Abstract
A man aged 65 years presented with symptomatic anaemia without overt gastrointestinal bleeding. An oesophagogastroduodenoscopy (EGD) was performed and he was found to have a large ulcerated pedunculated Brunner's gland hamartoma in the duodenal bulb. The polyp was resected using snare cautery in forward and retroflexed positions. Colonoscopy was also performed and a few diminutive polyps were resected. A year later, the patient returned for a surveillance EGD, and no residual polyp was noted. Haemoglobin and iron studies normalised within a few months after polypectomy, with resolution of symptoms.
Background
Brunner's gland hamartoma (BGH) is an extremely rare cause of iron deficiency anaemia. As shown in our case report, it can be treated successfully with endoscopic resection. There have been no prior published case reports of the use of the retroflexion technique for polypectomy in the first part of the duodenum. As shown here, retroflexion can be performed safely in the first part of the duodenum.
Case presentation
A man aged 65 years with a history of hypertension presented with generalised weakness and fatigue for 3 weeks. He denied overt gastrointestinal bleeding. Physical examination was unremarkable. Laboratory evaluation revealed haemoglobin of 8.5 mg/dL with a mean corpuscular volume (MCV) of 77 fL with iron studies consistent with iron deficiency (ferritin 10 ng/mL and transferrin saturation 3%). Oesophagogastroduodenoscopy (EGD) and colonoscopy were performed. EGD showed a 5 cm pedunculated polyp with an ulcerated surface extending from the pyloric channel to the second portion of the duodenum (figures 1 and 2). Given that this was a pedunculated, submucosal polyp, it was deemed to be amenable to complete endoscopic resection at the level of the stalk of the polyp without further work up. CT/EUS were not necessary in this particular case but could have been helpful if the lesion was not pedunculated. The polyp was resected endoscopically via snare cautery in the forward and retroflexed positions, given its large size and difficult position (figures 3 and 4). Retroflexion was performed by maximum deflection of both dials along with slight torque of the scope. Care was taken to avoid excessive pressure on the duodenal wall. Tighter bending section of the tip of the gastroscope made retroflexion possible in the narrow space of first part of the duodenum. After resection, clips were placed prophylactically to decrease the risk of postpolypectomy bleeding (figure 4). Histopathology showed BGH (figure 5). Colonoscopy was also performed and a few diminutive polyps were resected.
Figure 1.
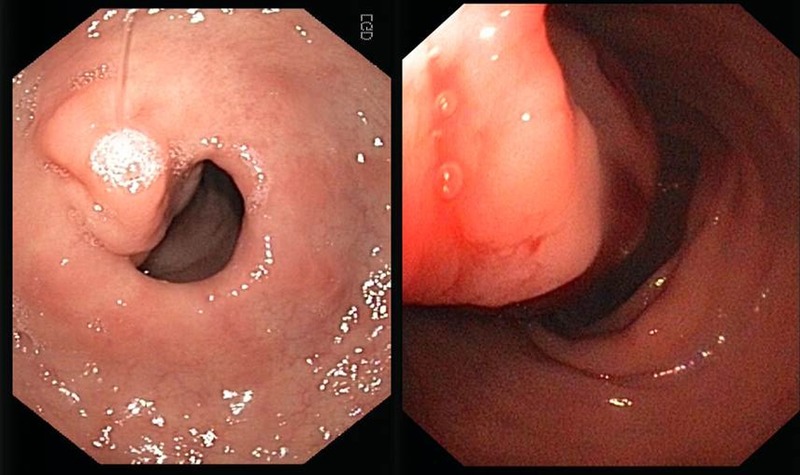
Large pedunculated polyp.
Figure 2.

Polyp extending to the second duodenum.
Figure 3.
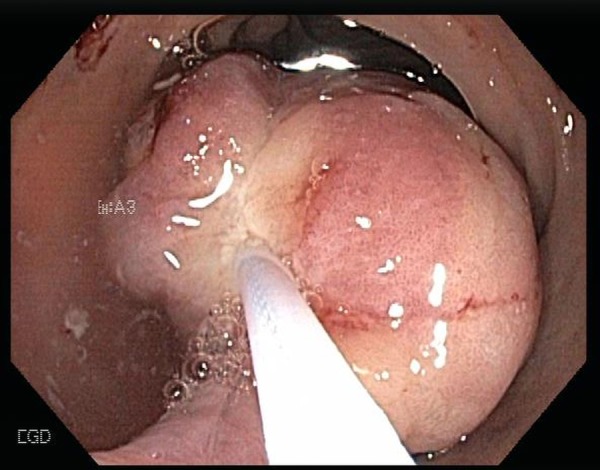
Polyp resection with snare cautery.
Figure 4.

Further resection and clip placement in retroflexion.
Figure 5.
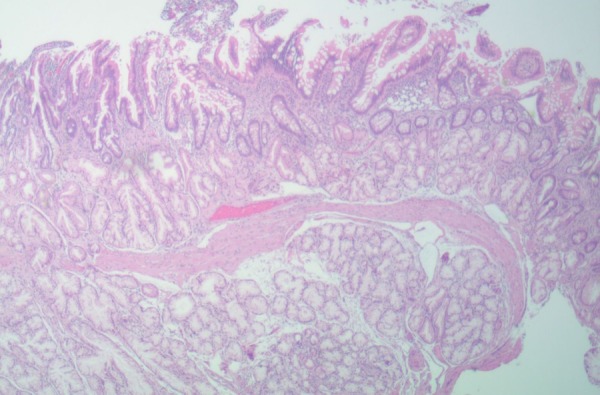
Brunner's gland hyperplasia—histology.
Outcome and follow-up
The patient underwent a repeat EGD after 1 year and no residual duodenal polyp was noted, which was expected, given initial complete resection through the stalk of the polyp. Haemoglobin and MCV normalised (15 mg/dL and 88 fL, respectively) in a few months after endoscopic polypectomy.
Discussion
BGH are extremely rare with an incidence of <0.01% reported in a single series of 215 000 autopsies.1 Their aetiology is unknown, but they may develop in response to peptic injury and, in some reports, Helicobacter pylori has been implicated.2 Most arise in the duodenal bulb, are pedunculated and range in size from 0.5 to 12 cm.3 The majority of them are asymptomatic and are typically found incidentally via imaging or endoscopy. Rarely, they can present with iron deficiency anaemia, bleeding, obstruction, or intussusception, or, if the ampulla is involved, with pancreatitis, obstructive jaundice or a biliary fistula.1 4 Resection is recommended to prevent complications and to differentiate BGH from other lesions such as adenomas, leiomyomas, lipomas, aberrant pancreatic tissue or malignancy.1 Diagnosis must be confirmed by histopathology. Management can include surgery (duodenostomy), though endoscopic resection, which is less invasive, is currently the preferred approach when possible.1 5 Endoscopic resection offers additional benefits of lower mortality and fewer complications.6 Our case highlights the importance of recognising BGH as a rare cause of iron deficiency anaemia and also demonstrates that a retroflexed position can be safely employed in first part of the duodenum to remove these lesions endoscopically, especially if the stalk is located in the duodenal bulb.
Learning points.
Brunner's gland hamartoma is a rare cause of iron deficiency anaemia.
Resection is recommended to prevent complications and to differentiate it from other lesions.
Polypectomy can be performed safely using the retroflexed position in the first part of the duodenum.
Footnotes
Contributors: SJ is responsible for drafting of the article, revision and final approval of the article. SP is responsible for drafting of the article, revision and final approval of the article. EL is responsible for final approval of the article. FA is responsible for revision and final approval of the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rocco A, Borriello P, Compare D et al. . Large Brunner's gland adenoma: case report and literature review. World J Gastroenterol 2006;12:1966–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kovacevic I, Ljubicic N, Cupic H et al. . Helicobacter pylori infection in patients with Brunner gland adenoma. Acta Med Croatica 2001;55:157–60. [PubMed] [Google Scholar]
- 3.Patel ND, Levy AD, Mehrotra AK et al. . Brunner's gland hyperplasia and hamartoma: imaging features with clinicopathologic correlation. Am J Roentgenol 2006;187:715–22. [DOI] [PubMed] [Google Scholar]
- 4.Mayoral W, Salcedo JA, Montgomery E et al. . Biliary obstruction and pancreatitis caused by Brunner gland hyperplasia of the ampulla of Vater: a case report and review of the literature. Endoscopy 2000;32:998–1001. doi:10.1055/s-2000-9623 [DOI] [PubMed] [Google Scholar]
- 5.Walden DT, Marcon NE. Endoscopic injection and polypectomy for bleeding Brunner gland hamartoma: case report and expanded literature review. Endoscopy 1998;47:403–7. [DOI] [PubMed] [Google Scholar]
- 6.Zhong YS, Shi Q, Wu HF et al. . Endoscopic resection for the treatment of duodenal Brunner's adenomas. J Laparoendosc Adv Surg Tech A 2012;22:904–9. doi:10.1089/lap.2012.0250 [DOI] [PubMed] [Google Scholar]


