Abstract
Introduction
Interoceptive awareness (IA) is defined as an ability to accurately perceive interoceptive processes, which comprise receiving, processing, and integrating body-relevant signals together with external stimuli. Interoceptive processes affect the motivated approach or avoidance behavior toward stimuli. Alcohol and other substances have effects on the autonomic system that result in altered interoceptive processes. Individuals who have disturbed IA may be at a higher risk of addiction because they are not able to utilize sufficiently body-relevant signals to guide their decision-making. The hypothesis that IA in alcohol-addicted patients would be affected and that the disturbed IA would be associated with alcohol craving was tested in this study.
Methods
The study was conducted with 55 patients diagnosed with alcohol addiction according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) criteria and who had been sober for at least two weeks and 52 non-addicted healthy controls. IA measurements were performed using the heartbeat perception performance method, which determines participants’ awareness of their own heartbeat by comparing the number of subjectively perceived heartbeats with an objective heart rate measure recorded with ECG during four separate intervals. In addition, the Alcohol Use Disorders Identification Test (AUDIT), Penn Alcohol Craving Scale (PACS), and Obsessive Compulsive Drinking Scale (OCDS) were performed on the alcohol-addicted patient group.
Results
IA scores were significantly lower in the alcohol-addicted patients than the control subjects. IA scores of alcohol-addicted patients were negatively correlated with the levels of alcohol craving sensations according to the PACS results.
Conclusion
Our results corroborate the suggestion that IA in alcohol-addicted patients would be affected and that poor IA would be associated with alcohol craving and could be a maintaining factor for drinking behavior.
Keywords: Alcohol addiction, interoceptive awareness, alcohol craving
INTRODUCTION
Alcohol addiction is a disorder that impairs mental and physical health; impairs the adjustment of the individual in the family, society and work; and has heterogeneous characteristics such as the inability to cut down or control alcohol use, in addition to its individual and social harms; issues with withdrawal symptoms in the case of discontinuation; tolerance development, with a strong desire or urge to use alcohol; and high relapse rates (1).
A very strong desire or urge to use a substance (craving) changes from person to person but can develop in some individuals into substance addiction. Craving can retain its presence and effect for a long time and may even continue after periods of prolonged abstinence and can cause relapses (2). Craving for the addicting substance is defined as “the strong subjective desire or urge to use the substance accompanying substance addiction” (3). The desire emerges in some cases as a compulsion such that it is impossible to resist obtaining and using the substance (4). Craving may appear without stimuli as well as in presence of internal or external stimuli that act as reminders of the substance (5). Internal stimuli about the substance may constitute emotional states (e.g., anxiety, anger) or withdrawal symptoms, and external stimuli include the environment and objects (e.g., bottles of alcoholic beverages, advertisements) related to the substance (6). Craving has been evaluated as being related to the failure of abstinence-based treatment as an outpatient, resistance to treatment, and severity of alcoholism and as being a strong predictive factor for relapse (7,8,9,10).
Substance abuse generates different physical effects, accompanied by unique emotions for the addicted individual (e.g., autonomic effects such as blood pressure and heart rate changes). The cessation of substance use may also cause withdrawal syndromes with unique autonomic effects, in addition to the effects of the substance use itself on the body (11). It is claimed that the changes in the perception and awareness of substance use or withdrawal-related interoceptive processes play a role in the onset and maintenance of addiction (12).
Interoceptive awareness (IA) is defined as the ability to accurately perceive interoceptive processes, which comprise receiving, processing, and integrating body-relevant signals, together with external stimuli. Awareness is the state of defining one’s experiences and bodily signals with mental processes. The concept of being aware/unaware has an influence on many behaviors that a person displays automatically. IA is involved in many situations that correspond to addiction, such as conditioning mechanisms, sensitivity toward bodily signals that act as reminders of the substance, emotional dysregulation, and failure of making the right decision in risky situations. Therefore, it is thought that the impairment of IA processes plays a role in physiological and psychological adaptations related to addiction; however, a proven direct relationship has not yet been found (11,12).
Studies about the neurobiology of addiction focus on the effects of subcortical systems such as the amygdala, ventral striatum, and mesolimbic regions on the urge and substance-seeking behavior. However, the insula, which is usually overseen, also plays an important role in the desire for substance use. The insula is seen as a region that adapts bodily signals to emotions and decision-making mechanisms in processes that include indefinite risk and reward (11). In studies conducted with substance addicts, stimuli acting as reminders of the substance have shown increased insular activation, and this situation has been reported to be associated with the craving intensity (11,13,14). It has been shown that the response of the insula to emotional stimuli decreases with alcohol use and the volume of insular gray matter is reduced in substance users (15,16). It has been reported that individuals with insular damage quit smoking more easily, have lower relapse rates, and experience lesser urge to smoke than individuals with damage to other brain regions (17). It has been demonstrated that the insula is the primary neural center related to IA processes (18,19). The insula plays an important role in perception of the physiological status of the body with the assistance of bodily signals and the generation of unique emotional states to maintain homeostasis and motivational processes that prompt approach/avoidance behavior toward stimuli (20).
An impaired IA is claimed to increase craving and drinking behavior in two ways. Emotional motivational processes are not active in decision-making mechanisms in addicts with decreased IA when they come across stimuli related to the substance because of weakening of the development of subjective emotions that could perceive the physiological state of the body and could obtain the internal balance of the body through bodily signals. An insufficiency of negative emotions that could prompt the avoidance behavior for stimuli will instead facilitate heading toward the rewarding/appetitive stimuli of the addict who already has impaired neurobiological and behavioral responses; therefore, craving and drinking behaviors may be enhanced by an increased activity of non-emotional motivational processes (e.g., habits, conditioning, positive expectations about drinking) (12). Addicts with increased IA may be under the risk of relapse triggered by negative emotions or stress due to more intensive experience of withdrawal. Negative emotions that are promoted by internal systems (e.g., perception of heart rate changes) and external systems (e.g., interpersonal stressors) and signs similar to withdrawal symptoms produced by internal processes may lead individuals toward seeking and using the substance. This situation could be explained by the negative reinforcing effects of the substance (12,21).
Counting the heart beats in short time periods while recording the heart beats of the subject with ECG and then comparing the real heart rate observed with the estimated heart rate for the subject is a proven effective method for the evaluation of IA (22,23,24). There is a recent study in the literature inspecting IA of alcohol addicts according to their heart rate perception performance (25).
The relationship between internal processes and IA may contribute to the phenomenological explanation of the inconsistencies between decreased insight, denial, intention, and deeds that play an important role in addiction (12). This study was conducted according to the assumption that the processes related to IA may be impaired in alcohol-addicted patients. The aim of the study was to compare the IA levels of sober alcoholics that are under treatment for alcohol addiction with those of healthy controls and to evaluate whether there is a relationship between craving and IA levels.
METHODS
Participants
Fifty-five patients who had been sober for at least two weeks and admitted as an inpatient or outpatient to the Trakya University School of Medicine, Department of Psychiatry Service, Edirne, Turkey, between March 2012 and August 2012, for the treatment of alcoholism and who met the alcohol addiction criteria according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) diagnosis criteria, and 52 healthy volunteers as a control group were included in the study. The study was conducted according to the voluntarism principle. The participants were informed about the study and written informed consents were obtained. The study was approved by the Trakya University School of Medicine Scientific Research Evaluation Council Ethical Committee, dated 22.02.2012, case number 06/09. A breathalyzer was used to measure the level of ethanol in expired air, and the breath alcohol concentrations of all the participants measured 0 promil.
All the participants underwent a mental status examination by the researchers and their psychiatric and medical histories were evaluated; the DSM-IV-TR diagnostic criteria and additional diagnostic evaluation were performed during the clinical evaluation. Exclusion criteria from the study were as follows: axis I psychiatric diagnosis other than alcohol addiction according to the DSM-IV-TR criteria, ongoing treatment for psychiatric disorders, delirium tremens and/or withdrawal state, mental retardation or other medical conditions that may cause difficulty to understand the instructions of the study, and clinically important abnormal ECG findings.
Materials
The American Psychiatric Association DSM-IV-TR criteria were implemented for the diagnosis of alcohol addiction (3). Individuals who had a problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least three of the given criteria, occurring within a 12-month period were defined as alcohol addicts. A socio-demographic data form prepared by the researchers was applied to participants who were qualified to be included in the study. Data about the socio-demographic status, such as the age, gender, marital status, education level and alcohol use and amount, smoking and amount, history of alcoholism treatment, and personal and family history of psychiatric disorders, were recorded on this form.
Alcohol Use Disorders Identification Test (AUDIT)
AUDIT was used to identify the alcohol use risk levels of the participants. The WHO has described four risk levels in the AUDIT guidelines (0–7, 8–15, 16–19, 20–40 points); increasing risk levels reflect increasing intervention levels. AUDIT was developed by WHO to identify at-risk drinking and alcohol-addicted patients in the context of “World Health Organization Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption” (26). It is a screening test that was investigated in primary medical care internationally, that could be filled in 5 minutes, and that was found to be reliable and valid. The first three questions examine the amount and frequency of alcohol use, and the following three questions examine the possible signs of addiction. The last four questions are about the current and lifetime problems related to alcohol use. Each question is scored with a five-level Likert (0–4) scale. High scores in AUDIT have been determined to be related to alcohol addiction (26). The Turkish version of the scale has been found to be reliable and valid (27).
Penn Alcohol Craving Scale (PACS)
The alcohol craving of the participants was evaluated with PACS. PACS is a questionnaire with five self-reporting statements and was developed to evaluate alcohol craving severity (frequency, intensity, duration, resistance, and general craving). Each statement is evaluated with a score of 0–6. The maximum total craving score is 30. The reliability and validity of PACS have been demonstrated (28). The Turkish version of PACS has been found to be reliable and valid for male inpatient alcohol addicts under treatment (29).
Obsessive Compulsive Drinking Scale (OCDS)
OCDS was used to evaluate the alcohol drinking characteristics of alcohol-addicted patients. The alcohol cravings of the participants were also evaluated with this scale. The maximum total craving score is 56. Various clinical, neurobiological and neuropsychological data indicate that obsessive thoughts about alcohol use and compulsive behavior are fragments of alcohol craving. The Yale–Brown Obsessive Compulsive Drinking Scale was modified and a self-reporting scale constituting 14 questions was produced (30). Each statement is scored with a point of 0–4. It provides information about alcohol craving in general and provides an evaluation of both obsessive and compulsive components. The Turkish version of the scale was found to be reliable and valid for male inpatient alcohol addicts under treatment (31).
Evaluation of IA
IA was measured with the heart rate tracking task described by Schandry (22), determining participants’ awareness of their own heartbeat by comparing the number of subjectively perceived heartbeats with an objective heart rate measure. This procedure was performed at the 25th, 35th, 45th, and the 100th second at four different stages based on the subject’s counting of their own heartbeat. A quiet environment in which the subjects could concentrate and count their heartbeats was acquired. The subject was requested to count their own heartbeat between “start” and “stop” orders without checking any device or pulse in a relaxed sitting position during the evaluation. The participants were not told about the duration that they would count their heartbeats. The actual heart rate was recorded with ECG simultaneously.
The IA value was calculated with the IA= 1/4∑(1 − (|RHB-CHB|)/RHB) formula. The results were between 0 and 1 and high scores demonstrated increased IA.
IA 25 sec = 1 − [(RHB 25 sec –CHB 25 sec)/RHB 25 sec]
IA 35 sec = 1 − [(RHB 35 sec – CHB 35 sec)/RHB 35 sec]
IA 45 sec = 1 − [(RHB 45 sec – CHB 45 sec)/RHB 45 sec]
IA 100 sec = 1 − [(RHB 100 sec – CHB 100 sec)/RHB 100 sec]
IA = (IA 25 sec + IA 35 sec + IA 45 sec + IA 100 sec)/4
Heartbeat perception is the most extensively researched aspect of IA and has been established as a valid indicator of substantial inter-individual differences (23,24).
Statistical Analysis
The Statistica 7.0 program was used for the statistical analysis. Conformity of the data to the normal distribution was inspected with the one-sample Kolmogorov–Smirnov test. The independent samples t-test was used to compare the means for parameters with a normal distribution between the groups, and the Mann–Whitney U test was used for parameters without a normal distribution. The chi-square test was used for investigation of the categorical variables between the groups. The Spearman’s test was conducted to evaluate the correlation of scales with each other. The significance cut-off value was set at a p value of <0.05 for all statistics.
RESULTS
The mean age of the alcohol addicted group was 43.38±10.83 and the mean age of the control group was 41.34±11.50. No significant difference was determined with regard to age and body mass index between the groups (p>0.05) (Table 1).
Table 1.
Age and BMI characteristics of the alcohol-addicted patients in comparison with those of the healthy controls
| Alcohol-addicted patients (n=55) | Healthy control group (n=52) | p | |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Age | 43.38±10.83 | 41.34±11.50 | 0.801 |
| BMI | 23.27±3.85 | 25.80±3.90 | 0.587 |
t-test. SD: standard deviation; BMI: body mass index
The two groups were compared with regard to gender distribution. Fifty (90.9%) of those in the patient group were males and 5 (9.1%) were females. Forty-seven (90.4%) of those in the control group were males and 5 (9,6%) were females. No significant difference related to gender distribution was determined between the groups (p>0.05) (Table 2).
Table 2.
Gender distribution of the alcohol-addicted patients in comparison with that of the healthy controls
| Gender | Alcohol-addicted patients (n=55) | Healthy control group (n=52) | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Male | 50 | 90.9 | 47 | 90.4 | 0.926 |
| Female | 5 | 9.1 | 5 | 9.6 | |
Chi-square test
The mean education duration of the patient group was 8.38 years, while it was 9.17 years in the control group. No significant difference was determined between the groups (p>0.05).
The two groups were compared with regard to alcohol consumption. Fifty-five individuals (100%) in the patient group and 23 individuals (44.2%) in the control group had a history of alcohol consumption. The difference between the two groups was significant (p<0.001). The mean alcohol consumption during the past year was calculated as 13.63 standard drinks per day in the patient group and 0.75 standard drinks per day in the control group. The difference between the two groups was significant (p<0.001). Thirty-four (61.8%) of those in the patient group had a history of addiction treatment, and 21 (38.2%) had been admitted for addiction treatment for the first time. There were no participants in the control group with a history of alcohol addiction diagnosis/treatment.
Fifty-one (92.7%) of the participants in the patient group were smokers and 4 (7.3%) were non-smokers. Twenty-eight (53.8%) of the participants in the control group were smokers and 24 (46.2%) were non-smokers. There was a significant difference between the two groups with regard to smoking (p<0.001). The mean daily cigarette smoking was 20.49±11.49 cigarettes per day in the patient group and 8.86±7.18 cigarettes per day in the control group. There was a significant difference between the two groups (p<0.001).
The mean IA score was 0.58±0.18 in the patient group and 0.71±0.16 in the control group. There was a significant difference between the two groups (p<0.05) (Figure 1).
Figure 1.
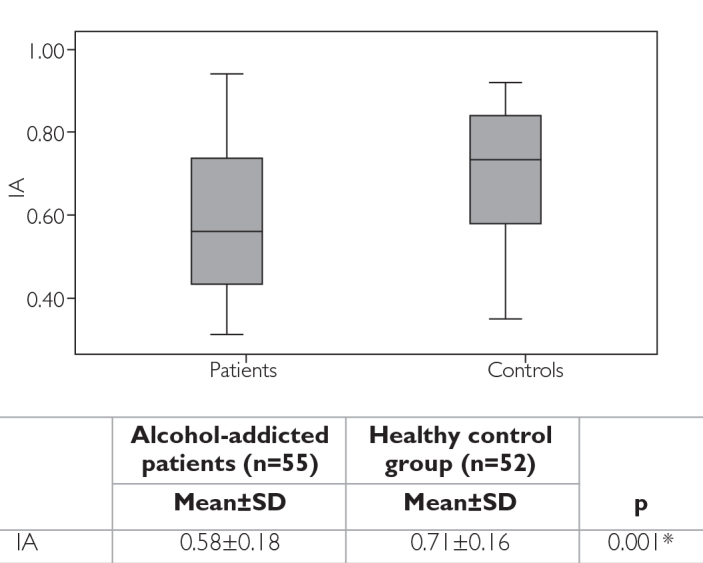
IA means of the alcohol-addicted patients in comparison with those of the healthy controls
Mann–Whitney U test. SD: Standard deviation; IA: interoceptive awareness
The correlation between the IA scores and AUDIT, PACS, and OCDS scores was evaluated. There was a negative correlation between the IA scores and AUDIT, PACS, and OCDS scores (correlation coefficients, −0.216, −0.330, and −0.216, respectively). The negative correlation with PACS scores was significant (p<0.05) (Table 3).
Table 3.
The correlation between the IA scores and AUDIT, PACS and OCDS scores
| AUDIT | PACS | OCDS | IA | ||
|---|---|---|---|---|---|
| AUDIT | Correlation coefficients | 1.000 | 0.390 | 0.419 | −0.216 |
| p | - | 0.003 | 0.001 | 0.114 | |
| PACS | Correlation coefficients | 1.000 | 0.512 | −0.330 | |
| p | - | 0.000 | 0.014* | ||
| OCDS | Correlation coefficients | 1.000 | −0.218 | ||
| p | - | 0.109 | |||
| IA | Correlation coefficients | 1.000 | |||
| p | - |
Spearman’s correlation. AUDIT: Alcohol Use Disorders Identification Test; PACS: PENN ALCOHOL CRAVING SCALE; OCDS: Obsessive Compulsive Drinking Scale; IA: interoceptive awareness
DISCUSSION
Our study based on the presumption of possible impaired IA processes in alcohol-addicted patients is the second study in the literature evaluating IA in alcohol-addicted patients based on heartbeat tracking performance. It was detected that compared with control subjects, IA was decreased among alcohol-addicted patients and there was a negative relation between PACS craving scores and heartbeat tracking performance.
There is a recent study evaluating IA based on heartbeat perception performance in alcohol-addicted patients in the literature (25). In this study, conducted with inpatient and outpatient sober alcohol addicts under treatment with no control group, heartbeat tracking performance and tension reduction expectancies (assessed with comprehensive alcohol expectancy questionnaire) were evaluated, and the relationship between the measured values and OCDS scores was investigated. The researchers did not determine a relationship between the IA values and craving; however, they reported that there was a negative relationship between IA values and craving in patients who had high tension decrease expectancies (e.g., decreasing negative affects after alcohol consumption). These findings were suggested to support the opinion that non-emotional motivational processes (e.g., habits, conditioning, positive expectations about alcohol use) are more effective on decision-making mechanism in alcohol-addicted patients with decreased IA and that decreased IA may increase the drinking behavior. The findings of our study support the opinion of a possible disturbed IA in alcohol addicts and that decreased IA may be related to cravings that lead to relapse. However, it is not possible to demonstrate a causative relationship with the texture and findings of our study.
IA was evaluated with only one measurement in or study. Heartbeat perception is the most extensively researched aspect of IA and has been established as a valid indicator of substantial inter-individual differences (23,24). The “compatibility of counted heartbeats with recorded heartbeats” was studied for the measurement of IA in different psychiatric disorders; in addition, the relationships between psychiatric symptoms and the IA values and distribution differences between the patient and control groups were investigated. Individual differences in cardiac perception were found to be related to cognitive-emotional events, time perception, pain perception, anxiety levels, mood changes, emotional attention and memory, emotional reactivity, alexythmia, and intuitive decision-making (32,33,34,35,36,37,38). Changes in these processes among substance-addicted patients are emphasized (12). It was reported that the feeling of hunger-satiety and the perception of bodily sensations were decreased in patients with eating disorders and obesity and that these processes were related to IA (39,40). It was reported that the anxiety symptoms were related to increased IA in patients with panic and anxiety disorder and that there was a negative relationship between depressive symptoms and IA in depression patients (41,42,43,44). A relationship between increased IA and anxiety-specific arousal symptoms has been detected in individuals with mood disorders (45). Alexithymia, which is described as the inability of recognizing, identifying, and expressing emotions, has been reported to have a negative relationship with IA (38). The mean IA value in healthy participants has been reported as 0.70–0.77 in the studies conducted with control groups. The mean value of the control group was 0.71 in our study. Further studies are required for detecting the distribution of this value among the normal population and for detecting the difference between various patient groups and the normal distribution.
Alcohol use was present in the control group of our study, although the use was not compatible with the addiction criteria. No distinction was made in the alcohol-addicted patient group according to the duration of alcohol use and amount. Smoking was statistically significant higher with the alcohol-addicted patients. No evaluation of alexithymia, which is related to IA, was made. IA measurements may have been affected by these parameters in our study. Depression and anxiety disorders are frequently observed among alcohol addicts, and it is known that there is a relationship between affective symptoms and IA. The depression and anxiety levels of the participants were not evaluated with any scale in our study. However, those who were detected to have depression and/or anxiety disorder during the initial clinical evaluation or those who were under treatment for these reasons were excluded from the study at the outset. The depression and anxiety levels of the participants may have affected the IA measurements, although depression and/or anxiety disorders were not detected during the mental state examination. Alcohol-addicted patients were chosen among those who had been sober for at least two weeks. No scale evaluating the withdrawal symptoms was used, but patients who displayed withdrawal symptoms during the clinical evaluation were not included in the study. Deviations from the basal state in physiological and cognitive processes may continue for a long time after the cessation of alcohol use. Physiological distress and medications administered for treatment during this period may have affected the IA measurements, although withdrawal symptoms were not detected clinically. The above-mentioned restrictions about the study methods may have caused some deficiencies during the interpretation of the results. Furthermore, physiological (e.g., blood pressure) and neurocognitive (e.g., attention and concentration) measurements could strengthen this study with regard to the evaluation of IA based on heartbeat perception.
IA processes in substance-addicted patients is not a widely researched topic. Demonstration of the insula as the primary center for IA processes, observation of changes in addiction behaviors in individuals with insula damage and in animal studies in which the insula is suppressed pharmacologically, and a number of neuroimaging studies that have shown insular cortex activation in association with cue reactivity and self-reported craving have raised the interest in this topic in the addiction field (11,12). Investigation of the relationship between processes (e.g., craving, negative affect, anxiety sensitivity) leading to relapses and IA, which is described as “correct or wrong interpretation of bodily feelings,” may be an important field of study. It is thought that the relationship between interoceptive sensations and awareness includes complicated physiological processes and different neuronal networks and brain circuits (12). Which interoceptive feelings are interpreted incorrectly by alcohol addicts and how these processes affect the desire for drinking, whether there is a causative relationship between IA and craving or drinking behavior, whether disturbed IA is a factor causing or contributing to relapse, and if so, whether it is related to other factors are topics that should be investigated. Observational studies conducted with reliable, valid, self-reporting scales that could evaluate IA in different dimensions with heart rate perception performance and that could evaluate the structural and functional changes in the insula are required.
The clinical significance of the study findings is that addicts with poor IA may benefit from therapies aimed at improving their awareness of the body (e.g., biological feedback educations, body-focused meditations, and mindfulness interventions) (12,20,46). Studies demonstrating the alterations in IA with awareness-based therapy applications, psychosocial interventions, and other relapse-preventing programs are required.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Fortuna JL, Smelson DA. The phenomenan of drug craving. J Psychoactive Drugs. 2008;40:255–261. doi: 10.1080/02791072.2008.10400640. http://dx.doi.org/10.1080/02791072.2008.10400640. [DOI] [PubMed] [Google Scholar]
- 3.Köroğlu E, translator and editor. Amerikan Psikiyatri Birliği. Ruhsal Bozuklukların Tanısal ve Sayımsal El Kitabı (DSM-IV-TR) 4. baskı. Ankara: Hekimler Yayın Birliği; 2007. [Google Scholar]
- 4.Tiffany ST, Carter BL, Singleton EG. Challenges in the manipulation assessment and interpretation of craving relevant variables. Addiction. 2000;95:177–187. doi: 10.1080/09652140050111753. http://dx.doi.org/10.1080/09652140050111753. [DOI] [PubMed] [Google Scholar]
- 5.Verheul R, Brink W, Geerlings P. A three pathway psychobiological model of craving for alcohol. Alcohol Alcohol. 1999;34:197–222. doi: 10.1093/alcalc/34.2.197. http://dx.doi.org/10.1093/alcalc/34.2.197. [DOI] [PubMed] [Google Scholar]
- 6.Swift RM. Medications and alcohol craving. Alcohol Res Health. 1999;23:207–213. [PMC free article] [PubMed] [Google Scholar]
- 7.O’Connor PG, Gottlieb LD, Kraus ML, Segal SR, Horwitz RI. Social and clinical features as predictors of outcome in outpatient alcohol withdrawal. J Gen Intern Med. 1991;6:312–316. doi: 10.1007/BF02597427. http://dx.doi.org/10.1007/BF02597427. [DOI] [PubMed] [Google Scholar]
- 8.Thomas SE, Deas D. The A-OCDS predicts both craving and alcohol cue reactivity in adolescent alcoholics. Addict Behav. 2005;30:1638–1648. doi: 10.1016/j.addbeh.2005.07.018. http://dx.doi.org/10.1016/j.addbeh.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 9.Glautier S, Drummond DC. Alcohol dependence and cue reactivity. J Stud Alcohol. 1994;55:224–229. doi: 10.15288/jsa.1994.55.224. http://dx.doi.org/10.15288/jsa.1994.55.224. [DOI] [PubMed] [Google Scholar]
- 10.Bottlender M, Soyka M. Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol Alcohol. 2004;39:357–361. doi: 10.1093/alcalc/agh073. http://dx.doi.org/10.1093/alcalc/agh073. [DOI] [PubMed] [Google Scholar]
- 11.Naqvi NH, Bechara A. The hidden island of addiction: the insula. Trends Neurosci. 2009;32:56–67. doi: 10.1016/j.tins.2008.09.009. http://dx.doi.org/10.1016/j.tins.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verdejo-Garcia A, Clark L, Dunn BD. The role of interoception in addiction: a critical review. Neurosci Biobehav Rev. 2012;36:1857–1869. doi: 10.1016/j.neubiorev.2012.05.007. http://dx.doi.org/10.1016/j.neubiorev.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Dom G, Sabbe B, Hulstijn W, Brink W. Substance use disorders and the orbitofrontal cortex: systematic review of behavioural decision-making and neuroimaging studies. Br J Psychiatry. 2005;187:209–220. doi: 10.1192/bjp.187.3.209. http://dx.doi.org/10.1192/bjp.187.3.209. [DOI] [PubMed] [Google Scholar]
- 14.Park MS, Sohn JH, Suk JA, Kim SH, Sohn S, Sparacio R. Brain substrates of craving to alcohol cues in subjects with alcohol use disorder. Alcohol Alcohol. 2007;42:417–422. doi: 10.1093/alcalc/agl117. http://dx.doi.org/10.1093/alcalc/agl117. [DOI] [PubMed] [Google Scholar]
- 15.Padula CB, Simmons AN, Matthews SC, Robinson SK, Tapert SF, Schuckit MA, et al. Alcohol attenuates activation in the bilateral anterior insula during an emotional processing task: a pilot study. Alcohol Alcohol. 2011;46:547–552. doi: 10.1093/alcalc/agr066. http://dx.doi.org/10.1093/alcalc/agr066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gadrini S, Venneri A. Reduced grey matter in the posterior insula as a structural vulnerability or diathesis to addiction. Brain Res Bull. 2012;87:205–211. doi: 10.1016/j.brainresbull.2011.11.021. http://dx.doi.org/10.1016/j.brainresbull.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 17.Naqvi NH, Rudrauf D, Damasio H, Bechara A. Damage to the insula disrupts addiction to cigarette smoking. Science. 2007;315:531–534. doi: 10.1126/science.1135926. http://dx.doi.org/10.1126/science.1135926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Critchley HD, Wiens S, Rotshtein P, Ohman A, Dolan RJ. Neural systems supporting interoceptive awareness. Nat Neurosci. 2004;7:189–195. doi: 10.1038/nn1176. http://dx.doi.org/10.1038/nn1176. [DOI] [PubMed] [Google Scholar]
- 19.Terasawa Y. How does interoceptive awareness interact with the subjective experience of emotion? An fMRI study. Hum Brain Mapp. 2013;34:598–612. doi: 10.1002/hbm.21458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paulus MP, Stewart JL, Haase L. Treatment approaches for interoceptive dysfunctions in drug addiction. Front Psychiatry. 2013;4:137. doi: 10.3389/fpsyt.2013.00137. http://dx.doi.org/10.3389/fpsyt.2013.00137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. http://dx.doi.org/10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- 22.Schandry R. Heart beat perception and emotional experience. Psychophysiology. 1981;18:483–488. doi: 10.1111/j.1469-8986.1981.tb02486.x. http://dx.doi.org/10.1111/j.1469-8986.1981.tb02486.x. [DOI] [PubMed] [Google Scholar]
- 23.Cameron OG. Interoception: the inside story-a model for psychosomatic processes. Psychosom Med. 2001;63:697–710. doi: 10.1097/00006842-200109000-00001. http://dx.doi.org/10.1097/00006842-200109000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Pollatos O, Kirsch W, Schandry R. Brain structures involved in interoceptive awareness and cardioafferent signal processing: a dipole source localization study. Hum Brain Mapp. 2005;26:54–64. doi: 10.1002/hbm.20121. http://dx.doi.org/10.1002/hbm.20121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmidt AF, Eulenbruch T, Langer C, Banger M. Interoceptive awareness, tension reduction expectancies and self-reported drinking behavior. Alcohol Alcohol. 2013;48:472–477. doi: 10.1093/alcalc/agt024. http://dx.doi.org/10.1093/alcalc/agt024. [DOI] [PubMed] [Google Scholar]
- 26.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test: guidelines for use in primary care. 2nd edition. World Health Organization; Geneva: 2001. WHO/MSB/01.6a. [Google Scholar]
- 27.Saatçioğlu O, Evren C, Çakmak D. Alkol kullanım bozuklukları tanıma testinin geçerliği ve güvenirliği. Türkiye’de Psikiyatri. 2002;4:107–113. [Google Scholar]
- 28.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res. 1999;23:1289–1295. http://dx.doi.org/10.1111/j.1530-0277.1999.tb04349.x. [PubMed] [Google Scholar]
- 29.Evren C, Flannery B, Çelik R, Durkaya M, Dalbudak E. Penn Alkol Aşerme Ölçeği (PAAÖ) Türkçe şeklinin yatarak tedavi gören erkek alkol bağımlısı hastalarda geçerliği ve güvenirliği. Bağımlılık Derg. 2008;9:128–134. [Google Scholar]
- 30.Anton RF, Moak DH, Latham P. The Obsessive Compulsive Drinking Scale: A self-rated instrument for the quantification of thoughts about alcohol and drinking behavior. Alcoholism: Clinical and Experimental Research. 1995;19:92–99. doi: 10.1111/j.1530-0277.1995.tb01475.x. http://dx.doi.org/10.1111/j.1530-0277.1995.tb01475.x. [DOI] [PubMed] [Google Scholar]
- 31.Evren C, Çelik S, Evren B, Aksoy R. Validation study of the Turkish version of the OCDS in male alcohol dependent inpatients. Düşünen Adam Psikiyatri Nöroloji Bilim Derg. 2011;24:1–12. [Google Scholar]
- 32.Meissner K, Wittmann M. Body signals, cardiac awareness, and the perception of time. Biol Psychol. 2011;86:289–297. doi: 10.1016/j.biopsycho.2011.01.001. http://dx.doi.org/10.1016/j.biopsycho.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 33.Stevens S, Gerlach AL, Cludius B, Silkens A, Craske MG, Hermann C. Heartbeat perception in social anxiety before and during speech anticipation. Behav Res Ther. 2011;49:138–143. doi: 10.1016/j.brat.2010.11.009. http://dx.doi.org/10.1016/j.brat.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Dunn BD, Dalgleish T, Ogilvie AD, Lawrence AD. Heartbeat perception in depression. Behav Res Ther. 2007;45:1921–1930. doi: 10.1016/j.brat.2006.09.008. http://dx.doi.org/10.1016/j.brat.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Wiens S. Interoception in emotional experience. Curr Opin Neurol. 2005;18:442–447. doi: 10.1097/01.wco.0000168079.92106.99. http://dx.doi.org/10.1097/01.wco.0000168079.92106.99. [DOI] [PubMed] [Google Scholar]
- 36.Matthias E, Schandry R, Duschek S, Pollatos O. On the relationship between interoceptive awareness and the attentional processing of visual stimuli. Int J Psychophysiol. 2009;72:154–159. doi: 10.1016/j.ijpsycho.2008.12.001. http://dx.doi.org/10.1016/j.ijpsycho.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 37.Pollatos O, Schandry R. Emotional processing and emotional memory are modulated by interoceptive awareness. Cogn Emot. 2008;22:272–287. http://dx.doi.org/10.1080/02699930701357535. [Google Scholar]
- 38.Herbert BM, Herbert C, Pollatos O. On the relationship between interoceptive awareness and alexithymia: is interoceptive awareness related to emotional awareness? J Pers. 2011;79:1149–1175. doi: 10.1111/j.1467-6494.2011.00717.x. [DOI] [PubMed] [Google Scholar]
- 39.Pollatos O, Kurz AL, Albrecht J, Schreder T, Kleemann AM, Schöpf V, Kopietz R, Wiesmann M, Schandry R. Reduced perception of bodily signals in anorexia nervosa. Eat Behav. 2008;9:381–388. doi: 10.1016/j.eatbeh.2008.02.001. http://dx.doi.org/10.1016/j.eatbeh.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 40.Volkow ND, Wang GJ, Tomasi D, Baler RD. Obesity and addiction: neurobiological overlaps. Obes Rev. 2013;14:2–18. doi: 10.1111/j.1467-789X.2012.01031.x. http://dx.doi.org/10.1111/j.1467-789X.2012.01031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Domschke K, Stevens S, Pfleiderer B, Gerlach AL. Interoceptive sensitivity in anxiety and anxiety disorders: an overview and integration of neurobiological findings. Clin Psychol Rev. 2010;30:1–11. doi: 10.1016/j.cpr.2009.08.008. http://dx.doi.org/10.1016/j.cpr.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 42.Zoellner LA, Craske MG. Interoceptive accuracy and panic. Behav Res Ther. 1999;37:1141–1158. doi: 10.1016/s0005-7967(98)00202-2. http://dx.doi.org/10.1016/S0005-7967(98)00202-2. [DOI] [PubMed] [Google Scholar]
- 43.Furman DJ, Waugh CE, Bhattacharjee K, Thompson RJ, Gotlib IH. Interoceptive awareness, positive affect, and decision making in major depressive disorder. J Affect Disord. 2013;151:780–785. doi: 10.1016/j.jad.2013.06.044. http://dx.doi.org/10.1016/j.jad.2013.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pollatos O, Traut-Mattausch E, Schandry R. Differential effects of anxiety and depression on interoceptive accuracy. Depress Anxiety. 2009;26:167–173. doi: 10.1002/da.20504. http://dx.doi.org/10.1002/da.20504. [DOI] [PubMed] [Google Scholar]
- 45.Dunn BD, Stefanovitch I, Evans D, Oliver C, Hawkins A, Dalgleish T. Can you feel the beat? Interoceptive awareness is an interactive function of anxiety and depression specific symptom dimensions. Behav Res Ther. 2010;48:1133–1138. doi: 10.1016/j.brat.2010.07.006. http://dx.doi.org/10.1016/j.brat.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Farb NA, Segal ZV, Anderson AK. Mindfulness meditation training alters cortical representations of interoceptive attention. Soc Cogn Affect Neurosci. 2013;8:15–26. doi: 10.1093/scan/nss066. http://dx.doi.org/10.1093/scan/nss066. [DOI] [PMC free article] [PubMed] [Google Scholar]


