Cardiac allograft vasculopathy (CAV) is a leading cause of long-term morbidity and mortality after heart transplantation [1]. Conventional methods for monitoring for CAV detect CAV after it has developed, which may be too late to modify its course. Endothelial dysfunction and the index of microcirculatory resistance (IMR) assessed soon after transplantation have both been shown in separate studies to predict development of CAV and long-term adverse outcome [2,3]. The purpose of this study (URL: https://www.clinicaltrials.gov, unique identifier: NCT01078363) is to quantify the combined impact of early endothelial dysfunction and elevated microvascular resistance as a marker of subsequent development of CAV at 1 year after cardiac transplantation.
Forty-four heart transplant recipients underwent intracoronary acetylcholine (Ach) injection (50–100 ug over 30 seconds), coronary physiology assessment, and volumetric intravascular ultrasound (IVUS) analysis performed in the left anterior descending (LAD) coronary artery within eight weeks after transplantation (baseline) and at one year. Endothelial dysfunction was defined as ≥20% percent change in diameter of the LAD as measured by quantitative angiography after Ach and compared to baseline angiography [2]. Elevated microvascular resistance was defined as an IMR ≥20 [3]. IMR was assessed with a coronary pressure/thermistor tipped wire and calculated by multiplying the mean distal coronary pressure by the mean hyperemic transit time during intravenous adenosine infusion (140 ug/kg/min). The study was approved by Stanford’s Internal Review Board and all participants provided informed written consent.
Endothelial dysfunction was observed in 23 (52.3%) patients. Elevated microvascular resistance was observed in 17 (38.6%) patients. During follow-up, plaque volume (PV) increased significantly in patients with endothelial dysfunction (3.10 ± 1.48 mm3/mm to 3.67 ± 1.63 mm3/mm; p=0.006) and in those with elevated microvascular resistance (3.03 ± 0.95 mm3/mm to 3.47 ± 1.37 mm3/mm; p=0.039). In multivariate linear regression analysis, endothelial dysfunction (β coefficient=21.0, 95% confidence interval 4.8 – 37.1; p=0.012) and elevated microvascular resistance at baseline (β coefficient=18.2, 95% confidence interval 0.66 – 35.7; p=0.042) were independent markers of subsequent % change in PV during the first year after cardiac transplantation. When patients were categorized into 3 groups based on endothelial function and microvascular resistance, patients with both endothelial dysfunction and elevated microvascular resistance had significantly greater % change in PV from baseline to 1 year compared to those with either endothelial dysfunction or elevated microvascular resistance alone (p=0.037) and to those with neither endothelial dysfunction nor elevated microvascular resistance (p=0.001), after adjustment for confounding variables (Figure). There was a significant difference in % change in PV from baseline to 1 year after heart transplantation among the 3 groups (p=0.009). There were no significant differences in the use of statin (p=0.438), incidence of allograft rejection ≥ grade 2R (p=0.438), or CMV infection (p=0.747) in the first year among the 3 groups. In multivariate regression analysis, the combination of endothelial dysfunction and elevated microvascular resistance was an independent marker of subsequent % change in PV from baseline to 1 year after adjusting for male donor status, cold ischemic time, and plaque volume at baseline (β coefficient=38.9, 95% confidence interval 9.9 – 67.9; p=0.01). Percent change in arterial diameter after Ach administration at baseline angiography correlated with % change in IMR (r=−0.331, p=0.028) from baseline to one year. Moreover, in those patients without endothelial dysfunction at baseline, IMR decreased from baseline to one year (p=0.05).
Figure 1.
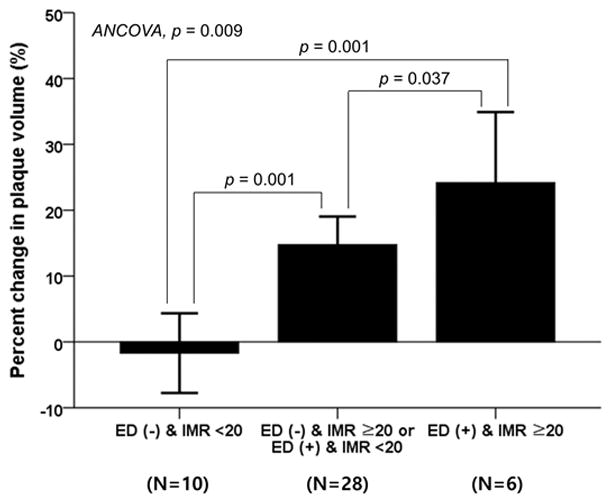
Percent change in plaque volume from baseline to 1 year in patients with no endothelial dysfunction or elevated microvascular resistance, with either endothelial dysfunction or elevated microvascular resistance, and with both endothelial dysfunction and elevated microvascular resistance. ED = endothelial dysfunction; IMR = index of microcirculatory resistance
Change in maximal intimal thickness (MIT) seen on serial IVUS has become the primary modality for identifying CAV [4,5]. However, this requires performing IVUS at two time points and identifies CAV after it has already developed. Ideally, one would like to identify at risk patients soon after transplantation, before CAV actually develops. The two main findings of this study are as follows: (1) endothelial dysfunction and elevated microvascular resistance soon after cardiac transplantation are independent markers of subsequent development of CAV; (2) the combination of endothelial dysfunction and elevated microvascular resistance is an independent marker of subsequent plaque progression at 1 year.
Although the presence of endothelial dysfunction has been shown previously to predict changes in MIT on IVUS examination, the correlation between endothelial dysfunction and changes in plaque volume and the additive value of elevated microvascular resistance in predicting CAV are new findings. Coronary microvascular function has an impact on long-term graft survival after heart transplantation [3]. However, the mechanism by which microvascular dysfunction impacts outcome is not well elucidated. In the present study, elevated microvascular resistance was associated with the development of CAV at 1 year. Moreover, the epicardial artery response to Ach correlated significantly with the change in microvascular resistance. This correlation may indicate that in the early stage of CAV, both the epicardial artery and the microvasculature are concordantly involved. In the present study, microvascular resistance improved in most patients during the first year, except in those with endothelial dysfunction. A possible explanation for the relationship between elevated microvascular resistance and epicardial endothelial dysfunction is that after heart transplantation, both are affected by vascular inflammation resulting from the recipient immune response, metabolic changes, and infection [1].
Integrating the assessment of endothelial function and microvascular resistance early after heart transplantation identifies patients at risk for developing CAV and may provide early treatment targets in the course of allograft vascular disease.
Acknowledgments
Sources of Funding: This study is supported by the NIH (5R01HL093475-05, PI: WFF).
Footnotes
Disclosures: WFF, an institutional research support from St. Jude Medical; YK, an institutional research fellowship grant from Boston Scientific. All other authors have nothing to disclose.
References
- 1.Lund LH, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Goldfarb S, Levvey BJ, Meiser B, Rossano JW, Yusen RD, Stehlik J. The Registry of the International Society for Heart and Lung Transplantation: Thirty-second Official Adult Heart Transplantation Report--2015; Focus Theme: Early Graft Failure. J Heart Lung Transplant. 2015;34:1244–54. doi: 10.1016/j.healun.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Davis SF, Yeung AC, Meredith IT, Charbonneau F, Ganz P, Selwyn AP, Anderson TJ. Early endothelial dysfunction predicts the development of transplant coronary artery disease at 1 year posttransplant. Circulation. 1996;93:457–62. doi: 10.1161/01.cir.93.3.457. [DOI] [PubMed] [Google Scholar]
- 3.Yang HM, Khush K, Luikart H, Okada K, Lim HS, Kobayashi Y, Honda Y, Yeung AC, Valantine H, Fearon WF. Invasive Assessment of Coronary Physiology Predicts Late Mortality After Heart Transplantation. Circulation. 2016;133:1945–50. doi: 10.1161/CIRCULATIONAHA.115.018741. [DOI] [PubMed] [Google Scholar]
- 4.Yeung AC, Davis SF, Hauptman PJ, Kobashigawa JA, Miller LW, Valantine HA, Ventura HO, Wiedermann J, Wilensky R. Incidence and progression of transplant coronary artery disease over 1 year: results of a multicenter trial with use of intravascular ultrasound: Multicenter Intravascular Ultrasound Transplant Study Group. J Heart Lung Transplant. 1995;14:S215–S220. [PubMed] [Google Scholar]
- 5.Kobashigawa JA, Tobis JM, Starling RC, Tuzcu EM, Smith AL, Valantine HA, Yeung AC, Mehra MR, Anzai H, Oeser BT, Abeywickrama KH, Murphy J, Cretin N. Multicenter intravascular ultrasound validation study among heart transplant recipients: outcomes after five years. J Am Coll Cardiol. 2005;45:1532–7. doi: 10.1016/j.jacc.2005.02.035. [DOI] [PubMed] [Google Scholar]


