Abstract
Objective
To assess the effects of winter/summer school breaks on occurrences of influenza-like illness (ILI).
Methods
We jointly analysed ILI surveillance data with the timing of school breaks in a temperate district in Beijing, China from 2008 to 2015. ILI incidence rate ratios (IRRs) of schoolchildren (5–14 and 15–24 years of age) to adults (25–59 and >60 years of age) were used to measure the age shift of ILI incidence before, during and after the 4-week winter/7-week summer breaks. Serfling-based Poisson regression model with adjustment for unmeasured confounders was built to further assess the effect of winter school breaks.
Results
ILI incidences were consistently lower during winter breaks than before winter breaks for all age groups. IRRs of younger schoolchildren aged 5–14 to adults were higher during winter school breaks than before breaks, while the opposite was true for the IRRs of older schoolchildren aged 15–24 to adults. Schoolchildren-to-adults IRRs during summer breaks were significantly lower than before or after school breaks (p<0.001).
Conclusions
Both winter and summer breaks were associated with reductions of ILI incidences among schoolchildren and adults. Our study contributes additional evidence on the effects of school breaks on ILI incidence, suggesting school closure could be effective in controlling influenza transmission in developing countries.
Keywords: incidence rate, influenza-like illness, school break
Strengths and limitations of this study.
We assessed the impact of school breaks on influenza activity.
Age shift of influenza-like illness incidence from schoolchildren to adults during school breaks indicated a reduction of influenza transmission in schoolchildren.
Serfling-based Poisson model was built to adjust for unmeasured confounders.
Residual confounding such as population mobility, change of health-seeking behaviour may exist.
Introduction
Schoolchildren play a major role in the spread of influenza considering their high clinical attack rates, high social contact rates and increased viral shedding compared with adults.1 Reactive school closure at the initial phase of a pandemic is considered as an effective non-pharmaceutical intervention to mitigate the spread of influenza. Both schoolchildren and their caregivers are expected to have a lower risk of infection after school closure by altering social mixing patterns.2 Several empirical studies have confirmed the effects of school closure on reducing influenza virus transmission after immediate closure of schools at an early stage of a pandemic, including studies from Hong Kong,3 France,4 Germany,5 eight European countries,6 Canada7 and USA.8
However, the assessment of effects of school closure on influenza transmission remains challenging. Reactive school closure during an influenza pandemic was often accompanied by other control measures such as intensive screening, border control measures and improved sanitation, which may confound the assessment of effects of school closure on influenza incidence. To differentiate the effects of school closure from other accompanied interventions and changed health-seeking behaviour, some studies have evaluated the effects of school closure on influenza transmission by focusing on school breaks rather than reactive school closures. As school calendars are usually set at the beginning of each school term, observed changes of influenza incidence before, during and after school breaks are believed to be less confounded than school closures aimed to control a pandemic.9 10 Significant associations between winter school breaks and temporary reductions of influenza-like illness (ILI) incidence have been found in Chile10 and Argentina,9 as children were less likely to be gathered during school breaks thus reducing the chance of influenza transmission. We hypothesised that the 4-week winter/7-week summer breaks in China might also be relevant to ILI incidence reductions among schoolchildren and adults. Our study aims to assess the effects of winter/summer school breaks on ILI incidence by estimating the ILI incidence ratio of schoolchildren to adults before, during and after the breaks in Xicheng District, Beijing, China.
Methods
Data
Beijing is located in northeastern China and has a temperate and continental climate with four distinct seasons. Xicheng District is located in the centre of Beijing. Weekly district-wide ILI time series during 2008–2015 was obtained from Beijing Medical Institutions in Communicable Disease Surveillance and Early Warning System. ILI was defined as fever (temperature of 38°C or greater) and a cough and/or a sore throat in the absence of a known cause other than influenza. The ILI reporting system recorded weekly ILI cases into five age groups (0–4, 5–14, 15–24, 25–59 and 60 years or older). Beijing Children's Hospital, affiliated with Capital Medical University is one of the sentinel hospitals for ILI surveillance, and accounts for more than half of the total paediatric outpatient visits in Beijing. To render our data more representative of ILI rates across the entire Beijing population, we age-standardised our ILI visit data in Xicheng District to the age distribution of Beijing's population. Age-specific population sizes in Xicheng District were collected from China's 2010 population census. We assumed that the age-stratified population remained constant over the study period. We ignored the immunised population as the influenza vaccination coverage was below 3% in the general population.
School calendars for winter/summer breaks of primary and secondary schools in Beijing were obtained directly from Beijing Municipal Education Commission. School calendars were usually announced ahead of each academic year. Winter breaks were often in January and February, which lasts for 4 weeks and covered the 7-day statutory holidays for national Chinese New Year. Summer breaks are in July and August, which last for 7 weeks. The exact starting dates of winter/summer school breaks varied slightly across years and schools. On average, winter breaks in Beijing started at the 5th week and ended at the 8th week, while summer breaks started at the 29th week and ended at the 35th week.
Data analysis
ILI incidence rate ratios (IRRs) of schoolchildren (5–14 and 15–24 years of age) to adults (aged 25–59 and 60 years or older) were used to measure the age shift of ILI incidence before, during and after the 4-week winter/7-week summer breaks. In this study, we used 25 years of age as the cut-off point for schoolchildren and adults, because the ILI surveillance system in Beijing reported weekly ILI numbers by age groups of 0–4, 5–14, 15–24, 25–59 and 60 years or older, without specific age for each case. Owing to data availability, we grouped individuals under 25 years of age as schoolchildren, which was close to but might be a bit older than the true cut-off for schoolchildren.
Similar to previous literature,10–12 we compared schoolchildren-to-adults IRRs before, during and after the winter/summer breaks using two-sided Z tests. As the reduction in the ILI incidence during the winter break was maintained on average for 2 weeks after the end of the winter break, we allowed a 2-week window and defined before/after school breaks as 2 weeks apart from the break. We considered a 4-week window before and after the winter/summer break as a sensitivity analysis.
In order to control the effects of unmeasured confounders of long-term and seasonal trends, we built a Serfling-specified Poisson regression model to assess the effect of winter breaks. A vector of dummy variables for each year was considered and sinusoidal terms of weeks were added in the Poisson model to adjust for long-term and seasonal trends, respectively. As weekly adjacent ILI visits were temporally correlated, we further added an autocorrelated regression term to adjust for autocorrelation in the Poisson model.13 Details of the model can be found in online supplementary appendix and tables S1-S2. Model fitting was evaluated by pseudo R2 values. IRRs of during/after to before winter breaks were used to evaluate the change of ILI incidence before, during and after winter breaks in each age group. IRRs of during/after to before winter breaks smaller than 1 indicated that ILI visits during/after winter breaks were lower than those before winter breaks. We presented the estimates as weekly IRRs, which was calculated by dividing the weekly ILI incidence during/after winter breaks to an average of ILI incidence 2 weeks before winter breaks. Data analyses were conducted in R V.3.2.3 using package nlme.14
bmjopen-2016-013159supp_appendix.pdf (1.1MB, pdf)
Results
From January 2008 to December 2015, Center for Disease Control and Prevention of Xicheng District in Beijing recorded 1 294 279 ILI visits and a total of 41 269 165 clinic attendances. Percentage of number of ILI visits to number of total clinic attendances (ILI%) had been widely used as an indicator for influenza activities.15 Figure 1A illustrates age-specific trends in weekly ILI% throughout 8 years. Peaks of influenza activities appear from end of December to middle of January across different age groups in the past years. Summer peaks were observed for groups of age 0–4 and 5–14 without a consistent annual pattern. During the winter school breaks, ILI incidence decreased substantially in age groups of 5–14 and 15–24, but modestly in age groups over 25 (figure 1B). During the summer school breaks, only ILI incidence in age group of 5–14 reduced dramatically, while levelled off for other age groups (figure 1B). A decline of schoolchildren-to-adults IRR during school breaks implied an age shift in patients with ILI towards adults, and further suggested a reduction of influenza transmission among schoolchildren.
Figure 1.
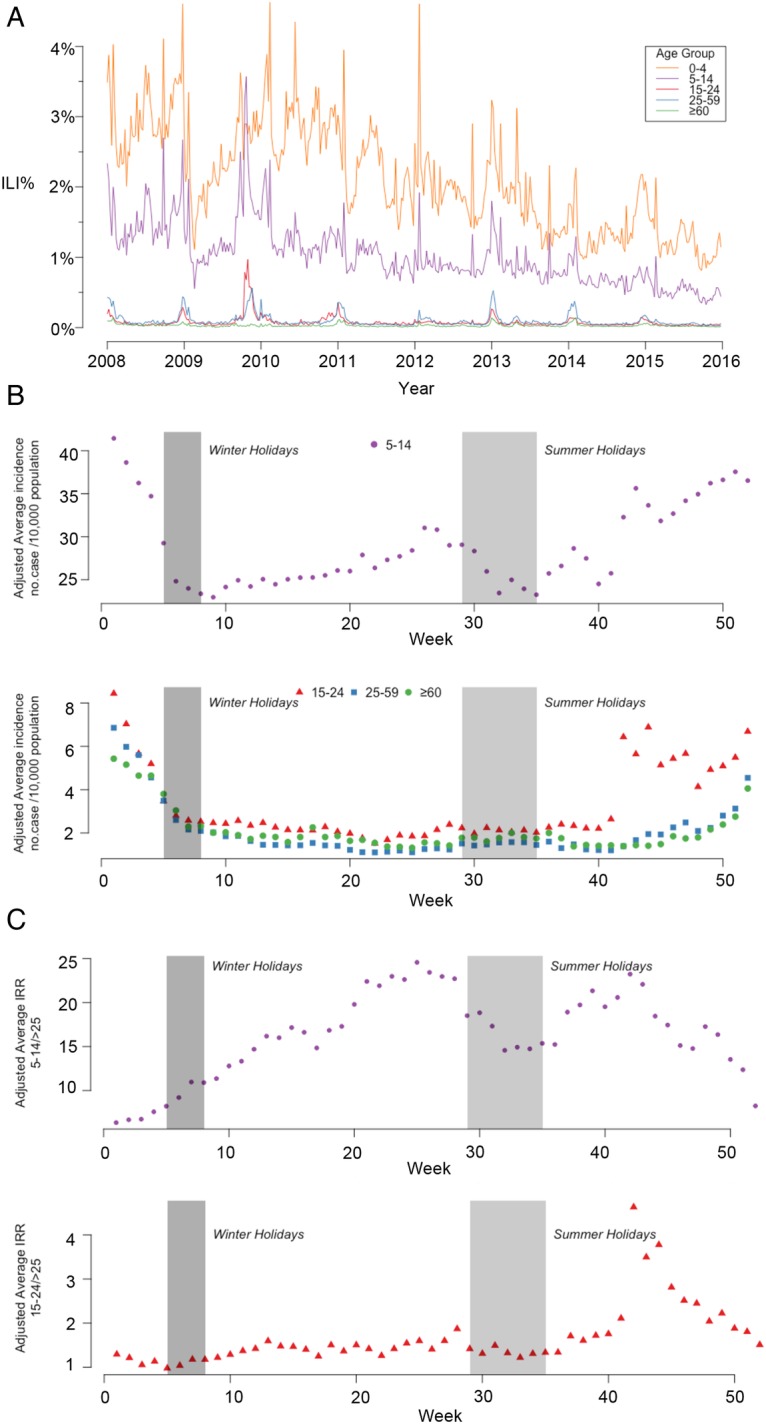
Age-specific ILI incidence rates, adjusted average ILI incidence rates, adjusted average ILI IRRs of influenza surveillance data by week in Beijing, 2008–2015. (A) Weekly ILI incidence rates for five age groups. (B) Adjusted average ILI incidence per 10 000 persons by week. (C) Adjusted average ILI incidence rate ratio of schoolchildren-to-adult by week. The upper plot is IRRs of age 5–14 to adults; the lower plot is IRRs of age 15–24 to adults. ILI, influenza-like illness; IRR, incidence rate ratio.
IRRs of younger schoolchildren aged 5–14 to adults was higher during winter school breaks than before breaks, while the opposite was true for the IRRs of older schoolchildren aged 15–24 to adults (table 1, figure 1C). During summer breaks, schoolchildren-to-adults IRRs were significantly lower than those of 2-week before or after school breaks (p<0.001). To be specific, IRRs of age 5–14 to age above 60 had declined by 13.3% (95% CI 3.59%, 22.1%). The above conclusion was robust when we considered a 4-week window before and after winter/summer break (see online supplementary table S3).
Table 1.
ILI IRRs of schoolchildren to adults during 2-week periods surrounding winter/summer breaks, by age group, Beijing, 2008–2015
| ILI IRR (95% CI) |
p Value* |
||||
|---|---|---|---|---|---|
| Age group | Before school break | During school break | After school break | Before to during | During to after |
| Winter | |||||
| 5–14 | |||||
| 25–59 | 7.26 (6.99 to 7.53) | 9.95 (9.61 to 10.3) | 13.6 (12.9 to 14.4) | <0.001 | <0.001 |
| ≥60 | 8.02 (7.50 to 8.58) | 9.20 (8.67 to 9.76) | 13.3 (12.1 to 14.7) | 0.003 | <0.001 |
| 15–25 | |||||
| 25–59 | 1.12 (1.06 to 1.19) | 1.03 (0.98 to 1.09) | 1.33 (1.22 to 1.45) | 0.04 | <0.001 |
| ≥60 | 1.24 (1.14 to 1.34) | 0.96 (0.89 to 1.03) | 1.30 (1.16 to 1.47) | <0.001 | <0.001 |
| Summer | |||||
| 5–14 | |||||
| 25–59 | 21.6 (20.2 to 23.0) | 17.0 (16.5 to 17.6) | 20.7 (19.4 to 22.1) | <0.001 | <0.001 |
| ≥60 | 19.5 (17.4 to 21.7) | 14.3 (13.6 to 15.1) | 19.5 (17.4 to 21.9) | <0.001 | <0.001 |
| 15–25 | |||||
| 25–59 | 1.63 (1.48 to 1.79) | 1.41 (1.34 to 1.48) | 1.71 (1.56 to 1.88) | 0.008 | <0.001 |
| ≥60 | 1.47 (1.29 to 1.67) | 1.19 (1.11 to 1.27) | 1.62 (1.42 to 1.85) | 0.004 | <0.001 |
*Small p values indicate that the IRR for the period before the break is significantly higher than that for the period during the break (or the IRR for the period during the break is significantly higher than that for the period after the break).
ILI, influenza-like illness; IRR, incidence rate ratio.
Since long-term trend and seasonal pattern of ILI visits could be two confounders in the previous analysis of IRRs, we used a Poisson regression model to assess the effect of school breaks on ILI incidence. The models generally well fitted the observed ILIs with adjusted pseudo R2 values for the five age groups (0–4, 5–14, 15–24, 25–59 and 60 years or older) ranging from 0.44 to 0.56. After incorporating the autocorrelation within error terms, we estimated IRRs of during/after to before winter break and their CIs (table 2). During-to-before IRRs were smaller than 1 for all age groups. However, the starting time and duration of the ILI reduction varied across different age groups. In age group of 15–24, ILI incidence dropped substantially by around 40% during the whole school break and lasted for 4 weeks thereafter. Declines of during-to-before IRRs for age groups of 0–4 and 5–14 were also observable but not necessarily smaller than declines in adults (table 2). For adults (age 25–59 and 60 years or older), ILI reductions were statistically significant in the second and third week of the break and lasted for about 2 weeks (table 2). Among all age groups, incidence of ILI visits returned to regular patterns with none of after–before IRRs statistically significant 3 weeks after the end of winter breaks (table 2).
Table 2.
Estimated ILI IRRs of visits by Poisson regression surrounding winter breaks, by age group, Beijing, 2008–2015
| Age | During winter break |
After winter break |
||||||
|---|---|---|---|---|---|---|---|---|
| 1st week | 2nd week | 3rd week | 4th week | 1st week | 2nd week | 3rd week | 4th week | |
| 0–4 | 0.96 (0.90–1.03) | 0.89 (0.81–0.98) | 0.89 (0.81–0.98) | 0.84 (0.75–0.94) | 0.86 (0.77–0.97) | 1.00 (0.89–1.12) | 1.03 (0.93–1.14) | 1.07 (0.98–1.18) |
| 5–14 | 0.89 (0.81–0.98) | 0.89 (0.78–1.01) | 0.84 (0.73–0.97) | 0.84 (0.73–0.98) | 0.81 (0.70–0.95) | 1.02 (0.88–1.19) | 1.03 (0.89–1.17) | 1.03 (0.91–1.16) |
| 15–24 | 0.61 (0.50–0.74) | 0.60 (0.47–0.78) | 0.65 (0.48–0.86) | 0.64 (0.47–0.87) | 0.76 (0.56–1.05) | 0.80 (0.59–1.09) | 0.91 (0.68–1.22) | 0.96 (0.74–1.23) |
| 25–59 | 0.92 (0.77–1.09) | 0.76 (0.90–0.96) | 0.72 (0.55–0.95) | 0.80 (0.60–1.06) | 0.90 (0.67–1.20) | 0.86 (0.64–1.14) | 1.07 (0.82–1.40) | 1.10 (0.87–1.38) |
| ≥60 | 0.90 (0.69–1.18) | 0.76 (0.54–1.06) | 0.61 (0.42–0.88) | 0.68 (0.46–1.01) | 0.64 (0.43–0.94) | 0.83 (0.56–1.23) | 0.82 (0.56–1.19) | 0.88 (0.62–1.23) |
Boldface indicates statistically significant changes at the 0.05 confidence level.
*IRRs were used to estimate whether incidence of ILI-associated visits in a particular week were lower, higher, or did not deviate from the expected seasonal ILI patterns. Each row represents a separate regression model.
ILI, influenza-like illness; IRR, incidence rate ratio.
Discussion
Consistent with other studies in China and other temperate regions,16 we found peaks of influenza in Beijing appeared synchronised across age groups in most winters and springs during 2008-2015. For age groups of 0–4 and 5–14, peaks of ILI% had also been detected before summer breaks, which might be driven by final examination stress, poor classroom ventilation, incompletely developed immune system and other unfavourable factors related to young children. Since ILI visits could be caused by influenza, respiratory tract infection and other illness, ILI% is a broad indicator of respiratory disease activity not entirely specific for influenza and could be affected by changes in health-seeking behaviour.10 Therefore, laboratory surveillance data are necessary for further conclusions on age-specific seasonal influenza activities from a public health perspective.
In this study, our findings generally support that winter/summer school breaks could achieve temporary reductions in ILI incidence rates, especially among schoolchildren (age of 5–14 and 15–24). In consistency with previous empirical studies in Chile, USA and European countries,10 17 the average reduction in schoolchildren-to-adult IRRs in Beijing lasted for up to 2 weeks (table 1) after school sessions resumed, and this allowed a few successive chains of transmission for influenza virus to reach full-scale transmission.10 The finding that ILI incidence rates decreased substantially in schoolchildren yet modestly in adults during winter breaks is consistent with past work on age-specific influenza transmission.17 Moreover, the reduction in ILI during the school holidays went beyond the dips in ILI ±4 weeks surrounding the holiday weeks (see online supplementary appendix), further supporting our suggestion of lower influenza transmission in schoolchildren during school breaks.
The finding that IRRs of schoolchildren aged 5–14 to adults increased significantly in winter breaks is inconsistent with findings of influenza activities in Chile.10 Although ILI incidence rates of age group 5–14 had been reduced by 26.3% (95% CI 24.9% to 27.7%) after entering winter breaks in 2008-2015, reductions in ILI incidence rates for adults' groups were even larger and thus resulted in increased IRRs of age group 5–14 to adult. In addition to different strains of influenza circulating in a certain year, there could be many other human behaviour factors playing a role in regulating seasonal age-specific ILI visits in China. For example, under pressure of final examinations before winter breaks, some schoolchildren are unwilling to spare any time to see a doctor when they had influenza-like symptoms. During Chinese Spring Festival vacation (covered by winter breaks), most of migrant workers in Beijing went back to their hometown18 19 and local people who stayed in the city were unwilling to seek medical advice for fear of missing family gatherings (see online supplementary figure S1). Moreover, apparent drops of total outpatient visits were observed in every January (see online supplementary figure S1), suggesting the change of healthcare-seeking behaviour around the holidays. In fact, IRRs of schoolchildren aged 5–14 to adults during Spring Festival were significantly higher than other weeks within winter breaks.20 21 Consequently, we infer the enhanced IRRs of schoolchildren aged 5–14 to adults in winter breaks are due to integrated effects of Spring Festival, population migration and changes in health-seeking behaviour.
We established an autocorrelated Poisson regression model to control the effect of potential confounders that may distort age-specific ILI incidence rates, such as seasonal change of ILI visits and year. We found a significant reduction in ILI incidence rates for age group of 5–14 when entering winter breaks, compared with those of 2 weeks before (IRR 0.89, 95% CI (0.81 to 0.98)). However, the reduction is less significant when comparing with the rates throughout the entire break for the adults' groups. The phenomenon that reduction of ILI incidence rates for age above 60 was larger than those for age 25–59 and close to those for age 15–24 (table 2) could be due to age-specific health-seeking behaviour, immune system characteristics and residual confounders of seasonal ILI visits. Although a Serfling model has been adopted, our model is still relatively conservative in controlling seasonal pattern of ILI because timing of peaks of influenza activities had severe overlaps with timing of winter breaks, and the overfitting could underestimate the effect of winter breaks on decrease of IRRs. Therefore, additional analysis that considers high variability in the temporal relationship between winter breaks and weekly ILI rates across influenza seasons are needed and incorporating environmental factors or human behaviour data may better clarify the relationship between age-specific influenza activity and winter breaks.
We quantified the reduction in IRRs, and also analysed age-specific timing of the decline in ILI incidence. Similar to the study in Argentina,9 a stepwise trend of the effect on ILI had been detected. Age groups of 5–14 and 15–24 experienced the initial significant decrease in ILI during the first week of winter breaks and lasted for 4 weeks. The reduction effect was caught up by other age groups, and lasted for 4 weeks for 0–4 age group and 2 weeks for adults' groups. The spread of influenza likely varies according to population subgroup.22 Overall, our study supports winter breaks as effective means to prevent the epidemic of winter-to-spring influenza activities.
Schoolchildren-to-adults IRRs consistently decreased during summer breaks compared with 2-week before summer breaks. According to our analysis, protective effect of summer breaks on schoolchildren of age 5–14 was more obvious than that on adults. We emphasise that results on effects of summer breaks on influenza activities should be interpreted with caution, because respiratory viruses other than influenza virus were active during summer that could make clinical surveillance less specific to influenza.23
Although our study sustains the positive effect of school breaks in controlling influenza activities, insufficient evidence is provided on the effect of school breaks in order to support the decision on duration of the break and the timing with respect to the influenza season. Furthermore, the economic cost of school breaks that is mainly due to absenteeism of working parents who have to stay home to take care of their children remains difficult to estimate.24 Further analysis of the environmental or social factors influencing the transmission of seasonal and pandemic influenza is required in order to provide additional information for policymakers and public health officials to use when considering measures to control pandemic influenza.
Footnotes
Contributors: All the authors listed meet the criteria for authorship. YC, X-LW, ZW, XZ, GQ, JS and XS conceived and designed the experiments. YC, JS, XS, JQ, ZX, JR and DQ performed the experiments. X-LW, JJ, ZW, XZ and GQ analysed the data. XZ, JJ and X-LW wrote the manuscript.
Funding: This work was partially supported by the Youth National Nature and Science Foundation of China (11501124; 81602936) and the National Nature and Science Foundation of China (11371100).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Longini IM Jr, Koopman JS, Monto AS et al. Estimating household and community transmission parameters for influenza. Am J Epidemiol 1982;115:736–51. 10.1093/oxfordjournals.aje.a113356 [DOI] [PubMed] [Google Scholar]
- 2.Glass LM, Glass RJ. Social contact networks for the spread of pandemic influenza in children and teenagers. BMC Public Health 2008;8:61 10.1186/1471-2458-8-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu JT, Cowling BJ, Lau EH et al. School closure and mitigation of pandemic (H1N1) 2009, Hong Kong. Emerg Infect Dis 2010;16:538–41. 10.3201/eid1603.091216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cauchemez S, Ferguson NM, Wachtel C et al. Closure of schools during an influenza pandemic. Lancet Infect Dis 2009;9:473–81. 10.1016/S1473-3099(09)70176-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mikolajczyk RT, Akmatov MK, Rastin S et al. Social contacts of school children and the transmission of respiratory-spread pathogens. Epidemiol Infect 2008;136:813–22. 10.1017/S0950268807009181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hens N, Ayele GM, Goeyvaerts N et al. Estimating the impact of school closure on social mixing behaviour and the transmission of close contact infections in eight European countries. BMC Infect Dis 2009;9:187 10.1186/1471-2334-9-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Earn DJ, He D, Loeb MB et al. Effects of school closure on incidence of pandemic influenza in Alberta, Canada. Ann Intern Med 2012;156:173–81. 10.7326/0003-4819-156-3-201202070-00005 [DOI] [PubMed] [Google Scholar]
- 8.Halloran ME. On influenza and school closings: time for prospective studies. Epidemiology 2009;20:793–5. 10.1097/EDE.0b013e3181ba43c9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garza RC, Basurto-Davila R, Ortega-Sanchez IR et al. Effect of winter school breaks on influenza-like illness, Argentina, 2005–2008. Emerg Infect Dis 2013;19:938–44. 10.3201/eid1906.120916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chowell G, Towers S, Viboud C et al. Rates of influenza-like illness and winter school breaks, Chile, 2004–2010. Emerg Infect Dis 2014;20:1203–7. 10.3201/eid2007.130967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chowell G, Echevarria-Zuno S, Viboud C et al. Characterizing the epidemiology of the 2009 influenza A/H1N1 pandemic in Mexico. PLoS Med 2011;8:e1000436 10.1371/journal.pmed.1000436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chowell G, Viboud C, Munayco CV et al. Spatial and temporal characteristics of the 2009 A/H1N1 influenza pandemic in Peru. PLoS ONE 2011;6:e21287 10.1371/journal.pone.0021287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowpertwait PSP, Metcalfe AV. Introductory time series with R. New York: Springer, 2008. [Google Scholar]
- 14.Faraway JJ. Linear models with R. 2nd edn. Boca Raton, FL: Taylor & Francis Group, 2014. [Google Scholar]
- 15.Prevention UCfDCa. Overview of Influenza Surveillance in the United State 2010. http://www.cdc.gov/flu/weekly/overview.htm
- 16.Yu H, Alonso WJ, Feng L et al. Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: spatio-temporal modeling of surveillance data. PLoS Med 2013;10:e1001552 10.1371/journal.pmed.1001552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cauchemez S, Valleron AJ, Boelle PY et al. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature 2008;452:750–4. 10.1038/nature06732 [DOI] [PubMed] [Google Scholar]
- 18.Gu C, Cai J, Zhang W et al. A study on the patterns of migration in Chinese large and medium cities. Acta Geogr Sin 1999;54:204–12. [Google Scholar]
- 19.Ding J, Liu Z, Cheng D et al. Areal differentiation of inter-provincial migration in China and characteristics of the flow field. Acta Geogr Sin 2005;60:1. [Google Scholar]
- 20.Xu C, Wang J, Wang L et al. Spatial pattern of severe acute respiratory syndrome in-out flow in 2003 in Mainland China. BMC Infect Dis 2014;14:721 10.1186/s12879-014-0721-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang JF, Meng B, Zheng XY et al. [Analysis on the multi-distribution and the major influencing factors on severe acute respiratory syndrome in Beijing]. Zhonghua Liu Xing Bing Xue Za Zhi 2005;26:164–8. [PubMed] [Google Scholar]
- 22.Cowling BJ, Lau EH, Lam CL et al. Effects of school closures, 2008 winter influenza season, Hong Kong. Emerg Infect Dis 2008;14:1660–2. 10.3201/eid1410.080646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thompson WW, Shay DK, Weintraub E et al. Influenza-associated hospitalizations in the United States. JAMA 2004;292:1333–40. 10.1001/jama.292.11.1333 [DOI] [PubMed] [Google Scholar]
- 24.Sadique MZ, Adams EJ, Edmunds WJ. Estimating the costs of school closure for mitigating an influenza pandemic. BMC Public Health 2008;8:135 10.1186/1471-2458-8-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-013159supp_appendix.pdf (1.1MB, pdf)


