Abstract
VOICE — a phase 2B, placebo-controlled, randomized trial testing daily use of an antiretroviral tablet (tenofovir or Truvada) or daily use of tenofovir gel in 5029 women from South Africa, Uganda, and Zimbabwe — found none of the drug regimens effective in reducing HIV-1 acquisition in the intent-to-treat analysis. More than half of women assigned to active products in a case cohort sample had no drug detected in any plasma specimens tested during the trial. Yet, in response to questions asked of participants during the trial, ≥90% of doses were reportedly taken. To explore factors associated with low adherence, a behavioral termination visit questionnaire was developed after early closure of the oral tenofovir and vaginal gel arms. We hypothesized that participants would be more forthcoming about nonuse after they exited the trial than during monthly/quarterly follow-up visits. Comparison of adherence reporting at routine follow-up visits with reporting at trial termination, however, indicates that disclosure of product nonadherence did not increase at the termination visit as anticipated. In resource-limited settings where women value the ancillary benefits provided by trial participation and are concerned that disclosure of nonuse may jeopardize trial participation, objective measures of adherence may yield more meaningful data regarding the inability or reluctance to use than measures of product use derived from self-report.
Keywords: Microbicide trials, Self-reports of adherence, sub-Saharan Africa
Introduction
Given limited options for women to protect themselves against HIV, considerable effort has been made in developing and testing vaginal microbicides and oral antiretroviral agents for preexposure prophylaxis (PrEP). Despite the apparent demand for such products — at least based on acceptability research [1, 2] — a major challenge in microbicide and PrEP trials in sub-Saharan Africa has been achieving levels of product adherence high enough to confer protection [3, 4]. If trial participants are unable or unwilling to use the products being tested — whether due to particular attributes of the products or incompatibility with their daily routines — or if the motivation for trial participation does not include a desire to test an HIV prevention product, it is unlikely that intent-to-treat analyses will demonstrate effectiveness, even with efficacious products [5-7]. Results from the recent VOICE trial — a phase 2B, placebo-controlled, randomized study involving daily treatment with oral tenofovir disoproxil fumerate (TDF), oral tenofovir-emtricitabine (TDF-FTC) or 1% tenofovir (TFV) vaginal gel in 5029 women from South Africa, Uganda and Zimbabwe — found that none of the study products were effective in reducing HIV-1 acquisition in the intent-to-treat analysis. Among a case-cohort sample of 647 participants in the three active arms, TFV was detected in 29% of plasma samples from women assigned to the oral TDF-FTC arm, 30% of samples from women in the oral TDF arm and 25% of samples from women assigned to the TFV gel arm.
In VOICE, plasma TFV levels contrasted markedly with the behavioral measures of adherence conducted throughout the trial. These included self-report and counts of product returned at monthly study visits. Indeed, during the trial, participants overwhelmingly reported that they regularly used product, and few acknowledged that they were not adherent. In response to questions on product use in the prior week asked at monthly follow-up visits using face-to-face interviews, and then summed across these visits, the mean proportion of doses reported to be taken was 90%, with almost no variability by study arm. Reporting of adherence at the quarterly and annual visits via audio computer assisted self-interviewing (ACASI) was almost as high; 88% of doses were reportedly taken, despite evidence from prior microbicide studies, albeit not entirely consistent, that reporting of sensitive behaviors may be more accurate with ACASI [8, 9]. In addition, estimates of adherence based on unused product that participants were asked to return were similarly high with mean rate across study arms of 86% [10].
The VOICE trial is not alone in observing inflated estimates of product use based on self-reports. Methodological challenges to obtaining accurate measurement of adherence have been discussed extensively in the microbicide literature [11, 12] and in clinical trials of other therapeutics, particularly in healthy populations [13]. Given investigators' expectations that participants comply with protocols during a clinical trial, participants may be understandably disinclined to admit to study staff that they have not used the product as directed.
In the VOICE trial, the oral TDF and vaginal TFV gel arms were stopped early due to futility. We subsequently developed a behavioral exit questionnaire to explore factors associated with suboptimal adherence. The underlying hypothesis was that women might respond to questions about nonuse of product more candidly at a termination visit when exiting the trial and after product use had ended than they would during study participation. If women are disinclined to discuss nonuse of product and the circumstances surrounding unwillingness or inability to use while “on product”, but are more forthcoming after they have terminated use, then we can decrease participant and staff burden during follow-up visits by reducing or eliminating questions devoted to adherence. This analysis explores whether disclosure of product nonadherence was higher at the study termination visit than at routine follow-up visits during the trial.
Methods
Design and Administration of Termination Exit Visit Questionnaire
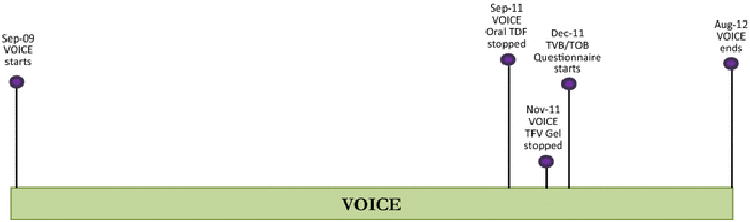
The VOICE trial [ClinicalTrials.gov identifier: NCT00705679], was conducted from 2009 to 2012 at 15 sites among 5029 women 18-45 years of age from Uganda, South Africa and Zimbabwe. The trial design, sample description, procedures, and primary findings are described elsewhere [10]. For the 2327 VOICE participants who were still enrolled in the trial in December 2011, representing nearly half (46.2%) of all participants, a Termination visit Vaginal or Oral product Behavioral questionnaire (TVB/TOB) was offered via face-to-face interview. Because we wanted to administer the form to as many VOICE participants as possible before they exited the trial, we did not pre-test the form. Figure 1 provides the trial timeline and indicates when the TVB/TOB was first administered.
Figure 1. VOICE Study Timeline.
The TVB/TOB was introduced to participants with the following statement emphasizing disclosure of nonuse:
Two of the VOICE products — the tenofovir tablets and the tenofovir gel —have been discontinued because the study did not show that they prevented HIV infection among VOICE women. One of the reasons for this finding may be that women did not use the study products on a daily basis. It is important for us to understand if women in VOICE did not use the products daily, and if so, why. We would like to learn from your experience while you were enrolled in the VOICE trial and we very much appreciate your honesty in answering these questions.
The TVB/TOB included 40 questions. In contrast to the quarterly and annual ACASI, which included a one-week retrospective calendar focusing on product use, and the monthly adherence and behavior assessment case report forms (CRFs), which asked questions about the number of days out of the past seven that the product was taken and not taken, the TVB/TOB did not include any adherence questions worded in terms of product use. Rather, it focused on nonuse of study product, specifically reasons, circumstances, and frequency of nonadherence, as well as when the participant started skipping doses. The first 21 questions included simple statements regarding reasons for nonuse that were to be answered by either “yes” or “no” including: “you forgot to insert the gel/take tablets every day,” “you didn't like inserting the gel/taking the tablets every day,” “you were not having sex”, “your sex partner did not want you to use the gel/tablets,” you travelled away from home” etc. Those who stated that they never missed inserting the gel/taking the tablets, were recorded as “not applicable, always inserted the gel/took the tablet.” These statements were then followed by two questions about frequency of missed or skipped days, “How often during the study did you miss or skip days?” and when this first occurred, “When during the study did you start skipping doses?” The final set of adherence assessments began with a question asking participants to rate their ability to take the product as directed, which was also included in the ACASI and quarterly adherence and behavioral assessment CRFs; prior research had found the self-rating scale to correlate well with HIV viral load and CD4 count in treatment studies [14, 15]. The TVB/TOB also included questions on motivation to take part in the trial and perception of HIV risk before and during the trial. Response options were not read to participants unless they requested clarification. Note, that while it is possible the early closure of arms affected the adherence among respondents still enrolled in the trial, it is not possible to determine whether that is the case because 1) other factors, in addition to early closure, could have affected adherence over time and 2) we did not specifically ask participants whether they were aware of the early closure during the trial and, if so, whether it affected their product use.
Adherence questions used in analysis
Table 1 lists the behavioral assessments conducted during VOICE and indicates those used in this paper. Table 2 lists the adherence questions in the TVB/TOB and the questions from the “Monthly Product Adherence and Behavior Assessment” (MBA) and quarterly “Oral and Vaginal Product Adherence and Behavior Assessments” (OPA/VPA) that are used in comparison. Note that we are not comparing TVB/TOB responses to questions about product use in the ACASI. As indicated above, self-reports of adherence in ACASI were nearly as inflated as the reports generated by the monthly and quarterly CRFs. Because the TVB/TOB was administered using a conventional face-to-face interview, it is more appropriate to compare reports from the TVB/TOB with reports from the monthly and quarterly CRFs focusing on nonuse, which were also administered face-to-face.
Table 1. Behavioral Assessments in VOICE.
| Assessment | When administered | Mode of administration | Used in analysis |
|---|---|---|---|
| Demographics | Screening | Interviewer | yes |
| Baseline behavioral assessment | Enrollment | Interviewer | no |
| Monthly product adherence and behavioral assessment (MBA) | Monthly (not administered at quarterly, semiannual, annual or PUEV visits) | Interviewer | yes |
| Oral product adherence and behavioral assessment (OPA) | Quarterly, PUEV | Interviewer | yes |
| Vaginal product adherence and behavioral assessment (VPA) | Quarterly, PUEV | Interviewer | yes |
| Menstrual practices and study disclosure assessment | Annual, PUEV, scheduled study exit (excludes early termination) | Interviewer | no |
| Audio computer assisted self-interviewing assessment (adherence, acceptability, sexual activity, intra-vaginal practices, product sharing) | Enrollment, quarterly, annual, PUEV, exit, (also administered when product held/discontinued for prior 4 weeks) | Self-administered via computer | no |
| Study exit behavior assessment | Scheduled study exit (excludes early termination visits) | Interviewer | no |
| Termination visit (TVB and TOB) | Exit | Interviewer | yes |
PUEV=product use end visit
Table 2. Adherence questions used in analysis.
| TVB/TOB Question | Monthly visits (MBA) | Quarterly visits (OPA/VPA) |
|---|---|---|
| Q24: How often during the study did you miss or skip days? Q25: When during the study did you start skipping doses? | Total number of months per ppt of Q3a: In the past 7 days how many days did you use no product? | Total number of months per ppt of Q14a: In the past 7 days how many days did you use no product? |
| Q32: In a typical month, how would you describe your ability to use the product as instructed? | NONE | Q13: Please rate your ability, over the past 4 weeks to use the product exactly as you were instructed. |
| Q33: When you say [category from Q32] in a typical month, on how many days did you not take the tablets/gel? | Average per ppt of Q3a: In the past 7 days how many days did you use no product? | Average per ppt of Q14a: In the past 7 days how many days did you use no product? |
| Q34: Did you ever not use the product for 1 week or more in a row? | Ever reported no dose for 7 days in Q3a: In the past 7 days how many days did you use no product? | Ever reported no dose for 7 days in Q14a: In the past 7 days how many days did you use no product? |
Follow-up visits with comparison data and participant exclusion due to product hold
Of 2327 women offered a TVB/TOB interview, all but 6 agreed to participate. Overall, among the 2321 participants with a TVB/TOB form, there were 34,565 follow-up visits with monthly/quarterly behavioral CRFs. The mean number of visits with CRFs was 14.9 and the median was 14. Only 6 participants (0.26%) had fewer than 3 follow-up visits, whereas 2232, over 96%, had 6 or more. Participants were not expected to use products when on a product hold; therefore, when analyzing responses to questions regarding adherence in the week prior to a visit, we included only those visits with 7 or more days of expected product use since last visit. As a result of this requirement, 12 out of 2321 participants did not have enough monthly/quarterly adherence information to be included in some of the comparative analyses.
Analysis
Because of the potential selectivity of participants to whom the TVB/TOB was administered and the possibility that differences in characteristics between the TVB/TOB sample and the non TVB/TOB sample affect findings regarding reporting of adherence, we first compared the characteristics of VOICE participants by whether the TVB/TOB was administered. Second, we described the level of nonadherence as measured categorically (very often, often, sometimes, occasionally, rarely) in the TVB/TOB in response to a question on frequency of missed or skipped days and investigated the association between self-reported nonadherence and reason for trial participation. We then compared frequency of missed/skipped doses with the calculated average number of times a dose was reported skipped in the prior 7 days at routine follow-up visits and documented in CRFs. Third, we compared reports on ever missed/skipped a dose in the TVB/TOB with reports on ever skipped a dose based on the monthly and quarterly CRFs. Fourth, self-reported ability to use the product as instructed in a typical month in the TVB/TOB was compared with aggregated self-reported ability in the 4 weeks prior to quarterly visits during the trial as well as the last quarterly visit. Fifth, we compared the number of days participants skipped a dose in a typical month as reported in the TVB/TOB with the average number of days skipped in the 7 days prior to follow-up visits as reported in the monthly and quarterly CRFs. Finally we compared reports of not using the product for 1 week or more in the TVB/TOB with reports of nonuse for 7 days at least once in a routine follow-up visit. Descriptive statistical tools (frequency distributions and cross tabulations), linear and logistic regression models were used for the comparisons between the reports in the monthly/quarterly CRFs and the TVB/TOB.
The VOICE protocol was approved annually by the Institutional Review Boards and ethics committees at each of the study sites, and was overseen by the regulatory infrastructure of the U.S. National Institutes of Health and the Microbicide Trials Network.
Results
Comparison of VOICE participants with and without administration of the TVB/TOB
Because the TVB/TOB was designed after early closure of the TDF oral and TFV gel arms, participants in these arms were much less likely to have the questionnaire administered; 20.6% of TVB/TOB respondents were assigned to these arms compared to 56.7% of non TVB/TOB respondents. Moreover, the distribution of TVB/TOB respondents by country differed from the VOICE trial. Of TVB/TOB respondents 70.7% were from South Africa, 9.0% from Uganda and 20.3% from Zimbabwe; of non TVB/TOB respondents, 89.9% were from South Africa, 4.2% from Uganda and 5.9% from Zimbabwe. In addition to study arm, multivariable logistic regression analysis indicated that a significantly greater proportion of participants with a TVB/TOB came from Uganda (AOR = 2.43 95% CI 1.59, 3.71, p<.001) and Zimbabwe (AOR=4.52 95% CI 3.16, 6.47, p<.001) than from South Africa, where participants were younger, and more likely to be unmarried. The IRB approval process for the TVB/TOB was more rapid in Uganda and Zimbabwe, and by the time it was administered in South Africa, a greater proportion of that country's participants had exited the trial. Given that plasma TFV detection in the random sub-cohort of active product arm participants in VOICE was positively associated with age and being married [10], the TVB/TOB sample is likely to have been somewhat more adherent than the VOICE sample as a whole.
Missed/skipped doses
Table 3 indicates the frequency of missed or skipped doses reported during VOICE according to Questions 24 and 25 in the TVB/TOB; (the percentage of participants who answered that they “always used” was obtained from Question 25). Fewer than 10% of participants indicated they missed or skipped a dose often or very often. We investigated whether there was an association between the most important reason for trial participation and having skipped/missed doses. Always using the product was reported by 53.1% of those (N = 1215) who said they were primarily motivated “to help test a product to prevent women from getting HIV,” by 44.6% of those (N = 585) who cited “free/better quality health care you received during the trial,” by 48.8% of those (N = 213) who cited “to be tested for HIV,” and by 51.3% of those (N = 195) who cited motivation “to get information about HIV prevention.” While the differences between categories were relatively small, the association between main reason for participating and reported adherence is significant (chi-squared p value = .03).
Table 3. Frequency of missed/skipped doses during VOICE reported in the TVB/TOB.
| N | % | |
|---|---|---|
| Always used | 1134 | 48.9% |
|
| ||
| Rarely (about once every 6 months or less) | 374 | 16.1% |
| Occasionally (less than once per month to once every 5 months) | 227 | 9.8% |
| Sometimes (about once a month) | 320 | 13.8% |
| Often (2-5 times per month; includes response of 1 time per week) | 107 | 4.6% |
| Very often (more than 1 time per week) | 107 | 4.6% |
| Missing | 52 | 2.2% |
|
| ||
| Total | 2321 | 100.0% |
We also assessed the association between responses to the TVB/TOB question on frequency of missed/skipped doses indicated in Table 3 and the calculated average number of times the participant reported skipping a dose in the 7 days before follow-up. The median and the mean number of times reported in the monthly/quarterly CRFs did not always increase with categories in Table 3 as one would expect if the responses were consistent. For example, for those who answered “occasionally” in the TVB/TOB, the median number of times reported skipped in the 7 days before the follow-up visit was 1.0 and the mean was 1.7. For those who answered “very often” in the TVB/TOB, the median and mean were 1.0 and 1.5.
We also compared the consistency in reports of missed/skipped dose between the follow-up visits and the TVB/TOB as shown in Table 4. Nearly half (48.9%) or 1134 of 2321 women with a TVB/TOB form reported at exit that they always used product. In contrast, only 812 of 2321 (35.0%) reported always using product at the monthly/quarterly visits. Moreover, 611 (53.9%) of the 1134 women who reported always using product at the TVB/TOB indicated at follow-up visits that they sometimes skipped doses whereas 184 (22.7%) of the 812 women who reported always using at follow-up indicated at the TVB/TOB that they had skipped doses.
Table 4. Consistency in reporting missed/skipped doses between monthly/quarterly visits and TVB/TOB.
|
|
TVB/TOB | ||||
|---|---|---|---|---|---|
| Monthly/Quarterly VISITS | Skipped a dose | don't know | always used | missing | Total (row %) |
| Skipped a dose | 601 | 252 | 611 | 31 | 1495 (64.4%) |
| always used | 184 | 97 | 512 | 19 | 812 (35.0%) |
| NA | 3 | 0 | 11 | 0 | 14(<0.1%) |
|
| |||||
| Total (column %) | 788 (34.0%) | 349 (15.0%) | 1134 (48.9%) | 50 (2.2%) | 2321 |
Rated ability to use product
Table 5 indicates the distribution of responses to the question asking the participant to rate her ability to use product as instructed, asked at quarterly visits and at TVB/TOB. On average each woman reporting at TVB/TOB had more than 5 quarterly visits.
Table 5. Distribution of responses to questions asking participant to rate her ability to use product at quarterly visits and at TVB/TOB.
| Quarterly visits | TVB/TOB | |||
|---|---|---|---|---|
|
|
|
|||
| N | % | N | % | |
| NA | 1136 | 9% | 53 | 2% |
| excellent | 2937 | 24% | 489 | 21% |
| very good | 2310 | 19% | 571 | 25% |
| good | 4991 | 41% | 945 | 41% |
| fair | 683 | 6% | 213 | 9% |
| poor | 78 | 1% | 38 | 2% |
| very poor | 45 | 0% | 12 | 1% |
|
| ||||
| Total | 12180 | 100% | 2321 | 100% |
A comparison between “fair/poor/very poor” rating of ability to use the product at quarterly visits versus at termination revealed no significant difference; whereas 6.6% reported those three categories during the course of the trial, their proportion increased to only 11.3% at termination, still far from pharmacokinetic measures of product adherence. Moreover, when we crosstabulated the rating response in the TVB/TOB with the rating at the last quarterly visit (not shown), no significant difference was observed (p=0.29).
Number of days skipped dose
A linear regression model was estimated to assess the association between number of days skipped in a typical month reported in the TVB/TOB and the number of days skipped in the week before each monthly visit. If adherence reports based on the TVB/TOB form and the monthly/quarterly visit CRFs were consistent, the ratio of skipped days in a typical month reported in the TVB/TOB and the average days skipped in the 7 days before each monthly/quarterly visit should be 4:1. However, the actual ratio was nearly 1:1 (0.99; 99% C.I. 0.76, 1.22), which suggests that participants were unwilling to report a large absolute number of days with missed doses regardless of the length of the time period reported on — a month in the TVB/TOB versus a week in the monthly/quarterly CRF.
Ever not use for 1 week or more in a row
In the TVB/TOB, 17.9% (406) of 2268 participants reported that they did not use the product for 1 week or more (53 participants did not answer this question). Of these 406 participants 44.1% (179) reported never skipping for one week or more at the monthly/quarterly visits. Correspondingly, of the 1915 who did not respond “yes” to the question about skipping product use for 1 week or more at the TVB/TOB, 31.2% (N=598) reported no dose for 7 days at least once in monthly/quarterly visits. In total 825 participants reported no dose for 7 days at least once in the monthly/quarterly visit — 227 who reported yes in the TVB/TOB + 598 who reported no in the TVB/TOB — a considerably larger number than the 406 who reported nonuse for 1 week or more in the TVB/TOB and contrary to what we hypothesized.
Discussion
This analysis comparing adherence reporting at routine follow-up visits during participation in VOICE with reporting at trial exit indicates that disclosure of product nonadherence did not increase at the termination visit, as anticipated; the findings do not support the hypothesis that women would be more forthcoming about nonuse after they exited the trial and were off product. Indeed, they are evidence that self-reports of adherence were as much, or possibly more, inflated at exit than during the course of the trial. While nearly one-quarter of women reporting perfect adherence during the course of the trial indicated at termination that they had missed doses, over half of participants reporting perfect adherence at termination reported missing doses during follow-up visits. In addition, about twice the proportion of the 2321 participants (35.5%, N=825) reported at least once that they took no dose for 7 days in the follow-up visits than those who reported nonuse for one week or more in the TVB/TOB (17.5% N=406). Moreover, scoring of ability to use study product as directed with the self-rating scale did not change significantly at termination; nearly the same, small, percentage of participants ranked themselves in the bottom three categories during the last quarterly visit as at termination. Note, however, that the rating question in the quarterly follow-up questionnaire was worded slightly differently than in the TVB/TOB in that the former asked the participant to rate ability to use the product “exactly” as instructed. All other things being equal, one therefore might expect that the quarterly follow-up question would generate lower ability to use the product than the TVB/TOB question. If that were the case then we might not observe lower reported ability in the TVB/TOB. In other words, the slight difference in the wording might have partially underestimated reporting of lower ability to use product in the TVB/TOB relative to the quarterly follow-up.
In addition, this analysis revealed considerable inconsistency between reports at follow-up and at TVB/TOB and not in ways that reflected increased reporting of nonadherence when they were no longer taking product. For example, participants were more inclined to report a large proportion of days with missed doses when the time interval was a week during follow-up visits than when it was a month at termination because of an apparent unwillingness to report a large number of absolute days with missed doses. This finding suggests that real time collection of adherence data with a narrow window of time via, for example, SMS, may reduce both recall and social desirability bias.
The analyses reported here indicate that regardless of when asked, women who did not use product as directed were generally unwilling to disclose that they did not use it. One explanation for the over-reporting of product use during follow-up visits and at exit is that the sheer number and complexity of behavioral assessments in the VOICE trial may have confused or annoyed participants. While some questions were complicated and some participants may have found the behavioral assessments difficult or bothersome, there is no evidence that these factors are responsible for the exaggeration of product use. Regardless of: 1) the nature of the question — frequency of use, frequency or timing of skipped doses, reasons for missing a dose, ability to use product as instructed, 2) the nature of the response category —yes/no, likert, or numeric — 3) the visit when the question was asked, 4) the placement of the question within an assessment, or 5) the interview mode —computerized or face-to-face— the self-reported data generated from VOICE indicate an extremely high level of adherence. Moreover, as noted earlier, adherence measured via clinic-based product count of empty pill bottles, and unused pills and applicators was also highly inflated [10]. As others have concluded, we believe that real time biological or respondent-independent markers of product use are needed if we are to establish the levels and patterns of adherence during trials in most settings [10]. When combined with in-depth interviews, pharmacokinetic measures are powerful tools to understand the determinants of product use in HIV prevention trials, in particular the aspects of participants' lives and the characteristics of the product and dosing regimen that either facilitate or undermine product use. Indeed, in the VOICE D qualitative sub-study of 127 active arm participants conducted after the trial was completed using interviewers who were not involved in the main trial, only in the second stage (November 2013-April 2014) when participants were retrospectively provided with their plasma drug levels from the trial did they finally disclose nonuse and offer explanations for this [16, 17]. In stage 1 of VOICE D (December 2012 – March 2013, N=88, 44 of whom also participated in stage 2), participants again did not acknowledge non-use; rather, they discussed other women not using [17]. So on their own, in-depth interviews, thought to encourage greater rapport between participants and study staff than conventional structured interviews, also failed to encourage disclosure of nonuse.
Despite efforts to improve counseling during the course of VOICE by encouraging staff to be more neutral, supportive and less judgmental [16], participants who were disinclined or unable to use products may have feared being terminated from the trial, a concern raised by African participants in FEM-PrEP [18]. In order to understand barriers to product use during HIV prevention trials in resource-limited settings, direct questions about nonadherence may provide little insight. Participants in VOICE valued the ancillary benefits provided by trial participation (e.g. health care and the reimbursement); a desire for continued access to these benefits may have reduced the likelihood of disclosure of product nonuse at exit, perhaps because participants wanted to be considered for future studies [19]. Unlike U.S. participants in MTN 001, an open label daily-use PrEP trial with TDF tablets and TFV gel, who reported that monetary payments instilled a sense of obligation to use the products [20], the African participants in that study — as in VOICE — did not necessarily operate within the same transactional framework. Rather, the payments may have instilled an obligation on the part of African participants to appear to use the products. Relative to U.S. participants, the African women may have less autonomy, and undoubtedly face more economic challenges as well as considerable stigma associated with taking an ARV for prevention; indeed, they are more likely to report barriers to use [21, 22]. In comparison to measures of product use derived from self-report, objective measures of adherence may yield more meaningful data regarding the inability or reluctance to use [19].
Acknowledgments
Funding: The Microbicide Trials Network is funded by the National Institute of Allergy and Infectious Diseases (UM1AI068633, UM1AI068615, UM1AI106707), with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health, all components of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank the study participants as well as the VOICE Study team members who implemented the trial. We also thank Elizabeth Montgomery for comments on an earlier draft.
References
- 1.Coly A, Gorbach PM. Microbicide acceptability research: recent findings and evolution across phases of product development. Curr Opin HIV AIDS. 2008 Sep;3(5):581–6. doi: 10.1097/COH.0b013e32830aba00. [DOI] [PubMed] [Google Scholar]
- 2.Mensch BS, van der Straten A, Katzen LL. Acceptability in microbicide and PrEP Trials: Current status and a reconceptualization. Curr Opin HIV AIDS. 2012 May 19;7(6):534–41. doi: 10.1097/COH.0b013e3283590632. PMC4026162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skoler-Karpoff S, Ramjee G, Ahmed K, et al. Efficacy of Carraguard for prevention of HIV infection in women in South Africa: a randomised, double-blind, placebo-controlled trial. Lancet. 2008 Dec 6;372(9654):1977–87. doi: 10.1016/S0140-6736(08)61842-5. [DOI] [PubMed] [Google Scholar]
- 4.Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22. doi: 10.1056/NEJMoa1202614. PMC3687217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trussell J, Dominik R. Will microbicide trials yield unbiased estimates of microbicide efficacy? Contraception. 2005 Dec;72(6):408–13. doi: 10.1016/j.contraception.2005.06.063. [DOI] [PubMed] [Google Scholar]
- 6.Masse BR, Boily MC, Dimitrov D, Desai K. Efficacy dilution in randomized placebo-controlled vaginal microbicide trials. Emerg Themes Epidemiol. 2009;6:5. doi: 10.1186/1742-7622-6-5. PMC2768687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rees H, Delany-Moretlwe S, Baron D, et al. FACTS 001 Phase III Trial of Pericoital Tenofovir 1% Gel for HIV Prevention in Women. Presentation at Conference on Retroviruses and Opportunistic Infections (CROI); 23-26 February; 2015; Seattle. [Google Scholar]
- 8.Gorbach P, Mensch BS, Husnik M, et al. Effect of computer-assisted interviewing on self-reported sexual behavior data in a microbicide clinical trial. AIDS Behav. 2013;17(2):790–800. doi: 10.1007/s10461-012-0302-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mensch BS, Hewett PC, Abbott S, et al. Assessing the reporting of adherence and sexual activity in a simulated microbicide trial in South Africa: an interview mode experiment using a placebo gel. AIDS Behav. 2011 Feb;15(2):407–21. doi: 10.1007/s10461-010-9791-z. [DOI] [PubMed] [Google Scholar]
- 10.Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2015 Feb 5;372(6):509–18. doi: 10.1056/NEJMoa1402269. PMC4341965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abbott SA, Friedland BA, Sarna A, et al. An evaluation of methods to improve the reporting of adherence in a placebo gel trial in Andhra Pradesh, India. AIDS Behav. 2013;17(6):2222–36. doi: 10.1007/s10461-012-0402-z. PMC3674160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van der Straten A, Montgomery ET, Hartmann M, Minnis A. Methodological lessons from clinical trials and the future of microbicide research. Curr HIV/AIDS Rep. 2012;10(1):89–102. doi: 10.1007/s11904-012-0141-9. [DOI] [PubMed] [Google Scholar]
- 13.Servick K. ‘Nonadherence’: A bitter pill for drug trials. Science. 2014 Oct 17;346(6207):288–9. doi: 10.1126/science.346.6207.288. [DOI] [PubMed] [Google Scholar]
- 14.Lu M, Safren SA, Skolnik PR, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS Behav. 2008 Jan;12(1):86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- 15.Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013 Jan 1;17(1):307–18. doi: 10.1007/s10461-012-0326-7. PMC3549002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Straten A, Mayo A, Brown ER, et al. Perceptions and experiences with the VOICE Adherence Strengthening Program (VASP) in the MTN-003 trial. AIDS Behav. 2015;19(5):770–83. doi: 10.1007/s10461-014-0945-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Musara P, Munaiwa O, Mahaka I, et al. HIV Research for Prevention Conference. Cape Town: 2014. The effect of presentation of pharmacokinetic (PK) drug results on self-reported study product adherence among VOICE participants in Zimbabwe. [Google Scholar]
- 18.Corneli AL, McKenna K, Perry B, et al. The science of being a study participant: FEM-PrEP participants' explanations for overreporting adherence to the study pills and for the whereabouts of unused pills. J Acquir Immune Defic Syndr. 2015 Apr 15;68(5):578–84. doi: 10.1097/QAI.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 19.van der Straten A, Montgomery ET, Musara P, et al. Disclosure of pharmacokinetic drug results to understand nonadherence. AIDS. 2015 Oct 23;29(16):2161–71. doi: 10.1097/QAD.0000000000000801. PMC4638164 (available on 2016-10-23) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minnis AM, van der Straten A, Salee P, Hendrix CW. Pre-exposure prophylaxis adherence measured by plasma drug level in MTN-001: comparison between vaginal gel and oral tablets in two geographic regions. AIDS Behav. 2015 May 13; doi: 10.1007/s10461-015-1081-3. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van der Straten A, Stadler J, Luecke E, et al. Perspectives on use of oral and vaginal antiretrovirals for HIV prevention: The VOICE-C qualitative study in Johannesburg, South Africa. J Int AIDS Soc. 2014 Sep 8;17(Suppl 2):19146. doi: 10.7448/IAS.17.3.19146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van der Straten A, Stadler J, Montgomery E, et al. Women's experiences with oral and vaginal pre-exposure prophylaxis: the VOICE-C qualitative study in Johannesburg, South Africa. PLoS ONE. 2014;9(2):e89118. doi: 10.1371/journal.pone.0089118. [DOI] [PMC free article] [PubMed] [Google Scholar]


