Dear Editor,
An 8-year-old girl presented with loss of consciousness, weakness on the right side of the body, jerky movements, and occasional episodes of stereotypy for 5 days. She was diagnosed with mumps 3 weeks before, which was confirmed microbiologically. With treatment, her condition initially improved. However, she began to develop slow and progressive weakness in the right side of the upper and lower limbs. Other symptoms included myoclonic seizure and drooling from the left corner of her mouth. She had paresis and hypertonia on the right side of body, deep tendon reflex was exaggerated, and she had left-sided facial palsy. She had missed her measles, mumps, and rubella immunization.
In laboratory investigations, complete blood count was normal; erythrocyte sedimentation rate was 50 mm/h. Mumps IgG titer and IgM titer were 8.20 AU/mL (<9 AU/mL) and 5.12 (<0.8), respectively. The cerebrospinal fluid (CSF) revealed glucose 44 mg/dl, protein 66 mg/dl, cell count 36/cm3 with 100% lymphocytes. Quantitative CSF IgM was 1.8 mg/dL (<0.26 mg/dL). Neither organisms nor oligoclonal bands were detected on CSF analysis. Serology and CSF polymerase chain reaction for Epstein–Barr virus, cytomegalovirus, herpes simplex virus 6, adenovirus, and parainfluenza virus were negative. A brain magnetic resonance imaging (MRI) showed ill-defined, hyperintense signal changes involving the bilateral fronto–parietal–occipital lobe parenchyma, with loss of the gray–white border distinction in the affected region on T2-weighted images [Figures 1 and 2].
Figure 1.
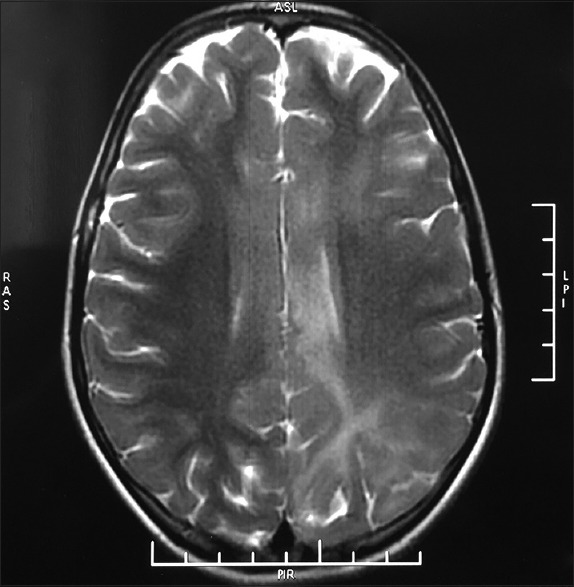
Ill-defined, hyperintense signal changes involving the bilateral fronto–parietal–occipital lobe parenchyma, with loss of the gray–white border distinction in the affected region on T2-weighted images
Figure 2.
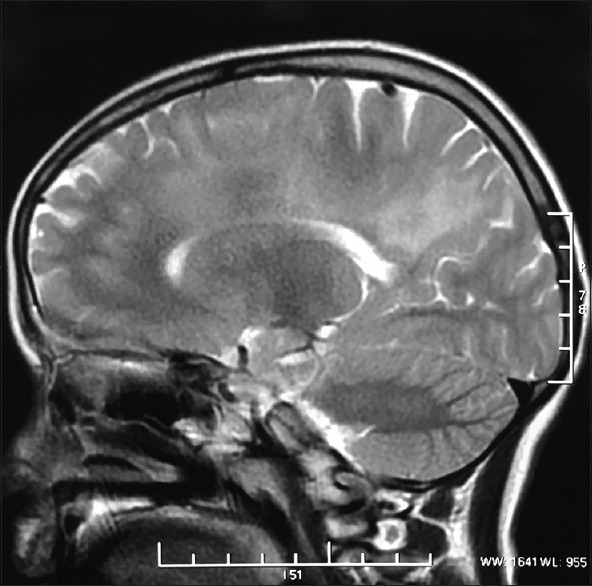
Ill-defined, hyperintense signal changes involving fronto–parietal–occipital lobe parenchyma
Based on the clinical, laboratory, and radiological findings, she was diagnosed as a case of acute disseminated encephalomyelitis (ADEM) secondary to mumps infection. The patient was admitted and administered 600 mg intravenous methylprednisolone for 3 days, oral sodium valproate 500 mg, oral baclofen 5 mg three times a day, and tapering dose of oral prednisolone 150 mg for the next 4 weeks. Within 4 weeks, there was significant improvement in her symptoms, including a decrease in weakness, jerking movements, rigidity, and myoclonic seizures.
Mumps is an acute onset, self-limiting disease. Possible complications of mumps include aseptic meningitis, encephalitis, and ADEM.[1] ADEM is an immune-mediated neurological condition, characterized by inflammation and demyelination of the white matter in the central nervous system. There is an antecedent history of viral infection or vaccination.[2] Approximately, one-third of ADEM cases in children have no clear association to a prior infection.[2] Neurological findings of ADEM generally appear days to weeks following an infection or immunization, with an average latency of 4–13 days.[3] The brain and spinal MRI findings are useful for distinguishing ADEM from other demyelinating diseases, i.e., multiple sclerosis. The drug commonly used for the treatment of ADEM is high-dose intravenous corticosteroids and includes supportive and immune modulatory therapy.[3]
This complication remains underdiagnosed in patients who are unimmunized against mumps and therefore, it is important that the risk of ADEM is highlighted to physicians to prevent misdiagnoses in the future. The priority should be to first exclude infective causes of meningoencephalitis and then demyelinating processes such as multiple sclerosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I would like to thank Dr. Amit Mishra (Radiology, Apollo Chennai) for his support and help.
References
- 1.Choi KM. Reemergence of mumps. Korean J Pediatr. 2010;53:623–8. doi: 10.3345/kjp.2010.53.5.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huynh W, Cordato DJ, Kehdi E, Masters LT, Dedousis C. Post-vaccination encephalomyelitis: Literature review and illustrative case. J Clin Neurosci. 2008;15:1315–22. doi: 10.1016/j.jocn.2008.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torisu H, Kira R, Ishizaki Y, Sanefuji M, Yamaguchi Y, Yasumoto S, et al. Clinical study of childhood acute disseminated encephalomyelitis, multiple sclerosis, and acute transverse myelitis in Fukuoka Prefecture, Japan. Brain Dev. 2010;32:454–62. doi: 10.1016/j.braindev.2009.10.006. [DOI] [PubMed] [Google Scholar]


