Abstract
Introduction:
Insomnia is one of the common but neglected conditions seen in family practice with long term and serious effects on health of a patient. Family physicians have the responsibility of diagnosing and adequately treating this. This study was done to find the prevalence of chronic insomnia in adult patients visiting a family medicine outpatient department (OPD) in a hospital and to assess the risk factors and co morbidities associated with it.
Materials and Methods:
A cross-sectional study was done in the family medicine OPD at St. Philomena's Hospital, Bengaluru. All adult patients attending the OPD from September 1 to October 30, 2015 were enrolled in the study after obtaining written consent. Athens Insomnia Scale was used to diagnose insomnia and information regarding medical co morbidities was collected. Data was analyzed for the prevalence of insomnia and its association with co morbidities.
Results:
Chronic insomnia was seen in 33% of the adult population sampled. Increasing age and diabetes were significantly associated with insomnia, while other socioeconomic factors and co morbidities were not significantly associated. Twenty-seven percent of patients who had insomnia did not perceive the condition, which was statistically significant.
Conclusion:
Insomnia is a common sleep disorder which is many times missed by a primary care physician until/unless asked for. Since there is a higher incidence with increasing age and co morbidities such as diabetes, all patients, especially middle-aged and diabetics, should be screened for insomnia by the primary care physician with a self assessed questionnaire and counseled.
Keywords: Chronic insomnia, comorbidities, prevalence, primary care
Introduction
Insomnia is defined as the subjective perception of difficulty with sleep initiation, duration, consolidation, or quality, which occurs despite adequate opportunity for sleep, and results in some form of daytime impairment.[1] Chronic insomnia is diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,[2] and the International Classification of Sleep Disorders,[3] which have similar criteria for making the diagnosis. These criteria specify that symptoms must cause clinically significant functional distress or impairment, be present for at least 3 nights/week for at least 3 months, and not be linked to other sleep, medical, or mental disorders. Various studies worldwide have shown the prevalence of insomnia in 10%–30% of the population, some even as high as 50%–60%. It is common in older adults, females, and people with medical and mental ill health.[4,5,6] The consequences of insomnia are significant, such as depression, impaired work performance, work- related/motor vehicle accidents, and overall poor quality of life. It is an easy-to-diagnose condition with many self-answerable questionnaires for aid, yet goes unrecognized in a significant number of patients coming to the outpatient department with other comorbid conditions. The objective of this study was to determine the prevalence of chronic insomnia, to look for any association with socioeconomic factors and medical comorbidities, and also to assess the patient's perception of having insomnia.
Materials and Methods
This cross-sectional study was conducted in the family medicine outpatient department (OPD) of a 450-bedded general hospital in Bengaluru - St. Philomena's Hospital. All adult patients attending the OPD from September 1 to October 30, 2015, were enrolled in the study after obtaining written consent. Data about age, gender, education, occupation, monthly family income in rupees, and medical comorbidities were collected using a questionnaire. Athens Insomnia Scale was given to the patient to score; illiterate patients were helped by asking the same questions in their local language. The perception of the patient was asked before answering the insomnia scale. A score of 6 or more was taken as positive for insomnia.
Collected data were alphanumerically coded and entered in an Excel sheet. The analysis was done using SPSS 19.0 software (IBM, Bangalore, India), and the Chi-square test was used for analyzing the association of risk factors. P < 0.05 was considered statistically significant for Chi-square test.
Inclusion and exclusion criteria
All adult patients attending family medicine OPD were included in the study. Patients <18 years and >60 years, patients with known psychiatric illnesses, acutely ill patients, and alcoholics were excluded from the study.
Results
Two hundred and seventy-eight patients were enrolled in the study after obtaining consent – 180 were female and 98 were male.
Table 1 shows the prevalence of insomnia with age and gender. Insomnia was found in 92 (33%) patients - 63 (68%) were female and 29 (32%) were male. Twenty-nine (32%) patients below the age of 35 had insomnia, of which 20 (69%) were female and 9 (31%) were male. Sixty-three (68%) patients were of age >35 years - of which 43 (68%) were female and 20 (32%) were male.
Table 1.
Prevalence of insomnia with age and gender
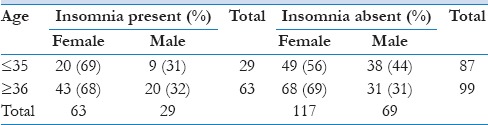
Table 2 shows the association of insomnia with socioeconomic variables. Insomnia was found to be significantly higher in patients >35 years of age (P = 0.015). The educational background did not significantly affect insomnia - 40% of illiterate or people with basic schooling, 19% of undergraduates, 30% of graduates, and 19% of postgraduate degree holders were found to have insomnia. Employment also had no significant correlation with insomnia - 38% unemployed, 33% unskilled laborers, 45% skilled workers, and 30% professionals were found to have insomnia although statistically insignificant. Family income was another insignificant variable - 29% of patients with monthly income <Rs. 25,000 had insomnia, 37% in the group of income between 26,000 and 50,000, 50% with income between 51,000 and 75,000, and 41% with income >Rs. 75,000 had insomnia.
Table 2.
Association of socioeconomic variables with insomnia
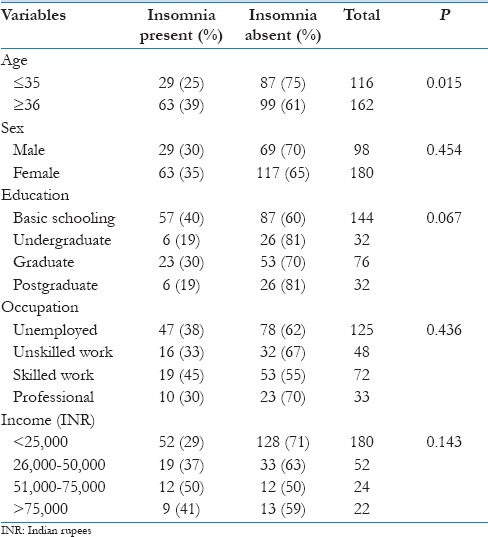
Table 3 shows the association of insomnia with medical comorbidities. Patients with diabetes had statistically significant insomnia compared to those without diabetes (P = 0.001). Fifty percent of patients with diabetes had insomnia compared to 27% without diabetes. Hypertension (37% vs. 32%), ischemic heart disease (50% vs. 33%), thyroid disorders (42% vs. 31%), respiratory disorders (35% vs. 33%), kidney diseases (67% vs. 33%), liver diseases (51% vs. 32%), and other disorders such as arthralgia/tuberculosis/seizures/gastrointestinal disorders (48% vs. 33%) were found to have statistically insignificant correlation with insomnia.
Table 3.
Association of medical comorbidities with insomnia
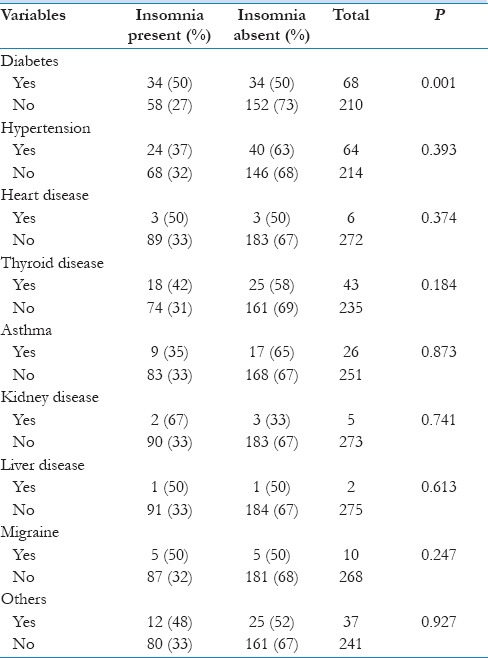
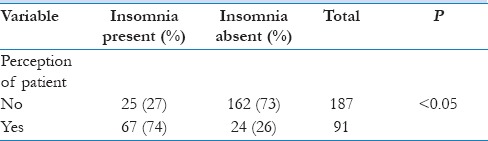
Table 4 shows the association of actual insomnia with the patient's perception. Twenty-five patients (27%) did not have the perception of insomnia although they had a score of >6 in Athens scale, which had a significant P value (P < 0.05).
Table 4.
Association of patient's perception with actual insomnia
Review of literature
The present study was done to determine the prevalence of chronic insomnia in the adult population in a family medicine outpatient clinic. In this study, the prevalence was found to be 33% with statistically significant correlation with increasing age and diabetes. A similar study conducted in South India found a prevalence of 18.6% among healthy adults attending a tertiary hospital[7] Another Indian study identified 15.4% prevalence of insomnia; Incidence was high in persons with comorbid chronic physical illness (28.1%) compared to persons free from that (10.9%), also higher among people living in joint families than those living in a nuclear family and increasing significantly with increasing age.[8] A recent study among corporate employees in India showed a prevalence of insomnia in 13.8% of participants, of which undiagnosed population was 96.4%. The common comorbid conditions associated with insomnia were anxiety, hypertension, and depression, and alcohol consumption was observed to be significantly higher in the sufferers of insomnia.[9] Our study showed a much higher prevalence rate compared to the above three Indian studies.
A multinational study done in Latin American countries using Athens Insomnia Scale and other sleep scales in middle-aged females showed 56.6% of surveyed women suffered from either insomnia, poor sleep quality, or both.[10] The prevalence of insomnia increased with age and menopausal stage. Increasing age, the presence of chronic disease, troublesome drinking, anxiety, depression, vasomotor symptoms, and drug use (hypnotics and hormone therapy) were significant risk factors related to the presence of sleep disturbances. Higher educational level related to less insomnia and better sleep quality. Many other international studies have also shown insomnia to be more common in women and elders.[11,12]
Dr. Ohayan's landmark review of approximately 50 prevalence studies reported roughly 30-20-10 rule for prevalence – i.e., 30% of adults have symptoms, 15%–20% report symptoms, and <10% are likely to meet the diagnostic and statistical criteria.[13]
A meta-analysis done in the US showed that of the patients attending primary care clinics, more than 50% complained of insomnia, only if specifically asked about it, 30% visit their general practitioners (GPs) on their own initiative, and only 5% go to consultation with the main objective of receiving treatment to solve their problem.[14]
Another international survey of sleep disorders in general population found that many individuals with insomnia (47%–67%) did not seek medical attention for their sleep difficulties. Among those who sought medical help, 50%–90% received treatment. Thus, insomnia remains a largely underdiagnosed and undertreated problem.[15]
A study on Malaysian patients attending primary care clinics showed that 38.9% patients had frequent insomnia symptoms (>3 times/week), 30.7% had chronic insomnia without daytime consequences, and 28.6% had chronic insomnia with daytime dysfunction. Indian ethnicity, age ≥50, anxiety symptoms, and depression symptoms were risk factors for chronic insomnia with daytime dysfunction.[16]
This study also analyzed the association of various comorbidities with insomnia and showed statistically significant correlation with patients having diabetes mellitus. In a similar study, Taylor et al.[4] demonstrated that people with chronic insomnia reported more of the following than did people without insomnia: Heart disease (21.9% vs. 9.5%), high blood pressure (43.1% vs. 18.7%), neurologic disease (7.3% vs. 1.2%), breathing problems (24.8% vs. 5.7%), urinary problems (19.7% vs. 9.5%), chronic pain (50.4% vs. 18.2%), and gastrointestinal problems (33.6% vs. 9.2%). Conversely, people with the following medical problems reported more chronic insomnia than did those without those medical problems: Heart disease (44.1% vs. 22.8%), cancer (41.4% vs. 24.6%), high blood pressure (44.0% vs. 19.3%), neurologic disease (66.7% vs. 24.3%), breathing problems (59.6% vs. 21.4%), urinary problems (41.5% vs. 23.3%), chronic pain (48.6% vs. 17.2%), and gastrointestinal problems (55.4% vs. 20.0%). When all medical problems were considered together, only patients with high blood pressure, breathing problems, urinary problems, chronic pain, and gastrointestinal problems had statistically higher levels of insomnia than those without these medical disorders.
Insomnia was also considered as a predictor for other sleep disorders such as obstructive sleep apnea in some studies.[17] A recent study done in Singapore illustrated that many patients with chronic insomnia have underlying primary sleep disorders.[18] Our study did not consider evaluating for other sleep disorders due to practical difficulties in doing sleep studies in primary care settings.
The perception of patients regarding insomnia was also significantly low in our study. A survey among adult French population in 2001–2002 regarding insomnia found that 25% of randomly selected respondents were dissatisfied with their sleep and only 13% had consulted a health-care provider, especially for insomnia.[19] In the South Indian study quoted above, only 2.2% people perceived themselves as having sleep-related problems.[7] In the study on Indian population in West Bengal, it was found that 43.2% of insomniac patients never seek medical advice for insomnia and only 15.3% actually consulted a doctor for their sleep problem.[8] In our population, no patient had actually presented with insomnia as their primary complaint, but 27% of insomniacs did not perceive their condition.
Discussion
Insomnia is the most commonly encountered sleep disorder and occurs in 10%–50% of the population according to studies conducted worldwide. The pathophysiology of insomnia can actually be somewhat complex (or at least multi-factorial) because of the many inputs to the sleep-wake system in general and the additional specific behaviors and cognitions which an individual layers on top of the physiologic substrates.[20]
Studies show that insomnia negatively affects work performance, impairs decision-making, can damage relationships, increase chances of work-related/motor vehicle accidents,[21] and lead to overall decline in quality of life. Despite the prevalence of poor sleep quality and insomnia in the general population, people with sleep problems often go unnoticed in the health-care system. GPs were identified as the most frequently consulted group for sleep disorders.[19]
Insomnia can be classified as acute and chronic/primary and secondary.[22,23,24] When insomnia lasts for 4 weeks or more, it is classified as chronic insomnia.[2] It is further subclassified into with or without comorbidities (medical and psychiatric) and associated with another primary sleep disorder.[25] Numerous self-report instruments exist for the assessment of sleep disturbance. Among them, the most widely used are Pittsburgh Sleep Quality Index, Epworth sleepiness scale, Athens Insomnia Score, and Insomnia Severity Index.
Athens Insomnia Scale was chosen for this study because of its simple language, ease of questions and calculation, effectiveness, and reprint rights.[26,27]
This study showed a prevalence of chronic insomnia in 33% in the sample population surveyed, with females being more affected compared to males but in statistically insignificant values. There was a significant prevalence in patients having diabetes irrespective of the duration of diabetes and drugs taken. Increasing age was also a significant contributor to insomnia in adults. There was no major correlation with education/social/economic factors and comorbid conditions such as hypertension, asthma, migraine, heart diseases, and liver or kidney diseases.
There is also poor knowledge and awareness about sleep disorders and their health-related negative consequences in our population.
Conclusion
Insomnia is a common sleep disorder which is many times missed by a primary care physician until/unless asked for; the prevalence of which was as high as 33% in this study. Diabetes and increasing age were significantly associated with insomnia. Hence, all diabetic patients should be screened for insomnia by the primary care physician/diabetologist with a self-assessed questionnaire. A caring physician should assess the sleep pattern of every patient and give adequate counseling or treatment for the same.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Diagnostic and Coding Manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. American Academy of Sleep Medicine. International Classification of Sleep Disorders. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manualof Mental Disorders. Fifth Edition (DSM-5) Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 3.American Academy of Sleep Medicine. The International Classification of Sleep Disorders – Third Edition (ICSD-3) Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 4.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30:213–8. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 5.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504. [PMC free article] [PubMed] [Google Scholar]
- 7.Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D. Sleep-related disorders among a healthy population in South India. Neurol India. 2012;60:68–74. doi: 10.4103/0028-3886.93601. [DOI] [PubMed] [Google Scholar]
- 8.Roy SK, Bhattacharjee AK, Chakraborti C, Singh R. Prevalence of insomnia in urban population of west Bengal: A community based cross sectional study. Int J Med Public Health. 2015;5:293–6. [Google Scholar]
- 9.Yardi N, Adsule S. A cross-sectional observational study to determine the prevalence of insomnia amongst Indian corporate employees. J Assoc Physicians India. 2015;63:20–5. [PubMed] [Google Scholar]
- 10.Blümel JE, Cano A, Mezones-Holguín E, Barón G, Bencosme A, Benítez Z, et al. A multinational study of sleep disorders during female mid-life. Maturitas. 2012;72:359–66. doi: 10.1016/j.maturitas.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Xu M, Bélanger L, Ivers H, Guay B, Zhang J, Morin CM. Comparison of subjective and objective sleep quality in menopausal and non-menopausal women with insomnia. Sleep Med. 2011;12:65–9. doi: 10.1016/j.sleep.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Rybarczyk B, Lund HG, Garroway AM, Mack L. Cognitive behavioraltherapy for insomnia in older adults: Background, evidence, and overview of treatment protocol. Clin Gerontol. 2013;36:70–93. [Google Scholar]
- 13.Ohayon MM. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 14.Smith MT, Perlis ML, Park A, Smith MS, Pennington J, Giles DE, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. 2002;159:5–11. doi: 10.1176/appi.ajp.159.1.5. [DOI] [PubMed] [Google Scholar]
- 15.Léger D, Poursain B, Neubauer D, Uchiyama M. An international survey of sleeping problems in the general population. Curr Med Res Opin. 2008;24:307–17. doi: 10.1185/030079907x253771. [DOI] [PubMed] [Google Scholar]
- 16.Zailinawati AH, Mazza D, Teng CL. Prevalence of insomnia and its impact on daily function amongst Malaysian primary care patients. Asia Pac Fam Med. 2012;11:9. doi: 10.1186/1447-056X-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glidewell RN, Roby EK, Orr WC. Is insomnia an independent predictor of obstructive sleep apnea? J Am Board Fam Med. 2012;25:104–10. doi: 10.3122/jabfm.2012.01.110123. [DOI] [PubMed] [Google Scholar]
- 18.Wong SH, Ng BY. Review of sleep studies of patients with chronic insomnia at a sleep disorder unit. Singapore Med J. 2015;56:317–23. doi: 10.11622/smedj.2015089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morin CM, LeBlanc M, Daley M, Gregoire JP, Mérette C. Epidemiology of insomnia: Prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Pigeon WR. Diagnosis, prevalence, pathways, consequences and treatment of insomnia. Indian J Med Res. 2010;131:321–32. [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Berglund PA, Coulouvrat C, Fitzgerald T, Hajak G, Roth T, et al. Insomnia, comorbidity, and risk of injury among insured Americans: Results from the America Insomnia Survey. Sleep. 2012;35:825–34. doi: 10.5665/sleep.1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. Sleep Disorders: Diagnostic and Statistical Manual of Mental Disorders: Diagnostic Criteria for Primary Insomnia. Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. pp. 597–661. [Google Scholar]
- 23.American Academy of Sleep Medicine. The International Classification of Sleep Disorders, Revised. Westchester, Ill: American Academy of Sleep Medicine; 1997. [Google Scholar]
- 24.World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders. World Health Organization, Geneva, Switzerland 26. TOP. Assessment to Diagnosis: Insomnia. Toward Optimized Practice (TOP) Program. 1992. [Last accessed on 2016 Sep 12]. Available from: http://www.topalbertadoctors.org/cpgs/?sid=18 and cpgcats=79 .
- 25.World health organization. The ICD-10 Classification of Mental and Behavioral Disorders. Geneva, Switzerland: WHO; 1992. [Google Scholar]
- 26.Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens insomnia scale: Validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48:555–60. doi: 10.1016/s0022-3999(00)00095-7. [DOI] [PubMed] [Google Scholar]
- 27.Soldatos CR, Dikeos DG, Paparrigopoulos TJ. The diagnostic validity of the Athens insomnia scale. J Psychosom Res. 2003;55:263–7. doi: 10.1016/s0022-3999(02)00604-9. [DOI] [PubMed] [Google Scholar]


