Abstract
Introduction:
Telemedicine incorporates electronic information and medical technology. It connects healthcare through vast distances which would benefit both patients and doctors. The aim of this questionnaire study was to evaluate the effects of telemedicine on patients and medical specialists.
Methods:
A cross-sectional study was conducted among 122 participants (71 patients and 51 doctors) on satisfaction in quality of service, cost-effectiveness, and problems encountered in healthcare provided by the telemedicine in Apollo Tele Health Services, Hyderabad, Telangana, India. The data for each group were calculated and compared.
Results:
About 80% patients and all the doctors reported their satisfaction on the quality of treatment given through telemedicine. Approximately, 90% of the participants found telemedicine cost-effective and 61% of the doctors found an increase in patient's inflow apart for their regular practice. Problems encountered in telemedicine were 47% in technical issues and 39% in time scheduling by doctors and 31% of patients were uncomfortable to face the camera, and 24% had technical issues.
Conclusions:
The results of the present study showed that telemedicine in healthcare could prove to be useful to patients in distant regions and to rural doctors in India. In the near future, telemedicine can be considered as an alternate to face to face patient care.
Keywords: Clinical medicine, health care, telehealth, telemedicine
Introduction
Health-care delivery follows a three-tier system, and health is the primary responsibility of the state. There is a difference in quality and accessibility to health care between urban and rural regions.[1] The North Eastern states in India are especially affected by poverty, nondevelopment, and civil conflict. The major limitations to the growth and development in these states have been limited infrastructure in the region and poor connectivity with the rest of the country.[2] This discrepancy in health care amid rural and urban regions can be bridged through telemedicine technology which can be integrated into the existing health-care delivery system. It is far easier to set up a telecommunication infrastructure in suburban and rural India than to place hundreds of medical specialists in these locations.[3]
Both government and private sectors have actively participated and contributed to various telemedicine activities. Telemedicine has been supported by the Indian Space Research Organization and the Department of Information Technology and implemented through the state governments.[4] A few corporate hospitals have developed their own telemedicine networks; one among them is Apollo Telemedicine Networking Foundation, which started telemedicine operations in January 2000.[5]
Telemedicine is defined as “the delivery of healthcare services, where distance is a critical factor, by all health-care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for the continuing education of health-care providers, all in the interests of advancing the health of individuals and their communities” (WHO 1998).[6] The prefix “tele” derives its meaning from Greek word “telos” which means “at a distance” hence telemedicine is medicine at a distance.[7] Patients and health-care experts who are used to personal visits may be hesitant to change their conventional methods of health care. This study was conducted to find out the perception of medical specialists and patients toward the upcoming telemedicine health-care service on the subject matter of cost-effectiveness, satisfaction on the quality of service, and problems encountered herein.
Materials and Methods
This study is a cross-sectional pilot questionnaire study conducted in a nodal Telemedicine Speciality Centre (TSC) in Apollo Hospital, Hyderabad, Telangana, India. The study was conducted in two phases – the first phase was a separate questionnaire for the medical specialists from different branches of medicine. The second phase was questions for the patients from the North Eastern states of India. The questions were close-ended; self-designed, and developed in English language by Dr. Rajesh V. Acharya. The questionnaire consisted of 13 questions pertaining to specialist perception and 9 questions concerning patient's point of view on satisfaction on the quality of service, economical feasibility in telemedicine and problems related to it.
The questionnaire was pretested for validity and reliability and modified accordingly. Reliability of questionnaire was tested using Cronbach's alpha. Reliability of specialists is good (alpha = 0.845) reliability of patients is acceptable (alpha = 0.765). To validate patient's questionnaire, paired t-test was used. P value was found to be not significant (P > 0.859) hence the questionnaire is validated. The study was approved by the Institutional Ethical Committee and written consent was obtained after providing all the relevant information about the study to the participants. The study was conducted over a period of 3 months from June to August 2013.
The first phase of the study included 71 specialists from different branches of medicine who worked in TSC, Apollo Hospital, Hyderabad. For the second phase of the study, 51 respondents were chosen from the North Eastern Regions of India (Assam, Nagaland, Siliguri, Sikkim, and Manipur). Patients were selected randomly from the registry of Apollo Telemedicine Consulting Centre (TCC) who were using telemedicine. The inclusion criteria were that all the respondents have used telemedicine services before; were willing to give written informed consent and willing to take part in the study. The exclusion criteria were participants who did not complete the questionnaire or were not willing to take part in the study. Data for the questionnaire were collected through e-mail and direct contact with the doctors and through telephonic conversation and e-mail with the patients.
The process of telemedicine includes connectivity between a TCC and a TSC. A TCC has various medical equipment such as computed tomography scan, color Doppler, and electrocardiography machine that have been integrated with the telemedicine software (MedIntegra) where the specialist at the TSC will be able to view the medical details and images of the patient. The consulting center has a high-end digital imaging and communications in medicine scanner for scanning X-rays and reports, for transmitting them to the specialty center, a web camera for net meetings, and video conferencing equipment for video conference between the patients at TCC and the specialist at the TSC. The connectivity from the TCC to the TSC can be through either one of the channels; internet protocol, leased line Integrated Service Digital Networks, or Very Small Aperture Terminal.
Statistical analysis
Data generated from the questionnaire were coded and imputed into the computer system and analyzed using Data Analysis and Statistical Software (STATA version 13; StataCorp LP, Texas, USA). Data were analyzed in terms of frequency percentages and parametric statistics like a mean and standard deviation. Qualitative data obtained from the respondents during the interview were also utilized to get the complete picture of telemedicine process and challenges.
Results
Apollo Tele Health Services provides infrastructure to the 116 specialists who practice telemedicine in the TSC and to the patients in TCC. A total of 51 specialists took part in this questionnaire survey. The profile of the doctors at TSC was summarized in Table 1. Seventy-one patients took part in the study. All the patients in this study had used the Apollo TCCs near their hometown either through e-mail, telephonic conversation, or video conferencing with a specialist. The complaints of patients varied from a headache to consultation and/or treatment in Orthopedics, Neurology, Cardiology, Psychiatry, Urology, Dermatology, General Medicine, Obstetrics and Gynecology, Rheumatology, and Oncology. The duration of treatment given through telemedicine ranges from one visit to as long as a year depending on the nature of cares given to the patient.
Table 1.
Details of specialists using telemedicine

Perception on telemedicine practice
All the doctors had telemedicine experience; 55% of the participants had 10–20 consultations per day, 22% had more than 20 consultations per day. Sixty-five percent of participants devoted 1–2 h per day of their time for consultation using telemedicine. All the doctors were satisfied with the treatment given through TSC. Ninety-four percent of the respondents answered that they got desirable results on the diagnosis of patient's condition. Recall percent of patients in this study was 71%. About 94% of providers were open to promoting telemedicine [Table 1].
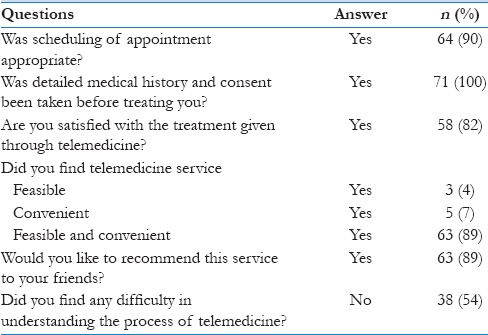
About 90% of the respondents said their appointment was scheduled according to their convenience. About 82% of the participants were satisfied with the treatment given through the medium of telemedicine and that they would recommend this medium to their relative and friends. Fifty-four percent of the patients acknowledged that they did not have a problem in understanding the usage of telemedicine [Table 2].
Table 2.
Patients feedback questionnaire
Cost-effectiveness on telemedicine
About 89% of the patients stated that the treatment was both feasible and convenient; 7% felt treatment through telemedicine was costly for them but convenient, and 4% of the participants felt it was economical but not convenient [Table 2].
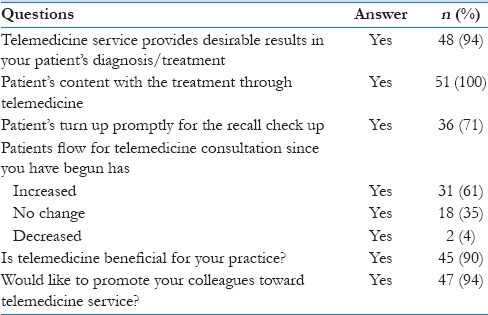
About 90% of the specialists reported that telemedicine was beneficial for them, and 61% patient's inflow increased since the commencement of telemedicine practice as compared to 35% who reported no change [Table 3].
Table 3.
Questions for the specialist
Problems encountered in telemedicine
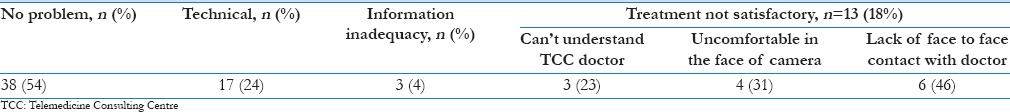
Issues faced by patients with the use of telemedicine were 24% on technical issues, and 18% were not satisfied with the treatment provided of which the major issue was not comfortable to face the camera and lack of personal face to face contact with the doctor [Table 4].
Table 4.
Problems encountered by patients
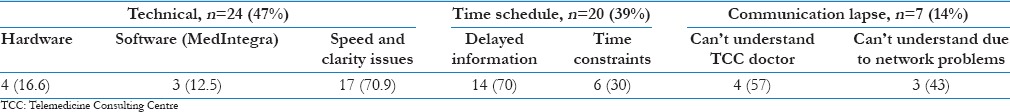
During the consultation, the doctors faced issues on the technical subject (47%), time scheduling (39%), and few of them (14%) had problems with communication lapse. None of the respondents had problems with the staff in TSC or TCC [Table 5].
Table 5.
Problems encountered by specialists
Discussion
The questions framed in this study were appropriate in pursuing the issue linked to telemedicine process from a patient's and doctor's point of view. Self-reporting approach was used for the data collection, which is considered to be appropriate for assessing physicians’ intention to adopt telemedicine technology. This method of collecting data through a questionnaire has been and has been proven to be effective.[8] The feedback from this survey will help to learn and evaluate the facets of telemedicine and its limitation. This will improve telemedicine care and make it faster, more handy, and easy to use. Telemedicine can benefit both the practitioner as well as the patient, but less is known in relation to financial benefit for both the doctor and the patient. The study was performed keeping all these points in mind.
On telemedicine practice
About 80% of the consumers were satisfied with the treatment given or provided through telemedicine which in accordance with the study done by Carr-Hill in 1992.[9] The reasons suggested for high patient, and provider satisfaction may include: easier access to specialists reduced travel period, shorter waiting times for appointments, improved effectiveness, economic savings, and increased interaction with a specialist, accurate diagnoses, and personalized care.[10]
Approximately, all the patients in a primary health care telemedicine center reported a positive impact on doctor/patient relationship.[11] In the study conducted by Greenwood et al.[12] telemedicine earned high scores even though rural patients recognize telemedicine as a one-off compared to face to face meets but they are grateful for not having to travel long distances for consultations. In this study, a few percent of the patients were not comfortable facing the camera or not having direct interaction with the provider. Collins et al.[13] found no distinction among telemedicine group and traditional group when questioned about the overall care.
Waller and Gilbody[14] found 56% of the participants completed a full course of therapy using telemedicine as compared to our 71% in our study and reported that the dropout rates were not due to the technology but more to do with people's personal circumstances, which would also apply to face to face fallouts. Andrew et al.[15] in a systematic review of 22 randomized control trials found that more often patients (86%) were satisfied and adhered to e-therapy, despite the reduced face to face contact.
In hospitals in the eastern province of Saudi Arabia, only 33.3% of health-care personnel were implementing telemedicine.[16] In comparison with our study, 44% of the specialist took part in the study. Considerable difference in years of experience in telemedicine was seen in the Saudi Arabian study; where consultants (56%) and those with more than 10–20 years of experience (48%) represented the highest frequency of actual implementation of telemedicine which was also seen in our study. Years of experience and knowledge gives them more insight for the requirement of new technology to improve and develop the quality of care.
Richards et al.[17] reported optimistic feedback from the practitioners particularly in the area of telemedicine's clinical utility (76%) and ease of use (74%) which was similar to our study. Ghia et al.[18] conducted a study in rural Maharashtra, India on the perception of telemedicine in 210 different health-care providers in the region. Forty-eight percent of the doctors strongly agreed that telemedicine should be implemented in all hospitals, 40% of the doctors agreed that telemedicine will increase the access of health care services for rural patients and 42% of the doctors strongly agreed that telemedicine will help to save the time and money of the patients. Physicians were very satisfied with both video visits and in person, but face to face examinations were preferred (P < 0.001). Skinner and Latchford in 2006[19] showed growing evidence that e-therapy can be clinically effective and clients can develop good therapeutic relationships.
Enright[20] conducted a study in Dublin in which the following areas were queried on: Current usage of technology were staff and patients happy with telemedicine solutions in receiving/giving care and with the comfort of use. Fifty-one participants took part in the study. Approximately, 38%–50% of respondents stated that they would be interested in using video conferencing.
Cost-effectiveness of telemedicine
In the study conducted by Dick et al.[21] 71% of patients responded with high scores on pediatric telemedicine consultations with cost savings of more than 1000$ per patient. Study have shown that using telemedicine in rural areas doctors can help patients as it reduces travel time, costs, and decreases the need to take time off work for patients.[20]
Individuals adopting telemedicine in Saudi Arabia recognized the benefits of telehealth as improving the quality of care, enhancing access to healthcare, and salvaging time and money.[16] Ekeland et al. in 2010[22] conducted a systematic review on the effectiveness of telemedicine and found effectiveness in the use of telemedicine but limited evidence of cost-effectiveness. A Canadian study was carried out to find evidence for the use of telehealth technology, and it was found that the benefits were an immediate response from doctors, easy accessibility, time and money saved.[23] A study was carried out on direct costs of conducting clinical interviews through real-time video conferencing versus in-person sessions with American Indians in rural locations in 2007. This study revealed that the transmission costs were less expensive than in-person sessions for providers. Shore et al.[24] concluded from this study that telehealth may result in increased effectiveness and reduction in the cost of research with rural, remote, and underserved populations.
Barriers to telemedicine
The barriers in execution and continuance of telemedicine in rural areas were provision to the adequacy of bandwidth, power and equipment repairs. The barriers to effectively implement telemedicine in rural areas were identified through the study done by Ghia et al.[18] in India which states inclusion of heavy investments in equipment, technical difficulties, concerns regarding patient confidentiality, negative attitude of patients, lack of user-friendly software, lack of staff educated in information technology, illiteracy, diversity in languages, and concern about legal responsibility.
Barriers reported in the Saudi Arabia study were the lack of basic knowledge and benefits of telemedicine (49%), difficulty in application (29%), and the lack of time to adopt telemedicine (22%);[16] in our study, the problems faced were with clarity and speed of network; not receiving information from the technician in time and time constraints. Shore et al.[24] in his study observed that if individuals are not shown how to use the technology, this can lead to disappointment. This could be remedied by education, knowledge, and early on-site support.
As this is a pilot study, 44% of the providers took part in the study which is satisfactory for a pilot study. A pilot study should be 10%–20% of the intended population (Baker, 1994).[25] The limitations of the study were that the responses of the questionnaire were prone to respondent bias; the results were limited to one group in each phase of the study. Studies with larger sample size and different groups comparing telemedicine care to face to face patient care could be performed.
Conclusions
Telemedicine has a variety of applications including critical care monitoring, telemedicine procedures/surgery, robotics, disease surveillance and program tracking, disaster management and continuing medical education and public awareness.[26] Seventy percent of our population lives in rural India, 90% of secondary and tertiary care facilities are in the cities and towns far away from the rural regions. As shown in this study, a significant proportion of patients in these remote locations could be productively managed with some advice and guidance from specialists and super-specialists in the cities and towns with the help of telemedicine.[25] In September 2005, Ministry of Health and Family Welfare, Government of India has taken the initiative to constitute National Task Force on Telemedicine.[27] National Health Policy 2015 draft was outlined to focus on a number of topics including improved deployment of information and communications technology for advancing the outcome of the Indian Health Care System.[28] At present, India has 500 telemedicine nodes across the country, and many more are in the pipeline.[29]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Materna B. Advances in International Telemedicine and eHealth Around the World. Vol. 1. Warsaw: Medipage Ltd; 2006. [Last cited on 2015 Jun 04]. pp. 9–68. Available from: http://www.aehti.eu/Advances_vol_1.pdf . [Google Scholar]
- 2.India's North-East Diversifying Growth Opportunities. Indian Chamber Commerce. [Last cited on 2015 May 25]. Available from: https://www.pwc.in/en_IN/in/assets/pdfs/publications/2013/north-east_summit-2013.pdf .
- 3.Dasgupta A, Deb S. Telemedicine: A new horizon in public health in India. Indian J Community Med. 2008;33:3–8. doi: 10.4103/0970-0218.39234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mishra S, Ganapathy K, Bedi BS. The Current Status of eHealth Initiatives in India. [Last cited on 2015 Jun 02]. Available from: http://www.ehealth-connection.org/files/conf-materials/Current%20Status%20of%20eHealth%20Initiatives%20in%20India_0.pdf .
- 5.Gupta RP. Telehealth Report – India 2011. Telemedicine Society of India. [Last cited on 2015 Jun 04]. Available from: http://www.slideshare.net/rajendrapgupta/telehealth-report-india .
- 6.World Health Organization. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009. Switzerland: WHO Press; 2009. [Last cited on 2015 May 25]. Available from: http://www.who.int/goe/publications/goe_telemedicine_2010.pdf . [Google Scholar]
- 7.Craig J, Patterson V. Introduction to the practice of telemedicine. J Telemed Telecare. 2005;11:3–9. doi: 10.1177/1357633X0501100102. [DOI] [PubMed] [Google Scholar]
- 8.Croteau AM, Vieru D. 35th Annual Hawaii International Conference on System Sciences (HICSS’02) Maui (Hawaii): IEEE Computer Society; 2002. Telemedicine adoption by different groups of physicians. [Google Scholar]
- 9.Carr-Hill RA. The measurement of patient satisfaction. J Public Health Med. 1992;14:236–49. [PubMed] [Google Scholar]
- 10.Whitten P, Love B. Patient and provider satisfaction with the use of telemedicine: Overview and rationale for cautious enthusiasm. J Postgrad Med. 2005;51:294–300. [PubMed] [Google Scholar]
- 11.Bratton RL, Cody C. Telemedicine applications in primary care: A geriatric patient pilot project. Mayo Clin Proc. 2000;75:365–8. doi: 10.4065/75.4.365. [DOI] [PubMed] [Google Scholar]
- 12.Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12:268–72. doi: 10.1080/j.1039-8562.2004.02097.x. [DOI] [PubMed] [Google Scholar]
- 13.Collins K, Walters S, Bowns I. Patient satisfaction with teledermatology: Quantitative and qualitative results from a randomized controlled trial. J Telemed Telecare. 2004;10:29–33. doi: 10.1258/135763304322764167. [DOI] [PubMed] [Google Scholar]
- 14.Waller R, Gilbody S. Barriers to the uptake of computerized cognitive behavioural therapy: A systematic review of the quantitative and qualitative evidence. Psychol Med. 2009;39:705–12. doi: 10.1017/S0033291708004224. [DOI] [PubMed] [Google Scholar]
- 15.Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PLoS One. 2010;5:e13196. doi: 10.1371/journal.pone.0013196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El-Mahalli AA, El-Khafif SH, Al-Qahtani MF. Successes and challenges in the implementation and application of telemedicine in the eastern province of Saudi Arabia. Perspect Health Inf Manag. 2012;9:1–27. [PMC free article] [PubMed] [Google Scholar]
- 17.Richards H, King G, Reid M, Selvaraj S, McNicol I, Brebner E, et al. Remote working: Survey of attitudes to eHealth of doctors and nurses in rural general practices in the United Kingdom. Fam Pract. 2005;22:2–7. doi: 10.1093/fampra/cmh716. [DOI] [PubMed] [Google Scholar]
- 18.Ghia CJ, Patil AS, Ved JK, Jha RK. Benefits of telemedicine and barriers to its effective implementation in rural India: A multicentric E-survey. [Last cited on 2015 May 26];Indian Medical Gazette. 2013 145:1–7. Available from: http://www.medind.nic.in/ice/t13/i1/icet13i1p1.pdf . [Google Scholar]
- 19.Skinner A, Latchford G. Attitudes to counselling via the internet: A comparison between in-person counselling clients and internet support group users. Couns Psychother Res. 2006;6:92–7. [Google Scholar]
- 20.Enright A. Telemedicine is Perceived to be Cost Effective by Health Organizations, with Many Wishing to Implement: But what are the Views of Staff and Patients? Dublin University; 2012. [Last cited on 2015 May 19]. Available from: https://www.scss.tcd.ie/postgraduate/health-informatics/assets/pdfs/Msc%20Aislinn%20enright%2004092012.pdf . [Google Scholar]
- 21.Dick PT, Filler R, Pavan A. Participant satisfaction and comfort with multidisciplinary pediatric telemedicine consultations. J Pediatr Surg. 1999;34:137–41. doi: 10.1016/s0022-3468(99)90244-0. [DOI] [PubMed] [Google Scholar]
- 22.Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: A systematic review of reviews. Int J Med Inform. 2010;79:736–71. doi: 10.1016/j.ijmedinf.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Telehealth Benefits and Adoption – Connecting People and Providers Across Canada a Study Commissioned by Canada Health Infoway. 2011. [Last cited on 2015 May 23]. Available from: http://www.file:///C:/Documents%20and%20Settings/kmsdch036/My%20Documents/Downloads/telehealth_report_2010_en.pdf .
- 24.Shore JH, Brooks E, Savin DM, Manson SM, Libby AM. An economic evaluation of telehealth data collection with rural populations. Psychiatr Serv. 2007;58:830–5. doi: 10.1176/ps.2007.58.6.830. [DOI] [PubMed] [Google Scholar]
- 25.Baker TL. Doing Social Research. 2nd ed. New York: McGraw-Hill Inc; 1996. [Google Scholar]
- 26.Major J. Telemedicine room design. J Telemed Telecare. 2005;11:10–4. doi: 10.1177/1357633X0501100103. [DOI] [PubMed] [Google Scholar]
- 27.Iyer M, Dev N, Joy JK. Telemedicine in India. Health and Medicine. 2014. [Last cited on 2015 Jun 03]. Available from: http://www.slideshare.net/ManishaS2/telemedicine-in-india-design-research?related=1 .
- 28.Ministry of Health & Family Welfare. National Health Policy 2015 Draft. India: 2014. [Last cited on 2016 Jan 08]. Available from: http://www.mohfw.nic.in/showfile.php?lid=3014 . [Google Scholar]
- 29.Telemedicine Adoption in India; the New Drivers. Elets News Network (ENN) 2007. [Last cited on 2015 Jun 03]. Available from: http://www.egoveletsonline.com/2007/05/telemedicine-adoption-in-india-the-new-drivers/


