Abstract
Using data from the Multi-Ethnic Study of Atherosclerosis baseline sample from 2000–2002 (N=5263; mean age=62) we examined cross-sectional racial/ethnic differences in ideal CVH, defined by the American Heart Association 2020 Impact Goals as a summary measure of ideal levels of blood pressure, fasting glucose, cholesterol, body mass index, diet, physical activity, and smoking. Using three different analytical approaches, we examined differences before and after adjustment for neighborhood socioeconomic, physical, and social environments. Significant racial/ethnic differences were present for all indicators of ideal CVH (excluding physical activity). Additional adjustments for neighborhood factors produced modest reductions in racial/ethnic differences. Future research is necessary to better understand the impact of neighborhood context on health disparities using longitudinal study designs.
Keywords: Racial/ethnic health disparities, neighborhood environments, cardiovascular health
INTRODUCTION
Persistent and pervasive racial/ethnic differences in health are a major public health concern (Institute of Medicine (US) Commitee on the Review and Assessment of the NIH's Strategic Research Plan and Budget to Reduce and Ultimately Eliminate Health Disparities, 2006; Kelley et al., 2005; Smedley et al., 2003). Racial/ethnic differences in the prevalence of cardiovascular disease (CVD) risk factors and incidence of and mortality due to cardiovascular diseases have been well documented, with blacks disproportionately burdened by adverse outcomes (Go et al., 2014; Mensah et al., 2005). Underlying causes of these differences remain poorly understood, but are most likely generated by multifactorial and multilevel causes that occur over the life-course. Much of the extant literature has focused on individual-level risk factors as explanations for racial/ethnic disparities (genetic, biological, socioeconomic, and psychosocial) (Kramer et al., 2004; Mensah and Dunbar, 2006; Safford et al., 2012). However, more attention has recently been placed on contextual factors such as neighborhood environments.
The increased interest in the intersection of race/ethnicity, neighborhood, and health has emerged in part from the increasing interest in the effects of neighborhoods on health generally. Studies have shown that living in socioeconomically disadvantaged neighborhoods is associated with increased morbidity and mortality, independent of individual-level factors (Borrell et al., 2004; Pickett and Pearl, 2001; Truong and Ma, 2006), and some of the most consistent evidence is from the area of cardiovascular disease (CVD) outcomes. (Borrell et al., 2004; Chaix, 2009; Diez Roux, 2003; Morenoff et al., 2007; Mujahid et al., 2011; Pickett and Pearl, 2001). In the area of CVD, studies have also shown that living in neighborhoods with poor physical environments (e.g. more unhealthy foods on average and fewer opportunities for physical activity) and social environments (e.g. less safety and social cohesion) are associated with increased risk of CVD risk factors such as obesity, diabetes, and hypertension, and fatal and non-fatal CVD (Christine et al., 2015; Diez Roux et al., 2016; Kaiser et al., 2016; Kershaw et al., 2015). Studies have also documented that blacks and other racial/ethnic minorities disproportionately reside in neighborhoods that are socioeconomically disadvantaged, and have poor access to health promoting resources. Combined, the aforementioned supports the hypothesis that neighborhood environments may be one underlying cause of racial/ethnic disparities in health. However, there is little empiric investigation explicitly testing this notion (Do et al., 2007; Dubowitz et al., 2008b; Morenoff et al., 2007; Mujahid et al., 2011; Robert and Reither, 2004).
Studies that have empirically investigated the contribution of neighborhood environments to racial/ethnic differences in health have most consistently examined estimates of differences before and after adjustment for neighborhood environments in a multivariable regression model without an explicit discussion of the major challenges and limitations in this approach (Do et al., 2007; Dubowitz et al., 2008b; Mujahid et al., 2011; Robert and Reither, 2004). These challenges include how best to: deal with the non-independence of observations within neighborhoods (Hubbard et al., 2010; Subramanian and O'Malley, 2010), account for the neighborhood context when all relevant factors may not be measured in a given study, and account for insufficient within-neighborhood sample size and variation in exposures and outcomes. A recent review by Schempf et al. (Schempf and Kaufman, 2012) provides an in-depth discussion of these issues, a comparison of analytic approaches that may address these issues, and compares the strengths and limitations of each analytic approach. Studies providing similar comparisons across analytic approaches remain scarce in the literature. (Morenoff et al., 2007; Schempf and Kaufman, 2012).
Given the increased attention to and importance of primordial prevention, as underscored by the recent American Heart Association 2020 Strategic Impact Goals to reduce cardiovascular mortality by 20% and increase ideal cardiovascular health by 20% (Lloyd-Jones et al., 2010), exploring the contribution of neighborhood environments to racial/ethnic differences in CVD risk in a multi-ethnic study is timely (Havranek et al., 2015). Thus, the overall goal of this study was to determine if cross-sectional racial/ethnic differences in ideal cardiovascular health (CVH) indicators were reduced after adjustment for neighborhood environments, and if results were robust to statistical methods of neighborhood adjustment.
METHODS
Study population
MESA is a prospective study of 6,814 adults of diverse racial/ethnic backgrounds (self-identified race/ethnicity as non-Hispanic white, non-Hispanic black, Hispanic, and non-Hispanic Chinese) from six study sites (Los Angeles County, California; Chicago, Illinois; Baltimore City and County, Maryland; St. Paul, Minnesota; Forsyth County, North Carolina; New York City, New York) (Bild et al., 2002). Study participants were 45–84 years of age and free from clinical cardiovascular disease at baseline (August 2000 to July 2002). A detailed description of the study recruitment procedures and methods has been previously described (Bild et al., 2002).
Our cross-sectional analyses are restricted to the MESA participants who provided consent to participate in the ancillary MESA Neighborhood Study (N=6191). Institutional review board approval was received at each of the MESA study sites.
Study variables
Study outcomes
We examined seven indicators of ideal CVH as defined by the American Heart Association 2020 Impact Goals (Lloyd-Jones et al., 2010) using either study questionnaire or clinical examination at baseline (2000–2002). Each indicator was categorized as poor, intermediate, and ideal based on established criteria and are defined in Table 1 (Lloyd-Jones et al., 2010). Cholesterol and fasting blood glucose were measured from a 75mL fasting blood sample obtained at the baseline clinical examination. Blood pressure (BP) was measured as the average of the second and third readings after five minutes resting in a seated position. BMI was assessed using measurements of height and weight obtained during clinical examination (BMI=height, m/weight, kg2). Smoking was based on self-reported data from study questionnaires and combined questions on whether a participant smoked in the past 30 days and the lifetime number of cigarettes smoked to create categories of never, current, and former smoking. We estimated minutes of moderate and vigorous exercise from walking, conditioning, and leisure-time activities based on participant’s assessment of the time and frequency spent on activities during a typical week in the past month (Ainsworth et al., 1999; Bertoni et al., 2009). We estimated five components of healthy diet using a 120-item food frequency questionnaire (Block et al., 1990), including high intake of healthy foods (fruits and vegetables; fish; whole grains) and low intake of unhealthy foods/nutrients (sugar sweetened beverages; sodium) similar to prior studies (Lloyd-Jones et al., 2010; Rasmussen-Torvik et al., 2013).
Table 1.
Indicators of Ideal Cardiovascular Health and Prevalence in Study Population
| Component | Score | Definition | % of MESA Participants (N=5263) |
|---|---|---|---|
| Cholesterol | |||
|
| |||
| Poor | ≥ 240 mg/dL | 9.6 | |
| Intermediate | 200–239 mg/dL or treated to < 200 mg/dL | 32.6 | |
| Ideal | <200 mg/dL, unmedicated | 57.8 | |
| Glucose | |||
| Poor | ≥ 126 mg/dL fasting | 10.1 | |
| Intermediate | 100–125 mg/dl fasting unmedicated or treated to <100mg/dL | 29.7 | |
| Ideal | <100mg/dL fasting, unmedicated | 60.2 | |
| BP | |||
| Poor | SBP ≥ 140 mmHg or DBP ≥ 90 mmHg | 23.5 | |
| Intermediate | SBP 120–139 mmHg or DBP 80–89 mmHg | 34.5 | |
| Ideal | SBP < 120 mmHg and DBP < 80 mmHg | 42.0 | |
| BMI | |||
| Poor | ≥ 30 kg/m^2 | 35.5 | |
| Intermediate | 25 – 29.9 kg/m^2 | 40.4 | |
| Ideal | < 25 kg/m^2 | 24.1 | |
| Physical Activity | |||
| Poor | no exercise | 21.8 | |
| Intermediate | 1–149 minutes of moderate or 1–74 minutes of vigorous exercise/week | 17.2 | |
| Ideal | 150+ minutes of moderate or 75+ minutes of vigorous exercise/week | 61.0 | |
| Smoking | |||
| Poor | Current Smoker | 13.5 | |
| Intermediate | Former Smoker, quit ≤ 12 months ago | 1.4 | |
| Ideal | Never Smoker or quit > 12 months ago | 85.1 | |
| Diet | |||
| Poor | 0–1 components of healthy diet | 47.7 | |
| Intermediate | 2–3 components of healthy diet | 51.2 | |
| Ideal | 4–5 components of healthy diet | 1.1 | |
We also created three summary measures of ideal CVH as the sum of each individual component score for health behaviors, health factors, and overall cardiovascular health. For the overall CVH measure, which ranged in value between 0 and 14, we created three categories based on the distribution of the data: poor (score of 0–8); intermediate (score of 9–10); and ideal (score of 11–14). In analyses we consider the 7 indicators of ideal CVH and 3 summary measures as dichotomous variables (1=ideal; 0=intermediate/poor).
Key covariates of interest
Neighborhood-level covariates
Neighborhoods were defined as census tracts based on previous work indicating good agreement across individuals residing within the same tract in relation to our neighborhood characteristics of interest (Mujahid et al., 2007). Three neighborhood-level socioeconomic indicators were derived from the 2000 U.S. Census based on methods previously described (Mujahid et al., 2008). The indicators combine 16 variables representing the dimensions of family structure, area crowding, residential stability, education, employment, occupation, and income/wealth) based on a principle components analysis with varimax orthogonal rotation to reduce the potential for multicollinearity in analytic models. The three factors account for 70 % of the total variance.
We calculated two physical environment indicators to represent physical activity and healthy food environment. Using data from the National Establishment Time Series Data (NETS) (Walls & Associates, 2012), we calculated kernel densities of all indoor and outdoor recreational facilities (excluding parks) around MESA participants’ home addresses at baseline year of enrollment. Facilities were defined using established Standardized Industrial Codes (SIC) based on prior work (Gordon-Larsen et al., 2006; Powell et al., 2007). We supplemented kernel densities with resident reports of the physical activity environment. MESA participants and an informant sample of non-MESA area residents were asked four items on whether or not their neighborhood (defined as the area within about a 20 minute walk or 1 mile from the home) was conducive to physical activity (Echeverria et al., 2004; Mujahid et al., 2007). We averaged across these items to create an overall score (Cronbach’s alpha=0.65). The kernel density and survey measure of physical activity environment were each standardized and aggregated to create an overall physical activity indicator for which higher scores represent a better physical activity environment. We used a similar process to create an overall indicator of neighborhood healthy foods (Auchincloss et al., 2012). Neighborhood social environment was characterized using survey items assessing neighborhood aesthetic quality (n=3 items), safety (n=2 items), and social cohesion (n=4 items). These items were shown to have good measurement properties based on prior work (Cronbach’s alpha=0.86) (Mujahid et al., 2011; Mujahid et al., 2008). We created an overall measure by aggregating responses across these items and empirical Bayes estimation techniques as previously described (Mujahid et al., 2008).
Individual-level covariates
All additional study covariates were collected during the baseline questionnaire (2000–2002). Self-reported race/ethnicity was categorized as white, non-Hispanic, black, non-Hispanic, Hispanic. Chinese were excluded due to limited sample size and limited geographic coverage across study sites. Additional covariates obtained from the study questionnaire included study site, age (continuous), sex (male, female), education (less than a high school diploma; high school diploma; some college; college graduate and beyond), and family income (less than $24,999; $25,000–$49,999; $50,000–$74,999; $75,000 or more).
Analysis plan and methods
All analyses were performed using Stata version 12. In descriptive analyses, we examined bivariate associations between each of the three summary measures of ideal CVH and study covariates. To examine the contribution of neighborhood context to racial/ethnic differences in CVH, we contrasted race coefficients in a neighborhood unadjusted logistic model (Model 1 below) to race coefficients from a series of models (models 2–4 below) that adjusted for neighborhood context in various ways (Morenoff et al., 2007; Schempf and Kaufman, 2012).
Model 1: Neighborhood unadjusted
Where logit(Yi) is the log odds of person i having ideal levels of the cardiovascular health, β1, and β2 are coefficients on binary indicator variables for black and Hispanic race/ethnicity respectively, and βk are the coefficients for the Xkis, a vector of individual-level covariates. In this model, we estimated racial/ethnic differences in ideal cardiovascular health, independent of only individual-level confounders (study site, gender, race/ethnicity, age, education, income). There is no adjustment for neighborhood-level factors and thus, we refer to this model as a neighborhood unadjusted model. Because neighborhood-level factors were unaccounted for in these models, it is considered a naïve model representing initial estimates of black-white differences in ideal cardiovascular health when neighborhood context is not taken into account.
Model 2: Fixed Effects
Where, logit(Yij) is the log odds of the ith person in the jth neighborhood having ideal levels of cardiovascular health, β0, β1, β2, βk, and Xkij have the same specifications as Model 1, and γl is a vector of n-1 coefficients, each corresponding to an indicator variable for each of the n-1 neighborhoods (Neighborhoodij = 1 if person i lives in the jth neighborhood, and is 0 otherwise). In this model we estimated racial/ethnic differences in the odds of ideal cardiovascular health, adjusted for individual-level covariates. This model is often considered the gold standard for accounting for group-level factors as it provides a summary of all measured and unmeasured group-level covariates. By controlling for all known and unknown characteristics of neighborhood environments, estimates of racial/ethnic differences represent the “weighted” average of within-neighborhood race/ethnic differences. However, there are also several limitations that warrant mention. First, this approach requires sufficient within-neighborhood sample size to ensure variation in study outcomes. For example, any neighborhood that does not have at least one participant with ideal levels of CVH and at least one participant without ideal levels of CVH is dropped from this analysis. This limitation is of particular concern given the levels of racial residential segregation that exists within the U.S. (Williams and Collins, 2001). A second limitation is when using this approach, one cannot estimate the specific features of neighborhoods that may account for reductions in racial/ethnic differences: the model represents all of the neighborhood features, both measured and unmeasured, by an indicator variable. As a result of this, there is also no way to examine potential interactions between neighborhood-level factors and other individual-level factors. A final limitation is the potential loss of statistical efficiency due to loss in degrees of freedom when there are a large number of clusters or limited within-cluster variation (Schempf and Kaufman, 2012).
Model 3: Random Effects (intercept)
Where logit(Yij) is the log odds of ideal cardiovascular health for the ith person in the jth neighborhood, β0j is the intercept for each neighborhood j, β1 and β2 are coefficients on indicator variables for black and Hispanic race/ethnicity for the ith person in the jth neighborhood, βk are coefficients on Xkij , a vector of individual-level covariates, and γl are coefficients on Wlj, a vector of neighborhood-level covariates (neighborhood physical, social, and socioeconomic indicators). The intercept β0j, is modeled as a random variable for each neighborhood j, where γ00 is the average log odds of ideal cardiovascular health averaged across all neighborhoods and μ0j is the deviation from the average log odds of ideal cardiovascular health for each neighborhood j and is assumed to have a normal distribution. The random effects or multi-level model has a number of benefits. Primarily, the ability to adjust for neighborhood and individual level variables allows for an assessment of both individual and neighborhood level variation in the data. Also, the ability to evaluate whether racial disparities in ideal cardiovascular health vary across neighborhoods provides an opportunity to investigate cross-level interactions. However, a limitation of this approach is that it assumes that the exposure, in this case race/ethnicity, is not conditionally correlated with the neighborhood random effects (Schempf and Kaufman, 2012). This is an assumption that is difficult to empirically evaluate, but theoretically easy to violate given the degree of racial residential segregation in the U.S.
Model 4: Hybrid Fixed Effects (cluster mean adjustment)
Where logit(Yij) is the log odds of ideal cardiovascular health for the ith person in the jth neighborhood, β0j is the intercept for each neighborhood j, β1 and β2 are coefficients on indicator variables for black and Hispanic race/ethnicity for the ith person in the jth neighborhood, βk are coefficients on Xkij , a vector of individual-level covariates, and γl are coefficients on Wlj, a vector of neighborhood-level covariates (neighborhood physical, social, and socioeconomic indicators). The intercept β0j, is modeled as a random variable for each neighborhood j and is a function of the proportion of each racial/ethnic group in that specific neighborhood. Here, γ00 is the average log odds of ideal cardiovascular health averaged across all neighborhoods, and are the proportion of people in the jth neighborhood who are black or Hispanic respectively, βb1 -− βw1 is the difference between the between-neighborhood association and within-neighborhood association between the proportion black in a given neighborhood j and the neighborhood-specific intercept, and μ0j is an error term for each neighborhood j and is assumed to have a normal distribution with variance .
Using a hybrid fixed effects model allows for a slightly different interpretation of coefficients in the logistic regression model because it accounts for between-neighborhood variation in race/ethnicity that contributes to neighborhood-level confounding. Here, the estimated coefficients on the race/ethnicity variables, βw1 and βw2 can be interpreted as the difference in ideal CVH between black and white (or Hispanic and white) people, holding the distribution of race/ethnicity (proportion black and proportion Hispanic) in the neighborhood constant (and holding the individual (Xk)- and neighborhood (Wl)- level confounders constant). Hybrid fixed effects models combine the strengths of the fixed effects and random effects models. The benefit from FE of being able to calculate marginal effects transfers to this model, but here we are able to make that estimate without ignoring all between-neighborhood variation, which is an advantage of using a RE model (Desai and Begg, 2008; Rabe-Hesketh and Skrondal, 2008; Schempf and Kaufman, 2012).
For all aforementioned models, we examined correlations among neighborhood features and assessed multicollinearity. There were modest to strong correlations between neighborhood indicators. The strongest correlations were for social environment and socioeconomic environment (r=−.78), physical activity and food environment (r=0.73), and physical activity and socioeconomic environment (r=−0.65). However, after assessing the variance inflation factors (all values less than 5) and tolerance (all values greater than .10) no violations of multicollinearity were found. For ease of interpretation and a useful way of comparing changes in model estimates of race/ethnic differences in ideal CVH across our models, we calculated the largest percent reduction as the change in estimates between Model 1, the model unadjusted for neighborhoods, compared to whichever Model 2–4 that resulted in the largest decrease in estimate based on the formula below where βu is the estimate from Model 1, and β* is the estimate from one of Models 2–4.
RESULTS
Among the 6191 MESA Neighborhood participants that provided consent to participate in the MESA Neighborhood Study, we excluded 728 Chinese participants for whom sample sizes were too small to examine neighborhood context. Additional exclusions included address errors (N=133) and missing information on study covariates (N=67) for a final analytic sample of N=5,263 representing 1033 neighborhoods with an average of 5 study participants per neighborhood (range 1 to 250). Among this analytic sample, the mean age was 62.0 (SD= 10.1), 52.7% were female, 34.3% had less than a high school education, and 26.3% had a family income of less than $25,000 per year. Ideal cardiovascular health, experienced by 4.1% of our analytic sample, varied by age, education, income, study site, and all neighborhood measures (excluding one of three neighborhood SES factor scores). The prevalence of ideal CVH decreased with age and was highest among those with the highest levels of education and family income (at least a college bachelor’s degree/earning ≥$75,000). As seen in previous studies (Unger et al., 2014), ideal CVH increases with increasing neighborhood physical, social, and socioeconomic environments (Table 2).
Table 2.
Distribution of Study Covariates Overall and by Ideal Cardiovascular Health
| Overall (N = 5263) | Poor (N = 3006) | Intermediate (N = 2042) | Ideal (N = 215) | P- value | |
|---|---|---|---|---|---|
| Individual-level Covariates | |||||
|
| |||||
| Age, mean (SD) | 62.0 (10.1) | 62.8 (9.8) | 61.2 (10.4) | 58.6 (10.0) | <0.001 |
| Gender, n (%) | 0.164 | ||||
| Male | 2491 (47.3) | 1442 (48.0) | 960 (47.0) | 89 (41.4) | |
| Female | 2772 (52.7) | 1564 (52.0) | 1082 (53.0) | 126 (58.6) | |
| Education, n (%) | <0.001 | ||||
| Completed high school/GED or less | 1807 (34.3) | 1244 (41.4) | 527 (25.8) | 36 (16.7) | |
| Some college/technical school/associate degree | 1563 (29.7) | 925 (30.8) | 592 (29.0) | 46 (21.4) | |
| Bachelor’s/graduate degree | 1893 (36.0) | 837 (27.8) | 923 (45.2) | 133 (61.9) | |
| Income, US $, n (%) | <0.001 | ||||
| <24,999 | 1383 (26.3) | 943 (31.4) | 414 (20.3) | 26 (12.1) | |
| 25,000–49,999 | 1530 (29.1) | 903 (30.0) | 564 (27.6) | 63 (29.3) | |
| 50,000–74,999 | 1417 (27.0) | 727 (24.2) | 626 (30.7) | 64 (29.8) | |
| ≥75,000 | 739 (14.0) | 296 (9.9) | 383 (18.8) | 60 (27.9) | |
| Missing | 194 (3.7) | 137 (4.6) | 55 (2.7) | 2 (0.9) | |
| Study Site, n (%) | <0.001 | ||||
| North Carolina (WFU) | 942 (17.9) | 556 (18.5) | 349 (17.1) | 37 (17.2) | |
| New York City, NY (Columbia) | 971 (18.5) | 530 (17.6) | 392 (19.2) | 49 (22.8) | |
| Baltimore, MD (Johns Hopkins) | 930 (17.7) | 558 (18.6) | 343 (16.8) | 29 (13.5) | |
| Minneapolis, MN (UMN) | 957 (18.2) | 549 (18.3) | 371 (18.2) | 37 (17.2) | |
| Chicago, IL (Northwestern) | 775 (14.7) | 358 (11.9) | 370 (18.1) | 47 (21.9) | |
| Los Angeles, CA (UCLA) | 688 (13.1) | 455 (15.1) | 217 (10.6) | 16 (7.4) | |
| Neighborhood-level Covariates | |||||
| Socioeconomic Environment, mean (SD) | |||||
| Factor 1 | −.1 (6.7) | 0.9 (6.2) | −.3 (7.0) | −3.4 (7.4) | <0.001 |
| Factor 2 | 1.9 (4.5) | 2.0 (4.6) | 1.8 (4.4) | 1.9 (4.4) | 0.155 |
| Factor 3 | −0.4 (1.0) | −0.3 (1.0) | −0.4 (1.0) | −0.5 (0.9) | <0.001 |
| Physical Environment, mean (SD) | |||||
| Health foods | −0.2 (1.7) | −0.4 (1.7) | −0.1 (1.9) | 0.2 (2.0) | <0.001 |
| Physical activity | −0.1 (1.7) | −0.3 (1.5) | 0.2 (1.9) | 0.7 (2.2) | <0.001 |
| Social Environment, mean (SD) | −0.1 (2.8) | −0.3 (2.8) | 0.0 (2.8) | 0.2 (2.9) | <0.001 |
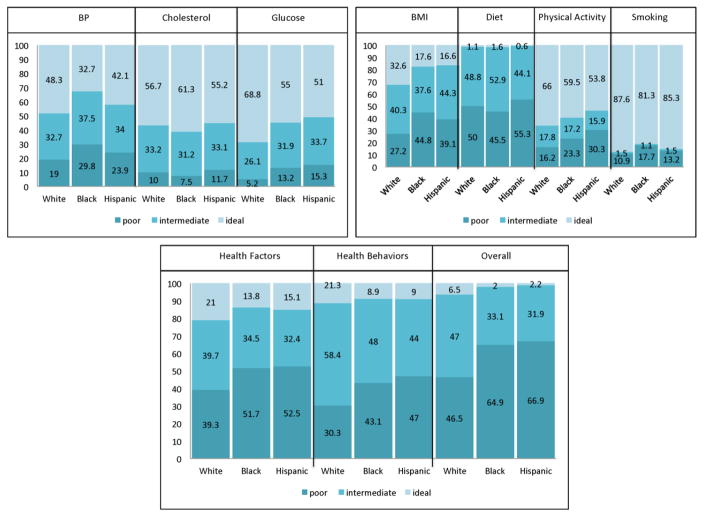
Figure 1 shows racial/ethnic differences in ideal cardiovascular health indicators. Significant differences were present for all components and summary measures (all p’s ≤ 0.01). Blacks had the lowest prevalence of ideal blood pressure and smoking, but highest prevalence of ideal cholesterol. Hispanics had the lowest prevalence of ideal BMI, glucose, physical activity, and diet. Blacks had the lowest prevalence of all summary measures (ideal health factors, health behaviors, and overall cardiovascular health).
Figure 1.
Race/Ethnic Differences in Indicators of Ideal Cardiovascular Health
Table 3 shows the odds ratios in ideal cardiovascular health factors comparing blacks and whites and Hispanics and whites. In initial models, the one-level logistic regression models, blacks as compared to whites were less likely to have ideal blood pressure (OR=0.510, 95% C.I.: 0.438–0.594) and fasting blood glucose (OR=0.581, 95% C.I.: 0.502, 0.673), independent of age, study site, gender, education, and family income. Adjustment for neighborhood-level factors resulted in a 21.45% and 16.2% reduction in black-white differences respectively. Similar patterns were documented in Hispanic-white differences in blood pressure (OR=0.600, 95% C.I.: 0.498, 0.724) and fasting blood glucose (OR=0.542, 95% C.I.: 0.450, 0.652) with 10.5% and 26.0% reductions. For cholesterol, blacks (OR=1.236; 95% C.I. 1.066–1.419) had a higher odds of ideal cholesterol levels compared to whites, independent of age, study site, gender, education, and family income. There were no significant Hispanic-white differences in ideal cholesterol.
Table 3.
Adjusted Racial/Ethnic Differences in Ideal Cardiovascular Health Factors (N=5263)
| Blood Pressurea | Cholesterola | Glucosea | |
|---|---|---|---|
|
| |||
| OR [95% C.I.] | OR [95% C.I.] | OR [95% C.I.] | |
| Black-white | |||
| Unadjustedc | 0.510 [0.438–0.594] † | 1.230 [1.066–1.419] † | 0.581 [0.502–0.673] † |
| Fixed Effectc,d | 0.597 [0.470–0.759] † | 1.248 [0.993–1.568] | 0.614 [0.485–0.777] † |
| Random Effectc,e | 0.545 [0.462, 0.642] † | 1.200 [1.028–1.401] † | 0.605 [0.514–0.713] † |
| Hybrid Fixed Effectc,f | 0.615 [0.490, 0.772] † | 1.211 [0.977–1.502] | 0.649 [0.521–0.808] † |
| Largest % change | 21.4% | N/A | 16.2% |
| Hispanic-white | |||
| Unadjustedc | 0.600 [0.498–0.724] † | 1.127 [0.943–1.348] | 0.542 [0.450–0.652] † |
| Fixed Effectc,d | 0.614 [0.470–0.803] † | 1.206 [0.932–1.561] | 0.640 [0.491–0.835] † |
| Random Effectc,e | 0.625 [0.516–0.757] † | 1.107 [0.923–1.328] | 0.555 [0.456–0.676] † |
| Hybrid Fixed Effectc,f | 0.642 [0.500–0.823] † | 1.167 [0.919–1.482] | 0.661 [0.516–0.846] † |
| Largest % changeg | 10.5% | N/A | 26.0% |
| P-valueb | |||
| Unadjustedc | <0.001 | 0.017 | <0.001 |
| Fixed Effectc,d | <0.001 | 0.100 | <0.001 |
| Random Effectc,e | <0.001 | 0.066 | <0.001 |
| Hybrid Fixed Effectc,f | <0.001 | 0.149 | <0.001 |
Sample size for fixed effects model: N=4510 for blood pressure, N=4501 for Cholesterol, and N=4505 for glucose
P-value<0.05 for beta coefficient for black-white or Hispanic-white comparison and CVH indicator
Outcome compares ideal vs. intermediate/poor CVH
p-value for overall association between race/ethnicity and CVH indicator
All models include the following covariates: study site, gender, race/ethnicity, age, education, income
Fixed effects model includes: neighborhood tract identifier
Random effects model includes: neighborhood SES, neighborhood physical environment, neighborhood social environment
Hybrid fixed effects model includes: neighborhood SES, neighborhood physical environment, neighborhood social environment, neighborhood proportion black, neighborhood proportion Hispanic
N/A listed for largest percent change if estimate was in the unexpected direction or racial/ethnic differences were not statistically significant in unadjusted model
Racial/ethnic differences in ideal cardiovascular health behaviors are presented in Table 4. Blacks (OR=0.401, 95% C.I. 0.339–0.475) and Hispanics (OR=0.417, 95% C.I. 0.324–0.520) were less likely to have ideal levels of BMI compared to whites and ideal levels of diet (OR=0.446 for blacks; OR=0.349 for Hispanics), independent of gender, age, education, income, and study site. Adjustment for neighborhood context resulted in minimal reductions in estimates for BMI (largest percent reduction: 2.3% reduction for blacks; 13.2% reduction in whites). Blacks were also less likely to have ideal smoking levels as compared to whites, independent of individual-level covariates (OR=0.713, 95% C.I.: 0.584, 0.872) and differences were reduced after adjusting for neighborhood context (largest percent reduction 31.4%). Alternatively, Hispanics were more likely to have ideal levels of smoking compared to whites, independent of individual-level covariates. There were no significant racial/ethnic differences in physical activity, independent of individual-level variables.
Table 4.
Adjusted Racial/Ethnic Differences in Ideal Cardiovascular Health Behaviors
| BMIa | Smokinga | Physical Activitya | Dieta | |
|---|---|---|---|---|
|
| ||||
| OR [95% C.I.] | OR [95% C.I.] | OR [95% C.I.] | OR [95% C.I.] | |
| Black-white | ||||
|
| ||||
| Unadjustedc | 0.401 [0.339– 0.475] † | 0.713 [0.584– 0.872] † | 0.894 [0.773– 1.034] | 0.446 [0.229– 0.870] † |
| Fixed Effectc,d | 0.363 [0.276– 0.478] † | 0.704 [0.509– 0.974] † | 0.954 [0.758– 1.201] | 0.319 [0.098– 1.036] |
| Random Effectc,e | 0.415 [0.344– 0.501] † | 0.803 [0.639– 1.007] | 0.998 [0.849– 1.173] | 0.421 [0.198– 0.893] † |
| Hybrid Fixed Effectc,f | 0.412 [0.320– 0.531] † | 0.747 [0.551– 1.014] | 0.969 [0.778– 1.207] | 0.370 [0.133– 1.029] |
| Largest % changeg | 2.3% | 31.4% | N/A | N/A |
| Hispanic-white | ||||
| Unadjustedc | 0.417 [0.334– 0.520] † | 1.265 [0.985– 1.624] | 0.864 [0.720– 1.037] | 0.349 [0.136– 0.899] † |
| Fixed Effectc,d | 0.454 [0.327– 0.628] † | 1.188 [0.849– 1.679] | 0.910 [0.700– 1.183] | 0.211 [0.034– 1.310] |
| Random Effectc,e | 0.428 [0.340– 0.538] † | 1.322 [1.013– 1.724] † | 0.920 [0.759– 1.114] | 0.349 [0.129– 0.941] † |
| Hybrid Fixed Effectc,f | 0.494 [0.366– 0.666] † | 1.170 [0.844– 1.621] | 0.942 [0.737– 1.205] | 0.319 [0.088– 1.146] |
| Largest % changeg | 13.2% | N/A | N/A | N/A |
| P-valueb | ||||
| Unadjustedc | <0.001 | <0.001 | 0.172 | 0.017 |
| Fixed Effectc,d | <0.001 | 0.035 | 0.757 | 0.049 |
| Random Effectc,e | <0.001 | 0.002 | 0.657 | 0.030 |
| Hybrid Fixed Effectc,f | <0.001 | 0.058 | 0.881 | 0.068 |
Sample size for fixed effects model: N=3981 for BMI; N=3687 for smoking; N=4412 for physical activity; N=978 for diet
P-value<0.05 for beta coefficient for black-white or Hispanic-white comparison and CVH indicator
Outcome compares ideal vs. intermediate/poor CVH
p-value for overall association between race/ethnicity and CVH indicator
All models include the following covariates: study site, gender, race/ethnicity, age, education, income
Fixed effects model includes: neighborhood tract identifier
Random effects model includes: neighborhood SES, neighborhood physical environment, neighborhood social environment
Hybrid fixed effects model includes: neighborhood SES, neighborhood physical environment, neighborhood social environment, neighborhood proportion black, neighborhood proportion Hispanic
N/A listed for largest percent change if estimate was in the unexpected direction or racial/ethnic differences were not statistically significant in unadjusted models
In examining racial/ethnic differences in three cardiovascular summary measures, significant black-white differences and Hispanic-white differences were present for all measures (Table 5). Blacks and Hispanics were less likely to have ideal health factors (OR=0.613, 95% C.I.: 0.505, 0.744 for blacks; OR=0.680, 95% C.I. 0.536, 0.862) for Hispanics), health behaviors (OR=0.362, 95% C.I. 0.292, 0.448 for blacks; OR=0.441, 95% C.I.: 0.334, 0.581 for Hispanics) and overall cardiovascular health (OR=0.324, 95% C.I.: 0.216, 0.487 for blacks; OR=0.403, 95% C.I. 0.245, 0.664) as compared to whites, independent of individual-level covariates. Adjustment for neighborhood context slightly reduced these differences, although they remained statistically significant (largest percent reduction range: 5.6%–20.2% for blacks; 8.2%–28.1% for Hispanics).
Table 5.
Adjusted Racial/Ethnic Differences in Ideal Cardiovascular Health Summary Measures
| Health Factors | Health Behaviors | Overall Ideal CVH | |
|---|---|---|---|
|
| |||
| OR [95% C.I.] | OR [95% C.I.] | OR [95% C.I.] | |
| Black-white | |||
|
| |||
| Unadjustedc | 0.613 [0.505– 0.744] † | 0.362 [0.292– 0.448] † | 0.324 [0.216– 0.487] † |
| Fixed Effectc,d | 0.691 [0.509– 0.939] † | 0.333 [0.234– 0.473] † | 0.419 [0.221– 0.797] † |
| Random Effectc,e | 0.622 [0.504– 0.766] † | 0.398 [0.313– 0.505] † | 0.349 [0.223– 0.548] † |
| Hybrid Fixed Effectc,f | 0.689 [0.516– 0.919] † | 0.387 [0.282– 0.533] † | 0.456 [0.256– 0.812] † |
| Largest % changeg | 20.2% | 5.6% | 19.5% |
| Hispanic-white | |||
| Unadjustedc | 0.680 [0.536– 0.862] † | 0.441 [0.334– 0.581] † | 0.403 [0.245– 0.664] † |
| Fixed Effectc,d | 0.770 [0.552– 1.075] | 0.435 [0.284– 0.668] † | 0.422 [0.205– 0.870] † |
| Random Effectc,e | 0.681 [0.535– 0.868] † | 0.477 [0.358– 0.636] † | 0.430 [0.257– 0.718] † |
| Hybrid Fixed Effectc,f | 0.765 [0.561– 1.044] | 0.527 [0.362– 0.769] † | 0.452 [0.236– 0.867] † |
| Largest % change | 28.1% | 15.4% | 8.2% |
| P-valueb | |||
| Unadjustedc | <0.001 | <0.001 | <0.001 |
| Fixed Effectc,d | 0.035 | <0.001 | 0.003 |
| Random Effectc,e | <0.001 | <0.001 | <0.001 |
| Hybrid Fixed Effectc,f | 0.021 | <0.001 | 0.004 |
P-value<0.05 for beta coefficient for black-white or Hispanic-white comparison and CVH indicator
Outcome compares ideal vs. intermediate/poor CVH
p-value for overall association between race/ethnicity and CVH indicator
All models include the following covariates: study site, gender, race/ethnicity, age, education, income
Fixed effects model includes: neighborhood tract identifier
Random effects model includes: neighborhood SES, neighborhood physical environment, neighborhood social environment
Hybrid fixed effects model includes: neighborhood SES, neighborhood physical environment, neighborhood social environment, neighborhood proportion black, neighborhood proportion Hispanic
In comparing the methods of adjusting for neighborhood context across models: fixed effect, random effects, and hybrid fixed effects models, the largest percent reduction was most consistently found with the hybrid fixed effect approach. The fixed effects model appears to be the least stable as some estimates of racial/ethnic differences were increased instead of decreased after adjustment for neighborhood-level factors. However, given the relatively modest differences in estimates across the three modeling approaches, our results were robust.
DISCUSSION
In a multi-ethnic cohort of middle-aged adults, we found significant black-white and Hispanic-white differences for all ideal health factors (blood pressure, cholesterol, and glucose), three of four ideal health behaviors (diet, body mass index, and smoking) and all ideal CVH summary measures (health factors, health behaviors, and overall ideal cardiovascular health), independent of sociodemographic characteristics. Adjustment for neighborhood context slightly reduced racial/ethnic differences, but differences remained statistically significant. Percent reductions in racial/ethnic differences ranged from 2.3% to 31.4%.
To our knowledge, we are the first study to examine the contribution of neighborhood environments to racial/ethnic disparities in a comprehensive set of CVD risk factors. There have been a few studies that examine neighborhood context in relation to racial/ethnic differences in specific CVD risk factors. For example, Morenoff et al. (Morenoff et al., 2007), found that black-white differences in hypertension were reduced by 100% and no longer statistically significant after controlling for neighborhood factors using fixed effects and random effects modeling approaches. Mujahid et al. (Mujahid et al., 2011), used MESA data (based on a subset of participants within 3 of 6 sites) to document an age and sex adjusted higher prevalence of hypertension in blacks and Hispanics compared to whites, and a 43% reduction after adjustment for neighborhood social environment indicators (neighborhood social cohesion, social disorder, and safety). In our analyses, we only found 21% reductions in black-white differences in blood pressure and 11% reductions in Hispanic-white differences and significant racial/ethnic differences in our study outcomes remained after adjustment for neighborhood context. Aside from a handful of studies that have examined the contribution of neighborhood context to racial/ethnic differences in obesity (Nicholson and Browning, 2012) and fruit and vegetable intake (Dubowitz et al., 2008a), this area remains under-investigated. Results across these different studies are not directly comparable due to differences in study population characteristics and differences in covariate adjustments. However, the range of reductions in racial/ethnic differences across studies should spur continued investigation into the effects of neighborhoods on racial/ethnic disparities in CVH.
In this study, we also examined whether reductions in racial/ethnic differences in ideal cardiovascular health indicators were robust across three modeling approaches. We compared results of fixed effects, random effects, and hybrid fixed effects models and found that the largest percent reduction was observed most consistently from the hybrid fixed effects approach. The fixed effects model, often considered the gold standard as the most conservative approach, adjusts for all measured and unmeasured neighborhood characteristics related to the study outcomes. However, this approach does not allow one to consider specific neighborhood characteristics that may contribute to the racial/ethnic differences. In our analyses, the fixed effects approach often led to very mild decreases or slight increases in racial/ethnic differences across study outcomes. As an example, blacks had a 60% lower odds of ideal BMI compared to whites in initial models unadjusted for neighborhood context (OR=0.401; 95% C.I. 0.339–0.475) and these differences increased using fixed effects adjustments (OR=0.363, 95% C.I. 0.276–0.478). Our ability to maximize the fixed effects modeling approach may have been compromised by having a limited number of individuals within neighborhoods and retaining only neighborhoods with at least two of the three racial/ethnic groups being compared in analyses. For example, we lost over half of our analytic sample in analyses of overall ideal CVH as there was not at least one white and either black or Hispanic participant with ideal levels of CVH in many neighborhoods. Alternatively, the random effects and hybrid fixed effects model allows for adjustment of neighborhood factors and inclusion of six neighborhood characteristics across socioeconomic, physical and social environments. These models produced larger reductions in racial/ethnic differences particularly in the case of the hybrid fixed effects models. However, reductions were still modest as none of these models fully attenuated results or reduced racial/ethnic differences to being non-statistically significant. Moreover, both the random and hybrid effects approaches have limitations. The random effects model assumes that race/ethnicity is conditionally uncorrelated with the neighborhood random effects, an assumption difficult to verify. Future research is necessary to compare these models and to identify the ideal circumstances to increase the performance of each model.
Strengths of this study include the use of the MESA study, which provides a racially and ethnically diverse set of individuals and information on a rich set of cardiovascular health indicators and indicators of neighborhood physical, social, and socioeconomic environments to allow for investigations of our research question. However, a few limitations of our study warrant consideration. First, although we had a multi-ethnic cohort, not all racial/ethnic groups are represented across study sites. White participants were the only group recruited across all study sites. Blacks were recruited from all sites except St. Paul, MN, and Hispanics were recruited from 3 of 6 sites, (New York, NY; Los Angeles CA; St. Paul, MN). Moreover, we had to exclude Chinese Americans from analyses due to limited sample sizes. Limited diversity across sites and the fact that MESA participants are free from CVD at baseline means that we may have an underestimate of the underlying racial/ethnic differences in the target populations.
There are also several limitations in relation to the neighborhood-level component of our study. Although we included a comprehensive set of neighborhood physical, social, and socioeconomic indicators, we defined neighborhoods as census tracts, and there is debate as to whether these geographic boundaries represent meaningful areas for residents or represent the relevant spatial scale for which processes related to neighborhoods conditions affect various health outcomes (Diez Roux, 2001; Diez Roux and Mair, 2010). Census tracts also vary substantially in spatial size depending on the population density of an area and more dense urban areas (e.g. New York, NY study site) will have smaller census tracts than less dense rural areas (e.g. Forsyth County, NC study site). Future work should consider whether associations vary by study site and whether results are robust to various specifications of neighborhood boundaries. Future work should also consider approaches to capture real-time place-based exposures as individuals move through space and time as well as the multiple spatial contexts individuals experience where they live, work, and play (Kestens et al., 2012; Moore et al., 2013; Zenk et al., 2011).
In this study, we used a variety of measurement tools to capture neighborhood environments including surveys of area residents, and linkages to geospatially referenced databases. Although we had an average of 5 respondents per neighborhood, the range was highly variable and some neighborhoods only included 1 individual. This may have led to bias in our survey-based responses as the reliability of aggregate neighborhood measures is sensitive to the within neighborhood sample size (Mujahid et al., 2007).
In our analyses we compared three statistical modeling approaches to account for neighborhood context, although the estimates across these models are not directly comparable given the assumptions underlying each model. We reported odds ratios to try to improve comparisons across models and to better facilitate comparisons of our study findings to other previous studies. However, odds ratios provide an overestimate of racial/ethnic differences among the highly prevalent components of the ideal cardiovascular health metric (all health factors and health behaviors with the exception of diet). There may also be other analytic approaches such as marginal structural models, that better account for residential selection especially within the context of a longitudinal study design. Also, controlling for context at the design phase of the study may be a better approach to balance residential selection characteristics of study participants. For example, LaVeist and colleagues explored black-white health differences in the Exploring Health Disparities in Integrated Communities Study (EHDIC), which identified communities in the U.S. that are integrated (having at least 35% blacks and 35% whites living in the census tract), and have comparable socioeconomic status across racial groups (LaVeist et al., 2008). Using a nationally representative data source, they found blacks had higher odds of hypertension as compared to whites, independent of age, gender, marital status, household income, and education level (OR=2.07, 95% C.I. 1.79, 2.40). However, these differences were less pronounced in the integrated communities with the same covariate adjustment (OR=1.45, 95% C.I. 1.12, 1.88; 30% reduction in black-white difference). Similar findings were documented in relation to diabetes and obesity among women.
Racial/ethnic differences in health remain alarming and may result from more than just differences in individual factors. We show that above and beyond individual-level sociodemographic factors, neighborhood context may also contribute to these disparities. Healthy People 2020 emphasizes the importance of creating physical and social environments conducive to healthy lifestyles as having the greatest potential to improve the health of the nation. Our study findings underscore the importance of this overarching goal for racial/ethnic minorities. Future research using longitudinal and life-course study designs is necessary to accurately capture the cumulative burden of living in physically, socially, and economically disadvantaged neighborhoods on racial/ethnic disparities over the lifespan.
Supplementary Material
Highlights.
Whites were 3 times more likely to have ideal CVH compared to blacks and Hispanics.
Neighborhood adjustment resulted in modest reductions in racial/ethnic differences
Study results were generally robust across analytic approach
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ainsworth BE, Irwin ML, Addy CL, Whitt MC, Stolarczyk LM. Moderate physical activity patterns of minority women: the Cross-Cultural Activity Participation Study. J Womens Health Gend Based Med. 1999;8:805–813. doi: 10.1089/152460999319129. [DOI] [PubMed] [Google Scholar]
- Auchincloss AH, Moore KAB, Moore LV, Diez Roux AV. Improving retrospective characterization of the food environment for a large region in the United States during a historic time period. Health Place. 2012;18:1341–1347. doi: 10.1016/j.healthplace.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertoni AG, Whitt-Glover MC, Chung H, Le KY, Barr RG, Mahesh M, Jenny NS, Burke GL, Jacobs DR. The association between physical activity and subclinical atherosclerosis: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2009;169:444–454. doi: 10.1093/aje/kwn350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- Borrell LN, Diez Roux AV, Rose K, Catellier D, Clark BL. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol. 2004;33:398–407. doi: 10.1093/ije/dyh063. [DOI] [PubMed] [Google Scholar]
- Chaix B. Geographic life environments and coronary heart disease: a literature review, theoretical contributions, methodological updates, and a research agenda. Annu Rev Public Health. 2009;30:81–105. doi: 10.1146/annurev.publhealth.031308.100158. [DOI] [PubMed] [Google Scholar]
- Christine PJ, Auchincloss AH, Bertoni AG, Carnethon MR, Sanchez BN, Moore K, Adar SD, Horwich TB, Watson KE, Diez Roux AV. Longitudinal Associations Between Neighborhood Physical and Social Environments and Incident Type 2 Diabetes Mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA) JAMA Intern Med. 2015;175:1311–1320. doi: 10.1001/jamainternmed.2015.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai M, Begg MD. A comparison of regression approaches for analyzing clustered data. Am J Public Health. 2008;98:1425–1429. doi: 10.2105/AJPH.2006.108233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80:569–589. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Mujahid MS, Hirsch JA, Moore K, Moore LV. The Impact of Neighborhoods on CV Risk. Glob Heart. 2016;11:353–363. doi: 10.1016/j.gheart.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do DP, Dubowitz T, Bird CE, Lurie N, Escarce JJ, Finch BK. Neighborhood context and ethnicity differences in body mass index: a multilevel analysis using the NHANES III survey (1988–1994) Econ Hum Biol. 2007;5:179–203. doi: 10.1016/j.ehb.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz T, Heron M, Bird CE, Lurie N, Finch BK, Basurto-Dávila R, Hale L, Escarce JJ. Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and Mexican Americans in the United States. Am J Clin Nutr. 2008a;87:1883–1891. doi: 10.1093/ajcn/87.6.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz T, Subramanian SV, Acevedo-Garcia D, Osypuk TL, Peterson KE. Individual and neighborhood differences in diet among low-income foreign and U.S.-born women. Womens Health Issues. 2008b;18:181–190. doi: 10.1016/j.whi.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echeverria S, Diez-Roux A, Link B. Reliability of self-reported neighborhood characteristics. J Urban Health. 2004;81:682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the Built Environment Underlies Key Health Disparities in Physical Activity and Obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW American Heart Association Council on Quality of, C., Outcomes Research C.o.E., Prevention, C.o.C., Stroke Nursing, C.o.L, Cardiometabolic, H., Stroke C. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- Hubbard AE, Ahern J, Fleischer NL, Van der Laan M, Lippman SA, Jewell N, Bruckner T, Satariano WA. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21:467–474. doi: 10.1097/EDE.0b013e3181caeb90. [DOI] [PubMed] [Google Scholar]
- Thomsom G, Mitchell F, Williams M, editors. Institute of Medicine (US) Commitee on the Review and Assessment of the NIH's Strategic Research Plan and Budget to Reduce and Ultimately Eliminate Health Disparities. Examining the health disparities research plan of the National Institutes of Health: Unfinished business. The National Academies Press; Washington DC: 2006. [PubMed] [Google Scholar]
- Kaiser P, Diez Roux AV, Mujahid M, Carnethon M, Bertoni A, Adar SD, Shea S, McClelland R, Lisabeth L. Neighborhood Environments and Incident Hypertension in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2016;183:988–997. doi: 10.1093/aje/kwv296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley E, Moy E, Stryer D, Burstin H, Clancy C. The national healthcare quality and disparities reports: an overview. Med Care. 2005;43:I3–I8. doi: 10.1097/00005650-200503001-00002. [DOI] [PubMed] [Google Scholar]
- Kershaw KN, Diez Roux AV, Bertoni A, Carnethon MR, Everson-Rose SA, Liu K. Associations of chronic individual-level and neighbourhood-level stressors with incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis. J Epidemiol Community Health. 2015;69:136–141. doi: 10.1136/jech-2014-204217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kestens Y, Lebel A, Chaix B, Clary C, Daniel M, Pampalon R, Theriault M, SVPS Association between activity space exposure to food establishments and individual risk of overweight. PLoS One. 2012;7:e41418. doi: 10.1371/journal.pone.0041418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, Jinagouda S, Shea S. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA) Am J Hypertens. 2004;17:963–970. doi: 10.1016/j.amjhyper.2004.06.001. [DOI] [PubMed] [Google Scholar]
- LaVeist T, Thorpe R, Jr, Bowen-Reid T, Jackson J, Gary T, Gaskin D, Browne D. Exploring health disparities in integrated communities: overview of the EHDIC study. J Urban Health. 2008;85:11–21. doi: 10.1007/s11524-007-9226-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD American Heart Association Strategic Planning Task, F., Statistics, C. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- Mensah GA, Dunbar SB. A framework for addressing disparities in cardiovascular health. J Cardiovasc Nurs. 2006;21:451–456. doi: 10.1097/00005082-200611000-00007. [DOI] [PubMed] [Google Scholar]
- Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- Moore K, Diez Roux AV, Auchincloss A, Evenson KR, Kaufman J, Mujahid M, Williams K. Home and work neighbourhood environments in relation to body mass index: the Multi-Ethnic Study of Atherosclerosis (MESA) J Epidemiol Community Health. 2013;67:846–853. doi: 10.1136/jech-2013-202682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007;65:1853–1866. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence (the Multi-Ethnic Study of Atherosclerosis) Am J Hypertens. 2011;24:187–193. doi: 10.1038/ajh.2010.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165:858–867. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, Shea S. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–598. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- Nicholson LM, Browning CR. Racial and Ethnic Disparities in Obesity During the Transition to Adulthood: The Contingent and Nonlinear Impact of Neighborhood Disadvantage. Journal Youth Adolescence. 2012;41:53–66. doi: 10.1007/s10964-011-9685-z. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Chaloupka FJ, Slater SJ, Johnston LD, O’Malley PM. The Availability of Local-Area Commercial Physical Activity–Related Facilities and Physical Activity Among Adolescents. Am J Prev Med. 2007;33:S292–S300. doi: 10.1016/j.amepre.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. Stata Press; College Station, TX: 2008. [Google Scholar]
- Rasmussen-Torvik LJ, Shay CM, Abramson JG, Friedrich CA, Nettleton JA, Prizment AE, Folsom AR. Ideal cardiovascular health is inversely associated with incident cancer: the Atherosclerosis Risk In Communities study. Circulation. 2013;127:1270–1275. doi: 10.1161/CIRCULATIONAHA.112.001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert SA, Reither EN. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Soc Sci Med. 2004;59:2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, Shikany JM, Prineas RJ, Samdarshi T, Bittner VA, Lewis CE, Gamboa C, Cushman M, Howard V, Howard G Investigators R. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308:1768–1774. doi: 10.1001/jama.2012.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schempf AH, Kaufman JS. Accounting for context in studies of health inequalities: a review and comparison of analytic approaches. Ann Epidemiol. 2012;22:683–690. doi: 10.1016/j.annepidem.2012.06.105. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR Institute of Medicine (U.S.) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: confronting racial and ethnic disparities in health care. National Academy Press; Washington, D.C: 2003. [PubMed] [Google Scholar]
- Subramanian SV, O'Malley AJ. Modeling neighborhood effects: the futility of comparing mixed and marginal approaches. Epidemiology. 2010;21:475–478. doi: 10.1097/EDE.0b013e3181d74a71. discussion 479–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong KD, Ma S. A systematic review of relations between neighborhoods and mental health. J Ment Health Policy Econ. 2006;9:137–154. [PubMed] [Google Scholar]
- Unger E, Diez-Roux AV, Lloyd-Jones DM, Mujahid MS, Nettleton JA, Bertoni A, Badon SE, Ning H, Allen NB. Association of neighborhood characteristics with cardiovascular health in the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7:524–531. doi: 10.1161/CIRCOUTCOMES.113.000698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls & Associates. National Establishment Time-Series (NETS) Database: 2012 Database Description. Denver, CO: 2012. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Matthews SA, Odoms-Young A, Wilbur J, Wegrzyn L, Gibbs K, Braunschweig C, Stokes C. Activity space environment and dietary and physical activity behaviors: a pilot study. Health Place. 2011;17:1150–1161. doi: 10.1016/j.healthplace.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.