Abstract
State‐of‐the‐art health care includes genome sequencing of the patient to identify genetic variants that contribute to either the cause of their malady or variants that can be targeted to improve treatment. The goal was to introduce state‐of‐the‐art health care to cats using genomics and a precision medicine approach. To test the feasibility of a precision medicine approach in domestic cats, a single cat that presented to the University of Missouri, Veterinary Health Center with an undiagnosed neurologic disease was whole‐genome sequenced. The DNA variants from the cat were compared to the DNA variant database produced by the 99 Lives Cat Genome Sequencing Consortium. Approximately 25× genomic coverage was produced for the cat. A predicted p.H441P missense mutation was identified in NPC1, the gene causing Niemann‐Pick type C1 on cat chromosome D3.47456793 caused by an adenine‐to‐cytosine transversion, c.1322A>C. The cat was homozygous for the variant. The variant was not identified in any other 73 domestic and 9 wild felids in the sequence database or 190 additionally genotyped cats of various breeds. The successful effort suggested precision medicine is feasible for cats and other undiagnosed cats may benefit from a genomic analysis approach. The 99 Lives DNA variant database was sufficient but would benefit from additional cat sequences. Other cats with the mutation may be identified and could be introduced as a new biomedical model for NPC1. A genetic test could eliminate the disease variant from the population.
Keywords: Feline, Felis silvestris catus, Lysosomal storage, NPC1, WGS
Abbreviations
- ALP
alkaline phosphatase
- ALT
alanine aminotransferase
- bp
base pair
- bpm
beats per minute
- KIT
v‐kit Hardy‐Zuckerman 4 feline sarcoma viral oncogene homolog
- MRI
magnetic resonance imaging
- NPC1
Niemann‐Pick type C1
- NPC2
Niemann‐Pick type C2
- NPC
Niemann‐Pick type C
- OMIA
Online Mendelian Inheritance in Animals
- OMIM
Online Mendelian Inheritance in Man
- PCR
polymerase chain reaction
- qPCR
quantitative PCR
- WGS
whole‐genome sequencing
The genetic and genomic resources available for health studies of the domestic cat are becoming robust and cost efficient. The sequencing of a cat's entire genome can now be completed for about the cost of a magnetic resonance imaging (MRI) scan. In humans, rapid turnaround whole‐genome sequencing such as the 26‐hour genome efforts has demonstrated how genomic medicine can be applied to health management for acute care cats with time‐critical morbidity and mortalities.1, 2 Although the availability of the bioinformatics infrastructure and turnaround time are not yet as accessible in cats as for humans, the DNA variant database developed by the 99 Lives Cat Genome Sequencing Initiative has proven a valuable first step. Developed from a variety of cats comprising diverse populations and breeds, including those with and without known genetic health problems, the cat variant database supports the identification of DNA variants that are causal for health conditions suspected to have a genetic component. Two whole‐genome sequencing (WGS) studies have already identified a DNA variant in cats associated with progressive retinal atrophy in Persians, a variant causing the bobbed tail of the Japanese Bobtail breed,3 and one responsible for congenital myasthenic syndrome in Devon rex and Sphynx—related cats.4
Precision medicine is an emerging approach for disease diagnosis, treatment, and prevention that takes into account individual variability in genes, environment, and lifestyle. Most medical treatments have been developed for the “average patient”. Precision medicine gives clinicians tools to better understand the complex mechanisms underlying a cat's health, disease, or condition, and to better predict which treatments will be most effective, or to determine polymorphisms requiring different drug dosages (pharmacokinetics).5 Overall, an individual's specific genetic makeup will become an intricate part of their standard health care. This case report shows the potential to apply precision medicine to the diagnosis of neurologic disease in cats.
A 12‐week‐old silver tabby intact female cat of suspected American shorthair lineage presented for a new kitten examination. Abnormal physical examination findings included a pendulous abdomen, soft nonformed feces, and a shaky, unsteady, hypermetric gait causing the cat to fall over. A presumptive diagnosis of cerebellar hypoplasia was made. Two months later, she presented for ovariohysterectomy. During the presurgery examination, her neurologic signs had progressed and she was having difficulty ambulating. Although well hydrated, her weight gain was 0.05 kg in 4 weeks. Presurgery blood tests revealed hypoalbuminemia (1.7 g/dL, reference interval, 2.5–4.4 g/dL), elevated ALT (436 U/L, reference interval 10–118 U/L) and ALP activities (184 U/L, reference interval 20–150 U/L), hyperbilirubinemia (0.6 mg/dL, reference interval 0.1–0.6 mg/dL), and hyperphosphatemia (7.0 mg/dL, reference interval 2.9–6.6 mg/dL). Abdominal radiographs and ultrasonography showed generalized hepatomegaly and splenomegaly. The hepatic parenchyma was hypoechoic and homogenous. The hepatic vasculature was within normal limits. The gall bladder was mildly distended with anechoic bile. Although enlarged, the spleen was homogenous in echogenicity. The remainder of the abdominal ultrasound examination was unremarkable. Postprandial bile acids were elevated (42.1 μmol/L, reference interval <20 μmol/L). The surgery was canceled and referral recommended for further evaluation.
The kitten was referred to the University of Missouri, Veterinary Health Center at 24 weeks of age for evaluation of concurrent hepatic and neurologic disease. On presentation, she was alert, responsive, well hydrated, and weighed 2.0 kg. Abnormalities noted included bradycardia (120 bpm), hepatomegaly, and a distended bladder. Additional neurologic abnormalities included inability to walk without support but with good motor function and hypermetria in all 4 limbs. Palpebral reflexes were normal and the cat was visual, but menace responses were absent. She also had a horizontal nystagmus with the fast phase to the right.
A serum biochemical profile showed hyperphosphatemia (5.6 mg/dL, reference interval, 2–5.3 mg/dL) consistent with a growing kitten; elevated ALT (326 U/L, reference interval 18–77 U/L); and ALP (159 U/L, reference interval 5–55 U/L) activities and total bilirubin (0.6 mg/dL, reference interval 0–0.3 mg/dL) most consistent with hepatocellular injury, cholestasis, and mild hepatic dysfunction. Serum creatine kinase was within the reference interval.
Based on the neurologic assessment, the lesion was localized to the cerebellum. Differential diagnoses included infectious disorders, such as toxoplasmosis, bartonellosis, feline infectious peritonitis encephalitis and others, a progressive developmental defect, and storage disorders. Although cerebellar hypoplasia caused by an intrauterine infection with feline parvovirus can produce cerebellar signs, the severity of signs seen in this cat would make that diagnosis very unlikely. Normally cats with cerebellar hypoplasia are ambulatory, and the disease does not progress. A storage disorder was considered the most likely diagnosis because of the combination of progressive hepatic and neurologic abnormalities, especially given there was hepatomegaly. Diagnosis of a storage disease would require a biopsy, for example, of the liver, which the owner declined.
When evaluated at 30 weeks of age, the cat was eating and drinking but had continued to lose weight. She was nonambulatory, but remained continent if carried to her litter box. She continued to decline and was euthanized at 38 weeks of age. Permission for necropsy was denied.
Methods
The remaining blood clots from the serum biochemical profile were processed for DNA isolation6 to aid diagnosis and to test the concept of precision medicine for cats, with owner informed consent and in accordance with an approved University of Missouri institutional Animal Care and Use Committee protocol (ACUC protocol # 8240). The DNA was submitted for whole‐genome sequencing to the McDonnell Genome Institute at Washington University. The sample was assessed for quantity, and 1000 ng aliquots were distributed for library construction. A TruSeq PCR‐free library (Illumina, San Diego, CA) was constructed with an average fragment size of 350–450 bp. Size selection was accomplished through a paramagnetic bead cleanup postfragmentation. The average insert size was expected to be approximately 350 bp. The concentration of the library was determined by qPCR according to manufacturer's protocols (Kapa Biosystems, Inc., Woburn, MA) to optimize cluster counts for the Illumina HiSeq X (Illumina Inc, San Diego, CA). Library adapters were designed with 8‐bp index sequences allowing for demultiplexing of samples after the sequencing process. Nine libraries from other cat samples from the 99 Lives project (http://felinegenetics.missouri.edu/99lives)3, 4 were pooled together in equal molar ratios, based on the concentration determined by qPCR and run across a HiSeq X flow cell to generate ~1 Tb of data as 2 × 150 bp paired‐end reads. This efficient pooling scheme targets ~30× coverage for each sample. The Illumina HiSeq X Ten was used to generate sequences. Approximately 25× genomic coverage was generated for the case cat. Generated sequences were processed, and the variants were analyzed with active filters provided by Maverix Biomics, Inc. (Santa Cruz, CA) as previously described3, 4 via comparison to the domestic cat reference genome7 and the genomes of 74 domestic cats and 9 wild felids of the 99 Lives Cat Genome Sequencing Initiative. Genes known to be involved with storage diseases were inspected for the presence of high and moderate impact variants. DNA variants were filtered by selecting only variants that were homozygous in the affected cat and not present in any of the other 73 domestic and 9 wild felid sequences in the 99 Lives sequence database.
Additional screening of the newly identified NPC1 variant in random bred and breed cats has been performed with an MassArray system (Agena Bioscience, San Diego, CA) as previously described,3 and primers details are presented in Table S1.
Results
All data have been or will be submitted to the short‐read archives in the United States and Europe upon publication. Current submitted sequences are under bioproject PRJNA308208 (http://www.ncbi.nlm.nih.gov/bioproject/?term=PRJNA308208). A predicted p.H441P missense mutation was identified in NPC1, the gene causing Niemann‐Pick type C1 (NPC1) on cat chromosome D3.47456793 caused by an adenine‐to‐cytosine transversion, c.1322A>C. The cat of this report was homozygous for the variant, and no other cats in the dataset had the variant. The histidine at position 441 is highly conserved across species (Fig 1). PolyPhen‐2 predicts the amino acid change to be benign with a damaging score of 0.43 (sensitivity: 0.89; specificity: 0.90).8 The NPC1 variant is rare as it was not identified in 190 cats (Figure S1).
Figure 1.
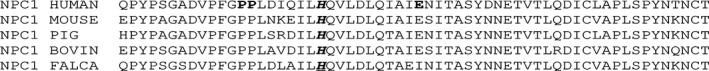
Protein alignment of NPC1 in cats and other species within critical region for the cat variant H441P. The mutation is within the luminal topological domain that includes amino acids 372 to 620. The conserved variant site for this case (p.H441P) is presented in bold italics and underlined. NPC1 in Felis catus has two amino acids shorter compared to human. In humans, three known variants at codon positions 433, 434, and 451 are associated with a disease phenotype and are bold in the alignment.33, 34, 35
Discussion
Niemann‐Pick type C (NPC) disease (NP‐C; OMIM#257220 and OMIM#607625) is an autosomal recessive neurovisceral lysosomal storage disorder that results in defective intracellular transport of cholesterol. Greater than 95% of all human NPC cases are because of variants in the NPC1 gene mapped to chromosome 18q11,9 which is homologous to cat chromosome D3.7, 10 NPC1 in cats was first described as a lipid disorder in a Siamese.11, 12, 13, 14, 15 A feline model of NPC1 (OMIA 000725‐9685) is characterized and is phenotypically, morphologically, and biochemically similar to human NPC1.16, 17, 18, 19, 20, 21, 22 Affected cats show cerebellar and vestibular signs beginning as early as 6 weeks of age. The ataxia progresses to the point where cats fell frequently at 11.8 ± 1.9 weeks of age and were unable to take 1 step without falling at 17 ± 2.1 weeks age. By 19 ± 3 weeks of age, they were unable to stand without assistance, and they were euthanized at 20.5 ± 4.8 weeks of age (range 11–29 weeks).21 The cat in this study was not evaluated before 12 weeks of age but had clear ataxia by 12 weeks of age with difficulty walking by 20 weeks of age. When examined at 24 weeks of age, the cat could not walk without assistance and she was euthanized at 38 weeks of age. Thus, the onset and progression of neurologic signs in this cat are comparable to those observe in the feline NPC1 colony. The cat in this report survived longer before euthanasia but that likely reflects additional nursing care provided to a pet versus cats in a research colony and reluctance to euthanize on the part of the owner. Serum ALP and ALT activities were elevated, and albumin concentrations decreased in the cat in this report comparable to NPC1 colony cats.22 Histopathology and biochemical studies would be necessary to confirm the diagnosis of NPC1 and demonstrate an effect of the variant identified on function. Unfortunately, the owners declined permission for biopsy or necropsy. Thus, we cannot prove the diagnosis of NPC1, which is a limitation of this study.
Complementation studies using cultured fibroblasts from NPC‐affected cats and NPC1‐affected humans support that the gene responsible for the NPC phenotype in this colony of cats is orthologous to the gene responsible for the major form of human NPC, NPC1.23 A single base substitution (c.2864G>C) is identified in these NPC1‐affected cats and in silico predicts a cysteine to a serine change (p.C955S)24 (GenBank # AF503633 and AF503634). The known cat NPC1 variant is predicted to be probably damaging using PolyPhen‐2 with a score of 0.981 (sensitivity: 0.75; specificity: 0.96).8 Heterozygous cats also have metabolic manifestations.19 The parents of the cat could not be obtained for evaluation. In addition, a published intronic c.82+5G>A mutation, which leads to a splicing error in another gene associated with NPC in humans (NPC2), has been identified in cats with similar presentation,25 but no significant variants were identified in NPC2 in the cat of this report. However, as presented in Orphanet (http://www.orpha.net/consor/cgi-bin/index.php?lng=EN), the mutations in NPC1 occur in 95% of the families with NPC type disease and more than 230 mutations have been identified.
The identified NPC1 variant in this cat is novel and predicts a nonconservative missense mutation, a histidine‐to‐proline substitution at position 441 of the NCP1 feline protein. The histidine is highly conserved in several species, and prolines generally cause significant disruption to the normal protein structure. The newly identified variant is not known in human patients, but several proline changes and a terminal variant are within the region of codons 421–474 (http://www.hgmd.cf.ac.uk/ac).26 Although the PolyPhen‐2 prediction was suggested as a benign effect on the protein, other benign predictions are associated with phenotypic effects in cats, such as the Gloving variants associated with KIT that are common to Birmans.7 The NPC1 variant is rare as it was not identified in 190 cats or the other 73 domestic cats and 9 wild felids in the 99 Lives sequence database. However, the population of origin of the affected cat could not be established for further screening of a specific breed.
Precision medicine by WGS has proven to be useful for diagnosis and rapid intervention and treatment for critically ill children.1, 2 Although the treatments for NPC1 are not ready for clinical trials in cats and would not have assisted the present cat, other undiagnosed diseases in cats could benefit from genomics techniques. A second NPC1 biomedical model in cats could be established if other afflicted or carrier cats could be identified, which would further support the development of potential treatments for the disease. Currently, cyclodextrin and miglustat have shown improvement in Purkinje cell survival, thereby preventing cerebellar dysfunction in cats.27, 28, 29, 30 Assuming the cat of this report is representative of a specific breed, its NPC1 variant could be segregating in a breeding population and other homozygous recessive cats may be produced which will succumb to the same condition if a genetic test is not implemented to avoid matings between carriers.
To date, over 40 genes with approximately 70 DNA variants have been documented to cause phenotypic, disease, or blood type variations in the domestic cat (for review).31 The clinical descriptions and phenotypes of each of these diseases and traits have been curated at the Online Mendelian Inheritance in Animals (OMIA) website (http://omia.angis.org.au/home/), which is an invaluable resource comparison of the phenotypes across 2216 animal species.32 These known and any newly identified DNA variants can be genotyped rapidly and cost‐effectively in panels appropriate for breeds, populations, or in cats as part of wellness care. The vigilance of veterinarians and their collaboration with geneticists could lead to the rapid discovery of undiagnosed genetic conditions in cats, which lead to more effective and proactive treatments and preventative strategies. Whole‐genome sequencing of rare and undiagnosed feline cases may be resolved using the precision medicine approach.
Supporting information
Table S1. Genotyping primer sequences for cat NPC1.
Figure S1. Cartesian plot of genotypes detected by mass spectrometry genotyping. Plot representing the genotyping results of 96 cats, only the affected Niemann‐Pick type C cat (upward triangle) was homozygous for the identified variant (c.1322A>C). One sample (circle) was excluded for low genotype quality.
Acknowledgments
We appreciate the laboratory assistance of Nick Gustafson and Erica Creighton. We appreciate the provision of cat DNA samples by Cristy Bird, Sam Boutin, Bruno Chomel, Jeanette Coleman‐Hall, Johnny Gobble, Terri Harris, Anthony Hutcherson, Kyung Sik Kim, Mark Kantrowitz, Sheri Moreau, Nassem N. Naimi of Best Friend Veterinary Clinic in Amman, Jordan, Anthony Nichols, Jean Papo, Julie Pomerantz, John Snape, Susanne and Claus Wehnert, Nancy Carpenter at Utah's Hogle Zoo, Ashleigh Lutz‐Nelson at San Francisco Zoo & Gardens, and Julie Feinstein at the American Museum of Natural History, Franklin Whittenberg.
Conflict of Interest Declaration: Dr. Lyons and Dr. Gandolfi have received funds from the Veterinary Genetics Laboratory (VGL) at the University of California, Davis. This laboratory could develop a commercial service for this mutation and offer genotyping to the public and scientific community. Part of the VGL's income could be used to support additional research for Drs. Lyons and Gandolfi.
Off‐label Antimicrobial Declaration: Authors declare no off‐label use of antimicrobials.
Appendix 1. 99 Lives Consortium (83 cat analysis)
Leslie A. Lyons1, Danielle Aberdein2, Paulo C. Alves3,4, Gregory S. Barsh5,6, Holly C. Beale7, Adam R. Boyko8, Jeffrey A. Brockman9, Marta G. Castelhano10, Patricia P. Chan7, N. Matthew Ellinwood11, Jonathan E. Fogle12, Dorian J. Garrick2,11, Christopher R. Helps13, Marjo K. Hytönen14, Maria Kaukonen14, Christopher B. Kaelin5,6, Emilie Leclerc15, Tosso Leeb16, Hannes Lohi14, Maria Longeri17, Richard Malik18, Michael J. Montague19, John S. Munday2, William J. Murphy20, Niels C. Pedersen21, Max F. Rothschild11, Joshua A. Stern21, William F. Swanson22, Karen A. Terio23, Rory J. Todhunter10, Yu Ueda21, Wesley C. Warren19, Elizabeth A. Wilcox10, Julia H. Wildschutte24, Barbara Gandolfi1.
1Department of Veterinary Medicine and Surgery, College of Veterinary Medicine, University of Missouri, Columbia, Missouri, 65211.
2Institute of Veterinary, Animal and Biomedical Sciences, Massey University, Palmerston North 4474 New Zealand.
3CIBIO/InBIO, Centro de Investigação em Biodiversidade e Recursos Genéticos/InBIO Associate Lab & Faculdade de Ciências, Universidade do Porto, Campus e Vairão, 4485–661 Vila do Conde, Portugal.
4Wildlife Biology Program, University of Montana, Missoula, Montana, 59812.
5HudsonAlpha Institute for Biotechnology, Huntsville, Alabama, 35806.
6Department of Genetics, Stanford University, Stanford, California, 94305.
7Maverix Biomics, Inc., San Mateo, California, 94402.
8Department of Biomedical Sciences, College of Veterinary Medicine, Cornell University, Ithaca, New York, 14853.
9Hill's Pet Nutrition Inc., PO Box 1658, Topeka, KS 66601.
10Department of Clinical Sciences, College of Veterinary Medicine, Cornell University, Ithaca, New York, 14853.
11Department of Animal Science, College of Agriculture and Life Sciences, Iowa State University, Ames, Iowa, 50011.
12College of Veterinary Medicine, North Carolina State University, Raleigh, NC 27607.
13Langford Veterinary Services, University of Bristol, Langford, Bristol, BS40 5DU UK.
14Department of Veterinary Biosciences and Research Programs Unit, Molecular Neurology, University of Helsinki and Folkhälsan Research Center, Helsinki 00014 Finland.
15Diana Pet food, Inc. SPF – ZA du Gohelis, 56250 Elven, France.
16Vetsuisse Faculty, Institute of Genetics, University of Bern, 3001 Bern, Switzerland.
17Dipartimento di Medicina Veterinaria, University of Milan, 20122 Milan, Italy.
18Centre for Veterinary Education, University of Sydney, Sydney, NSW, 2006 Australia.
19The McDonnell Genome Institute, Washington University School of Medicine, St. Louis, Missouri, 63108.
20Department of Veterinary Integrative Biosciences, College of Veterinary Medicine, Texas A&M University, College Station, Texas, 77845.
21Department of Medicine and Epidemiology, School of Veterinary Medicine, University of California at Davis, Davis, California, 95616.
22Center for Conservation and Research of Endangered Wildlife (CREW), Cincinnati Zoo & Botanical Garden, Cincinnati, Ohio, 45220.
23Zoological Pathology Program, University of Illinois, Brookfield, IL 60513.
24Bowling Green State University, Department of Biological Sciences, Bowling Green, OH 43403.
Work: The cat was referred to the Veterinary Health Center at the University of Missouri, Columbia, Missouri, the genetic studies and analysis at the University of Missouri, Columbia, Missouri, the whole‐genome sequencing was performed as fee‐for‐service at The McDonnell Genome Institute at Washington University in St. Louis, Missouri, and partial genome sequence analysis was conducted as fee‐for‐service at Maverix Biomics, Inc., San Mateo, California.
Funding: This work was supported in part by funding from the National Center for Research Resources R24 RR016094 and the Office of Research Infrastructure Programs/OD R24OD010928, and the Winn Feline Foundation (W10‐014, W16‐030) the George Sydney and Phyllis Redman Miller Trust (MT‐13‐010), the National Geographic Society Education Foundation (2P‐14), public and private donations to the 99 Lives Cat Genome Initiative project, including the Associazione Nazionale Felina Italiana, Zoetis, Orivet Genetic Pet Care, Langford Veterinary Services, the World Cat Federation, public donations, and the University of Missouri, College of Veterinary Medicine Gilbreath McLorn endowment.
Presentation: This paper has not been presented at any scientific meeting.
Authors contributed equally to the research.
References
- 1. Miller NA, Farrow EG, Gibson M, et al. A 26‐hour system of highly sensitive whole genome sequencing for emergency management of genetic diseases. Genome Med 2015;7:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Saunders CJ, Miller NA, Soden SE, et al. Rapid whole‐genome sequencing for genetic disease diagnosis in neonatal intensive care units. Sci Transl Med 2012;4:135–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lyons LA, Creighton EK, Alhaddad H, et al. Whole genome sequencing in cats, identifies new models for blindness in AIPL1 and somite segmentation in HES7 . BMC Genom 2016;17:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gandolfi B, Grahn RA, Creighton EK, et al. COLQ variant associated with Devon Rex and Sphynx feline hereditary myopathy. Anim Genet 2015;46:711–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lu YF, Goldstein DB, Angrist M, et al. Personalized medicine and human genetic diversity. Cold Spring Harb Perspect Med 2014;4:a008581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sambrook J, Fritsch EF, Maniatis T. Molecular Cloning: A Laboratory Manual, 2nd ed New York, New York: Cold Spring Laboratory Press; 1989. [Google Scholar]
- 7. Montague MJ, Li G, Gandolfi B, et al. Comparative analysis of the domestic cat genome reveals genetic signatures underlying feline biology and domestication. Proc Nat Acad Sci USA 2014;111:17230–17235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Adzhubei IA, Schmidt S, Peshkin L, et al. A method and server for predicting damaging missense mutations. Nat Methods 2010;7:248–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Burlina A. Niemann‐Pick disease type C: Introduction and main clinical features. J Neurol 2014;261(Suppl 2):S525–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. O'Brien SJ, Wienberg J, Lyons LA. Comparative genomics: Lessons from cats. Trends Genet: TIG 1997;13:393–399. [DOI] [PubMed] [Google Scholar]
- 11. Crisp CE, Ringler DH, Abrams GD, et al. Lipid storage disease in a Siamese cat. J Am Vet Med Assoc 1970;156:616–622. [PubMed] [Google Scholar]
- 12. Percy DH, Jortner BS. Feline lipidosis. Light and electron microscope studies. Arch Pathol 1971;92:136–144. [PubMed] [Google Scholar]
- 13. Wenger DA, Sattler M, Kudoh T, et al. Niemann‐Pick disease: A genetic model in Siamese cats. Science 1980;208:1471–1473. [DOI] [PubMed] [Google Scholar]
- 14. Snyder SP, Kingston RS, Wenger DA. Niemann‐Pick disease. Sphingomyelinosis of Siamese cats. Am J Pathol 1982;108:252–254. [PMC free article] [PubMed] [Google Scholar]
- 15. Baker HJ, Wood PA, Wenger DA, et al. Sphingomyelin lipidosis in a cat. Vet Pathol 1987;24:386–391. [DOI] [PubMed] [Google Scholar]
- 16. Lowenthal AC, Cummings JF, Wenger DA, et al. Feline sphingolipidosis resembling Niemann‐Pick disease type C. Acta Neuropathol 1990;81:189–197. [DOI] [PubMed] [Google Scholar]
- 17. Brown DE, Thrall MA, Walkley SU, et al. Feline Niemann‐Pick disease type C. Am J Pathol 1994;144:1412–1415. [PMC free article] [PubMed] [Google Scholar]
- 18. Munana KR, Luttgen PJ, Thrall MA, et al. Neurological manifestations of Niemann‐Pick disease type C in cats. J Vet Intern Med 1994;8:117–121. [DOI] [PubMed] [Google Scholar]
- 19. Brown DE, Thrall MA, Walkley SU, et al. Metabolic abnormalities in feline Niemann‐Pick type C heterozygotes. J Inherit Metab Dis 1996;19:319–330. [DOI] [PubMed] [Google Scholar]
- 20. March PA, Thrall MA, Brown DE, et al. GABAergic neuroaxonal dystrophy and other cytopathological alterations in feline Niemann‐Pick disease type C. Acta Neuropathol 1997;94:164–172. [DOI] [PubMed] [Google Scholar]
- 21. Vite CH, Ding W, Bryan C, et al. Clinical, electrophysiological, and serum biochemical measures of progressive neurological and hepatic dysfunction in feline Niemann‐Pick type C disease. Pediatr Res 2008;64:544–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bagel JH, Sikora TU, Prociuk M, et al. Electrodiagnostic testing and histopathologic changes confirm peripheral nervous system myelin abnormalities in the feline model of niemann‐pick disease type C. J Neuropathol Exp Neurol 2013;72:256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Somers KL, Wenger DA, Royals MA, et al. Complementation studies in human and feline Niemann‐Pick type C disease. Mol Genet Metab 1999;66:117–121. [DOI] [PubMed] [Google Scholar]
- 24. Somers KL, Royals MA, Carstea ED, et al. Mutation analysis of feline Niemann‐Pick C1 disease. Mol Genet Metab 2003;79:99–103. [DOI] [PubMed] [Google Scholar]
- 25. Zampieri S, Bianchi E, Cantile C, et al. Characterization of a spontaneous novel mutation in the NPC2 gene in a cat affected by Niemann Pick type C disease. PLoS ONE 2014;9:e112503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McKay Bounford K, Gissen P. Genetic and laboratory diagnostic approach in Niemann Pick disease type C. J Neurol 2014;261(Suppl 2):S569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ward S, O'Donnell P, Fernandez S, et al. 2‐hydroxypropyl‐beta‐cyclodextrin raises hearing threshold in normal cats and in cats with Niemann‐Pick type C disease. Pediatr Res 2010;68:52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stein VM, Crooks A, Ding W, et al. Miglustat improves purkinje cell survival and alters microglial phenotype in feline Niemann‐Pick disease type C. J Neuropathol Exp Neurol 2012;71:434–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ottinger EA, Kao ML, Carrillo‐Carrasco N, et al. Collaborative development of 2‐hydroxypropyl‐beta‐cyclodextrin for the treatment of Niemann‐Pick type C1 disease. Curr Top Med Chem 2014;14:330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vite CH, Bagel JH, Swain GP, et al. Intracisternal cyclodextrin prevents cerebellar dysfunction and Purkinje cell death in feline Niemann‐Pick type C1 disease. Sci Transl Med 2015;7:276ra226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lyons LA. DNA mutations of the cat: The good, the bad and the ugly. J Feline Med Surg 2015;17:203–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nicholas FW, Le Tissier PR. Online Mendelian Inheritance in Animals, OMIA. Faculty of Veterinary Science, University of Sydney. Available at: http://omia.angis.org.au/ Accessed March 10, 2016.
- 33. Fernandez‐Valero EM, Ballart A, Iturriaga C, et al. Identification of 25 new mutations in 40 unrelated Spanish Niemann‐Pick type C cats: Genotype‐phenotype correlations. Clin Genet 2005;68:245–254. [DOI] [PubMed] [Google Scholar]
- 34. Park WD, O'Brien JF, Lundquist PA, et al. Identification of 58 novel mutations in Niemann‐Pick disease type C: Correlation with biochemical phenotype and importance of PTC1‐like domains in NPC1. Hum Mutat 2003;22:313–325. [DOI] [PubMed] [Google Scholar]
- 35. Tarugi P, Ballarini G, Bembi B, et al. Niemann‐Pick type C disease: Mutations of NPC1 gene and evidence of abnormal expression of some mutant alleles in fibroblasts. J Lipid Res 2002;43:1908–1919. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Genotyping primer sequences for cat NPC1.
Figure S1. Cartesian plot of genotypes detected by mass spectrometry genotyping. Plot representing the genotyping results of 96 cats, only the affected Niemann‐Pick type C cat (upward triangle) was homozygous for the identified variant (c.1322A>C). One sample (circle) was excluded for low genotype quality.


