Abstract
The class of immune response against autoantigens could profoundly influence the onset and/or outcome of autoimmune diseases. Until now, there is only limited information on the antigen-specific balance between proinflammatory and regulatory responses in humans. Here we analyzed the natural immune response against a candidate autoantigen in rheumatoid arthritis, human cartilage glycoprotein-39 (HC gp-39). Peripheral blood mononuclear cells from healthy individuals reacted against HC gp-39 with the production of IL-10 but not IFN-γ. Ex vivo assays indicated that the naturally occurring HC gp-39-specific immune response in bulk is powerful enough to suppress antigen-specific recall responses, demonstrating that rather than being unresponsive, the HC gp-39-directed immune response in healthy individuals shows a strong bias toward a regulatory phenotype. Moreover, CD4+ T cell lines directed against HC gp-39 expressed CD25, glucocorticoid-induced tumor necrosis factor receptor, and Foxp3 molecules and were capable of suppressing antigen-specific T cell responses. Cell–cell contact was required for this suppression. As opposed to healthy individuals, the HC gp-39-directed immune response in 50% of patients with rheumatoid arthritis exhibits polarization toward a proinflammatory T helper 1 phenotype and is significantly less powerful in suppressing antigen-specific recall responses. Together these findings indicate that the presence of HC gp-39-specific immune responses in healthy individuals may have an inhibitory effect on inflammatory responses in areas where HC gp-39 is present. Furthermore, these data indicate that the class of HC gp-39-directed immune response in rheumatoid arthritis patients has shifted from an antiinflammatory toward a proinflammatory phenotype.
Keywords: regulatory T cells, autoantigen
Rheumatoid arthritis (RA) is a chronic inflammatory disease with a variable disease outcome, which is characterized by an inflammatory process of unknown origin in multiple joints. Although the pathogenesis of RA is multifactorial, RA susceptibility and/or severity is strongly associated with the presence of isotype-switched autoantibodies and certain HLA class II alleles. These observations clearly point to a role for T cells in the pathological processes underlying RA. Therefore, much interest has focused on the phenotype of the T cell response that is present in the inflamed joints of RA patients. In general, these T cells display a typical T helper (Th)1-like phenotype (1). These T cells, either directly or indirectly, contribute to the proinflammatory cascades and inflammatory environment that is observed within the joints of RA patients (2). In contrast, other mechanisms are likely to be involved in the protection against autoimmunity such as the production of antiinflammatory cytokines such as IL-10 and TGF-β. In this respect, a population of naturally occurring T cells, T regulatory (Treg) cells, have regained much interest in the last decade. These cells display antiinflammatory and antiproliferative functions. In several animal model systems, it has been shown that Treg cells play a critical role in the generation and maintenance of tolerance and generally inhibit immune responses that are potentially deleterious to the host (3). Several T cell subsets have been described that mediate these protective immunoregulatory effects, of which the most extensively studied T cell subset is characterized by the expression of CD4 and CD25 in both mice and humans (4–6).
Investigations into the role of Treg cells have been difficult because no specific marker for Treg cells has been identified so far. The expression of CD25, cytotoxic T lymphocyte antigen-4, the tumor necrosis factor (TNF) family molecule glucocorticoid-induced TNF receptor (GITR), and Foxp3 have been used to identify Treg cells but, in general, Treg cells are characterized on the basis of a functional definition through their ability to down-regulate other immune responses (7, 8).
In vitro studies indicate that T cell receptor triggering by, for example, anti-CD3 is required for Treg cell function (3, 9), indicating that antigen recognition most likely represents the natural trigger initiating Treg cell activity. However, there is only limited evidence for autoantigen-specific regulatory T cell populations in humans. Nonetheless, knowledge on the autoantigens capable of inducing regulatory circuits in humans is important because this knowledge can be used for the design of rationally defined vaccines that prevent and/or inhibit autoimmune diseases. Studying the question whether a certain antigen can induce regulatory circuits in humans has been proven difficult because of various technical aspects related to low precursor frequencies and the inherent difficulty of expanding cells with a regulatory phenotype in vitro. Moreover, the choice of the antigenic stimulus is particularly important and, in case a certain antigen is selected for further studies, high purity to avoid immune activation by contaminants, such as lipopolysaccharide, within the antigen preparation is essential.
Here, we have studied the natural immune responses against human cartilage glycoprotein-39 (HC gp-39), a candidate autoantigen in RA. HC gp-39 is a major constituent of human cartilage and is overexpressed in synovial specimens and cartilage from RA patients (10). It has been shown that HC gp-39 is efficiently processed and presented in the context of MHC class II molecules by dendritic cells (DCs) and macrophages (11, 12). HC gp-39 can also serve as a target for T cells, because HC gp-39-specific MHC class-II-restricted T cell responses can readily be induced in HLA-DR4-transgenic mice (13). Moreover, proliferative responses have been described in RA patients, indicating that HC gp-39-directed T cells are present also in humans (13–15). Interestingly, intranasal treatment with HC gp-39 suppressed murine collagen-induced arthritis (16). These observations indicate that HC gp-39 can activate/boost regulatory circuits that interfere with arthritis in case the antigen is presented in an environment that is adapted to induce tolerogenic responses to innocuous antigens. Moreover, they indicate that HC gp-39-directed T cells can escape thymic deletion and that HC gp-39-specific T cells are present in the natural T cell repertoire. Together, these observations identify HC gp-39 as an interesting human autoantigen and have led us to hypothesize that HC gp-39 is driving regulatory responses in humans. Therefore, the aim of this work was to determine whether HC gp-39 could stimulate regulatory or suppressive immune responses in healthy individuals and whether the bias of HC gp-39-directed immunity is altered in RA patients.
Materials and Methods
Blood Samples and HLA-DR Typing. After informed consent, citrated or heparinized venous blood was collected from healthy blood bank donors and RA patients classified as having definite RA according to the 1987 American College of Rheumatology criteria for RA (17). The characteristics of the RA patients are summarized in Table 1. Peripheral blood mononuclear cells (PBMCs) were isolated and used directly or were cryopreserved in liquid nitrogen. HLA-DR typing was performed on genomic DNA by using the sequence specific oligonucleotide (PCR-SSO) as described in refs. 18 and 19. In this study, DRB1*04-positive donors were selected for further analysis.
Table 1. Characteristics of RA patients.
| No. of patients tested | 43 |
| Age, years | 53.7 ± 13.9 (24.0-78.5)* |
| Male/female | 15/28 |
| HLA-DR4 | 43/43 |
| Disease duration, years | 6.8 ± 1.8 (3.3-9.7)* |
| Erosive disease | 34/43 (81.0%) |
| RF positive | 33/43 (76.7%) |
| DMARD treatment | 40/43 (93.0%) |
| More than one DMARD in use | 11/43 (25.6%) |
| More than one DMARD used in past | 30/43 (69.8%) |
| Methotrexate treatment | 23/43 (53.5%) |
| Prednisolone treatment | 3/43 (7.0%) |
RF, rheumatoid factor-IgM (RF positive if ≥5 units); DMARD, disease-modifying antirheumatic drug.
Expressed as mean ± SD (range, in parentheses).
Antigens. Clinical-grade human recombinant HC gp-39 (Org 39141; 10 μg/ml final conc.) was kindly provided by N.V. Organon, Oss, The Netherlands. The recall-response antigen mix consisted of a mixture of tetanus toxoid (T.tox) (0.75 limit of flocculation unit/ml final conc.; National Institute of Public Health and the Environment, Bilthoven, The Netherlands), purified protein derivative (PPD) from Mycobacterium tuberculosis (5 μg/ml final conc.; Statens Serum Institute Copenhagen), and Candida albicans (0.005%, HAL Allergenen Lab, Haarlem, The Netherlands).
Keyhole limpet hemocyanin (KLH; 10 μg/ml final conc.) was obtained from Pierce Biotechnology. Phytohaemagglutinin (PHA HA16; 2 μg/ml final conc.) was obtained from Remel (Lenexa, KS). Clinical-grade human insulin (Actrapid; 10 μg/ml final conc.) was obtained from Novo Nordisk, Bagsvaerd, Denmark. The preferentially expressed antigen of melanoma (PRAME)-derived peptide PRA142–151 (SLYSFPEPEA; 5 ng/ml final conc.) was synthesized by solid-phase strategies on an automated multiple peptide synthesizer (Abimed AMS 422, Langenfeld, Germany) and subsequently stored at –20°C until usage.
Cytokine Elispot Analysis. PBMCs were stimulated with antigen in culture medium supplemented with 10% FCS for 4 days in 24-well plates. Thereafter, the cells were seeded in 4 replicate wells at a density of 105 cells per well (IFN-γ) or 1.5 × 105 cells per well (IL-10) of a MultiScreen 96-well plate (Millipore), coated with IFN-γ or IL-10 catching antibody (MABTECH, Natcha, Sweden). After overnight incubation at 37°C, the plates were developed according to the manufacturer's procedures. The number of visible spots was counted in a BioReader 3000 (BioSys, Karben, Germany). To examine the nature of the responder cells, PBMCs were cultured as described above or depleted of CD3+ T cells (>97% pure). The CD3-negative fraction was seeded at a density of 5 × 104 cells per well. For statistical analysis of differences between cocultures in the inhibition assays, Student's t test was used. Differences in IFN-γ production between healthy donors and RA patients were analyzed by the Mann–Whitney U test.
Detection of Antigen-Specific IL-10-Secreting Cells. Fresh PBMCs were stimulated with antigen in culture medium supplemented with 10% autologous or AB-serum for 4 days in 24-well plates. Thereafter, the cells were labeled with anti-IL-10 antibody (Miltenyi Biotec, Amsterdam) and subsequently seeded overnight in six-well plates. Next, the IL-10 secreting cells were stained according to the manufacturer's procedures and analyzed on a FACSCalibur (Becton Dickinson). Isotype-matched mouse IgG1-phycoerythrin-conjugated control mAb (clone X40) was obtained from Becton Dickinson.
Generation of T Cell Lines. PBMCs were stimulated in vitro (2 × 106 per ml) with PPD (5 μg/ml), T.tox. (0.75 limit of flocculation unit/ml) or HC gp-39 (10 μg/ml). After 4–5 days, cells were expanded for 11–13 days in culture medium supplemented with 10% FCS and recombinant human IL-2 (rhIL-2; 25 units/ml; Chiron) alone [T cell line raised against PPD from Mycobacterium tuberculosis (TPPD)/T cell line raised against T.tox. (TT.tox)] or rhIL-2 combined with rhIL-15 (10 units/ml; TEBU BIO Peprotech, Heerhugowaard, The Netherlands) for the T cell line raised against HC gp-39 (THCgp-39).
Proliferation Assays. Proliferation of T cell lines was measured in 96-well plates in 4–6 replicate cultures. To analyze putative toxic properties of HC gp-39, 2.5 × 103 cells from TPPD or TT.tox were incubated per well together with PPD or T.tox and 5 × 103 irradiated (3,000 rad) autologous PBMCs as antigen-presenting cells (APCs) with or without HC gp-39. No inhibition of proliferation was detected in TPPD or TT.tox, indicating that HC gp-39 was nontoxic. For the inhibition assays, each well contained 104 TPPD cells, 104 autologous THCgp-39 cells, 2 × 104 irradiated autologous PBMCs as APCs, and antigen. Control antigen clinical grade insulin (Actrapid) was heat pretreated to disrupt 3D structures and prevent putative cell interactions. After 4 days of culturing, proliferation was determined by overnight incorporation of [3H]thymidine. For statistical analysis the two-tailed Student's t test for unpaired samples was used.
Carboxyfluorescein Diacetate Succinimidyl Ester (CFSE)-Labeled Cell Division Analysis. TPPD or TT.tox were labeled with 0.5 μM CFSE (Molecular Probes). The CFSE-labeled cells (5 × 105) were incubated with 106 irradiated PBMCs as APCs, antigen, and with or without 5 × 105 unlabeled cells from an autologous THCgp-39. After 3 days, the CFSE content of the TPPD was analyzed on a FACSCalibur. To quantify the absolute number of divided CFSE-labeled cells and to correct for apoptotic or dead CFSE-labeled cells, the number of analyzed cells was standardized by the addition of 15 × 103 Flow-Count fluorospheres per sample (Beckman Coulter). Acquisition was stopped when 3 × 103 beads were counted.
In the transwell experiments, THCgp-39 (5 × 105) or control cell line TT.tox were cultured in the inner wells (24-well plate) in medium containing 5 × 105 irradiated PBMCs as APCs with or without HC gp-39 protein. Equal numbers of CFSE-labeled TPPD cells and APCs were added into the outer wells in the same medium with or without PPD. After 4 days of culture, the CFSE content of the TPPD was analyzed on a FACSCalibur.
Recall Suppression Assays. PBMCs were incubated with or without HC gp-39 in a 24-well plate. After 3–5 h, the cultures were supplemented with a recall-response antigen mix (see above). After 4 days of culturing, the overnight IFN-γ excretion of the culture was analyzed by elispot (see above). Differences in the HC gp-39-induced changes in IFN-γ excretion between healthy donors and RA patients were analyzed by the Mann–Whitney U test.
Cytotoxic T Lymphocyte (CTL) Inhibition Assays. An HLA-A2-restricted CTL clone directed against a tumor-associated antigen PRAME-derived peptide was a kind gift from J. Kessler (Leiden University Medical Center). The isolation, maintenance, and properties of the CTL clone are described in ref. 20. During stimulation with the PRAME peptide, this CTL clone produces high amounts of IFN-γ. For inhibition assays, PBMCs from an HLA-A2-positive donor known to secrete IL-10 after incubation with HC gp-39 were incubated with or without HC gp-39 protein. After 48 h, the PRAME peptide together with 30,000 A2-restricted PRAME-specific CTLs was added. The overnight IFN-γ excretion of the coculture was analyzed by elispot (see above).
Results
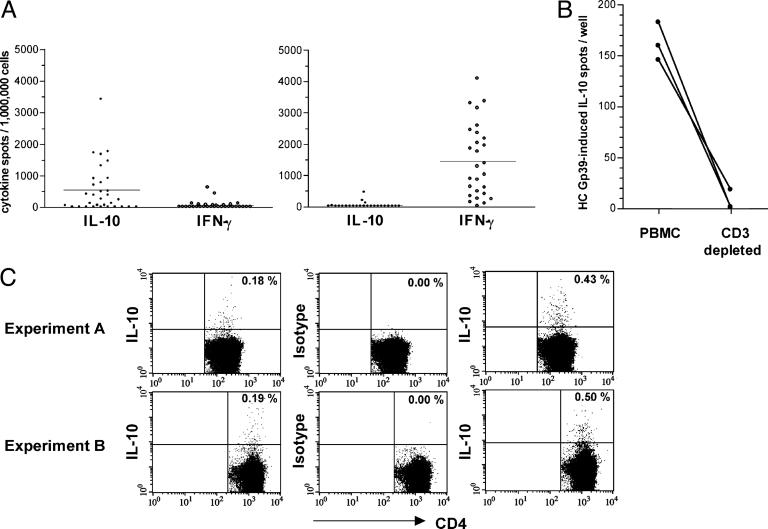
HC gp-39-Specific Immune Reactivity Is Characterized by IL-10 Production. Because various observations indicate the presence of HC gp-39-directed T cells in the human T cell repertoire, combined with the finding that presentation of HC gp-39 in a noninflammatory/tolerogenic environment can induce regulatory circuits (16), we wished to evaluate the natural HC gp-39-directed immune response in healthy individuals. As elispot analyses allow the detection of low precursor frequencies with preservation of the class of immune responsiveness (e.g., as measured by IFN-γ or IL-10 production), we used elispot analyses after a short, 4-day culture of PBMCs with antigens. Our data show that the PBMCs from 17 of 31 healthy donors analyzed reacted against HC gp-39 with the production of IL-10 without the concomitant production of IFN-γ (Fig. 1A Left). This response is specific for HC gp-39 because responses toward a mix of typical Th1-associated recall antigens are dominated by IFN-γ production (Fig. 1A Right). Importantly, HC gp-39 was not toxic to the cells, because relatively high doses of HC gp-39 did not suppress the proliferative capacity of defined T cell lines (data not shown). No IL-10 responses could be detected anymore after depletion of CD3+ cells from the PBMC cultures stimulated with HC gp-39 (Fig. 1B). In contrast, IL-10 responses remained in CD3-depleted cultures stimulated with phytohemag-glutinin. Together, these findings indicate that T cells or CD3+ natural killer cells are responsible for the IL-10 production after stimulation of PBMCs with HC gp-39. To further validate the source of IL-10 production after HC gp-39-stimulation, we investigated whether CD4+ cells produce IL-10 in response to HC gp-39 by flow cytometry. Although we were not able to detect IL-10 production toward HC gp-39 in most donors by this technique (presumably as a result of a lower sensitivity of this assay compared with elispot analyses), we reproducibly detected CD4+ IL-10+ cells in a donor harboring a high frequency of cells reacting against HC gp-39. As shown in Fig. 1C, IL-10 was produced by 0.4–0.5% of CD4+ cells (Right), whereas unstimulated PBMCs produced only background amounts of IL-10 (0.2%) (Left). Together, these results indicate that the natural immune response against HC gp-39 in healthy donors is hallmarked by the production of IL-10 mediated by HC gp-39-directed T cells.
Fig. 1.
HC gp-39-specific immune reactivity in healthy donors. (A) PBMCs from healthy donors (n = 31) react against HC gp-39 by production of IL-10 but not IFN-γ (Left). Responses induced by “control” recall antigens are dominated by IFN-γ production (Right). (B) HC gp-39-induced IL-10 responses are mediated by T cells. Shown in an analysis of PBMCs from three different donors for IL-10 responses to HC gp-39, in which HC gp-39 was cultured with unmanipulated PBMCs or PBMCs immunomagnetically depleted of CD3+ T cells before elispot analysis. Background responses (medium alone) were subtracted from HC gp-39 responses. (C) CD4+ T cells respond to HC gp-39 with the production of IL-10. Unstimulated CD4+ T cells (Left) produce background amounts of IL-10 (0.2%), whereas IL-10 was produced by 0.4–0.5% of HC gp-39-stimulated CD4+ T cells (Right). As a control, HC gp-39-stimulated CD4+ T cells (Center) were stained with an isotype-matched control mAb (0.0% staining).
Phenotypic and Immunological Characterization of CD4+ T Cell Lines Against HC gp-39. The observation that CD3+ T cells produce IL-10 and not IFN-γ on exposure to HC gp-39 prompted us to investigate whether HC gp-39-responsive T cells represent T cells with immunoregulatory properties. For this purpose, we generated T cell lines against HC gp-39 (THCgp-39). THCgp-39 were expanded by HC gp-39-specific stimulation in the presence of IL-2 and IL-15 (21, 22) and subsequently analyzed for the presence of various markers that are associated with CD4+ Treg cells. Phenotypic analyses of the generated THCgp-39 showed that THCgp-39 were CD4+ expressing high levels of CD25 and glucocorticoid-induced tumor necrosis factor receptor that produced increased levels of IL-10, tumor necrosis factor α, and IFN-γ on stimulation with HC gp-39 (data not shown). Moreover, real-time PCR revealed that the THCgp-39 also expressed relatively high levels of Foxp3, a transcription factor highly expressed in CD4+ CD25+ Treg cells (23, 24). Control Th1 cell lines against PPD and T.tox. that were derived from the same donors displayed similar markers, although the level of expression was often considerably lower (data not shown). These results indicate that the phenotype of the T cell lines against HC gp-39 is compatible with the molecular makeup typically found on naturally occurring CD4+ CD25+ Treg cells.
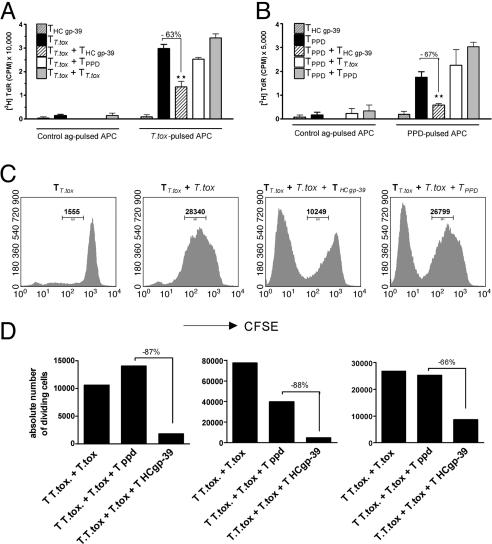
Nonetheless, more definitive evidence of CD4+ Treg cells resides in the demonstration that these cell lines can inhibit proliferation of conventional CD4+ T cells in functional assays. Therefore, we set out to determine the regulatory capacities of HC gp-39-directed T cells in suppression assays. To this end, THCgp-39 cells were titrated into cultures consisting of TPPD or TT.tox. The proliferative responses of T.tox-activated TT.tox cell lines (Fig. 2A) and PPD-activated TPPD cell lines (Fig. 2B) were suppressed (P < 0.01) by the addition of THCgp-39 by up to 67%. In contrast, addition of T.tox-directed T cells to PPD-directed T cells and vice versa did not result in inhibition of proliferation, indicating that the suppression observed after adding THCgp-39 was not because of competition for space or nutrients at high cell concentrations. Moreover, inhibition required the presence of THCgp-39 cells because APCs pulsed with the HC gp-39 protein were not able to mediate suppression (data not shown). HC gp-39-directed T cell lines did not display detectable proliferative responses toward HC gp-39 (data not shown), which is in line with their regulatory phenotype. Together, these findings indicate that HC gp-39 by itself is not able to polarize the APCs into a “regulatory” APC and, more importantly, indicate that HC gp-39-directed T cell lines display regulatory functions.
Fig. 2.
CD4+ T cell lines raised against HC gp-39 (THCgp-39) are suppressive. (A and B) THCgp-39 suppresses proliferation of autologous T cell lines specific for recall antigens, TT.tox (A) and TPPD (B). Background responses (unstimulated TT.tox and TPPD) were subtracted from stimulated TT.tox and TPPD. **, P < 0.01. (C) THCgp-39 can inhibit cell division of autologous CFSE-labeled TT.tox.TT.tox (Far Left) was incubated with T.tox-pulsed APCs alone (Center Left) or together with THCgp-39 (Center Right) or TPPD (Far Right). The absolute number of dividing cells is indicated in each histogram. Similar results were obtained in four donors. (D) THCgp-39 can inhibit proliferation of autologous TT.tox and TPPD. T cell lines directed against T.tox, PPD, and HC gp-39 were generated from three different donors (Left, Center, and Right). Although some suppression of TT.tox proliferation was sometimes observed after addition of TPPD (center bar in Center), a pronounced suppressive activity is displayed by THCgp-39. These data are representative of nine donors analyzed. Similar data were obtained when TPPD was used as a readout, adding TT.tox and THCgp-39 as suppressors (data not shown). Background responses (unstimulated TT.tox and TPPD) were subtracted from T.tox and PPD-stimulated TT.tox and TPPD, respectively.
The suppressive capacity of HC gp-39-directed T cell lines was confirmed in a read-out system where CFSE-labeled T.tox or PPD-directed T cell lines were cocultured with autologous HC gp-39-directed T cells. In this manner, the inhibition of proliferation of antigen-specific T cell lines can be monitored directly in a quantitative manner. Fig. 2C shows that addition of THCgp-39 results in the inhibition of TT.tox cell division by 62% (from 28 × 103 to 10 × 103 divided cells), whereas no such inhibition was observed by adding the “crowding” control TPPD. In Fig. 2D, the results of three independent experiments are shown employing T cell lines obtained from three different donors. Although we also observed inhibition of the proliferative response after addition of an irrelevant control cell line in one of three cases, the addition of THCgp-39 resulted in a considerably stronger inhibition.
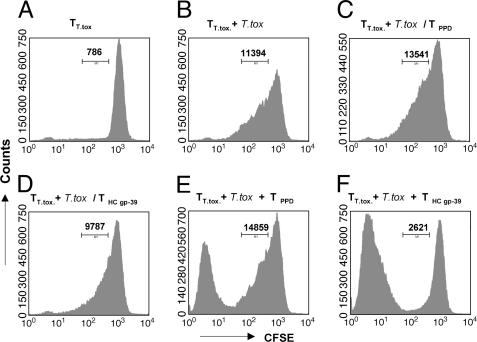
The observation that THCgp-39 displays a regulatory phenotype led us to investigate whether cell–cell contact was required for HC gp-39-directed T cell lines to inhibit other CD4+ effector T cells. The suppressive action of THCgp-39 on CFSE-labeled cell division was abrogated when cell–cell contact between THCgp-39 and CFSE-labeled TT.tox or TPPD was prevented in transwell assays (Fig. 3 A–D). As the control, a simultaneously performed coculture assay was performed in which strong suppression of the proliferative activity of CSFE-labeled T.tox- or PPD-directed T cell lines was observed (Fig. 3 E and F), indicating that the THCgp-39 cells were viable and immunosuppressive. Together these results indicate that THCgp-39 cells are able to mediate suppression in a cell–cell contact-dependent fashion.
Fig. 3.
Cell–cell contact is required for the immunosuppressive activity of CD4+ T cell lines directed against HC gp-39. The absolute number of dividing CFSE-labeled TT.tox cells is indicated in each histogram. (A) Unstimulated TT.tox in outer wells (B) TT.tox stimulated with T.tox-pulsed APCs in outer wells. (C) TT.tox stimulated with T.tox-pulsed APCs in outer wells and TPPD in inner wells. (D) TT.tox stimulated with T.tox-pulsed APCs in outer wells and THCgp-39 in inner wells. (E) TT.tox stimulated with T.tox-pulsed APCs and TPPD together in outer wells. (F) TT.tox stimulated with T.tox-pulsed APCs and THCgp-39 together in outer wells.
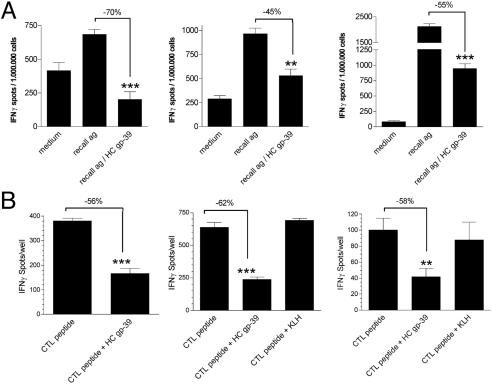
Ex Vivo HC gp-39-Directed Immune Responses Can Suppress Recall Responses and CD8+ T Cell Activity. As described above, our in vitro assays indicate that THCgp-39, once activated, down-regulate other immune responses in a cell–cell contact-dependent manner. To address the question of whether the HC gp-39-reactive immune response directly after cells are taken from the donors is efficient enough to suppress other immune responses, donors that displayed IL-10 responses after stimulation with HC gp-39 were selected for further study. PBMCs from these donors were stimulated with a 10× diluted mixture of recall antigens to induce intermediate recall antigen-specific IFN-γ responses as measured by elispot analyses. To study whether stimulation by HC gp-39 can suppress this IFN-γ production, we triggered the PBMCs simultaneously with HC gp-39 to activate regulatory cells and the recall antigen mixture to activate recall antigen-specific memory cells. HC gp-39 could stimulate regulatory circuits as observed by a marked inhibition of the recall response (Fig. 4A).
Fig. 4.
Ex vivo HC gp-39-directed immune responses can suppress other immune responses. (A) HC gp-39-activated PBMCs are able to suppress IFN-γ responses to recall antigens in three different healthy donors. (B) HC gp-39-stimulated HLA-A2+ PBMCs from three different healthy donors are capable of suppressing IFN-γ production of activated HLA-A2+ CTLs. **, P < 0.005; ***, P < 0.0005.
Next, we determined whether HC gp-39 stimulation could also inhibit CD8+ T cell responsiveness. Therefore, an HLA-A2-restricted CTL clone directed against a peptide derived from the tumor antigen PRAME was used. PBMCs from HLA-A2+ donors were stimulated with HC gp-39 and, after 48 h, loaded with the PRAME peptide. Subsequently, the PRAME-specific CTL clone was added, and IFN-γ production was measured by elispot analyses. HC gp-39-stimulated HLA-A2+ PBMCs were able to suppress IFN-γ production of activated PRAME-specific CTL as shown in Fig. 4B. Together these data indicate that the “naturally” occurring HC gp-39-reactive immune response is highly effective in suppressing other immune responses.
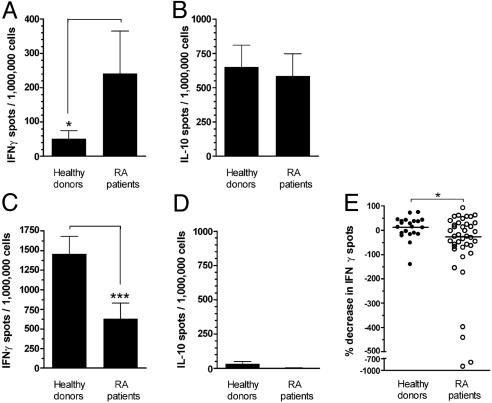
The HC gp-39-Directed Immune Response in RA Patients Is Biased Toward a Proinflammatory Response. Intrigued by the antiinflammatory properties of HC gp-39-directed immune responses in healthy donors, we postulated that the immune response in RA patients might have shifted toward a proinflammatory response. Therefore, the immune response in RA patients was evaluated by employing IFN-γ and IL-10 elispots. In contrast to healthy donors, which produce primarily IL-10 (Figs. 1 A and 5 A and B), RA patients produce considerable amounts of IFN-γ (P < 0.05; i.e., 17 of 34 patients analyzed produced IFN-γ). These findings could not be attributed to a generalized increase in IFN-γ production in RA patients because the recall antigen-specific immune reactivity is diminished in RA patients compared with controls (Fig. 5 C and D). Next we compared PBMC cultures from RA patients (n = 40) with the ability of PBMC cultures from healthy donors (n = 21) to reduce recall antigen responses after costimulation with HC gp-39. It was found that HC gp-39 was less effective in stimulating regulatory response in PBMC cultures from RA patients compared with cultures from healthy controls (Fig. 5E) because the majority of PBMC cultures from RA patients gave rise to more IFN-γ spots after costimulation with HC gp-39. In some patients, this increase was even 4-fold or higher. Together these data imply that a disease-associated bias is displayed by the HC gp-39-directed immune response.
Fig. 5.
IFN-γ and IL-10 responses to HC gp-39 and recall antigens by PBMCs from healthy donors (n = 31) and RA patients (n = 34) as determined by elispot. (A and B) Healthy donors produce primarily IL-10 but not IFN-γ, whereas RA patients produce both IL-10 and considerable amounts of IFN-γ in response to HC gp-39 (*, P < 0.05). (C and D) Recall antigen-directed reactivity is characterized by IFN-γ production but not IL-10 production in both RA patients and healthy donors. Moreover, PBMCs from healthy donors produce more IFN-γ after exposure to recall antigens as compared with RA patients (***, P < 0.001). (E) HC gp-39-stimulated PBMCs from healthy donors (n = 21; unbiased for HC gp-39-induced IL-10 production) are better suppressors of recall antigen-induced IFN-γ production than HC gp-39-stimulated PBMCs from RA patients (n = 40). *, P < 0.03. Line represents the median in percent decrease per group.
These findings indicate that HC gp-39 serves as an autoantigen in both healthy donors and RA patients. However, despite a reduced Th1 response against recall antigens, the HC gp-39-directed immune responsiveness in RA patients is shifted toward a proinflammatory phenotype in a substantial number of RA patients as more IFN-γ is produced and is paralleled by a reduced suppression of recall responses.
Discussion
In the present study, we demonstrated a clear discrepancy in immune reactivity between healthy donors and RA patients against the naturally occurring autoantigen HC gp-39. IFN-γ production by PBMC cultures from the majority of healthy donors that were stimulated by recall antigens could be inhibited by costimulation by HC gp-39. In contrast, the majority of such cultures from RA patients displayed an increase in IFN-γ-producing cells. Moreover, in contrast to HC gp-39-activated cells from RA patients that also produced IFN-γ, the HC gp-39-directed immune response of healthy individuals was hallmarked by the production of IL-10. IL-10 production depended on CD3-expressing cells, and CD4+ T cell lines against HC gp-39 displayed regulatory capacities.
These findings clearly indicate that healthy individuals, rather than being nonresponsive, frequently react to HC gp-39 with the production of IL-10. Our data can best be explained by the presence of HC gp-39-directed Treg cells in healthy subjects because these cells have the potential to effectively suppress various proliferative and inflammatory responses.
The observations that the immune response of a considerable number of RA patients displays a proinflammatory polarization toward HC gp-39 and is less capable of inhibiting other immune responses are intriguing. Although some caution is required in interpreting these results because the lack of detecting suppression does not necessarily indicate the absence of suppressive responses, these data suggest that the inflammatory processes accompanying RA development/progression favor the induction of HC gp-39-directed Th1 cells. To become activated, naïve T cells have to encounter their specific antigens presented by HLA molecules on DCs. Although this event alone causes naïve T cell division, it does not necessarily establish a productive immune response because full mobilization to effector cells crucially depends on proper maturation of DCs (25). It is plausible that the inflammatory environment observed in the joints of RA patients meets the requirements for proper maturation of local DCs, enabling the induction of Th1 cell responses. Moreover, it has been reported that DCs present in the synovial tissue are able to present HC gp-39-derived peptides in the context of HLA class II molecules (11, 12). Therefore, we hypothesize that the emergence of IFN-γ-producing HC gp-39 directed T cells in RA patients is the result of HC gp-39 presentation by maturated DCs that have the capacity to activate Th1 cells as a consequence of the maturation signals present in the inflamed synovium. In this way, the HC gp-39-specific Th1 cells are a result, rather than a cause, of the disease and could also be present in other (rheumatic) diseases.
The observation that a disease-associated bias is present with respect to the class of HC gp-39-directed immune response might point toward a more generalized phenomenon because it has recently been shown also that in diabetes and multiple sclerosis the autoreactive T cell response is polarized toward a proinflammatory Th1 phenotype, whereas a regulatory response is observed in health (26, 27). Although these observations have been made in different diseases, together these findings clearly indicate that induction of autoimmunity not only requires the emergence of pathogenic T cells (Th1 and/or Th2 cells) but also is associated with the loss of Treg cell function that normally protects against autoimmunity. These findings are highly relevant for the development of antigen-specific intervention protocols because they suggest an approach for controlling immune responses. Particularly, RA might represent an autoimmune disease that is especially suited for targeting Treg cells because, due to its systemic nature, a systemic approach is required to dampen the inflammatory reaction. It is likely that Treg cells will focus on areas of inflammation, such as the inflamed joint, because they carry several receptors for inflammatory chemokines (5, 28–30). Indeed, the presence of Treg cells in the inflamed joint, in addition to activated potentially pathogenic T cells, was recently demonstrated in synovial fluid of RA patients (31). Moreover, we have shown that CD4+ CD25+ Treg cells are also involved in collagen-induced arthritis because depletion of CD4+ CD25+ T cells significantly increased severity and incidence of the disease, whereas reconstitution studies showed that infusion of CD4+ CD25+ Treg cells conferred disease protection (32). The challenge for the future will be to induce and/or expand residual antigen-specific Treg cell activity to treat autoimmune diseases in an antigen-specific manner.
Acknowledgments
This work was supported by The Dutch Arthritis Association. R.E.M.T. is supported by a Vidi Grant from the Netherlands Organization for Scientific Research. H.v.D. is supported by The Netherlands Organization for Health Research and Development.
Author contributions: J.H.M.v.B., H.v.D., T.W.J.H., R.R.P.d.V., and R.E.M.T. designed research; J.H.M.v.B., H.v.D., L.R.L., E.I.H.v.d.V., D.G.E., and A.M.B. performed research; A.M.M.M. contributed new reagents/analytic tools; J.H.M.v.B., H.v.D., L.R.L., E.I.H.v.d.V., D.G.E., and A.M.B. analyzed data; and J.H.M.v.B. and R.E.M.T. wrote the paper.
Abbreviations: APC, antigen-presenting cell; CFSE, carboxyfluorescein diacetate succinimidyl ester; CTL, cytotoxic T lymphocyte; DC, dendritic cell; HC gp-39, human cartilage glycoprotein-39; PBMC, peripheral blood mononuclear cell; PPD, purified protein derivative; PRAME, preferentially expressed antigen in melanoma; RA, rheumatoid arthritis; Th, T helper; Treg cell, regulatory T cell; THCgp-39, T cell line raised against HC gp-39; TPPD, T cell line raised against PPD from Mycobacterium tuberculosis; T.tox, tetanus toxoid; TT.tox, T cell line raised against T.tox.
References
- 1.Dolhain, R. J., van der Heiden, A. N., ter Haar, N. T., Breedveld, F. C. & Miltenburg, A. M. (1996) Arthritis Rheum. 39, 1961–1969. [DOI] [PubMed] [Google Scholar]
- 2.Choy, E. H. & Panayi, G. S. (2001) N. Engl. J. Med. 344, 907–916. [DOI] [PubMed] [Google Scholar]
- 3.Shevach, E. M. (2000) Annu. Rev. Immunol. 18, 423–449. [DOI] [PubMed] [Google Scholar]
- 4.Asano, M., Toda, M., Sakaguchi, N. & Sakaguchi, S. (1996) J. Exp. Med. 184, 387–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sakaguchi, S., Sakaguchi, N., Asano, M., Itoh, M. & Toda, M. (1995) J. Immunol. 155, 1151–1164. [PubMed] [Google Scholar]
- 6.Thornton, A. M. & Shevach, E. M. (1998) J. Exp. Med. 188, 287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakaguchi, S., Sakaguchi, N., Shimizu, J., Yamazaki, S., Sakihama, T., Itoh, M., Kuniyasu, Y., Nomura, T., Toda, M. & Takahashi, T. (2001) Immunol. Rev. 182, 18–32. [DOI] [PubMed] [Google Scholar]
- 8.Wood, K. J. & Sakaguchi, S. (2003) Nat. Rev. Immunol. 3, 199–210. [DOI] [PubMed] [Google Scholar]
- 9.Thornton, A. M. & Shevach, E. M. (2000) J. Immunol. 164, 183–190. [DOI] [PubMed] [Google Scholar]
- 10.Hakala, B. E., White, C. & Recklies, A. D. (1993) J. Biol. Chem. 268, 25803–25810. [PubMed] [Google Scholar]
- 11.Tsark, E. C., Wang, W., Teng, Y. C., Arkfeld, D., Dodge, G. R. & Kovats, S. (2002) J. Immunol. 169, 6625–6633. [DOI] [PubMed] [Google Scholar]
- 12.Baeten, D., Steenbakkers, P. G., Rijnders, A. M., Boots, A. M., Veys, E. M. & De Keyser, F. (2004) Arthritis Rheum. 50, 444–451. [DOI] [PubMed] [Google Scholar]
- 13.Cope, A. P., Patel, S. D., Hall, F., Congia, M., Hubers, H. A., Verheijden, G. F., Boots, A. M., Menon, R., Trucco, M., Rijnders, A. W., et al. (1999) Arthritis Rheum. 42, 1497–1507. [DOI] [PubMed] [Google Scholar]
- 14.Vos, K., Miltenburg, A. M., van Meijgaarden, K. E., van den Heuvel, M., Elferink, D. G., van Galen, P. J., van Hogezand, R. A., Vliet-Daskalopoulou, E., Ottenhoff, T. H., Breedveld, F. C., et al. (2000) Rheumatology (Oxford) 39, 1326–1331. [DOI] [PubMed] [Google Scholar]
- 15.Verheijden, G. F., Rijnders, A. W., Bos, E., Coenen-de Roo, C. J., van Staveren, C. J., Miltenburg, A. M., Meijerink, J. H., Elewaut, D., De Keyser, F., Veys, E., et al. (1997) Arthritis Rheum. 40, 1115–1125. [DOI] [PubMed] [Google Scholar]
- 16.Joosten, L. A., Coenen-de Roo, C. J., Helsen, M. M., Lubberts, E., Boots, A. M., van den Berg, W. B. & Miltenburg, A. M. (2000) Arthritis Rheum. 43, 645–655. [DOI] [PubMed] [Google Scholar]
- 17.Arnett, F. C., Edworthy, S. M., Bloch, D. A., McShane, D. J., Fries, J. F., Cooper, N. S., Healey, L. A., Kaplan, S. R., Liang, M. H., Luthra, H. S., et al. (1988) Arthritis Rheum. 31, 315–324. [DOI] [PubMed] [Google Scholar]
- 18.Verduyn, W., Doxiadis, I. I., Anholts, J., Drabbels, J. J., Naipal, A., D'Amaro, J., Persijn, G. G., Giphart, M. J. & Schreuder, G. M. (1993) Hum. Immunol. 37, 59–67. [DOI] [PubMed] [Google Scholar]
- 19.Faas, S. J., Menon, R., Braun, E. R., Rudert, W. A. & Trucco, M. (1996) Tissue Antigens 48, 97–112. [DOI] [PubMed] [Google Scholar]
- 20.Kessler, J. H., Beekman, N. J., Bres-Vloemans, S. A., Verdijk, P., van Veelen, P. A., Kloosterman-Joosten, A. M., Vissers, D. C., ten Bosch, G. J., Kester, M. G., Sijts, A., et al. (2001) J. Exp. Med. 193, 73–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koenen, H. J., Fasse, E. & Joosten, I. (2003) J. Immunol. 171, 6431–6441. [DOI] [PubMed] [Google Scholar]
- 22.Bacchetta, R., Sartirana, C., Levings, M. K., Bordignon, C., Narula, S. & Roncarolo, M. G. (2002) Eur. J. Immunol. 32, 2237–2245. [DOI] [PubMed] [Google Scholar]
- 23.Hori, S., Nomura, T. & Sakaguchi, S. (2003) Science 299, 1057–1061.12522256 [Google Scholar]
- 24.Ramsdell, F. (2003) Immunity 19, 165–168. [DOI] [PubMed] [Google Scholar]
- 25.Sotomayor, E. M., Borrello, I., Tubb, E., Rattis, F. M., Bien, H., Lu, Z., Fein, S., Schoenberger, S. & Levitsky, H. I. (1999) Nat. Med. 5, 780–787. [DOI] [PubMed] [Google Scholar]
- 26.Arif, S., Tree, T. I., Astill, T. P., Tremble, J. M., Bishop, A. J., Dayan, C. M., Roep, B. O. & Peakman, M. (2004) J. Clin. Invest. 113, 451–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Viglietta, V., Baecher-Allan, C., Weiner, H. L. & Hafler, D. A. (2004) J. Exp. Med. 199, 971–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huehn, J., Siegmund, K., Lehmann, J. C., Siewert, C., Haubold, U., Feuerer, M., Debes, G. F., Lauber, J., Frey, O., Przybylski, G. K., et al. (2004) J. Exp. Med. 199, 303–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Annunziato, F., Cosmi, L., Liotta, F., Lazzeri, E., Manetti, R., Vanini, V., Romagnani, P., Maggi, E. & Romagnani, S. (2002) J. Exp. Med. 196, 379–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Belkaid, Y., Piccirillo, C. A., Mendez, S., Shevach, E. M. & Sacks, D. L. (2002) Nature 420, 502–507. [DOI] [PubMed] [Google Scholar]
- 31.Cao, D., Malmström, V., Baecher-Allan, C., Hafler, D., Klareskog, L. & Trollmo, C. (2003) Eur. J. Immunol. 33, 215–223. [DOI] [PubMed] [Google Scholar]
- 32.Morgan, M. E., Sutmuller, R. P., Witteveen, H. J., van Duivenvoorde, L. M., Zanelli, E., Melief, C. J., Snijders, A., Offringa, R., de Vries, R. R. & Toes, R. E. (2003) Arthritis Rheum. 48, 1452–1460. [DOI] [PubMed] [Google Scholar]