Abstract
Background:
The purpose of this study was to determine the prevalence and related factors of low birth weight (LBW) in the Southeast of Iran.
Methods:
This cross-sectional study was carried out in Kerman province. Data were collected from Iranian Maternal and Neonatal Network at public and private hospitals. All live births from March 2014 to March 2015 considered as the source population. The risk factors including maternal age, gravida, parity, abortion, pregnancy risk factors, maternal nationality, maternal education, maternity insurance, place of living, consanguinity, neonate sex, preterm labor, place of birth, delivery manager, and delivery type were compared between LBW and normal birth weight groups.
Results:
The prevalence of LBW was 9.4% in the present study. Preterm labor (odds ratio [OR]: 22.06; P < 0.001), neonate female sex (OR: 1.41; P < 0.001), low parity (OR: 0.85; P < 0.001), pregnancy age <18 years (OR: 1.26; P = 0.012), pregnancy age >35 years (OR: 1.21; P = 0.001), delivery by cesarean section (OR: 1.17; P = 0.002), pregnancy risk factors (OR: 1.67; P < 0.001), maternal illiteracy (OR: 1.91; P < 0.001), living in the rural area (OR: 1.19; P < 0.001), consanguineous (OR: 1.08; P = 0.025), and delivery by obstetrician (OR: 1.12; P = 0.029) were identified as significant factors associated with LBW in this study.
Conclusions:
Prevention of preterm labor, consanguineous marriage, pregnancy age <18 and >35 years old, and maternal medical risk factors are some critical interventions to reduce its burden. Increasing the access to high-quality health-care services in rural and deprived areas is another effective strategy for the prevention of LBW.
Keywords: Low birth weight, prevalence, risk factor
INTRODUCTION
Low birth weight (LBW) as a significant public health indicator is defined as weight at birth fewer than 2500 g by the World Health Organization.[1,2] LBW is one of the main causes of infant mortality including around 40% of all death among children under 5 years old which occurs in neonatal or newborn.[1] The mortality rate of LBW is approximately twenty times more than heavier infants.[2] Totally, about 15.5% of all birth is LBW while 95.6% of it occurs in developing countries. In addition, the incidence of LBW in low-income societies is more than twice in compare to middle incomes.[2,3]
Growth disorder, cognitive development defects, and chronic diseases later in life are the other adverse effects of LBW.[4] The risk of some diseases such as coronary diseases, stroke, hypertension, and diabetes are higher in adults with a history of LBW than normal birth weight (NBW).[5,6,7]
There are many risk factors for LBW including maternal demographic, anthropometric, medical and behavioral factors, paternal and fetal factors, environmental and nutritional factors, and lack of prenatal care.[3,8] Furthermore, social determinants of health such as income, education, housing, addiction, and living place (urban/rural) have an important role in LBW.[9,10]
While LBW associated factors are well studied in developed countries, there are not enough evidence in developing countries.[11] The aim of this study was to determine the 1-year prevalence and related factors of LBW in the Southeast of Iran.
METHODS
This cross-sectional study was performed in Kerman province, known as the largest province in Iran. Kerman province is located in the Southeast of Iran.
All live births from March 2014 to March 2015 considered as the source population. Data were collected from Iranian Maternal and Neonatal Network (IMaN Net) at public and private hospitals. IMaN Net is one of the major sources of information to evaluate the maternal and neonatal health status in Iran that was designed by Iran's Ministry of Health and Medical Education. This information system includes both maternal and neonatal data in an online form. Then, data are entered into Excel file. We exported data from Excel file to SPSS software, Version 21.0 (IBM SPSS Inc. Chicago, IL, USA). Maternal data were included maternal age (years), gravida (number), parity (number), abortion (number), pregnancy risk factors (yes, no), maternal nationality (Iranian, non-Iranian), maternal education level (illiterate, primary school, secondary school, high school, university), maternity insurance (yes, no), place of living (urban, rural), and consanguinity (yes, no). Assembled neonatal and delivery data were neonate sex (female, male) and weight (g), gestational age (week), birth anomalies (yes, no), place of birth (hospital, other), and delivery manager (midwife, obstetrician, other).
Exclusion criteria to assess risk factors of LBW were as follows: birth weight >4000 g, congenital anomalies, and multiple births. All live births were divided into two groups including LBW (<2500 g) and NBW (2500–4000 g).
The study was registered by the ethical committee of the Kerman University of Medical Sciences (ethical code: K/93/596).
Statistical analysis
The data were analyzed using SPSS 21. In the first step, quantitative and qualitative data were analyzed using t-test and Chi-square, respectively. Then, multivariable logistic regression was used to assess the relationship between independent variables and LBW, considering confounding factors. The level of significance was set to 0.05.
RESULTS
A total of 60,273 live birth occurred during the 1-year study period, in which 5679 were LBW. Therefore, the prevalence of LBW was estimated as 9.4%. The birth weight of 631 live cases (1.05%) was very LBW (birth weight <1500 g), and 276 newborns (0.46%) had extremely very LBW (birth weight <1000 g). The highest and lowest prevalence of LBW according to the city of delivery were Kahnuj (10.8%) and Manujan (4.4%), respectively [Figure 1].
Figure 1.
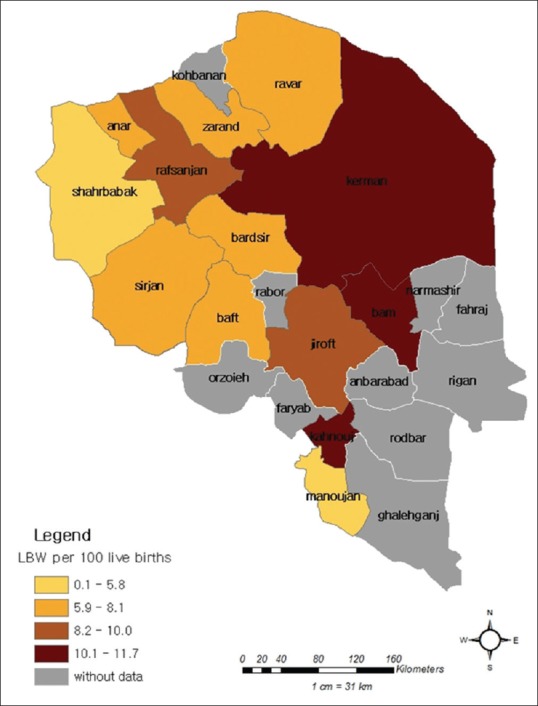
The geography of low birth weight prevalence in Kerman province according to the city of delivery
The mean (±standard deviation [SD]) birth weight of live births was 3061.9 (±509.9) g, and gestational age mean (±SD) was 38.4 (±1.8) week. From total live birth, 58,195 newborns were included in the study to assess risk factors of LBW (52,977 NBW and 5218 LBW).
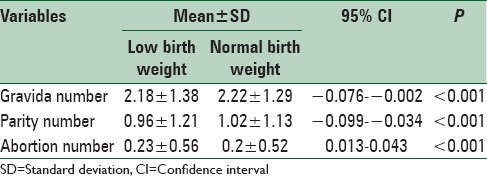
Statistically, there was a significant difference between NBW and LBW in delivery factors includes gravida, parity, and abortion number by t-test (P < 0.001). Parity and gravid number had negative association with LBW, but abortion number was vice versa [Table 1].
Table 1.
Comparison of delivery factors between low birth weight and normal birth weight newborns
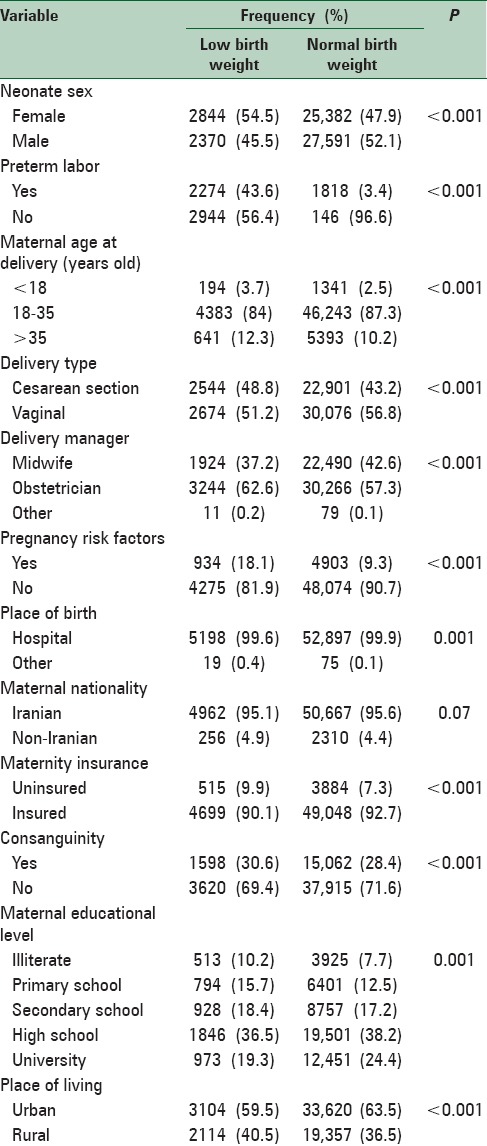
Preterm labor, neonate female sex, pregnancy age <18 and >35 years old, delivery by cesarean section, maternal medical risk factors in current pregnancy, lower maternal education level, living in the rural area, consanguineous, delivery by obstetrician, birth in hospital, non-Iranian maternal nationality, and uninsured were more frequent in LBW than NBW. Among all maternal and neonatal factors between LBW and NBW, maternal nationality was not significant (P = 0.07) [Table 2].
Table 2.
Comparison of maternal and neonatal factors between low birth weight and normal birth weight newborns
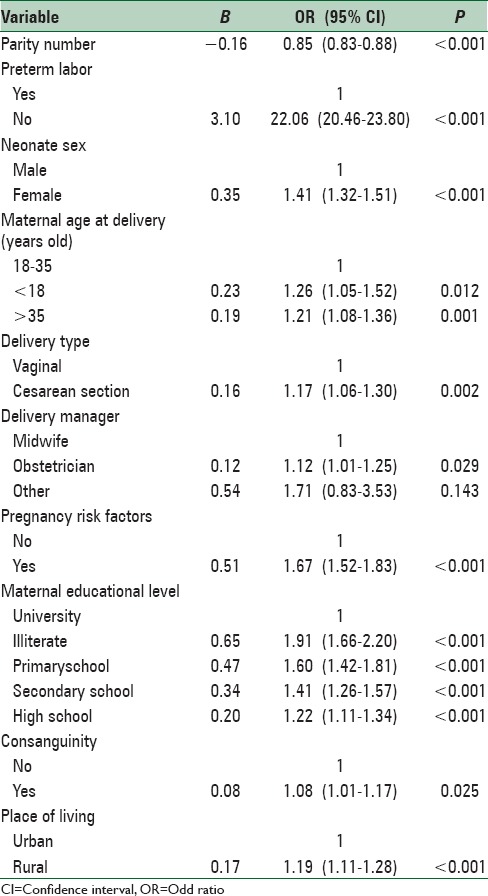
The results of logistic regression analysis revealed that preterm labor, neonate sex, parity number, maternal age at delivery, mode of delivery, pregnancy risk factors, maternal education level, place of living, consanguinity, delivery manager were significantly related to LBW while it was not associated with gravida number, abortion number, place of birth, maternity insurance, and maternal nationality. According to this model, preterm labor was the strongest factors associated with LBW. The risk of LBW was 22 times more in preterm than terms births (odds ratio [OR] = 22.1; 95% confidence interval [CI] = 20.46–23.80). Illiteracy was the most second factor associated with LBW (OR = 1.91; 95% CI = 1.66–2.20). Consanguinity had lowest association with LBW (OR = 1.08; 95% CI = 1.01–1.17) [Table 3].
Table 3.
Results of the logistic regression model comparing low birth weight versus normal birth weight newborns
DISCUSSION
The prevalence of LBW was 9.4% in Kerman province. It was similar to national reports. A systematic review study showed that the prevalence of LBW is between 5% and 12% in Iran.[9] According to the city of delivery, the highest and lowest prevalence of LBW were Kahnuj and Manujan, respectively. Kahnuj city is a referral center for nearby cities, including the city of Manujan, and high-risk pregnancies are referred to Kahnuj.
In the most studies, the preterm birth reported as a dominant risk factor for LBW.[10,12,13] This study showed that preterm birth is the main contributing factor to LBW.
Our research indicated that the female sex was associated with risk of LBW. One study was carried out in Brazil demonstrated this issue because the mean weight of a female fetus is lower than that of a male one.[14]
A negative association was observed between parity number and the risk of LBW. Some studies have indicated that primiparity is associated with increased incidence of LBW.[11,14]
Maternal age at delivery <18 and >35 years old was associated with increased risk of LBW. A large number of epidemiological studies have shown that LBW occurs in young and old mothers. There are social disadvantages such as low socioeconomic status, low education, poor nutrition, and low body mass index responsible for these results in younger mothers; however, in the older mothers, biological factors such as chromosomal anomalies, preeclampsia, and diabetes are responsible for this issue.[8,10,11,15]
Cesarean section was a risk factor for LBW. Our result was similar to a study was conducted in Malaysia. However, this relationship may be confounded by other pregnancy risk factors such as severe preeclampsia, eclampsia, and bleeding placenta previa.[13]
Maternal medical risk factors including gestational hypertension, gestational diabetes mellitus (GDM), and anemia were found significantly associated with LBW. A large number of epidemiological and biological evidence support this fact. Gestational hypertension leads to reduce uteroplacental flow, which increases the risk of LBW. GDM can lead preterm labor and other complications as well. Furthermore, conventional treatment for GDM increases the risk of LBW.[3,8,13,16]
This study revealed that lower maternal education level was accompanied with increased risk of LBW. Other national and international studies confirmed this issue.[17,18,19,20] This may be justified by increasing information of educated mothers about health services.
Similar to some studies, living in the rural area was significantly related to LBW.[18,21,22] Inaccessibility to high-quality health-care systems and more appropriate nutrition for pregnant women who live in the rural area could increase LBW.
In the present study, consanguineous rather than nonconsanguineous was considered as risk factor for LBW. A study conducted in Qatar supports our claim.[12]
Being delivered by obstetrician rather than midwife was associated with higher odds of LBW. To the best of our knowledge, there are no studies about this issue in the world. However, LBW infant mothers may be having pregnancy risk factors that were referred to an obstetrician.
Large sample size and collecting data from all labor centers throughout Kerman province are the strength of this study. Due to using secondary data, researchers cannot measure some risk factors of LBW including health-care service, behavioral, environmental, and nutritional factors. Future studies can be designed with adequate sample size for measuring above-mentioned factors. In addition, the trend of LBW should be monitored in Kerman province.
CONCLUSIONS
Preterm labor, neonate female sex, low parity, pregnancy age <18 and >35 years old, delivery by cesarean section, maternal medical risk factors in current pregnancy, lower maternal education level, living in the rural area, consanguineous, delivery by obstetrician were identified as significant factors associated with LBW in this study. Controlling these risk factors and increasing access to high-quality health-care services in rural and deprived areas are effective strategies for prevention of LBW.
Financial support and sponsorship
The Vice-Chancellor for research at Kerman University of Medical Sciences funded this project (Grant number: 93/550).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank the Maternal Health Office of Iran's Ministry of Health and Medical Education for providing the data of this research project.
REFERENCES
- 1.Ramakrishnan U. Nutrition and low birth weight: From research to practice. Am J Clin Nutr. 2004;79:17–21. doi: 10.1093/ajcn/79.1.17. [DOI] [PubMed] [Google Scholar]
- 2.Wardlaw TM. Low Birthweight: Country, Regional and Global Estimates. UNICEF and WHO Publications. 2004 [Google Scholar]
- 3.Ohlsson A, Shah P. Determinants and Prevention of Low Birth Weight: A Synopsis of the Evidence. Alberta, Canada: Institute of Health Economics; 2008. [Google Scholar]
- 4.Chiarotti F, Castignani AM, Puopolo M, Menniti-Ippolito F, Minniti De Simeonibus E, Di Paolo A. Effects of socio-environmental factors on neurocognitive performance in premature or low-birth weight preschoolers. Ann Ist Super Sanita. 2001;37:553–9. [PubMed] [Google Scholar]
- 5.Rich-Edwards JW, Stampfer MJ, Manson JE, Rosner B, Hankinson SE, Colditz GA, et al. Birth weight and risk of cardiovascular disease in a cohort of women followed up since 1976. BMJ. 1997;315:396–400. doi: 10.1136/bmj.315.7105.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dabelea D, Pettitt DJ, Hanson RL, Imperatore G, Bennett PH, Knowler WC. Birth weight, type 2 diabetes, and insulin resistance in Pima Indian children and young adults. Diabetes Care. 1999;22:944–50. doi: 10.2337/diacare.22.6.944. [DOI] [PubMed] [Google Scholar]
- 7.Shan X, Chen F, Wang W, Zhao J, Teng Y, Wu M, et al. Secular trends of low birthweight and macrosomia and related maternal factors in Beijing, China: A longitudinal trend analysis. BMC Pregnancy Childbirth. 2014;14:105. doi: 10.1186/1471-2393-14-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valero De Bernabé J, Soriano T, Albaladejo R, Juarranz M, Calle ME, Martínez D, et al. Risk factors for low birth weight: A review. Eur J Obstet Gynecol Reprod Biol. 2004;116:3–15. doi: 10.1016/j.ejogrb.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 9.Karimlou M, Sajadi H, Dejman M. Low birth weight and its association factors in Iran: According world health organization model. J Rehabil. 2012;13:75–87. [Google Scholar]
- 10.Momeni M, Esfandyarpour R, Danaei M. The neglected sociobehavioural risk factors of low birth weight. Soc Determ Health. 2016;1:97–103. [Google Scholar]
- 11.Badalyan V. Case control study aimed at revealing risk factors of low birth weight in Yerevan city. College of Health Sciences, American University of Armenia (AUA) 2014 [Google Scholar]
- 12.Bener A, Saleh NM, Salameh KM, Basha B, Joseph S, Al Buz R. Socio-demographic and consanguinity risk factors associated with low birthweight. J Pak Med Assoc. 2013;63:598–603. [PubMed] [Google Scholar]
- 13.Sutan R, Mohtar M, Mahat AN, Tamil AM. Determinant of low birth weight infants: A matched case control study. Open J Prev Med. 2014;4:91–99. [Google Scholar]
- 14.Barbieri MA, Silva AA, Bettiol H, Gomes UA. Risk factors for the increasing trend in low birth weight among live births born by vaginal delivery, Brazil. Rev Saúde Pública. 2000;34:596–602. doi: 10.1590/s0034-89102000000600006. [DOI] [PubMed] [Google Scholar]
- 15.Viengsakhone L, Yoshida Y, Sakamoto J. Factors affecting low birth weight at four central hospitals in vientiane, Lao PDR. Nagoya J Med Sci. 2010;72:51–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Bakker SJ, ter Maaten JC, Gans RO. Thiamine supplementation to prevent induction of low birth weight by conventional therapy for gestational diabetes mellitus. Med Hypotheses. 2000;55:88–90. doi: 10.1054/mehy.1999.1037. [DOI] [PubMed] [Google Scholar]
- 17.Yadav DK, Chaudhary U, Shrestha N. Risk factors associated with low birth weight. J Nepal Health Res Counc. 2011;9:159–64. [PubMed] [Google Scholar]
- 18.Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, et al. Mental health surveillance among children – United States, 2005-2011. MMWR Suppl. 2013;62:1–35. [PubMed] [Google Scholar]
- 19.Nobile CG, Raffaele G, Altomare C, Pavia M. Influence of maternal and social factors as predictors of low birth weight in Italy. BMC Public Health. 2007;7:192. doi: 10.1186/1471-2458-7-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eghbalian F. Low birth weight causes survey in neonates. Iranian J Pediatr. 2007;17(Suppl 1):27–33. [Google Scholar]
- 21.Jalil A, Zakar R, Zakar MZ. A Secondary analysis of maternal factors determining low birth weight in Pakistan. Iran J Public Health. 2015;44:136–7. [PMC free article] [PubMed] [Google Scholar]
- 22.Ebrahimi MM, Ahmadi BP, Arefhosseini SR, Koosha A. Association between maternal anthropometric measures and incidence of low birth weight: A case-control study. Medical Journal of Tabriz University of Medical Sciences. 2012;33:7–12. [Google Scholar]


