Abstract
Objective
Determine if second opinion reviews of PET/CT examinations by subspecialists alters reporting of malignant findings.
Methods
This IRB-approved study compared 240 FDG PET/CT consecutively dictated reports by two nuclear medicine subspecialists against the original outside institution reports. Subspecialist reviews documented if malignant findings on the outside report were malignant, and noted additional malignant findings not described on the outside report. Final diagnosis of malignancy or benignity was determined by pathology when available, otherwise by imaging follow-up.
Results
22 findings (in 20 reports) called suspicious/malignant on the outside reports were deemed benign by subspecialist review. A final diagnosis was available for 20 of 22 findings by pathology (3) or follow-up imaging (17). The subspecialist review was accurate in 20 of 20 (100%) cases where a final diagnosis was available. The subspecialist review called 11 findings (in 11 reports) suspicious/malignant that were not described or deemed benign on the outside reports. Definitive diagnosis was available for 10 of 11 findings by pathology (7) or follow-up imaging (3). The second opinion report was accurate in 7 of 10 (70%) cases where a final diagnosis was available.
Conclusions
In 31 of 240 (13%) FDG PET/CT examinations performed at an outside institution, subspecialist review resulted in at least one discordant opinion of malignancy. For 28 discrepant cases where a final diagnosis was available, the subspecialist review defined malignancy or benignity correctly in 25 of 28 (89%) cases. This provides evidence for cost and effort invested in performing second opinion reviews of PET/CT studies.
Keywords: FDG, PET/CT, second opinion
INTRODUCTION
In many specialty oncologic centers, radiology studies initially performed and interpreted at an outside institution undergo a second review by in-house specialists. At our institution the numbers of requests for in-house specialist reassessments of FDG PET/CT studies has been rapidly increasing. In 2010, 629 second opinion reviews of FDG PET/CT scans were performed at our institution. By 2012, that number had increased to 1,157, and in 2015, 2,053 second opinion reviews of FDG PET/CT scans were performed. Several studies have suggested that subspecialty review of body CT, neuroradiology, and mammography exams have varying levels of benefit, with discrepancy rates between the initial report and the specialist reassessment ranging between 1 and 19% [1–8]. The value of subspecialist review of FDG PET/CT scans is unknown. Determining the value of subspecialist review of outside institution PET/CT examinations is an important issue, particularly when considering the allocation of limited personnel and resources to perform these second opinion reassessments, as well as whether a rationale exists for reimbursement of these reassessments, which add cost to patient care. In this study, we investigated if nuclear medicine subspecialist review of outside institution PET/CT examinations resulted in more accurate reporting of malignant findings, with pathology or follow-up imaging as the gold standard.
MATERIALS AND METHODS
This study was performed with institutional review board approval. The cohort consisted of 240 consecutive outside institution FDG PET/CT examinations reassessed by two nuclear medicine subspecialists (GAU and MD) between June and December 2010. Institutional policy requires an outside hospital report to accompany examinations submitted for in-house reassessments, thus outside hospital reports were available on all studies. All studies were digitized into the institutional PACS and viewed as multiplanar FDG PET, CT, and hybrid PET/CT images using GE PET/CT software (AW suite).
Each exam was interpreted by a single specialist. The specialist reassessment included an evaluation of each organ system called suspicious or malignant on the outside report (for example, right breast cancer with thoracic nodal, lung, and osseous metastases). For each organ system called suspicious or malignant on the outside report, the specialist documented if they believed the imaging findings were indeed malignant, or benign. Specialist reassessment also documented additional organ systems believed to be suspicious for or containing malignancy that were either not mentioned on the outside report or were described as benign. All patients were then followed prospectively to document pathology and/or follow-up imaging which provided a final diagnosis of malignancy or benignity. Pathology was given precedence as the gold standard, but many findings described as benign on the subspecialist review were not histologically sampled, and in these cases follow-up imaging was used. Follow-up was continued until December 2015.
RESULTS
A total of 240 outside hospital PET/CT examinations—one per patient—were reviewed for a second opinion, and the outside hospital report was available for all 240 examinations. The most common primary malignancies of the patients in this study were breast cancer, lymphoma, and lung cancer. The characteristics for the 240 patients are reported in Table 1.
TABLE 1.
Characteristics of 240 patients with outside hospital FDG PET/CT scans reviewed
| Age (median, (range)) | 64 (7–80) |
| Sex (n, (%)) | |
| Male | 126 (53) |
| Female | 114 (47) |
| Primary malignancy (n) | |
| Anal | 5 |
| Bladder | 4 |
| Breast | 37 |
| Cervical | 12 |
| Colorectal | 19 |
| Endometrial | 8 |
| Esophageal | 6 |
| Ewing Sarcoma | 3 |
| Head/Neck Squamous Cell | 8 |
| Lymphoma | 31 |
| Lung cancer | 27 |
| Lung nodule | 12 |
| Melanoma | 2 |
| Mesothelioma | 3 |
| Multiple Myeloma | 13 |
| Osteogenic sarcoma | 2 |
| Ovarian | 11 |
| Pancreatic | 5 |
| Thyroid | 8 |
| Uterine Leiomyosarcoma | 2 |
| Unknown Primary | 15 |
| Other | 7 |
Other = carcinoid (1), cholangiocarcinoma (1), desmoplastic small round cell tumor (1), “hilar mass” (1), “increased CEA” (1), neuroblastoma (1), synovial sarcoma (1)
Of the 240 FDG PET/CT examinations initially interpreted at an outside institution, 20 outside reports described suspicious/malignant findings that were called benign in the specialist review. This includes two examinations containing two findings called suspicious/malignant on the outside report that were both deemed to be benign in the specialist review. Thus, a total of 22 findings in 20 examinations were called suspicious/malignant in outside reports but were deemed to be benign by specialist review (Table 2). After prospective follow-up, a final diagnosis was available in 20 of these 22 findings by pathology (n=3) or follow-up imaging (n=17). In all 20 cases where a final diagnosis was available, the final diagnosis was benign. Thus, the specialist review accurately predicted benignity in all 20 of 20 cases (100%). The most common findings called suspicious/malignant on outside reports but benign on second opinion review were benign FDG-avid mediastinal lymph nodes, FDG-avid adnexal cysts in premenopausal women, and physiologic rectal sphincter FDG avidity (Table 1). Examples of findings called suspicious/malignant on initial outside hospital reports but called benign on the second opinion report are demonstrated in Figures 1 and 2.
TABLE 2.
Twenty-two findings in 20 patients called suspicious/malignant on initial outside hospital PET/CT report were called benign on the second opinion report. In all 20 cases with a diagnosis on follow-up, a benign etiology was confirmed.
| n | n with follow-up | |
|---|---|---|
| FDG-avid symmetric mediastinal/hilar nodes | 4 | 3 |
| FDG-avid adnexal cyst in premenopausal woman | 3 | 3 |
| FDG-avid rectal sphincter | 3 | 3 |
| FDG-avid post-radiation pneumonitis | 2 | 1 |
| FDG-avid thyroid lobes called nodes | 1 | 1 |
| FDG-avid thymus | 1 | 1 |
| Loculated pleural effusion called a mass | 1 | 1 |
| FDG-avid post-surgical inflammation | 1 | 1 |
| FDG-avid symmetric palatine tonsils | 1 | 1 |
| FDG-avid posterior cricoarytenoid muscle | 1 | 1 |
| FDG-avid brown fat | 1 | 1 |
| Bone marrow statistical noise | 1 | 1 |
| FDG-avid subcentimeter neck node | 1 | 1 |
| FDG-avid ulcerative colitis | 1 | 1 |
| Total | 22 | 20 |
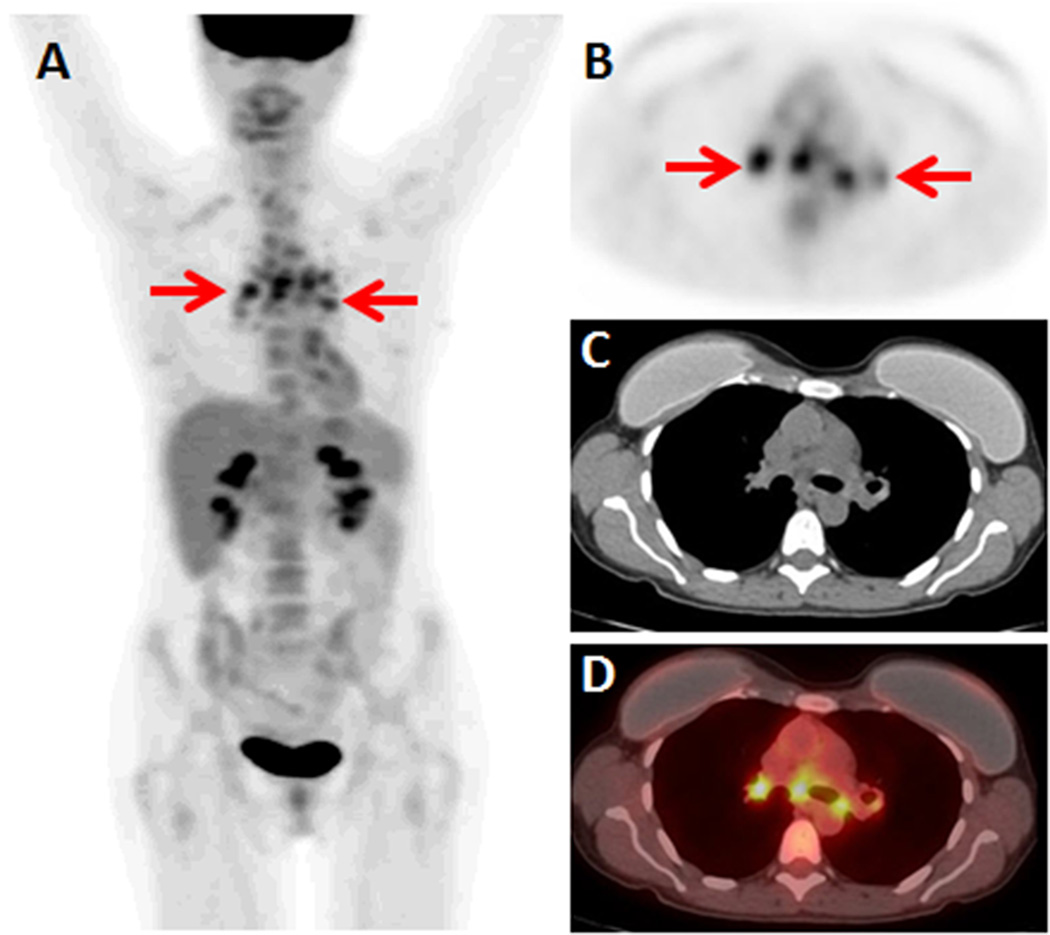
Figure 1.
48-year-old woman with invasive ductal breast cancer. FDG PET/CT was ordered for systemic staging. (A) FDG PET MIP demonstrates multiple FDG-avid foci in the medial thorax (arrows). (B) Axial FDG PET, (C) axial non-contrast CT, and (D) axial FDG PET/CT demonstrate the FDG-avid foci localize symmetrically to the mediastinum and bilateral hila (arrows), without corresponding masses on CT. These findings were called nodal metastases on the initial report. Second opinion report called these findings likely benign, noting that bilateral hilar and mediastinal nodal metastases without axillary or internal mammary nodal metastases would be highly unlikely. A mediastinal biopsy was performed, yielding a diagnosis of sarcoidosis.
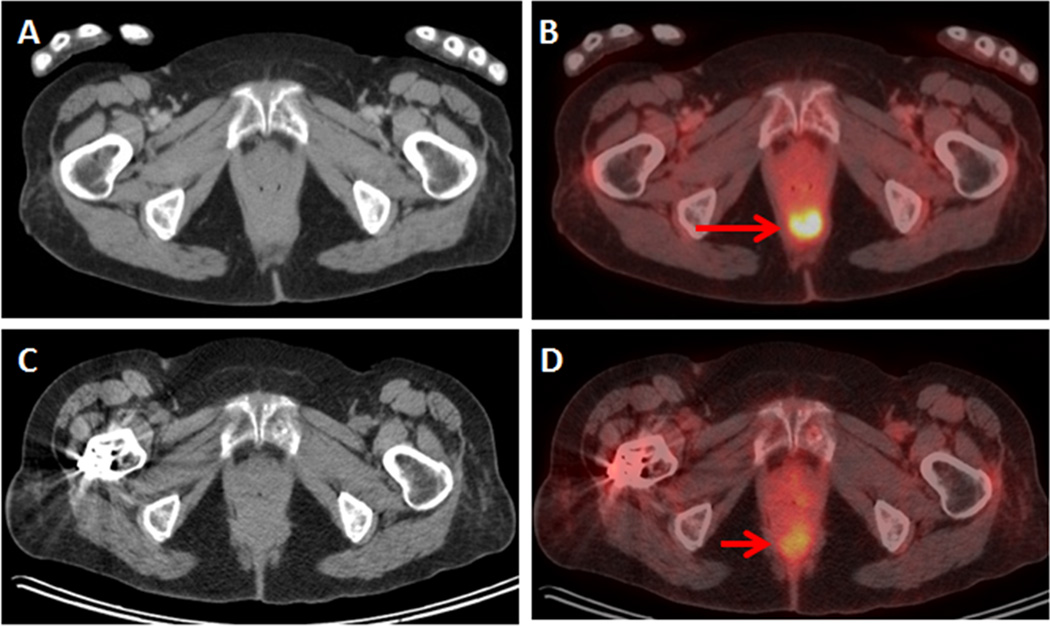
Figure 2.
73-year-old woman with ovarian cancer. FDG PET/CT was ordered for staging. (A) Axial CT and (B) axial fused PET/CT demonstrate an FDG-avid focus in the inferior pelvis, without corresponding mass on CT. This was called malignant on the initial report. Second opinion report called this finding benign, noting the FDG-avid focus localized to the distal rectum and represented the rectal sphincter. Follow-up FDG PET/CT with (C) axial CT and (D) axial fused PET/CT demonstrated resolution of the FDG-avid focus, consistent with benign rectal sphincter avidity.
Also within the cohort of 240 FDG PET/CT examinations were 11 examinations where additional suspicious/malignant findings were noted on the subspecialist second opinion report, but were not included or were called benign on the initial outside hospital report (Table 3). After prospective follow-up, a final diagnosis was available in 10 of the 11 cases by pathology (n=7) or follow-up imaging (n=3). In 7 of 10 cases where a final diagnosis was available, the final diagnosis was malignant (70%). Thus, the specialist review accurately predicted additional malignancy in 70% of the cases where additional malignancy was described, but was incorrect in the remaining 30%. The most common finding called suspicious/malignant on the second opinion report, but were not included or were called benign on the initial outside hospital report were lung nodules with absent or low FDG-avidity. An example of a finding called suspicious/malignant on the second opinion report but was not included or called benign on the initial report is demonstrated in Figure 3.
TABLE 3.
Eleven findings in 11 patients called suspicious/malignant on the second opinion report were not included or were called benign on the initial outside hospital PET/CT report. Of the 11 findings, follow-up demonstrated 6 to be malignant and 4 to be benign. Follow-up was not available on one finding.
| n | |
|---|---|
| Follow-up was malignant | |
| Lung nodules | 3 |
| Cervical node called muscle on initial report | 1 |
| Pelvic node called physiologic bowel on initial report | 1 |
| Bladder mass not mentioned on initial report | 1 |
| FDG-avid scapula focus | 1 |
| Follow-up was benign | |
| Lung nodule | 1 |
| FDG-avid brain focus | 1 |
| FDG-avid stomach wall thickening | 1 |
| No follow-up available | |
| FDG-avid muscle focus | 1 |
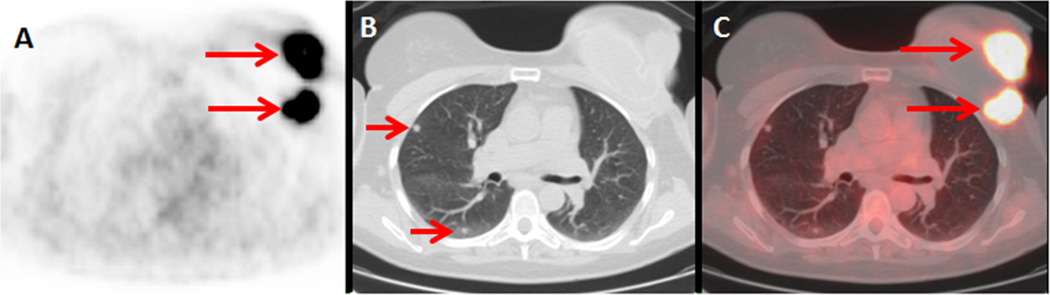
Figure 3.
55-year-old woman with invasive ductal breast cancer. FDG PET/CT was ordered for systemic staging. (A) Axial FDG PET, (B) axial non-contrast CT, and (C) axial FDG PET/CT demonstrate the FDG-avid locally advanced left breast cancer (long arrows). The CT on lung windows demonstrated multiple small rounded nodules, without corresponding FDG avidity on PET. The nodules were called probably benign on the original report, noting lack of FDG avidity. Second opinion report called the lung nodules probably malignant. Biopsy demonstrated metastatic breast cancer, which increased the patient’s tumor stage to IV.
In addition to discrepancies with benignity/malignancy, second opinion reports detected one case of pneumomediastinum and one case of left vocal cord paralysis that were not mentioned on the outside hospital report.
DISCUSSION
Given limited personnel and resources, determining whether there is value to second opinion reviews of FDG PET/CT examinations is an important issue. In this study, we demonstrate that second opinion review of FDG PET/CT exams performed at outside institutions resulted in a change in assignment of malignancy/benignity in 31 of 240 (13%) of cases. When a case had a discrepancy, a definite diagnosis was available for 28 of 31 (90%) cases. In the 28 cases where a definitive diagnosis was available, the second opinion review was correct in 25 of them (89%). These results suggest that subspecialist review of PET/CT examinations performed at an outside institution increases the accuracy of exam interpretation.
The most common discrepancies were common physiologic and inflammatory sources of FDG avidity being described as suspicious/malignant and overlooked lung nodules. It is important to recognize FDG-avid lesions that are benign, which in this study were most commonly benign FDG-avid mediastinal lymph nodes from inflammatory etiologies [9], FDG-avid physiologic adnexal cysts in premenopausal women [10], and physiologic rectal sphincter FDG avidity. Not all malignancies will be appreciably FDG-avid, and may be detected on the CT component of the FDG PET/CT [11, 12]. Lung nodules may be malignant despite apparent lack of FDG avidity [13]. As the field of PET/CT advances, and certain findings become more widely recognized, the discrepancies revealed by second opinion reviews may change.
At our institution, not all outside hospital FDG PET/CTs are submitted for formal second opinion reviews; the referring clinicians determine which studies are submitted for formal reviews. Thus, there is almost certainly selection bias in which studies were submitted for second opinion reviews. Clinicians may have selected studies for a second opinion if they found that the initial report did not match their clinical impression or if they disagreed with the report findings. This may have increased the proportion of studies for which a second opinion reader was likely to find a discrepancy.
The finding that second opinion reads by subspecialists increase the accuracy of interpretations of the submitted exams does not necessarily mean that the subspecialists perform better reads. In order to demonstrate that, initial reads performed by subspecialists would need to undergo second opinion review by non-subspecialists to determine the proportion of studies where second opinion review improves upon the subspecialist read. Then those results would need to be compared to the results of the current study.
A relatively large number of PET/CT reports with unknown primary tumor were reviewed in this study (n = 15 of 240). It may be that our referring clinicians selected these patients as ones for which they wanted subspecialist review. The only discrepancy noted by subspecialist review of the 15 cases of unknown primary tumor was one case where the subspecialist noted FDG-avid stomach wall thickening and suggested work-up. Endoscopy and biopsy demonstrated that this was benign gastritis.
The strengths of this study include the availability of reports for sequential outside hospital PET/CT examinations, which reduces the potential for selection bias by investigators, as well as the prospective follow-up of patients with discrepancy interpretations to allow for a diagnosis in the vast majority of cases. The limitations of the study include the potential for selection bias in which PET/CT examinations were submitted for second opinion reviews (as described above), the fact that the second opinion review was performed at a different time as the initial read and clinical scenario may not have been identical at the two time points, and the single institutional study design which may limit generalizability.
Subspecialist second opinion review of PET/CT examinations performed at an outside institution appears to increase accuracy of exam interpretation. This provides evidence for the value of second opinion review of PET/CT exams, as well as a rationale for the use of limited resources and accommodating the costs associated with performing second opinion reviews. Larger studies may be needed to confirm these results and determine the tumor types that derive the largest benefit from subspecialist second opinion reviews.
Acknowledgments
Financial Disclosure: This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
References
- 1.Gollub MJ, Panicek DM, Bach AM, Penalver A, Castellino RA. Clinical importance of reinterpretation of body CT scans obtained elsewhere in patients referred for care at a tertiary cancer center. Radiology. 1999;210(1):109–112. doi: 10.1148/radiology.210.1.r99ja47109. [DOI] [PubMed] [Google Scholar]
- 2.Loughrey GJ, Carrington BM, Anderson H, Dobson MJ, Lo Ying Ping F. The value of specialist oncological radiology review of cross-sectional imaging. Clin Radiol. 1999;54(3):149–154. doi: 10.1016/s0009-9260(99)91003-6. discussion 154-145. [DOI] [PubMed] [Google Scholar]
- 3.Loevner LA, Sonners AI, Schulman BJ, Slawek K, Weber RS, Rosenthal DI, et al. Reinterpretation of cross-sectional images in patients with head and neck cancer in the setting of a multidisciplinary cancer center. AJNR American journal of neuroradiology. 2002;23(10):1622–1626. [PMC free article] [PubMed] [Google Scholar]
- 4.Jordan MJ, Lightfoote JB, Jordan JE. Quality outcomes of reinterpretation of brain CT imaging studies by subspecialty experts in neuroradiology. Journal of the National Medical Association. 2006;98(8):1326–1328. [PMC free article] [PubMed] [Google Scholar]
- 5.Leung JW, Margolin FR, Dee KE, Jacobs RP, Denny SR, Schrumpf JD. Performance parameters for screening and diagnostic mammography in a community practice: are there differences between specialists and general radiologists? AJR Am J Roentgenol. 2007;188(1):236–241. doi: 10.2214/AJR.05.1581. [DOI] [PubMed] [Google Scholar]
- 6.Briggs GM, Flynn PA, Worthington M, Rennie I, McKinstry CS. The role of specialist neuroradiology second opinion reporting: is there added value? Clin Radiol. 2008;63(7):791–795. doi: 10.1016/j.crad.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Zan E, Yousem DM, Carone M, Lewin JS. Second-opinion consultations in neuroradiology. Radiology. 2010;255(1):135–141. doi: 10.1148/radiol.09090831. [DOI] [PubMed] [Google Scholar]
- 8.Hatzoglou V, Omuro AM, Haque S, Khakoo Y, Ganly I, Oh JH, et al. Second-opinion interpretations of neuroimaging studies by oncologic neuroradiologists can help reduce errors in cancer care. Cancer. 2016;122(17):2708–2714. doi: 10.1002/cncr.30083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rayamajhi SJ, Mittal BR, Maturu VN, Agarwal R, Bal A, Dey P, et al. (18)F-FDG and (18)F-FLT PET/CT imaging in the characterization of mediastinal lymph nodes. Annals of nuclear medicine. 2016;30(3):207–216. doi: 10.1007/s12149-015-1047-6. [DOI] [PubMed] [Google Scholar]
- 10.Bagga S. A corpus luteal cyst masquerading as a lymph node mass on PET/CT scan in a pregnant woman with an anterior mediastinal lymphomatous mass. Clin Nucl Med. 2007;32(8):649–651. doi: 10.1097/RLU.0b013e3180a1ab8f. [DOI] [PubMed] [Google Scholar]
- 11.Hogan MP, Goldman DA, Dashevsky B, Riedl CC, Gonen M, Osborne JR, et al. Comparison of 18F-FDG PET/CT for Systemic Staging of Newly Diagnosed Invasive Lobular Carcinoma Versus Invasive Ductal Carcinoma. J Nucl Med. 2015;56(11):1674–1680. doi: 10.2967/jnumed.115.161455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dashevsky BZ, Goldman DA, Parsons M, Gonen M, Corben AD, Jochelson MS, et al. Appearance of untreated bone metastases from breast cancer on FDG PET/CT: importance of histologic subtype. Eur J Nucl Med Mol Imaging. 2015 doi: 10.1007/s00259-015-3080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Velloso MJ, Bastarrika G, de-Torres JP, Lozano MD, Sanchez-Salcedo P, Sancho L, et al. Assessment of indeterminate pulmonary nodules detected in lung cancer screening: Diagnostic accuracy of FDG PET/CT. Lung cancer (Amsterdam, Netherlands) 2016;97:81–86. doi: 10.1016/j.lungcan.2016.04.025. [DOI] [PubMed] [Google Scholar]