Abstract
The syndrome of inappropriate sinus tachycardia (IST) is a well-described and generally benign condition outside pregnancy. There is, however, little information in the literature about IST during pregnancy and nothing about the likely mechanism in such cases. Equally there is a paucity of information about the effects on maternal and fetal well-being in patients who develop IST during pregnancy. Here, we describe the case of a woman who developed IST for the first time during pregnancy. We have first given a brief clinical summary of events and then follow this with the patient's personal account which she has written herself specifically for this case report. We believe that this case highlights some of the important issues associated with the condition when it occurs during pregnancy. We hope that the publication of this case report will increase the awareness of IST during pregnancy. This is important as we believe that the correct diagnosis and understanding of the condition and its consequences will allow clinicians to manage women afflicted by the condition empathetically and appropriately.
Background
The syndrome of inappropriate sinus tachycardia (IST) is a well-described, poorly understood condition that occurs in ∼1% of the population and is generally considered benign.1 There is, however, little information in the literature about IST during pregnancy and nothing about the likely mechanism in such cases. Equally there is a paucity of information about the effects on maternal and fetal well-being in patients who develop IST during pregnancy.
Despite the lack of literature on the subject of IST during pregnancy we believe that it occurs relatively frequently although it is often unrecognised. In the past 12 months, our maternity cardiology service has managed 20 patients with IST during pregnancy. Here, we detail the case of a woman, referred to our maternity cardiology service, who developed IST for the first time during pregnancy. We have first given a brief clinical summary of events and then follow this with the patient's personal account which she has written herself specifically for this case report. The case is representative of the cohort of patients that we have managed and exemplifies many of the problems faced by physicians and patients trying to manage this poorly understood condition.
Case presentation
A 32-year-old gravida 4 para 3+1 woman was referred to our multidisciplinary maternity cardiology service for evaluation 4 months after her fourth pregnancy. She had no medical history of note and had no problems (cardiac or otherwise) during her previous pregnancies. The first two (6 and 4 years previously) pregnancies culminated in the birth of healthy infants after spontaneous vaginal deliveries; the third (a year previously) had, unfortunately, ended in a miscarriage. During her latest pregnancy she was asymptomatic until 36 weeks gestation when she developed effort intolerance, palpitations and non-orthostatic dizziness. As a result of these symptoms she was first admitted to her local hospital and then admitted, a week later, to our institute. She was seen by obstetricians, general physicians and cardiologists with all attendant clinicians agreeing that her symptoms were due to a sinus tachycardia (having correlated symptoms and rhythm) without an identifiable cause and, therefore, not life threatening and unlikely to cause harm. She was on no regular medication at the time of presentation and none was prescribed at this point in time. However, on her second admission, her symptoms had become so intrusive and distressing that it was agreed to proceed with induction of labour. She was reviewed by an anaesthetist who recommended labour in a larger clinical delivery room with routine monitoring. Labour was subsequently induced at 37+2 weeks gestation and resulted in a normal vaginal delivery; the baby weighed 3150 g and had a 5 min APGAR score of 10. The patient and her baby were discharged but the patient required readmission 2 days postpartum for a persistent tachycardia. She was, again, diagnosed with a sinus tachycardia that was attributed on this occasion to a (minor) uterine infection; the infection was managed conservatively with oral antibiotics and no specific treatment was given for her tachycardia. After discharge she had a further four consultations with general physicians and cardiologists for her ongoing cardiac symptoms and tachycardia; at one point being prescribed a β-blocker for symptomatic relief. She did not take the prescribed β-blocker due to concerns that it may be expressed in breast milk and effect baby. Eventually, at ∼8 weeks postpartum, her palpitations and dizziness resolved. When seen in our clinic at 4 months postpartum she was asymptomatic with a good exercise capacity and felt back to her normal self.
Investigations
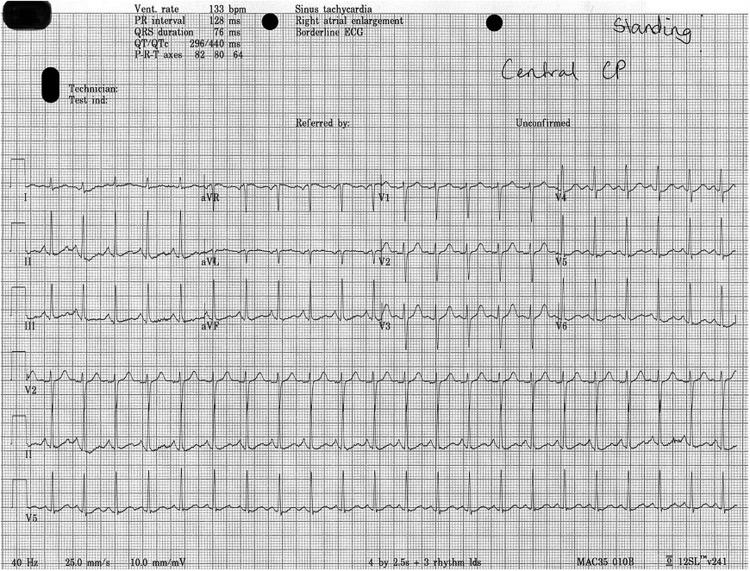
When seen in the maternity cardiac clinic 4 months postpartum, the cardiovascular examination was normal. Review of her previous investigations revealed that all available 12-lead ECGs demonstrated sinus rhythm with a PR interval of 120 ms and no QRS, ST, T nor QT abnormalities; the highest recorded resting heart rate on ECG being 133 bpm (figure 1). A 24-hour ambulatory heart monitor undertaken between 36 and 37 weeks gestation recorded sinus rhythm throughout with rates of 69–148 bpm (24-hour mean heart rate 94 bpm) with preserved diurnal variability and no pathological arrhythmias. During the time when the patient had her cardiac symptoms appropriate and extensive (haematological, biochemical, radiological and cardiological) investigations were undertaken to identify any potential cause for her sinus tachycardia. Apart from diagnosing a mild uterine infection postpartum, all other investigations were normal (including full blood count, renal function, bone profile, liver function tests, magnesium, thyroid function, glucose, pH, lactate, cardiac troponin, plasma metanephrines, chest X-ray, lung perfusion scan and echocardiogram).
Figure 1.
ECG during symptoms demonstrating inappropriate sinus tachycardia.
Differential diagnosis
Considering all factors, we felt the patient had suffered from symptomatic pregnancy-related IST. This diagnosis was made in accordance with the 2015 Heart Rhythm Society expert consensus.2
Treatment
As the patient was asymptomatic when seen in our clinic, we did not recommend any treatment at that point.
Outcome and follow-up
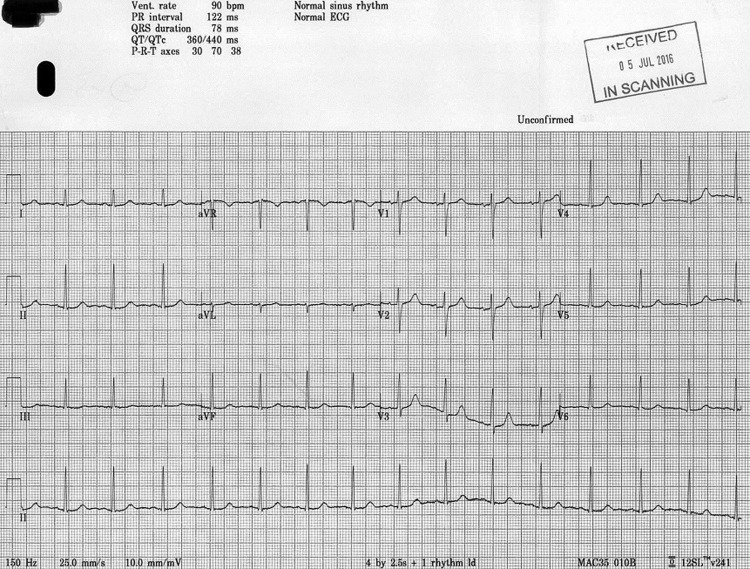
Further follow-up was undertaken at 9½ months postpartum. The patient continued without cardiac symptoms, 12-lead ECG was normal (figure 2) and an ambulatory 24-hour ECG monitoring demonstrated sinus rhythm throughout with rates of 57–164 bpm (24-hour mean 80 bpm) with good diurnal variability and no arrhythmias.
Figure 2.
ECG when asymptomatic demonstrating normal sinus rhythm.
Discussion
This case brought the concept of pregnancy-related IST to our awareness and we have, subsequently, identified a number of other cases. In the majority of these cases, we have managed the individuals' had no medical history or cardiac symptoms until they became pregnant and their symptoms resolved postpartum. All cases have a number of similarities that underline the importance of increasing the awareness of this condition:
Patients experienced intrusive and distressing physical symptoms.
After appropriate and extensive investigations a sinus tachycardia was concluded to be the cause of the symptoms and felt to be non-pathological and compatible with normal pregnancy.
The attendant clinicians tried to reassure the patients and that this led, almost universally and paradoxically, to greater distress (as the women continued with debilitating symptoms while believing that the medical professionals thought that there was nothing wrong with them).
Prognosis
In the literature, there are three case reports of IST-associated cardiomyopathy in adults; two of which were related to pregnancy and all of which resolved on treating the tachycardia.3–5 Otherwise there have been no reports of serious adverse events or patients dying as a direct result of IST. As such, the condition may be considered benign with respect to mortality and significant physical morbidity. Also, the case we present here (and the others we have been involved with) had a good maternal and fetal outcome when compared with other cardiac conditions.6 Despite this, however, the woman described above (and many of the others) had symptoms that were sufficiently distressing to require multiple admissions to hospital. This in itself, we believe, indicates a sufficient degree of associated morbidity to conclude that IST, when it occurs during pregnancy, is not a truly benign condition.
Recognising the condition
In addition to the direct physical, psychological and emotional impact of IST on pregnant women, another area of concern that the presented case highlights is the lack of recognition of IST by the attendant clinicians and the consequent, indirect, increase in patient distress. The lack of recognition likely reflects the failure to differentiate the normal physiological changes in heart rate that occur during pregnancy from IST. The physicians are probably aware that, during normal pregnancy, due to physiological adaptation, the resting heart rate increases progressively throughout pregnancy by 10–20 bpm reaching a maximum heart rate during the third trimester.7–9 They may, however, not realise that the upper limit of resting heart rate has rarely been shown to exceed 95 bpm in population-based studies and that pregnant women presenting with resting heart rates >100 bpm require further investigation.10 11 We hope that by publishing this case report, the awareness of IST during pregnancy will be increased and the suffering of affected individuals will be reduced. It will increase the likelihood of clinicians correctly diagnosing affected individuals thus ensuring patients receive the empathetic care with effective communication that has been shown to improve outcomes in IST.12 13
Treatment options (non-pregnant population)
Having made the correct diagnosis, there are a number of management strategies described in the literature; mainly in non-pregnant individuals but that could be applied to a pregnant woman. Lifestyle adjustments with maintenance of adequate fluid intake and exercise training are advocated by some authors;14 these approaches have evidence base for use in postural orthostatic tachycardia syndrome and may be transferable to patients with IST who share a number of pathophysiological and symptomatic characteristics.15 16 Reduction of the sinus rate can often be achieved (but does not necessarily alleviate all symptoms) by pharmacological therapies and, in drug refractory cases, non-pharmacological (radiofrequency catheter ablation (RFA)) therapeutic approaches. Pharmacological strategies have historically employed β-blockers as the first-line therapy with non-dihydropyridine calcium channel blockers (eg, verapamil or diltiazem) and amiodarone being used if the patient was unresponsive to them. However, the use of all these agents is frequently limited by side effects and patient intolerance.17–19 Recently, ivabradine used alone or in combination with a β-blocker has demonstrated superiority in reducing heart rate and relieving symptoms with less adverse effects in patients suffering with IST.20–25 For those patients whose tachycardia does not respond to drug treatment radio frequency ablation of the sinus node is an option. The current approach consists of in sinus node modification that is achieved by ablation of the cranial part of the sinus node to eliminate faster sinus rates while trying to preserve chronotropic competence.26 While this is usually achieved with a purely endocardial approach, the effectiveness of the procedure may be enhanced with a combined endocardial and epicardial approach.27 The use of RFA, while a promising alternative to drug therapy, is not universally effective and has associated risks, although these will likely reduce as techniques improve.28–30
Treatment options (adjusting for pregnancy)
When managing patients with IST during pregnancy, we believe that the focus should be on empathetic care, effective communication, good hydration and regular gentle exercise. β-blockers are a reasonable choice for patients with debilitating symptoms. The British National Formulary (BNF) advises caution when using β-blockers during pregnancy but states that labetolol is not known to be harmful. Bisoprolol, labetolol, metoprolol and propanolol have been classified by the US Food and Drug Administration (US FDA) as category C (meaning that either studies in animals have revealed adverse effects on the fetus (and there are no controlled studies in women), or studies in women and animals are not available) and they should, therefore, only given if the potential benefits to the mother justify the potential risk to the fetus. Atenolol is classified as category D and should not be given.31 With respect to alternatives to β-blockers, the BNF advises against the use of non-dihydropyridine calcium channel blockers and ivabradine in pregnancy. The US FDA classifies non-dihydropyridine calcium channel blockers as category C.31 Although not explicitly classified, the US FDA states that ivabradine may cause fetal toxicity when administered to a pregnant woman based on animal studies. Despite these cautions, the use of ivabradine has been described in a pregnant patient with IST and a tachycardia-induced cardiomyopathy.4 In drug refractory IST, RFA is an option but is associated with a risk of significant fetal irradiation; despite this relative contraindication, its use has also been described in a separate pregnant woman with IST and tachycardia-induced cardiomyopathy.5
Future perspectives
In the case presented in this paper (and others we have been involved with), the individual had no medical history or cardiac symptoms until she became pregnant and her symptoms resolved postpartum. This is quite different from cases where the IST predates pregnancy and is exacerbated by increasing gestation. It suggests the possibility that there may be a distinct form of IST that only occurs during pregnancy and may reflect an exaggerated cardioautonomic response to the physiological changes of pregnancy. This is theoretically plausible in so far as we know that during pregnancy there is an increase in sympathetic tone and a change in baroreceptor reflex sensitivity;32 33 these changes could be exaggerated in individuals who develop IST during pregnancy with the changes resulting from variable hormonal fluctuations encountered during their pregnancy similar to those seen during the menstrual cycle.34 Alternatively, there could be a hormonally mediated increase in sinus node sensitivity to the increased sympathetic tone of pregnancy. These postulations, we believe, warrant further investigation as a better understanding of the mechanism of the condition might lead to better management of women whose pregnancy would otherwise be blighted by the distressing symptoms of palpitations, dizziness and exercise intolerance.
Conclusions
IST is not usually a life-threatening condition but, when occurring during pregnancy, can be associated with the development of tachycardia-induced cardiomyopathy putting both mother and baby at risk.
In the absence of deteriorating cardiac function, IST occurring during pregnancy is still not truly benign as it can result in significant distress and hospitalisation.
Awareness of the condition and early diagnosis will allow patients' to receive empathetic care (with effective communication that will likely reduce their distress) and, when necessary, be given timely and appropriate pharmacological and/or invasive treatment.
Patient's perspective.
My fourth pregnancy was fairly straight forward up until 35+6 weeks when I started feeling unwell. I visited the maternity unit and they found that my heart rate was high (140+). I was kept on the heart monitor and it eventually settled back down; the midwife advised me to take it easy and sent me home. I visited my local midwife for scheduled 36-week check the following morning where my heart rate was 140 increasing to over 180 with minimal physical activity. I was dizzy with heart palpitations, pale complexion, breathless and just felt extremely unwell. The midwife has seen me through three of my pregnancies so knew me well and wasn’t happy with how I was presenting. She called the doctor for assessment and both midwife and doctor decided I needed to be transferred to hospital immediately (with a suspected blood clot). My main concerns at this point were: Why is this happening, what is the cause, will it harm me (as I have two beautiful children at home who need their mum) and will it harm my unborn baby?
On admission to my local hospital (different from the maternity hospital) I had numerous checks. The ECG reported sinus tachycardia and bloods reported raised d-dimer. I was advised I needed to have a VQ scan to rule out a clot on the lung. I asked to be induced to avoid any complications for my unborn baby but this was declined. I waited in hospital in the A&E short stay until the scan. Care became disjointed; classified as ‘high risk’ I couldn’t be transferred to maternity and A&E was not equipped to monitor my baby. This was frightening but I was pleased when the scan was completed and no blood clot was found. The consultants, therefore, believed it to be related to normal pregnancy and I was discharged. Later that week I had a consultation with my obstetrician and was admitted to be induced at 37 weeks. I breathed a sigh of relief when my beautiful baby was here safely and believed the horror of the previous week would soon be a distant memory.
However, my symptoms of dizziness, palpitations and breathless persisted. After I had given birth the maternity unit discharged me home and the next day, at the community midwife check, my heart rate was over 140 with no physical activity. She called the maternity unit who advised I needed A&E not their care. I was then sent to A&E with my 2-day old baby, which made me extremely anxious about the germs. On arrival at A&E my heart rate was still 140 increasing as soon as stood up or walked in excess of 190. I was advised to come in to hospital but told my baby couldn’t! I argued that my daughter was 2 days old and solely breast fed; I was told it wasn’t safe for my baby to be on the cardiology unit so I asked if we could go to the maternity unit. I was told this wasn’t possible as I was classified too ‘high risk’ to be on the maternity ward and that it was better for her to go home on bottle feeds with Daddy; I would only be a couple of days (this couple of days is crucial bonding time!!). I refused and, eventually, a side room on the cardiology ward was organised. I stayed in for 24 hours then discharged for ongoing outpatient follow-up. For a further 8 weeks (maybe longer) after giving birth to my baby daughter my heart symptoms continued and I returned to hospital many times. When I wasn't visiting hospital I felt extremely debilitated. I couldn’t walk my other children (6 and 4 years) to school or go to the park. I barely left the house during this time due to feeling so unwell and yet no one had any answers. I found all of this extremely hard.
In addition to feeling physically unwell I found this whole period psychologically and emotionally extremely testing. I felt that my other two children (6 and 4 years old) were having to deal with a new baby sister and with mummy being in and out of hospital; I was scared that this could be detrimental to their relationship with their new sibling (luckily they loved her instantly and were very patient). Also, my husband had to take a lot of time off work to care for both myself and our children; it impacted my whole family and took away some of the initial enjoyment of a new baby.
The whole period was extremely frightening for both, me personally and for my family. I feel that had there been more continuity of care and a better understanding of my condition from the beginning that some of my worry may have been reduced. While it wouldn’t have made me feel physically better it would have improved things emotionally and psychologically and certainly would have made my experience more bearable.
Learning points.
A resting heart rate >100 bpm and/or a mean 24-hour ambulatory heart rate >90 bpm in a pregnant woman is not normal and requires further investigation.
If all known causes of sinus tachycardia are excluded with appropriate investigations, then the likely diagnosis is inappropriate sinus tachycardia.
Inappropriate sinus tachycardia is not usually a life-threatening condition but, when occurring during pregnancy, can be associated with the development of tachycardia-induced cardiomyopathy putting both mother and baby at risk. In the absence of deteriorating cardiac function, inappropriate sinus tachycardia occurring during pregnancy is still not truly benign as it can result in significant distress and hospitalisation.
Simply reassuring the patient that there is nothing to worry about will likely lead to greater distress as the woman will continue to have distressing symptoms while believing that the medical professionals think that there is nothing wrong.
Correct diagnosis and understanding of the condition and its consequences will allow the clinician to compassionately explain the symptoms to the patient and manage them appropriately.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Still AM, Raatikainen P, Ylitalo A et al. . Prevalence, characteristics and natural course of inappropriate sinus tachycardia. Europace 2005;7:104–12. 10.1016/j.eupc.2004.12.007 [DOI] [PubMed] [Google Scholar]
- 2.Sheldon RS, Grub BP II, Olshansky B et al. . 2015 HRS expert consensus statement on the diagnosis of POTS, IST and vasovagal syncope. Heart Rhythm 2015;12:e41–57. 10.1016/j.hrthm.2015.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Winum PF, Cayla G, Rubini M et al. . A case of cardiomyopathy induced by inappropriate sinus tachycardia and cured by ivabradine. Pacing Clin Electrophysiol 2009;32:942–4. 10.1111/j.1540-8159.2009.02414.x [DOI] [PubMed] [Google Scholar]
- 4.Sağ S, Çoşkun H, Baran I et al. . Inappropriate sinus tachycardia-induced cardiomyopathy during pregnancy and successful treatment with ivabradine. Anatol J Cardiol 2016;16:212–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szumowski L, Szufladowicz E, Orczykowski M et al. . Ablation of severe drug-resistant tachy-arrhythmia during pregnancy. J Cardiovasc Electrophysiol 2010;21:877–82. 10.1111/j.1540-8167.2010.01727.x [DOI] [PubMed] [Google Scholar]
- 6.Siu SC, Sermer M, Colman JM et al. , Cardiac Disease in Pregnancy (CARPREG) Investigators. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001;104:515–21. [DOI] [PubMed] [Google Scholar]
- 7.Carruth JE, Mivis SB, Brogan DR et al. . The electrocardiogram in normal pregnancy. Am Heart J 1981;102(pt 1):1075–8. [DOI] [PubMed] [Google Scholar]
- 8.Clapp JF III, Capeless E. Cardiovascular function before, during, and after the first and subsequent pregnancies. Am J Cardiol 1997;80:1469–73. [DOI] [PubMed] [Google Scholar]
- 9.Grindheim G, Estensen ME, Langesaeter E et al. . Changes in blood pressure during healthy pregnancy: a longitudinal cohort study. J Hypertens 2012;30:342–50. 10.1097/HJH.0b013e32834f0b1c [DOI] [PubMed] [Google Scholar]
- 10.Mahendru AA, Everett TR, Wilkinson IB et al. . A longitudinal study of maternal cardiovascular function from preconception to the postpartum period. J Hypertens 2014;32:849–56. 10.1097/HJH.0000000000000090 [DOI] [PubMed] [Google Scholar]
- 11.Savu O, Jurcuţ R, Giuşcă S et al. . Morphological and functional adaptation of the maternal heart during pregnancy. Circulation Cardiovasc Imaging 2012;5:289–97. [DOI] [PubMed] [Google Scholar]
- 12.Marrouche NF, Beheiry S, Tomassoni G et al. . Three- dimensional nonfluoroscopic mapping and ablation of inappropriate sinus tachycardia. Procedural strategies and long-term outcome. J Am Coll Cardiol 2002;39:1046–54. [DOI] [PubMed] [Google Scholar]
- 13.Greenwood JP, Scott EM, Stoker JB et al. . Sympathetic neural mechanisms in normal and hypertensive pregnancy in humans. Circulation 2001;104:2200–4. [DOI] [PubMed] [Google Scholar]
- 14.Olshansky B, Sullivan RM. Inappropriate sinus tachycardia. J Am Coll Cardiol 2013;61:793–801. 10.1016/j.jacc.2012.07.074 [DOI] [PubMed] [Google Scholar]
- 15.Fu Q, Vangundy TB, Galbreath MM et al. . Cardiac origins of the postural orthostatic tachycardia syndrome. J Am Coll Cardiol 2010;55:2858–68. 10.1016/j.jacc.2010.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winker R, Barth A, Bidmon D et al. . Endurance exercise training in orthostatic intolerance: a randomized, controlled trial. Hypertension 2005;45:391–8. 10.1161/01.HYP.0000156540.25707.af [DOI] [PubMed] [Google Scholar]
- 17.Cossu SF, Steinberg JS. Supraventricular tachyarrhythmias involving the sinus node: clinical and electrophysiologic characteristics. Prog Cardiovasc Dis 1998;41:51–63. [DOI] [PubMed] [Google Scholar]
- 18.Femenía F, Baranchuk A, Morillo CA. Inappropriate sinus tachycardia: current therapeutic options. Cardiol Rev 2012;20:8–14. [DOI] [PubMed] [Google Scholar]
- 19.Lee RJ, Shinbane JS. Inappropriate sinus tachycardia. Diagnosis and treatment. Cardiol Clin 1997;15:599–605. [DOI] [PubMed] [Google Scholar]
- 20.Ptaszynski P, Kaczmarek K, Ruta J et al. . Metoprolol succinate vs. ivabradine in the treatment of inappropriate sinus tachycardia in patients unresponsive to previous pharmacological therapy. Europace 2013;15:116–21. 10.1093/europace/eus204 [DOI] [PubMed] [Google Scholar]
- 21.Cappato R, Castelvecchio S, Ricci C et al. . Clinical efficacy of ivabradine in patients with inappropriate sinus tachycardia: a prospective, randomized, placebo-controlled, double-blind, crossover evaluation. J Am Coll Cardiol 2012;60:1323–9. 10.1016/j.jacc.2012.06.031 [DOI] [PubMed] [Google Scholar]
- 22.Calo L, Rebecchi M, Sette A et al. . Efficacy of ivabradine administration in patients affected by inappropriate sinus tachycardia. Heart Rhythm 2010;7:318–1323. [DOI] [PubMed] [Google Scholar]
- 23.Kaplinsky E, Comes FP, Urondo LS et al. . Efficacy of ivabradine in four patients with inappropriate sinus tachycardia: a three month-long experience based on electrocardiographic, Holter monitoring, exercise tolerance and quality of life assessments. Cardiol J 2010;17:166–71. [PubMed] [Google Scholar]
- 24.Zellerhoff S, Hinterseer M, Felix Krull B et al. . Ivabradine in patients with inappropriate sinus tachycardia. Naunyn Schmiedebergs Arch Pharmacy 2010;382:483–6. [DOI] [PubMed] [Google Scholar]
- 25.Ptaszynski P, Kaczmarek K, Ruta J et al. . Ivabradine in combination with metoprolol succinate in the treatment of inappropriate sinus tachycardia. J Cardiovasc Pharmacol Ther 2013;18:338–44. 10.1177/1074248413478172 [DOI] [PubMed] [Google Scholar]
- 26.Gianni C, Di Biase L, Mohanty S et al. . Catheter ablation of inappropriate sinus tachycardia. J Interv Card Electrophysiol 2016;46:63–9. 10.1007/s10840-015-0040-2 [DOI] [PubMed] [Google Scholar]
- 27.Jacobson JT, Kraus A, Lee R et al. . Epicardial/endocardial sinus node ablation after failed endocardial ablation for the treatment of inappropriate sinus tachycardia. J Cardiovasc Electrophysiol 2014;25:236–41. 10.1111/jce.12318 [DOI] [PubMed] [Google Scholar]
- 28.Frankel DS, Lin D, Anastasio N et al. . Frequent additional tachyarrhythmias in patients with inappropriate sinus tachycardia undergoing sinus node modification: an important cause of symptom recurrence. J Cardiovasc Electrophysiol 2012;23:835–9. 10.1111/j.1540-8167.2012.02297.x [DOI] [PubMed] [Google Scholar]
- 29.Callans DJ, Ren JF, Schwartzman D et al. . Narrowing of the superior vena cava-right atrium junction during radiofrequency catheter ablation for inappropriate sinus tachycardia: analysis with intracardiac echocardiography. J Am Coll Cardiol 1999;33:1667–70. [DOI] [PubMed] [Google Scholar]
- 30.Vatasescu R, Shalganov T, Kardos A et al. . Right diaphragmatic paralysis following endocardial cryothermal ablation of inappropriate sinus tachycardia. Europace 2006;8:904–6. 10.1093/europace/eul089 [DOI] [PubMed] [Google Scholar]
- 31.Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C et al. . ESC guidelines on the management of cardiovascular diseases during pregnancy. Eur Heart J 2011;32:3147–97. 10.1093/eurheartj/ehr218 [DOI] [PubMed] [Google Scholar]
- 32.Jarvis SS, Shibata S, Bivens TB et al. . Sympathetic activation during early pregnancy in humans. J Physiol (Lond) 2012;590(pt 15):3535–43. 10.1113/jphysiol.2012.228262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leduc L, Wasserstrum N, Spillman T et al. . Baroreflex function in normal pregnancy. Am J Obstet Gynecol 1991;165(pt 1):886–90. [DOI] [PubMed] [Google Scholar]
- 34.Minson CT, Halliwill JR, Young TM et al. . Influence of the menstrual cycle on sympathetic activity, baroreflex sensitivity, and vascular transduction in young women. Circulation 2000;101:862–8. [DOI] [PubMed] [Google Scholar]