Dear Editor,
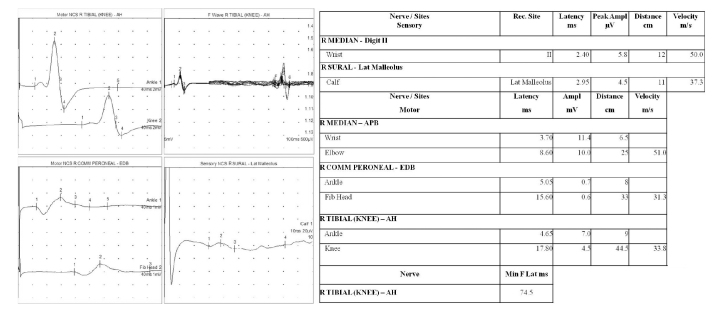
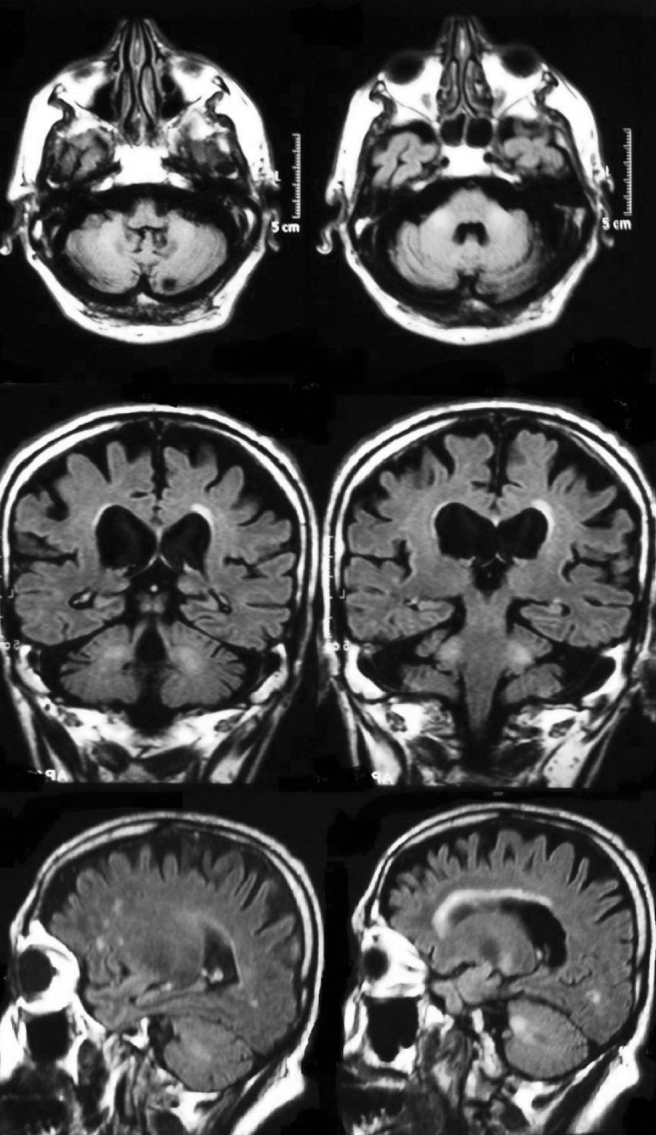
We report a typical fragile X-associated tremor/ataxia syndrome (FXTAS) case with the consent of the patient. A 68-year-old man presented to our clinic with a 12-year history of progressive gait ataxia and bilateral hand tremor. The patient also experienced problems with impotence, occasional episodes of diarrhea/constipation, and lightheadedness. His family history revealed that his sister and her daughter had a history of premature ovarian failure, and his neurological examination revealed bradymimia, bilateral mild postural and action tremor with terminal dysmetria, and ataxic wide-based gait. Both loss of distal reflexes and reduction in vibratory sense were observed. A detailed neurocognitive evaluation revealed mild frontal-type dysfunction. His cranial MRI showed generalized cerebral atrophy and increased T2 signal intensity in bilateral middle cerebellar peduncles and lateral periventricular areas (Figure 1). Nerve conduction studies showed motor and sensory demyelinating polyneuropathy in his lower extremities (Figure 2). His heart rate variability test revealed autonomic system involvement toward parasympathetic activity, and his genetic test revealed expanded CGG repeat above 60 within the premutation range (55–200) in the fragile X mental retardation 1 (FMR1) gene.
Figure 1.
Cranial MRI showing generalized cerebral atrophy and increased T2 signal intensity in bilateral middle cerebellar peduncles and lateral periventricular areas
Figure 2.
Nerve conduction studies showing motor and sensory demyelinating polyneuropathy in the lower extremities
FXTAS is a late onset progressive degenerative movement disorder. Since the disorder was first found in 2001, the advancement of knowledge of this disorder has occurred very quickly (1). Its diagnostic criteria describe in 2003 first time in 26 patients with two main clinical features: ataxia and tremor (2). Associated features include parkinsonism, cognitive dysfunction, peripheral neuropathy, and autonomic dysfunction. Expanded CGG triplets in the premutation range (55–200 CGG) in the FMR1 gene are responsible for this syndrome (2,3,4,5). Pathological studies show that FXTAS is an inclusion disorder, likely to be related to an RNA toxicity mechanism precipitated by an increased level of FMR1 mRNA, which includes CGG expansion. The most prominent neuropathological features obtained from autopsy researches of FXTAS are as follows: ubiquitin-positive eosinophilic intranuclear inclusions in neurons and astrocytes throughout the brain and brainstem and spongiform changes in the white matter with mild axonal and myelin loss (3,4,5,6). The increased signal intensity in the middle cerebellar peduncle (MCP) has been incorporated in the diagnostic criteria for “definite” FXTAS (2,3,4). Bilateral MCP involvement though distinctive and consider major radiologic diagnostic criteria, but it is found in only approximately 64% of individuals with FXTAS and is not specific to FXTAS. In addition to major clinical criteria, neuropathic and autonomic dysfunctions, which are not take place in diagnostic criteria, commonly occur in FXTAS. Signs of peripheral neuropathy, including decreased reflexes and impaired vibration sense, which are most consistent with a large fiber sensory neuropathy in the distal lower extremities, are present in many affected male premutation carriers. Some individuals also have evidence of substantial autonomic dysfunction, including orthostatic hypotension, impotence, and progressive loss of bowel and bladder control. The severity of neuropathic signs correlates with CGG repeat length and ataxia severity. These neuropathic signs are associated with the fragile X premutation, presumably occurring through the same mechanism proposed for CNS disease: toxicity from expanded CGG repeat FMR1 mRNA (3,5). Our definite FXTAS patient also had these common disabling neuropathic findings, which are clearly revealed on electrophysiological evaluation. Although there are many reports about peripheral neuropathy in FMR1 premutation carriers with FXTAS, this common feature has not been added to the diagnostic criteria (1,2,5,7,8). Postmortem pathological analysis of individuals with FXTAS has shown this widespread central and peripheral nervous system and non-nervous system involvement (3,6,9). FXTAS is a late life neurodegenerative disorder involved in both the central and peripheral nervous systems. Although tremor and ataxia are the hallmarks of this widespread disorder, the phenotype is highly variable. The diagnostic criteria can be rearranged in light of these miscellaneous well-defined variable clinical symptoms (10). Nearly a decade after its clinical characterization, FXTAS is potentially under-recognized and misdiagnosed. We need to be familiar of the variable features of FXTAS to prevent diagnostic delay. Early diagnosis is important to ensure genetic counseling for the family.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Hagerman RJ, Leehey M, Heinrichs W, Tassone F, Wilson R, Hills J, Grigsby J, Gage B, Hagerman PJ. Intention tremor, parkinsonism, and generalized brain atrophy in male carriers of fragile X. Neurology. 2001;57:127–130. doi: 10.1212/wnl.57.1.127. http://dx.doi.org/10.1212/WNL.57.1.127. [DOI] [PubMed] [Google Scholar]
- 2.Jacquemont S, Hagerman RJ, Leehey M, Grigsby J, Zhang L, Brunberg JA, Greco C, Des Portes V, Jardini T, Levine R, Berry-Kravis E, Brown WT, Schaeffer S, Kissel J, Tassone F, Hagerman PJ. Fragile X premutation tremor/ataxia syndrome: molecular, clinical, and neuroimaging correlates. Am J Hum Genet. 2003;4:869–878. doi: 10.1086/374321. http://dx.doi.org/10.1086/374321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry-Kravis E, Abrams L, Coffey SM, Hall DA, Greco C, Gane LW, Grigsby J, Bourgeois JA, Finucane B, Jacquemont S, Brunberg JA, Zhang L, Lin J, Tassone F, Hagerman PJ, Hagerman RJ, Leehey MA. Fragile X-associated tremor/ataxia syndrome: clinical features, genetics, and testing guidelines. Mov Disord. 2007;14:2018–2030. doi: 10.1002/mds.21493. http://dx.doi.org/10.1002/mds.21493. [DOI] [PubMed] [Google Scholar]
- 4.Juncos JL, Lazarus JT, Graves-Allen E, Shubeck L, Rusin M, Novak G, Hamilton D, Rohr J, Sherman SL. New clinical findings in the fragile X-associated tremor ataxia syndrome (FXTAS) Neurogenetics. 2011;12:123–135. doi: 10.1007/s10048-010-0270-5. http://dx.doi.org/10.1007/s10048-010-0270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berry-Kravis E, Goetz CG, Leehey MA, Hagerman RJ, Zhang L, Li L, Nguyen D, Hall DA, Tartaglia N, Cogswell J, Tassone F, Hagerman PJ. Neuropathic features in fragile X premutation carriers. Am J Med Genet A. 2007;143:19–26. doi: 10.1002/ajmg.a.31559. http://dx.doi.org/10.1002/ajmg.a.31559. [DOI] [PubMed] [Google Scholar]
- 6.Hall DA, O’keefe JA. Fragile x-associated tremor ataxia syndrome: the expanding clinical picture, pathophysiology, epidemiology, and update on treatment. Tremor Other Hyperkinet Mov (N Y) 2012;2 doi: 10.7916/D8HD7TDS. pii: tre-02-56-352-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hagerman RJ, Coffey SM, Maselli R, Soontarapornchai K, Brunberg JA, Leehey MA, Zhang L, Gane LW, Fenton-Farrell G, Tassone F, Hagerman PJ. Neuropathy as a presenting feature in fragile X-associated tremor/ataxia syndrome. Am J Med Genet A. 2007;143A:2256–2260. doi: 10.1002/ajmg.a.31920. http://dx.doi.org/10.1002/ajmg.a.31920. [DOI] [PubMed] [Google Scholar]
- 8.Soontarapornchai K, Maselli R, Fenton-Farrell G, Tassone F, Hagerman PJ, Hessl D, Hagerman RJ. Abnormal nerve conduction features in fragile X premutation carriers. Arch Neurol. 2008;65:495–498. doi: 10.1001/archneur.65.4.495. http://dx.doi.org/10.1001/archneur.65.4.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunsaker MR, Greco CM, Spath MA, Smits APT, Navarro CS, Tassone F, Kros JM, Severijnen LA, Berry-Kravis E, Berman RF, Hagerman PJ, Willemsen R, Hagerman RJ, Hukema RK. Widespread non-central nervous system organ pathology in fragile X premutation carriers with fragile X-associated tremor/ataxia syndrome and CGG knock-in mice. Acta Neuropathol. 2011;122:467–479. doi: 10.1007/s00401-011-0860-9. http://dx.doi.org/10.1007/s00401-011-0860-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Apatis E, Blancher A, Meissner WG, Guyant-Maréchal L, Maltete D, De Broucker T, Legrand AP, Bounzenada H, Thanh HT, Sallansonnet-Froment M, Wang A, Tison F, Roué-Jagot C, Sedel F, Charles P, Whalen S, Heron D, Thobois S, Poisson A, Lesca G, Ouvrard-Hernandez AM, Fraix V, Palfi S, Habert MO, Gaymard B, Dussaule JC, Pollak P, Vidailhert M, Durr A, Barbot JC, Gourlet V, Brice A, Anheim M. FXTAS: new insights and the need for revised diagnostic criteria. Neurology. 2012;79:1898–1907. doi: 10.1212/WNL.0b013e318271f7ff. http://dx.doi.org/10.1212/WNL.0b013e318271f7ff. [DOI] [PubMed] [Google Scholar]