Abstract
A 56-year-old male, who is an active intravenous drug abuser (IVDA) (heroin) with a history of diabetes, hypertension, chronic kidney disease, and hepatitis C-related liver cirrhosis, presented with generalized anasarca, bilateral pneumonic infiltrations, and heart failure. His blood cultures were positive for Pseudomonas aeruginosa and were treated with antibiotics. Echocardiogram showed multiple uncommon manifestations of left-sided endocarditis. Surprisingly, he did not have right-sided involvement. Furthermore, echocardiogram revealed undiagnosed large atrial septal defect suggesting a paradoxical seeding of infective vegetation. This case illustrates the uncommon manifestations of Pseudomonas endocarditis in an IVDA and indicates that it is very important to check comprehensively for an atrial septal defect or patent foramen ovale or any shunt in such high-risk patients who may be at risk for left-sided endocarditis which is catastrophic when compared to right-sided endocarditis. If detected early in IVDA patients, these shunts need to be closed to prevent paradoxical embolism of vegetation.
Keywords: Echocardiography, intravenous drug abuser, Pseudomonas endocarditis
Introduction
Pseudomonas endocarditis is rare, more commonly seen in intravenous drug abusers (IVDAs) (right-sided endocarditis, 90%) or hospital acquired, especially in immunocompromised patients or those with instrumentation (left-sided endocarditis, 10%).[1,2,3] Left-sided involvement has a high mortality of about 80%.[1,2] Here, we present a patient who is an IVDA, who developed uncommon cardiac manifestations of left-sided Pseudomonas endocarditis due to the presence of an undetected atrial septal defect without the involvement of right side of the heart.
Case Report
A 56-year-old male, who is an active IVDA (heroin) with long-standing history of diabetes, hypertension, chronic kidney disease (creatinine 204 mmol/L; glomerular filtration rate = 31 ml/min/1.73 m2), and hepatitis C-related liver cirrhosis/portal hypertension, with no past cardiac history presented with generalized anasarca, bilateral pneumonic infiltrations, and heart failure. Three sets of blood cultures grew Pseudomonas aeruginosa susceptible to piperacillin-tazobactam, cefepime, gentamicin, and ciprofloxacin. The transthoracic echocardiography showed large ostium secundum atrial septal defect with left-to-right shunt, vegetation over mitral and aortic valve with moderate-to-severe mitral and tricuspid regurgitation, and trivial aortic regurgitation. The left ventricular ejection fraction was 35% and right ventricular systolic pressure was 55 mmHg. There was mild circumferential pericardial effusion. Transesophageal echocardiographic (TEE) examination confirmed a large atrial septal defect [Figure 1a, arrowheads], a large parachute-shaped mass attached to aortic valve [Figure 1b, right arrowheads], and a large mass in the left atrial appendage [Figure 1b, left arrowheads and Video 1], suggestive of vegetation. In the longitudinal plane, TEE demonstrated multiple vegetation attached to mitral valve leaflets [Figure 2a, arrowheads] with a large fluttering saccular mass (1.4 cm × 4 cm) in the left atrium attached to the posterior mitral valve leaflet bulging into the left atrium, suggestive of mitral valve aneurysm [Figure 2a and b, arrowheads and Video 1]. Interestingly, on modified view, the left atrial mass intermittently resembled a “cat” face with prominent eyes, nose, and mouth [Figure 3 and Video 2] measuring 4.9 cm × 1.9 cm. There were no vegetation over tricuspid or pulmonic valve. In view of his severe comorbid problems, cardiac surgeons advised conservative therapy. He was treated with piperacillin-tazobactam 4.5 g twice daily. Gentamycin was not given in view of renal impairment. Over 3 weeks, he deteriorated with overlap hepatic encephalopathy and expired.
Figure 1.
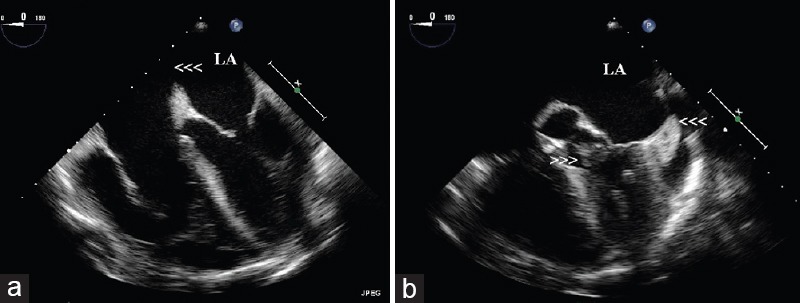
Transesophageal echocardiographic examination showing a large atrial septal defect (a, arrowheads), a large parachute-shaped mass attached to aortic valve (b, right arrowheads), and a large mass in the left atrial appendage (b, left arrowheads, Video 1), suggestive of vegetation in a patient with intravenous drug abuse and Pseudomonas endocarditis.
Figure 2.
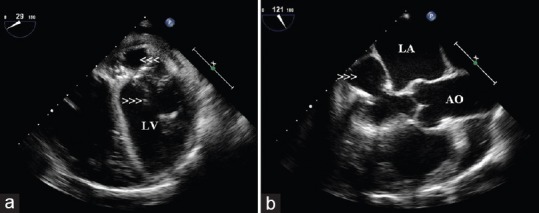
Transesophageal echocardiographic examination demonstrating multiple vegetation attached to mitral valve leaflets (a, arrowheads) with a large fluttering saccular mass (1.4 cm × 4 cm) in the left atrium attached to the posterior mitral valve leaflet bulging into the left atrium suggesting mitral valve aneurysm (a and b, arrowheads, Video 1) in a patient with intravenous drug abuse and Pseudomonas endocarditis.
Figure 3.
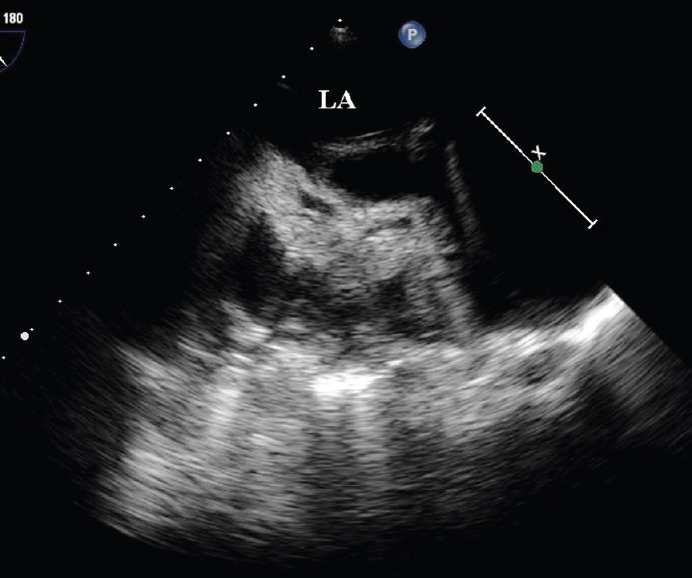
Transesophageal echocardiographic examination showing a large left atrial vegetation intermittently resembling a “cat” face with prominent eyes, nose, and mouth (Video 2) measuring 4.9 cm × 1.9 cm in a patient with intravenous drug abuse and Pseudomonas endocarditis.
Discussion
This case illustrates the uncommon cardiac manifestations of left-sided Pseudomonas endocarditis in an IVDA. There was no right-sided involvement, but due to the presence of an undetected atrial septal defect, there was fulminant left-sided involvement resulting in a mitral valve aneurysm and a rare intracardiac image of the left atrial vegetation resembling a “cat” face. An interesting feature about this case is paradoxical seeding of vegetation through atrial septal defect without the involvement of right side of the heart. As noted in this patient, mitral valve aneurysm was seen as a localized saccular bulge of the mitral leaflet toward the left atrium communicating with the left ventricle with systolic expansion and diastolic collapse. In one large survey, non-HACEK Gram-negative bacteria were present in 1.8% of the endocarditis cases with 4% reported in IVDAs.[4] Escherichia coli (29%) and P. aeruginosa (14%) were the common organisms, and nearly 50% of the cases needed surgery with overall in-hospital mortality of 24%.[4] In a case series of Pseudomonas endocarditis, the best antimicrobial regimen in patients with normal renal function included a combination of cefepime, 6 g/day, in three divided doses, plus high-dose tobramycin, 8 mg/kg/day, given as a single daily dose for 6 weeks along with surgery when indicated.[5] This case illustrates the uncommon manifestations of Pseudomonas endocarditis in an IVDA and indicates that it is very important to check comprehensively for an atrial septal defect or patent foramen ovale or any shunt in patients with IVDA who may be at risk for left-sided endocarditis which is catastrophic when compared to right-sided endocarditis. If detected early in IVDA patients, these shunts need to be closed to prevent paradoxical embolism of vegetation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Vidoes Available on: www.jcecho.org
References
- 1.Dawson NL, Brumble LM, Pritt BS, Yao JD, Echols JD, Alvarez S. Left-sided Pseudomonas aeruginosa endocarditis in patients without injection drug use. Medicine (Baltimore) 2011;90:250–5. doi: 10.1097/MD.0b013e3182252133. [DOI] [PubMed] [Google Scholar]
- 2.Hassan KS, Al-Riyami D. Infective endocarditis of the aortic valve caused by Pseudomonas aeruginosa and treated medically in a patient on haemodialysis. Sultan Qaboos Univ Med J. 2012;12:120–3. doi: 10.12816/0003099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panduranga P, Mukhaini MK. Pacemaker lead thrombo-endocarditis in an intravenous drug abuser. J Saudi Heart Assoc. 2011;23:155–7. doi: 10.1016/j.jsha.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morpeth S, Murdoch D, Cabell CH, Karchmer AW, Pappas P, Levine D, et al. Non-HACEK Gram-negative bacillus endocarditis. Ann Intern Med. 2007;147:829–35. doi: 10.7326/0003-4819-147-12-200712180-00002. [DOI] [PubMed] [Google Scholar]
- 5.Reyes MP, Ali A, Mendes RE, Biedenbach DJ. Resurgence of Pseudomonas endocarditis in Detroit, 2006-2008. Medicine (Baltimore) 2009;88:294–301. doi: 10.1097/MD.0b013e3181b8bedc. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


