fatigue has been reported in 75%–87% of patients with multiple sclerosis (MS) and two-thirds of these patients indicated fatigue as one of the worst three common symptoms that they experienced. This study was conducted to measure the intensity, frequency and the characteristics of fatigue in patients with MS. Moreover, the effect of fatigue on the quality of life and its association with depression and disability were evaluated.
Methods
One hundred and twenty patients with multiple sclerosis (84 women and 36 men) were included in our study. The patients’ sociodemographic characteristics and their experiences on symptoms of fatigue were questioned. Presence and degree of fatigue were assessed using the fatigue severity scale (FSS). Disability status was detected with expanded disability status scale (EDSS). The Multiple Sclerosis Quality of Life (MSQoL-54) survey was conducted to evaluate the quality of life of patients and Beck Depression Inventory (BDI) was used to determine the current depression status. Patients were grouped into fatigue and non-fatigue groups based on FSS. Both groups were compared according to their age, sex, MS clinical types, course of the disease and scores of EDSS, BDI and MSQoL-54.
Results
Seventy percent of patients reported fatigue and 38% of these patients defined fatigue as their most disabling symptom. There was no correlation of fatigue with age, sex and disease duration. The correlation of fatigue and educational level was negative and weak (p<.05, r=−.214) and the correlation between fatigue and MS clinical types were significant but weak (p<.01, r=.228). Patients with fatigue had higher EDSS and BDI scores. In addition, FSS scores were found to be statistically meaningful and positively correlated with both EDSS and BDI scores (r=.404, r=.476, p<.01). Furthermore, our findings revealed that the quality of life in patients with MS and fatigue was poor (r=−.58 p<.01). Similarly, a negative connection was found between MSQoL-54 sub-scales and fatigue.
Conclusion
This study proved that fatigue has a positive correlation with depression and disability and a negative significant relation with the quality of life of patients with MS.
Keywords: Multiple sclerosis, fatigue, depression, quality of life
INTRODUCTION
Fatigue associated with multiple sclerosis (MS) observed by the patient or caregiver is a lack of physical and mental energy (1). In studies, 75%–87% of patients with MS complained of fatigue. Two-third of these patients indicated fatigue as one of the worst three common symptoms that they experienced (2,3,4). Fatigue in patients with MS is more frequently and more likely to affect daily activities than the fatigue in healthy adults or individuals with other diseases. There is a serious amount of loss of energy and motivation in these patients. However, when questioned in details that does not seem to be related with the patients’ emotional state or insomnia (5,6). Some studies asserted that fatigue in patients with MS is directly related to the underlying pathophysiological processes of MS, such as immune disorders, inflammation, neuronal dysfunction and demyelination (5,7). Common features of fatigue in people with MS and those without MS are exercise, stress, depression, prolonged physical activity and increase in the afternoons; however, it decreases with resting, sleeping and positive life experiences (1).
This study aims to investigate the correlation between fatigue and the level of disability, MS clinical types and depression and also the effects of fatigue on quality of life in patients with MS followed in the neurology clinic of our hospital.
METHODS
In this study, we consecutively interviewed 126 outpatients MS neurology who complied with the inclusion and exclusion criteria. All the patients were informed regarding the study conditions and their consents were received. Inclusion criteria was defined as definitely being diagnosed with MS according to the McDonald criteria, not having had any attacks in last month and not having used steroid. Exclusion criteria was defined as patients who have diseases other than MS, having restless legs syndrome, having periodic leg movements during the sleep, having sleep disorders, such as apnea syndrome and using benzodiazepines, muscle relaxants, antihistamines and sedatives besides interferon and glatiramer, which affect fatigue. After performing physical examination and laboratory tests, the detection of two patients with new attack and four patients with infection were excluded from the study. In this study that included 120 patients with MS, the following information were recorded in the patient registration form: duration of disease, number of episodes and the medicines that were taken, socio-demographic characteristics, such as gender, age, occupation, education level and marital status. The patient’s commuting distance to the hospital was not taken into account.
Neurological examination was performed in all the patients and their current disability conditions were scored based on the Expanded Disability Status Scale of Kurtzke (EDSS). Status of the patients’ depression was evaluated according to Beck Depression Inventory (BDI). The presence and severity of fatigue were assessed using the fatigue severity scale (FSS). The patients responded to the nine-question scale by scoring their states from 1 to 7. FSS calculation was done by taking the average of the total values. The cut-off value of pathologic fatigue was defined as 4 and above. In these patients, the clinical significance of fatigue was recorded as pathological levels of fatigue. The lower the total score was, the lower the fatigue. Multiple Sclerosis Quality of Life-54 (MSQoL-54) questionnaire was used to evaluate the quality of life (8). The study of MSQoL-54’s adaptation and validation to the Turkish society was performed on 183 cases with MS by Egemen Idiman et al. at the “Dokuz Eylul University Faculty of Medicine Department of Neurology,” and it was found that it can be understood and accepted by Turkish patients (9). As a result of this scale, patients had two separate points one of which was physical and the other was mental.
To eliminate differences of the evaluations, all the patients’ neurological examinations and EDSS scoring, FSS, BDI and MSQoL-54 questionnaire assessments were performed on the same day by the same doctor.
The patients were divided into two groups based on FSS score; patients with FSS scores 4 and above were grouped in “MS with fatigue” and patients with FSS scores below 4 were group in “MS with non-fatigue.” Both groups were compared with their age, gender, clinical type of MS, duration of disease, FSS scores, EDSS score, Beck Depression score and MSQoL-54.
Statistical Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) 13.0 statistical program along with Spearman’s rank correlation coefficient and Pearson’s rank correlation in the following tests: the Kolmogorov–Smirnov and Lilliefors tests, independent t-test (Student’s t test), Mann–Whitney U–test and chi-square test.
RESULTS
Sociodemographic and clinical features of patients in the study were shown in Table 1.
Table 1.
Demographic and clinical characteristics of the patients
| Number of patients (n=120) | |
|---|---|
| Gender | |
| Female | 84 (70%) |
| Male | 36 (30%) |
| Age (years) | 34.24±8.042 (17–54) |
| Educational status | n (%) |
| Illiterate | 3 (2.5) |
| Elementary school | 59 (49.2) |
| High school | 41 (34.2) |
| University | 17 (14.2) |
| Mean duration of disease (years) | 8.08±5.64 (1–28) |
| MS clinical types | n (%) |
| Relapsing-remitting (RR) | 101 (84.2) |
| Secondary progressive (SP) | 18 (15) |
| Primer progressive (PP) | 1 (0.8) |
| Mean number of episodes | 5.53±3.114 (0–15) |
| Mean score of EDSS | 2.867±1.446 (0,5–7) |
| Mean score of FSS | 4.81±1.743 (1–7) |
| Mean score of BDI | 14.04±8.809 (0–39) |
| Mean score of MSQOL-54 | |
| Mean physical score of MSQOL-54 | 58.42±19.84 (15.11–96.49) |
| Mean mental score of MSQOL-54 | 56.76±22.13 (15.67–98.84) |
MS: multiple sclerosis; EDSS: expanded disability status scale; FSS: fatigue severity scale; BDI: Beck Depression Inventory; MSQOL: Multiple Sclerosis Quality of Life
According to FSS values, the number of patients with fatigue was defined 84 (70%) and the number of patients that are non-fatigue was 36 (30%). Fatigue was stated as the first biggest complaint by 32 (38.1%) patients out of the 84 with fatigue and the second biggest complaint by 22 (26.2%) of the 84 patients with fatigue. Eighty (95.2%) patients stated that they experienced fatigue >6 weeks and four (4.8%) patients stated that they experienced fatigue <6 weeks. The daily distribution when queried: 42(50%) patients stated that they become fatigued in the afternoon, 14 (16.7%) patients in the evening, nine (10.7%) patients in the morning and 10 (11.9%) patients have fatigue throughout the day. The factors that affect fatigue were stated as stress by 29 (34.5%) patients, an increase in weather temperature by 22 (26.2%) patients, physical activity by four (4.8%) patients and 17 (20.2%) patients stated that they have experienced all of these factors. Twenty-three of these patients were not using any medication, 31 patients were on interferon beta-1b, 39 patients were on interferon beta-1a and 27 patients were receiving treatment with glatiramer acetate. However, statistical correlation between fatigue and treatment were not performed because of the low number of patients.
No significant difference between FSS scores and age and gender (p>.05) was found. According to education level of in patients with MS, FSS scores in patients with higher education were found lower than patients with elementary and high school graduates (r=−.214, p=.019). When mean of FSS was calculated based on MS types, the result for relapsing remitting patient group was 4.60±1.78 and for secondary progressive-primer progressive (SP-PP) patient group was 5.92±1.016. The groups’ variances were not equal; therefore, the median of the groups were compared by Mann–Whitney U test. The correlation between the FSS’ values of RR and SP-PP groups were significant but weak (p<.01, r=.228). The relationship between duration of disease and the FSS values were not found statistically significant (p=.327, r=.09).
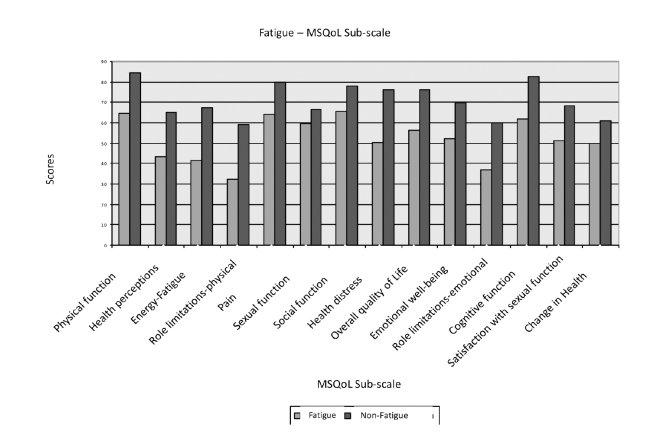
The mean of EDSS score in 84 patients with fatigue was found to be 3.155±1.429 and the mean of EDSS score in 36 patients without fatigue was found to be 2.194±1.267. A statistically significant and moderately positive (r=.404) correlation between FSS and EDSS values (p<.01) was found. Thirty-four patients with fatigue were depressive and their mean value of BDI score was found to be 16.04±8.356. Five patients without fatigue were depressive too and their mean value of BDI score was 9.36±8.132. A statistically significant positive correlation was found between FSS scores and BDI scores (p<.01, r=.476). The mean number of fatigue and non-fatigue patients and MSQoL-54 physical and mental component values are shown in Table 2. A strong negative correlation was found between physical and mental scores of MSQoL-54 and the FSS scores (r=−.58, p<.01). When the correlation between fatigue and MSQoL-54 subscales were evaluated, non-fatigue patients’ scores were observed to be higher in all scales (Figure 1).
Table 2.
The relationship between fatigue and MSQOL-54 physical and mental scores
| Fatigue status | Mean | SD |
|---|---|---|
| Physical MSQOL | ||
| Fatigue(+) | 52,47932 | 18,028131 |
| Fatigue (−) | 72,28972 | 16,871951 |
| Mental MSQOL | ||
| Fatigue (+) | 50,44356 | 19,870278 |
| Fatigue (−) | 71,35147 | 20,361845 |
SD: standard deviation; MSQOL: Multiple Sclerosis Quality of Life
Figure 1.
The relationship between fatigue and MSQoL-54 sub-scales
DISCUSSION
Fatigue in patients with MS had been known as a rare symptom up until early 1980s. Later on, studies revealed that >75% of patients experience fatigue and 28% of these patients stated fatigue as an initial complain of all their other symptoms (2,3). Furthermore, in our study, fatigue was found in 70% of patients and 38% of them indicated fatigue as the biggest complain that they experienced.
Many factors indirectly can cause pathological fatigue. Among these factors, sleep disorders and medicines used in treating the other symptoms of MS are important (5,6,7). In patients with MS, because of the motor problems, such as nocturnal spasms and spasticity, duration and quality of sleep at night are deteriorated. In addition, nocturia and incontinence can cause fatigue by disrupting sleep. Obstructive sleep apnea in patients with MS, which is not related with MS, can be commonly observed (7). Therefore, in patients with fatigue, it is essential to receive their sleep information either from themselves or their partners to identify their sleep disorders; if necessary, polysomnography test should be run. In our study, these cases were excluded based on the questioning. Medicines used for spasticity and pain in some of the MS symptoms could cause side effects that can lead to pathological fatigue. Most analgesics, antispasticity agents, sedative, anticonvulsant and antihistamines can cause side effects that lead to fatigue (1). In addition, fatigue can be seen as a side effect of interferon beta. In general, flu-like symptoms, such as fever and chills, decrease over time after injection. In our study, the patients’ who take medicines that cause fatigue were questioned. Patients taken non-immunomodulatory treatment were excluded; however, because of the small number of patients, the usage of interferon was disregarded.
According to the literature regarding the studies about investigating the relationship between pathological fatigue and level of disability, conflicting results were observed. Some studies reported that there was no correlation between pathological fatigue and level of disability; this finding could be because of the following reasons: working with small case groups (2); evaluating EDSS done by different neurologists (2,10,11); changing FSS scores during the treatments (2,10,11,12), including patients only with moderate EDSS scores (11,12); and not doing EDSS and fatigue assessment simultaneously (10). In prospective study of Bakshi et al. (13) other medical diseases and psychoactive medications were excluded and patients’ disability rate was kept wide. Moreover, EDSS and fatigue were evaluated on the same day by the same neurologist. Therefore, fatigue was explained as an independent of physical disability because a weak correlation was found between EDSS and fatigue. In one study, Dijatti et al. (14) aimed to objectively measure pathological fatigue. It is reported that pathological fatigue severity was more in patients who captured pyramidal tracts and have had attacks on theses tracts. In a different study conducted by Iriarte et al. (15), it was stated that 85% patients with MS and fatigue had pyramidal affect. In other study, Turkbay et al. (16) examined 209 patients with MS using the modified fatigue impact scale. They found that positive correlation existing between EDSS and fatigue. In other study by Flachenecker et al. (17), significant positive correlation was stated between EDSS score and fatigue. The results in our study were that the mean values of EDSS in fatigue patients were found higher than those in the non-fatigue patients. Furthermore, the difference between them was statistically significant.
More than half of the patients with MS are diagnosed with depression during the course of their disease (18). Depressive symptoms increase the fatigue either directly or as a result of its psychological consequences (19,20,21,22). In the prospective study of Bakshi et al. (13) that was conducted over a two-year period, 106 patients were interviewed and 71 of them were included in the study. Fatigue was assessed with FSS and depression was assessed with DSM-IV criteria. However, patients who exhibited severe depressive symptoms were assessed with both the Hamilton Depression Inventory (HDI) and BDI. In patients with MS and fatigue, higher HDI and BDI scores were determined. In addition to this, HDI and BDI scores were significantly and positively correlated with FSS scores (13). These researchers stated there are common underlying mechanisms, such as psychological factors and specific brain lesions, that play an important role in correlation between fatigue and depression. In another study conducted on 155 patients with MS, anxiety and depression scores were higher in patients with fatigue (15).
In another study, 207 patients with MS were assessed using FSS and the self-rating depression scale to investigate the correlation between MS-related fatigue and the following: depression, disability and disease type. Fatigue scores were found highly correlated with depression and EDSS scores. Fatigue in patients with primary and secondary progressive type of MS was found to be more frequent than fatigue in patients with relapsing-remitting type of MS; however, it was indicated that frequency may be because of differences in the level of disability in patients with MS. In this respect, it was recommended to review the results of other studies (23). Our results in patients with secondary progressive MS, FSS scores were defined highly significant. However, when evaluated statistically, the type of the course of MS and fatigue revealed a weak correlation.
In the study conducted by Roelcke et al. (24), regional cerebral glucose metabolism in 47 patients with MS and 60 healthy control subjects was measured using PET-FDG and fatigue was assessed using FSS and depression was assessed using BDI. They reported that significant correlation between fatigue and depression (FSS-BDI) exists. Moreover, cerebral metabolic rate of glucose in patients with MS and fatigue were decreased; however, there were no findings that revealed a correlation between BDI and global cerebral glucose metabolism (24). In another study that was conducted on 79 patients with MS grouped according to their FSS scores, similar to our results, severity of disability and depression were found higher in the group with fatigue (25). In our study, it was found that 40.5% of the patients with fatigue and 14% of patients without fatigue had depression. In addition, a positive and significant correlation was found between BDI and FSS values (p<.01, r=.476).
There are various studies regarding the impact of fatigue, depression and disability on the quality of life in patients with MS. In the study of Amato et al. (26), the effects of fatigue on quality of life in patients with MS was assessed using MSQoL-54 questionnaire; based on the results, depression, disability and fatigue were stated as independent factors that affect quality of life. Moreover, in this study, a moderate correlation between MSQoL-54 physical sub-score and EDSS and a strongly significant correlation between FSS and HDI were found (26). In another study performed prospectively, 60 patients had been followed up for 2 years. Similar to our study, MSQoL-54, EDSS and FSS tests were evaluated on the same day; however, the difference from our study was that the evaluation of depression was assessed using DSM-IV and HDI within 72 h by a psychiatrist who did not know the patients. Therefore, there was no correlation between MSQoL-54 and the following: age, gender and duration of disease. When the quality of life was evaluated in the MS types, particularly in patients with secondary progressive MS, it was reported to be lower. In the same study, increase in EDSS significantly affected MSQoL-54 physical and mental health scales, weakly affected cognitive and sexual dysfunction subscales and in addition to these findings, in patients with MS and fatigue as well as depression, lower MSQoL scales were determined (27).
In the study conducted by Benedict et al. (28), 120 patients with MA and 44 healthy control subjects were assessed using MSQoL-54. It was found that physical sub-scale could be correlated with fatigue, depression and disability and mental sub-scale could be associated with depression and fatigue (28). In our country, the 79 patients with MS evaluated in the study demonstrated that both MSQoL-54 mental and physical scores have a negative correlation with disability, fatigue and depression and also depression has the most powerful effect on quality of life (29). In another study, 151 patients with MS were evaluated before and after the rehabilitation and EDSS and BDI both revealed significantly positive correlation with FSS scores. Moreover, the significant negative correlation was found between FSS and MSQoL-54’ mental and physical scores (30). In our study, significantly important negative relationships were determined between MSQoL-54 mental and physical scores and FSS scores (r=−.58, p<.01, r=−.58, p<.01). The results were complied with literature. The values of quality of life in patients with fatigue and high level of disability were found to be lower. Similarly, a negative correlation was found between MSQoL-54 subscales and fatigue. In conclusion, this study demonstrated that fatigue is seen quite often in patients with MS (70%). Moreover, it has a positive association with depression and disability, whereas having a negative significant relationship with the patients’ quality of life.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Multiple Sclerosis Council for Clinical Practice Guidelines. Fatigue and Multiple Sclerosis Evidence-Based Management Strategies for Fatigue in Multiple Sclerosis. Washington: Paralyzed Veterans of America; 1998. [Google Scholar]
- 2.Krupp LB, Alvarez LA, LaRocca NG, Scheinberg LC. Fatigue in multiple sclerosis. Arch Neurol. 1988;45:435–437. doi: 10.1001/archneur.1988.00520280085020. http://dx.doi.org/10.1001/archneur.1988.00520280085020. [DOI] [PubMed] [Google Scholar]
- 3.Freal JE, Kraft GH, Coryell JK. Symptomatic fatigue in multiple sclerosis. Arch Phys Med Rehabil. 1984;65:135–138. [PubMed] [Google Scholar]
- 4.Murray TJ. Amantadine therapy for fatigue in multiple sclerosis. Can J Neurol Sci. 1985;12:251–254. doi: 10.1017/s0317167100047107. [DOI] [PubMed] [Google Scholar]
- 5.Comi G, Leocani L, Rossi P, Colombo B. Physiopathology and treatment of fatigue in multiple sclerosis. J Neurol. 2001;248:174–179. doi: 10.1007/s004150170222. http://dx.doi.org/10.1007/s004150170222. [DOI] [PubMed] [Google Scholar]
- 6.Krupp LB. Fatigue in multiple sclerosis: definition, pathophysiology and treatment. CNS Drugs. 2003;17:225–234. doi: 10.2165/00023210-200317040-00002. http://dx.doi.org/10.2165/00023210-200317040-00002. [DOI] [PubMed] [Google Scholar]
- 7.Krupp LB. Fatigue in Multiple Sclerois: A Guide to Diagnosis and Management. New York: Demos Medical Publishing Inc; 2004. [Google Scholar]
- 8.Vickrey BG, Hays RD, Harooni R, Myers LW, Ellison GW. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995;4:187–206. doi: 10.1007/BF02260859. http://dx.doi.org/10.1007/BF02260859. [DOI] [PubMed] [Google Scholar]
- 9.Idiman E, Uzunel F, Ozakbas S, Yozbatiran N, Oguz M, Callioglu B, Gokce N, Bahar Z. Cross-cultural adaptation and validation of multiple sclerosis quality of life questionnaire (MSQoL-54) in a Turkish multiple sclerosis sample. J Neurol Sci. 2006;240:77–80. doi: 10.1016/j.jns.2005.09.009. http://dx.doi.org/10.1016/j.jns.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Fisk JD, Ritvo PG, Ross L, Haase DA, Marrie TJ, Schlech WF. Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis. 1994;18(Suppl 1):79–83. doi: 10.1093/clinids/18.supplement_1.s79. http://dx.doi.org/10.1093/clinids/18.Supplement_1.S79. [DOI] [PubMed] [Google Scholar]
- 11.Vercoulen JH, Hommes OR, Swanink CM, Jongen PJ, Fennis JF, Galama JM, van der Meer JW, Bleijenberg G. The measurement of fatigue in patients with multiple sclerosis. A multidimensional comparison with patients with chronic fatigue syndrome and healthy subjects. Arch Neurol. 1996;53:642–649. doi: 10.1001/archneur.1996.00550070080014. http://dx.doi.org/10.1001/archneur.1996.00550070080014. [DOI] [PubMed] [Google Scholar]
- 12.Van der Werf SP, Jongen PJ, Lycklama a Nijeholt GJ, Barkhof F, Hommes OR, Bleijenberg G. Fatigue in multiple sclerosis: interrelations between fatigue complaints, cerebral MRI abnormalities and neurological disability. J Neurol Sci. 1998;160:164–170. doi: 10.1016/s0022-510x(98)00251-2. http://dx.doi.org/10.1016/S0022-510X(98)00251-2. [DOI] [PubMed] [Google Scholar]
- 13.Bakshi R, Shaikh ZA, Miletich RS, Czarnecki D, Dmochowski J, Henschel K, Janardhan V, Dubey N, Kinkel PR. Fatigue in multiple sclerosis and its relationship to depression and neurologic disability. Mult Scler. 2000;6:181–185. doi: 10.1177/135245850000600308. http://dx.doi.org/10.1191/135245800701566052. [DOI] [PubMed] [Google Scholar]
- 14.Djaldetti R, Ziv I, Achiron A, Melamed E. Fatigue in multiple sclerosis compared with chronic fatigue syndrome: A quantitative assessment. Neurology. 1996;46:632–635. doi: 10.1212/wnl.46.3.632. http://dx.doi.org/10.1212/WNL.46.3.632. [DOI] [PubMed] [Google Scholar]
- 15.Iriarte J, Subira ML, Castro P. Modalities of fatigue in multiple sclerosis: correlation with clinical and biological factors. Mult Scler. 2000;6:124–130. doi: 10.1177/135245850000600212. http://dx.doi.org/10.1191/135245800678827572. [DOI] [PubMed] [Google Scholar]
- 16.Türkbay TG, Yıldırım Y, Özakbaş S. Multiple sklerozlu hastalarda yorgunluk ve yorgunluğun etkisinin değerlendirilmesi. Arch Neuropsychiatr. 2004;10:515–520. [Google Scholar]
- 17.Flachenecker P, Kumpfel T, Kallmann B, Gottschalk M, Grauer O, Rieckmann P, Trenkwalder C, Toyka KV. Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler. 2002;8:523–526. doi: 10.1191/1352458502ms839oa. http://dx.doi.org/10.1191/1352458502ms839oa. [DOI] [PubMed] [Google Scholar]
- 18.Sadovnick AD, Remick RA, Allen J, Swartz E, Yee IM, Eisen K, Farquhar R, Hashimoto SA, Hooge J, Kastrukoff LF, Morrison W, Nelson J, Oger J, Paty DW. Depression and multiple sclerosis. Neurology. 1996;46:628–632. doi: 10.1212/wnl.46.3.628. http://dx.doi.org/10.1212/WNL.46.3.628. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz CE, Coulthard-Morris L, Zeng Q. Psychosocial correlates of fatigue in multiple sclerosis. Arch Phys Med Rehabil. 1996;77:165–170. doi: 10.1016/s0003-9993(96)90162-8. http://dx.doi.org/10.1016/S0003-9993(96)90162-8. [DOI] [PubMed] [Google Scholar]
- 20.Randolph JJ, Arnett PA. Depression and fatigue in relapsing-remitting MS: the role of symptomatic variability. Mult Scler. 2005;11:186–190. doi: 10.1191/1352458505ms1133oa. http://dx.doi.org/10.1191/1352458505ms1133oa. [DOI] [PubMed] [Google Scholar]
- 21.Rasova K, Brandejsky P, Havrdova E, Zalisova M, Rexova P. Spiroergometric and spirometric parameters in patients with multiple sclerosis: are there any links between these parameters and fatigue, depression, neurological impairment, disability, handicap and quality of life in multiple sclerosis? Mult Scler. 2005;11:213–221. doi: 10.1191/1352458505ms1155oa. http://dx.doi.org/10.1191/1352458505ms1155oa. [DOI] [PubMed] [Google Scholar]
- 22.Ünver V, Kılıç B, Bolu A, Demirkaya Ş. An analysis of the fatigue-related factors and coping strategies in multiple sclerosis patients. J Neurol Sci. 2012;29:306–315. [Google Scholar]
- 23.Kroencke DC, Lynch SG, Denney DR. Fatigue in multiple sclerosis: relationship to depression, disability, and disease pattern. Mult Scler. 2000;6:131–136. doi: 10.1177/135245850000600213. http://dx.doi.org/10.1177/135245850000600213. [DOI] [PubMed] [Google Scholar]
- 24.Roelcke U, Kappos L, Lechner-Scott J, Brunnschweiler H, Huber S, Ammann W, Plohmann A, Dellas S, Maguire RP, Missimer J, Radu EW, Steck A, Leenders KL. Reduced glucose metabolism in the frontal cortex and basal ganglia of multiple sclerosis patients with fatigue: a 18F-fluorodeoxyglucose positron emission tomography study. Neurology. 1997;48:1566–1571. doi: 10.1212/wnl.48.6.1566. http://dx.doi.org/10.1212/WNL.48.6.1566. [DOI] [PubMed] [Google Scholar]
- 25.Kaya T, Karatepe AG, Demirhan A, Günaydın R, Gedizlioğlu M, Çe P. Fatigue and Related Factors in Patients With Multiple Sclerosis. J Neurol Sci. 2009;26:190–197. [Google Scholar]
- 26.Amato MP, Ponziani G, Rossi F, Liedl CL, Stefanile C, Rossi L. Quality of life in multiple sclerosis: the impact of depression, fatigue and disability. Mult Scler. 2001;7:340–344. doi: 10.1177/135245850100700511. http://dx.doi.org/10.1191/135245801681138059. [DOI] [PubMed] [Google Scholar]
- 27.Janardhan V, Bakshi R. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002;205:51–58. doi: 10.1016/s0022-510x(02)00312-x. http://dx.doi.org/10.1016/S0022-510X(02)00312-X. [DOI] [PubMed] [Google Scholar]
- 28.Benedict RH, Wahlig E, Bakshi R, Fishman I, Munschauer F, Zivadinov R, Weinstock-Guttman B. Predicting quality of life in multiple sclerosis: accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. J Neurol Sci. 2005;231:29–34. doi: 10.1016/j.jns.2004.12.009. http://dx.doi.org/10.1016/j.jns.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 29.Göksel Karatepe A, Kaya T, Günaydın R, Demirhan A, Ce P, Gedizlioğlu M. Quality of life in patients with multiple sclerosis: the impact of depression, fatigue, and disability. Int J Rehabil Res. 2011;34:290–298. doi: 10.1097/MRR.0b013e32834ad479. http://dx.doi.org/10.1097/MRR.0b013e32834ad479. [DOI] [PubMed] [Google Scholar]
- 30.Drulovic J, Bursac LO, Milojkovic D, Tepavcevic DK, Gazibara T, Pekmezovic T. MSQoL-54 predicts change in fatigue after inpatient rehabilitation for people with multiple sclerosis. Disabil Rehabil. 2013;35:362–366. doi: 10.3109/09638288.2012.704122. http://dx.doi.org/10.3109/09638288.2012.704122. [DOI] [PubMed] [Google Scholar]