Abstract
Introduction:
Janani Suraksha Yojana (JSY) direct benefit transfer scheme was launched in the year 2013 in India and there is a paucity of information affecting it. The study aimed to assess the proportion of eligible beneficiaries utilizing JSY direct cash benefit transfer in Puducherry and to identify its barriers and facilitating factors.
Methods:
This cross sectional study was conducted from January to March 2015 among 152 eligible JSY beneficiaries residing in rural and urban field practice areas of a tertiary care institution in Puducherry, India. Data were collected using a pretested semi structured questionnaire and presented as proportion or percentages.
Results:
About 144 beneficiaries participated in the study with a response rate of 94.7%. About 46% (66) of them availed cash transfer benefit. The mean time of receiving the benefit is 95.8 days (interquartile range 60–120 days). Among those who have not received (78), about 49 (62.8%) had not applied and 29 (37.18%) filled applications were rejected due to various reasons. About 77.1% (111) of beneficiaries were informed about JSY scheme through health workers. About 52.1% (75/144) still preferred direct bank transfer through the bank. The reasons for not availing benefits includes not having a bank account (24.3%), followed by not having Aadhaar number (9.7%), 11.8% had no ration card, and 13.8% stayed in their mother house.
Conclusion:
Majority of the beneficiaries did not receive direct cash transfer benefits in urban area than rural area and there is a need to simplify the procedures to improve the uptake of services to this group.
Keywords: Beneficiaries, direct benefit transfer, Janani Suraksha Yojana
Introduction
Conditional cash transfer schemes are intended as a financial incentive given to the beneficiaries to follow health-seeking behaviors and to improve the utilization of health schemes by reducing or eliminating economic barriers in availing the benefits.[1] Janani Suraksha Yojana (JSY) is a conditional cash transfer scheme with the aim of promoting institution delivery. In high performing states, a financial incentive of Rs. 700 for rural area and Rs. 600 for urban area is provided for this purpose.[2] The government started providing assistance to JSY beneficiaries through the direct benefits transfer (DBT) model since the year 2013.[3]
Multiskilled competent primary care provider's knowledge is an important issue to be considered in evolving schemes and initiatives of our health-care systems.[4] There are many hurdles in the delivery of cash incentives to the beneficiaries under JSY scheme. A study conducted by Behera et al. in North India reported a delay in JSY cash delivery even up to 1 year.[5] Another study in Madhya Pradesh found difficulty in getting money due to Aadhaar-linked direct cash transfer because women need their own bank account and they (94.33%) preferred immediate cash instead of bank transfer.[6] A recent World Bank study estimates bank account penetration across India as 35%, a rate that falls even lower for the poorest households. Many cash transfer schemes will cause nonpayment, late payment, or inadequate payment to the beneficiaries.[7] A recent Supreme Court judgment insisted that Aadhaar is not mandatory for government schemes, but it is not followed in many states.[8] In view of the above, it is important to introspect the factors influencing JSY DBT scheme.
Some studies evaluated the JSY cash scheme through direct cash benefit,[5] but studies focused on Aadhaar-enabled DBT to the bank account of the beneficiaries are limited in India. There is also a paucity of JSY data in the urban and rural areas regarding the proportion of eligible JSY beneficiaries receiving DBT. With this background, the study aimed to assess the proportion of eligible beneficiaries utilizing JSY cash benefits in Puducherry and to identify the barriers and facilitating factors in availing JSY cash benefits in this area. The information may help the concerned authorities or policymakers for corrective measures required for improvement of the JSY system.
Materials and Methods
Setting
This cross-sectional study was conducted from January to March 2015 among eligible JSY beneficiaries residing in rural and urban field practice areas of a tertiary care medical institution in Puducherry, India.
Sample size calculation and sampling technique
Using a proportion of 30.1% as beneficiaries of JSY cash scheme from Vikram et al.'s study[9] and relative precision as 30% and 10% of nonresponse rate, the minimum sample size was 115. However, it was decided to interview all 152 beneficiaries present in institute rural and urban health center service area in Puducherry, India. All JSY eligible beneficiaries confirmed with birth and the antenatal register registered in the institute rural and urban health center and delivered from September 1, 2013, to August 31, 2014, were included in the study.
Method of data collection
The study was approved by the Scientific and Ethical Committee of the Institute. The purpose of the study was explained to the study subjects and written informed consent was taken. At the first step, JSY eligible beneficiaries were contacted by the principal investigator through the house-to-house survey. This part of the study collected the data on the proportion of eligible beneficiaries utilizing JSY cash transfer benefits and barriers and facilitating factors in availing JSY cash transfer benefits using a pretested semi-structured questionnaire.
Data were entered in Statistical Package for Social Sciences (SPSS) version 19 (PASW STATISTICS-19.0, IBM) and analyzed using proportion or percentages.
Results
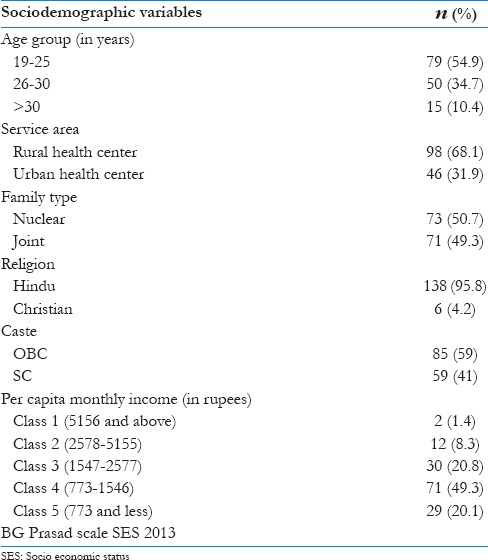
About 144 subjects beneficiaries in the study with a response rate of 94.7% (144/152). About 98 beneficiaries participated from the rural health center and 46 beneficiaries participated from the urban health center. More than half of the beneficiaries (54.9%) belong to 19–25 years of women. The proportion of scheduled caste mothers was 41% (59) and OBC was 59% (85). Most of the beneficiaries were Hindu, i.e., 138 (95.8%), and nearly half of the beneficiaries were in the joint family, i.e., 71 (49.3%). About 130 (79%) beneficiaries per capita income was below class 3 category [Table 1].
Table 1.
Distribution of sociodemographic variables of beneficiaries (n=144)
About 46% (66) of the eligible beneficiaries availed cash transfer benefit while 54% (78) did not receive it. Of 46 beneficiaries from the urban health center, 30 (65.21%) had availed the cash transfer benefits. However, in rural health center area, of 98 beneficiaries, only 36 (36.73%) availed JSY cash transfer benefits.
Among those who have not received (78), about 49 (62.8%) had not applied and 29 (37.18%) of women gave filled application which was rejected due to various reasons. Those who received it (66) knew their information on receiving the cash benefits by checking the bank accounts (46, 69.7%), SMS (15, 22.7%), Anganwadi worker (3, 4.5%), and health worker (2, 3%).
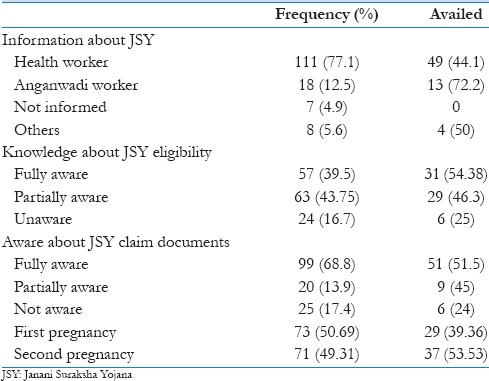
The mean time of receiving the benefit is 95.8 days (interquartile range-60–120 days) [Table 2]. About 77.1% of beneficiaries were informed about JSY scheme through health workers and 12.5% of beneficiaries by Anganwadi worker and 4.9% of women were uninformed by anyone and the rest of them by others. About knowledge on JSY eligibility, around 40% of women rightly told about eligibility criteria [Table 3].
Table 2.
Distribution of receiving cash benefit according to time since delivery (n=66)
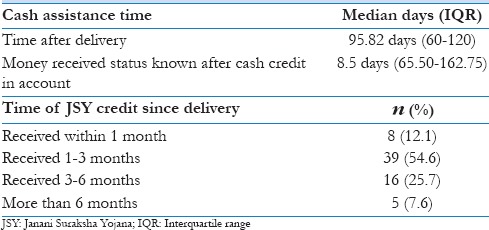
Table 3.
Distribution of factors related to receiving cash benefits (n=144)
Of 66 beneficiaries who availed JSY money, about 51.52% (34) felt delay in getting the cash benefits and the rest, i.e., 48.48% (32), did not feel any delay. Among 24 beneficiaries who felt difficulty in getting JSY benefit, about 9 (37.5%) women faced difficulty due to cumbersome procedure in collecting the required documents, followed by 9 (37.5%) felt difficulty in opening bank account and the rest 6 (25%) told leaving the child in home, staff unavailable, and crowd in bank.
Of 66, nearly half of the beneficiaries, i.e., 29 (43.9%), have not spent the given money, and it was in a personal savings account. Around 11 (16.7%) beneficiaries used for general family expenditure and 16 (24.2%) beneficiaries used for child requirement and only 5 (7.5) used for mother health needs. A few women, i.e., 5 (7.5%), used for their personal use.
About 75/144 (52.1%) preferred direct bank transfer through bank, followed by direct cash 67 (46.5%) and rest wanted a check. Among the beneficiaries who preferred cash, 46% opined that they could meet the emergency need at the time of delivery and 33% of them said that they could reduce delay in availing cash benefits. Among those who prefer bank transfer, 66% of them said that it could be helpful in future savings, and 33% told that they could meet expenses when need arises.
About 24.3% of beneficiaries had not bank account, followed by 9.7% of women not having Aadhaar account, 11.8% not having ration card, 13.8% of beneficiaries stayed in their mother house after delivery, around 18% of women did not get JSY money due to late submission and lack of help from their husband, 4.1% of women have not got any information from the health workers, 4.86% have not any interest to apply, and around 18% of them told problem in National Rural Health Mission (NRHM) processing problem [Figure 1].
Figure 1.
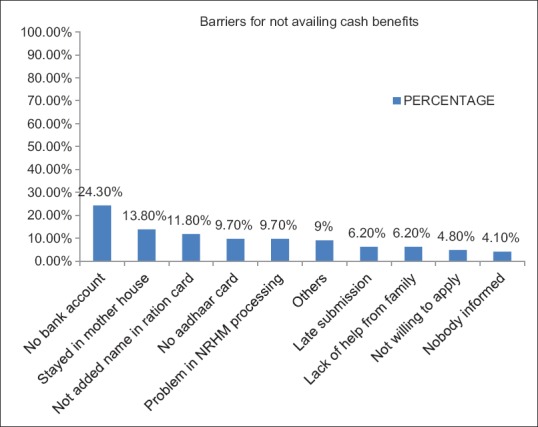
Barriers in availing Janani Suraksha Yojana cash benefit (n = 78)
Discussion
As per the Indian Public Health Standards, one of the important duties of primary care physicians working in government health centers and accredited private hospitals is to provide facilities under JSY and timely payment of money to JSY beneficiaries, which will increase institutional deliveries and also reduce the out-of-pocket expenditure among them to a certain extent.[10] Primary health-care physicians working in government health centers such as primary health centers, community health centers, district or state level hospitals, and accredited private hospitals should aware and disseminate the information regarding these benefits to the beneficiaries so that effective care can be given to the mother and baby in the hospital during delivery and afterward. Under the JSY scheme, if a doctor is not available or that the list of empaneled doctors is very few, specialist doctors from the private sector also may be empaneled to conduct cesarean section or management of obstetric complications. In this regard, the contribution of primary care physicians in the delivery of JSY scheme is of paramount important in the health-care delivery system.
Our study showed that nearly half of the eligible beneficiaries received the cash transfer benefit to their bank account, which is comparable to other studies where direct cash was given to the beneficiaries. However, in rural area, the availability of this benefit was comparatively less than other studies. Panja et al. showed that among JSY eligible beneficiary, about 50.5% of women received JSY cash benefits.[11] Another study carried out in New Delhi by Vikram et al. found that 30.1% of eligible JSY beneficiary availed cash benefits, whereas the United Nations Fund for Population Activities (UNFPA) concurrent assessment study in 2009 showed that 76.2% of women availed JSY money.[9,12] The different findings in various studies may be due to the influence of various factors across different states at the country level. Less percentage of women received JSY cash transfer benefits, especially in the rural area in this study, may be due to nonavailability of bank account with Aadhaar proof, which resulted in nonsubmission of documents to the National Health Mission Authorities.
Our study highlighted that the money was received late after the delivery. Singh and Tamulee's results showed that 68% of women received JSY money immediately and remaining 32% of women received after 6 months to 1 year.[13] Behera et al. found that 7.6% of women received money in 1 month, and 48.8% of subjects received after 3 months.[5] In general, JSY money should be received within 1 week after submission of documents. In the state government hospital primary health centers, the required documents will be collected immediately after delivery, whereas women delivered in a private hospital has to submit their required proof to the respective primary health center. In such a situation, women have not presented their evidence in a prescribed time with the necessary proof. Some of the other reasons for the delay may be due to the tradition of staying in the mother's house after delivery.
In this study, 43.9% of women have not spent their availed JSY money. In Sandeep and Malik JS study, nearly half of the JSY mothers (47.22%) spent JSY money for the purpose of child and self-care, while remaining proportion (52.78%) of JSY mothers were utilized for general family expenditure.[14] In this study, many women had not gone to the bank to take the money and kept the money in the savings account itself. Although some beneficiary spent their money for family general expenditure, majority of them did not use for the medicine, nutrition, and need of the mother or child.
Facilitating factors and barriers
In this study, about three-fourth of beneficiary was informed about JSY scheme through health worker. The majority (83.3%) of women correctly said the eligibility criteria of the scheme. About 82.6% of women were partially or fully aware of the required documents to get the JSY money. Only 39.36% of women availed money in the first pregnancy, and in the second pregnancy, it was 53.53%. Singh and Tamulee's study showed that 72.7% of women had information about JSY through neighbor and 18.4% of women through the accredited social health activists (ASHA) in contrast to our study, where ASHA worker is not there in the health-care system.[13] Studies on assessment of awareness level of eligibility and knowledge on documents required for availing JSY benefits are limited.
A study by Gupta et al. (2008–2009) showed that almost 94.3% of eligible beneficiaries preferred cash payment in contrast to 46.5% in this study.[6] Even though mobile SMS had been sent to the beneficiary after credit deposit, many of the women were not able to understand the message and the text message was sent to husband's mobile number in many cases.
Kumar et al. found difficulty in getting documents and bank account as the reason for nonavailing benefits similar to this study. The proofs required include Aadhaar card, ration card, and own bank account along with application to the NRHM office. The processing of documents was time-consuming and cumbersome. The amount of traveling cost to get the reimbursement also exceeds the given amount.[15] Aadhaar account was not there in 17 (11.8%) beneficiaries in this study similar to a Hamza and Narain's case study in Andhra Pradesh.[16] Women who come from nearby Tamil Nadu or from other service areas after marriage did not get their eligible documents such as ration card. Some of the women did not have own bank account may be due to the problem in initial deposit for opening account and/or not having correct address proof for opening bank account. There is a need to explore the possible causes for nonavailability of JSY cash benefits by further qualitative studies.
This study considered urban and rural health center beneficiaries to differentiate the issues pertaining to JSY scheme. Further identified the lacunae in the utilization of JSY cash scheme among a weaker section of society and acknowledged the problems in Aadhaar-linked DBT scheme through a bank account in availing the cash benefit. The results of the study differ from place to place because the study was conducted with a particular population in a particular geographical area, and hence, the study cannot be generalized to the whole region of the state. The study did not include noneligible JSY beneficiaries for comparison of utilization of services.
Conclusion
Majority of the beneficiaries did not receive direct cash transfer benefits and proportion is lesser in rural area. There was no bank account in the name of the beneficiary is the common reason for not receiving it. Simplify the procedures in availing direct cash transfer benefits may be considered to improve the quality of services to this group.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the support of the National Health Mission, Government of Puducherry, for giving support to conduct the study.
References
- 1.Maclennan M, Mason C, Mason E, Mbizvo M, Mendis S, Mertens T, et al. The World Health Report 2013 (Research on Universal Health Coverage) WHO Press-Luxembourg. [Last accessed on 2015 March 23]. Available from: http://www.apps.who.int/iris/bitstream/10665/85761/2/9789240690837eng.pdf?ua=1 .
- 2.Ministry of Health and Family Welfare, Government of India. New Delhi. Janani Suraksha Yojana, Features and Frequently Asked Question and Answers. Maternal Health Division. October, 2006. [Last accessed on 2015 Mar 23]. Available from: http://www.mohfw.nic.in/dofw website/JSY_features_FAQ .
- 3.Ministry of Health and Family Welfare Government of India, Health Minister Reply in Rajya Sabha about JSY Programme. Press Information Bureau. August. 2014. [Last accessed on 2015 Mar 23]. Available from: http://www.pib.nic.in/newsite/PrintRelease.aspx?relid=97339 .
- 4.Kumar R. Empowering primary care physicians in India. J Family Med Prim Care. 2012;1:1–2. doi: 10.4103/2249-4863.94438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Behera B, Kalhan M, Malik J, Punia A. Utilization of financial assistance under Janani Suraksha Yojna in Rural North India. Niger J Basic Clin Sci. 2013;10:8. [Google Scholar]
- 6.Gupta SK, Pal DK, Tiwari R, Garg R, Sarawagi R, Kumar A. Assessment of Janani Suraksha Yojana (JSY) – In Jabalpur, Madhya Pradesh: Knowledge, attitude and utilization pattern of beneficiaries: A descriptive study. Int J Curr Biol Med Sci. 2011;1:6–11. [Google Scholar]
- 7.Demirguc-Kunt A. Policy Research Working Paper, Measuring Financial Inclusion the Global Findex Database. Washington. The World Bank Development Research Group Finance and Private Sector Development Team 2012. [Last accessed on 2015 Mar 23]. Available from: http://www.econ.worldbank.org .
- 8.Rajagopal K. Don’t insist on Aadhaar, Warns SC. The Hindu (Daily). 2015 March, 16; News-National. [Last accessed on 2015 Mar 25]. Available from: http://www.thehindu.com/news/national/aadhaar-notmandatory-sc-reiterates/article6999924.ece .
- 9.Vikram K, Sharma AK, Kannan AT. Beneficiary level factors influencing Janani Suraksha Yojana utilization in urban slum population of trans-Yamuna area of Delhi. Indian J Med Res. 2013;138:340–6. [PMC free article] [PubMed] [Google Scholar]
- 10.Indian Public Health Standards (IPHS) Guidelines for Primary Health Centres, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India. 2012. [Last accessed on 2016 Jun 14]. Available from: http://www.health.bih.nic.in/Docs/Guidelines/Guidelines-PHC-2012.pdf .
- 11.Panja TK, Mukhopadhyay DK, Sinha N, Saren AB, Sinhababu A, Biswas AB. Are institutional deliveries promoted by Janani Suraksha Yojana in a district of West Bengal, India? Indian J Public Health. 2012;56:69–72. doi: 10.4103/0019-557X.96980. [DOI] [PubMed] [Google Scholar]
- 12.GFK Mode Development Research Services. Concurrent Assessment of Janani Suraksha Yojana (JSY) in Selected States. New Delhi. United Nation Population Fund-India. 2009. [Last accessed on 2015 Mar 28]. p. 7. Available from: http://countryoffice.unfpa.org/india/drive/JSYConcurrentAssessment.pdf .
- 13.Singh HS, Tamulee P. Janani Surasksha Yojana: Impact on socio-economic conditions among beneficiary families. International Journal of Scientific Research Publications. 2012;2:8–11. [Google Scholar]
- 14.Sandeep S, Malik JS. Assessment of maternal and child health (MCH) practices with a focus on Janani Suraksh Yojana (JSY) Glob J Med Public Health. 2012;1:1–9. [Google Scholar]
- 15.Kumar D, Manisha, Dwivedi A. Has Janani Suraksha Yojana Stimulated Institutional Delivery? A Study in Una District of Himachal Pradesh. Ankur Welfare Association, Reaching the Unreached: Rapid Assessment Studies of Health Programmes Implementation in India. 2009. [Last accessed on 2015 Mar 29]. pp. 19–32. Available from: http://www.chsj.org/uploads/1/0/2/1/10215849/has_janani_suraksha_yojana_stimulated_institutional__delivery_-_a_study_in_una_district_of_himachal_pradesh_-_deepak_kumar_manisha_and_archana_dwivedi.pdf .
- 16.Hamza AS, Narain N. A Case Study on Aadhaar Enabled Direct Benefit Transfer in East Godavari Micro Save (Market Led Solutions for Financial Services) 2013. [Last accessed on 2015 Mar 30]. p. 15. Available from: http://www.microsave.net/files/pdf/130213_MicroSave_Case_Study_AEDBT_East_Godavari.pdf .


