Abstract
Background
Excessive gestational weight gain (GWG) during pregnancy is associated with adverse outcomes for mothers and offspring. Early, mid, and late pregnancy GWG have different associations with fetal growth and later life adiposity, but associations with cord blood hormones, which might predict later health, are not well studied.
Methods
In 978 pregnant women from the pre-birth Project Viva cohort, we calculated trimester-specific GWG using clinically recorded prenatal weights. Outcomes were levels of umbilical cord blood hormones related to fetal and postnatal growth. We used linear regression models adjusted for maternal race/ethnicity, pre-pregnancy BMI, parity, education, pregnancy smoking status and child sex; 2nd and 3rd trimester models were additionally adjusted for GWG in prior trimesters.
Results
Mean ± SD pre-pregnancy BMI was 24.9 ± 5.5 kg/m2, 30% were non-white, and 63% were college graduates. Mean ± SD cord blood hormone levels were insulin-like growth factor [IGF]-1 (56.4 ± 24.3 ng/mL), IGF-2 (408.5 ± 92.7 ng/mL), IGFBP-3 (1084 ± 318 ng/mL), insulin (6.5 ± 7.2 uU/mL), C-peptide (1.0 ± 0.6 ng/mL), leptin (9.0 ± 6.6 ng/mL) and adiponectin (28.7 ± 6.8 μg/mL). Mean ± SD 1st, 2nd and 3rd trimester GWG rates were 0.22 ± 0.22, 0.49 ± 0.19 and 0.46 ± 0.22 kg/wk. Greater 1st trimester GWG (per 0.2 kg/wk) was associated with higher insulin (0.5 uU/mL; 95% CI 0.1, 0.9) and c-peptide (0.06 ng/mL; 95% CI 0.02, 0.09) and lower adiponectin (−0.4 μg/mL; 95% CI −0.9, 0.0). Greater 2nd trimester GWG (per 0.2 kg/wk) was associated with higher IGF-1 (2.3 ng/mL; 95% CI 0.6, 4.0), IGF-2 (7.9 ng/mL; 95% CI 1.2, 14.6), IGFBP-3 (41.6 ng/mL; 95% CI 19.4, 63.7) and leptin (0.9 ng/mL; 0.4, 1.4). 3rd trimester GWG was not associated with cord blood hormones.
Conclusion
1st trimester weight gain appears to matter more for cord blood hormones related to offspring glucose/insulin regulation, whereas 2nd trimester gain matters more for hormones related to growth and adiposity.
Keywords: pregnancy, gestational weight gain, umbilical cord blood, hormones, insulin- like growth factor (IGF), leptin, c-peptide
Introduction
Maternal weight gain during pregnancy is an important determinant of birth outcomes. Gestational weight gain (GWG) is directly associated with birth weight for gestation length, a marker of fetal growth, which1,2 is directly associated with child adiposity and long term risks of cancer and cardiometabolic health.3–5 By alteration of the intrauterine environment, the amount and the timing of weight gained during pregnancy not only influences fetal growth6–10 but also may result in persistent programming of child health,6–8,11 as has been shown previously with other intrauterine exposures such as maternal smoking and gestational diabetes mellitus.12,13
Early, mid, and late pregnancy GWG have different associations with fetal growth. Greater GWG in early pregnancy represents mainly maternal fat gain and might influence placental nutrient transfer differently than later GWG, which reflects fetal and placental growth and maternal fluid expansion in addition to maternal fat gain. Late pregnancy GWG has been consistently reported to be associated with birth weight.7,11 In our cohort, rates of GWG in all 3 trimesters were associated with higher fetal growth, with the greatest effect of 2nd trimester GWG.6 We have also found that greater early and mid-pregnancy weight gain predicted offspring adiposity in mid-childhood, whereas 3rd trimester GWG did not,6 similar to results from other cohorts.8
One of the pathways by which GWG might influence offspring growth and development is through changes in the regulation of mitogenic hormones and adipokines, including insulin, the insulin-like growth factor (IGF) axis, adiponectin, and leptin. We are not aware of prior studies that examined associations of trimester-specific GWG with multiple cord blood hormones, which might predict later health. Therefore, we conducted the present study to examine the extent to which trimester-specific rates of GWG are associated with cord blood hormone levels.
Methods
Between 1999 and 2002 we recruited pregnant women at 8 obstetric offices of Atrius Harvard Vanguard Medical Associates, a multispecialty group practice in eastern Massachusetts.14 Exclusion criteria included multiple gestation, inability to answer questions in English, gestational age ≥22 weeks at recruitment, and plans to move away from the study area before delivery. All participating women provided written informed consent, and institutional review boards reviewed and approved the project in line with ethical standards established by the Declaration of Helsinki.
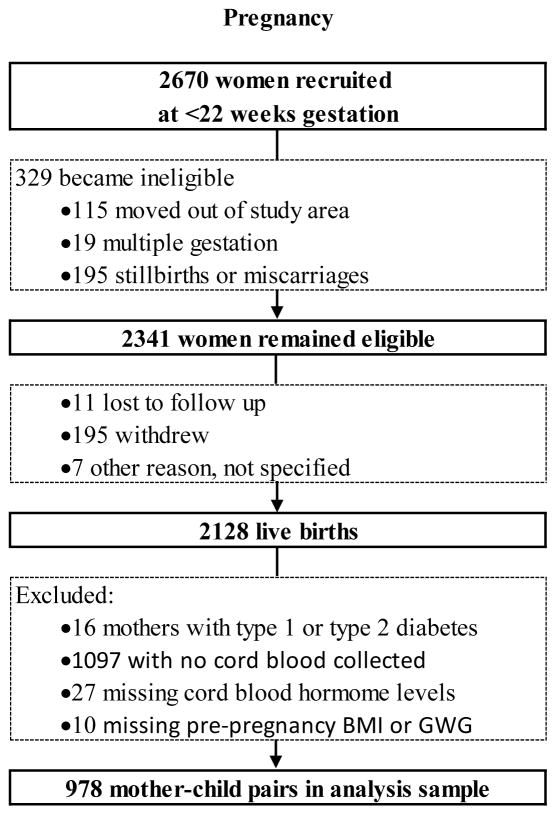
We followed women throughout their pregnancies and obtained clinical data on obstetric and delivery outcomes on 2,128 live singleton births. We collected umbilical cord blood from infants delivered at one hospital that accounted for approximately three-quarters of the cohort births. We obtained cord blood from about two-thirds of deliveries at that hospital, or about one-half of the whole cohort. The midwife or obstetrician obtained umbilical cord blood via syringe and needle from the umbilical vein. Collection of cord blood was challenging given the varied timing of deliveries attended by different clinicians whose primary focus was on clinical care, not research. For this analysis, we excluded 16 mothers with type 1 or type 2 diabetes, 1097 with no cord blood collected, 27 missing cord blood hormone levels, and 10 missing pre-pregnancy BMI or gestational weight gain. Thus the final analysis sample included 978 mother-child pairs with information on gestational weight gain and cord blood hormone levels (Figure 1). Among these 978 vs. the 1150 excluded participants, we found similar mean maternal age (32 years in both groups), pre-pregnancy BMI (24.9 vs. 24.8 kg/m2), total gestational weight gain (15.5 kg in both groups) and rates of smoking during pregnancy (13% in both groups). Women included were less likely to have completed a college degree (63 vs. 66%), more likely to be white (70 v. 63%), and had lower annual household income (60 vs. 62% reported ≥$70,000/year) and had slightly longer gestation length (39.6 vs. 39.2 weeks).
Figure 1.
Participant flow from recruitment through analysis sample in the Project Viva cohort
Measures
Exposures – definition of total and trimester-specific GWG
We collected self-reported pre-pregnancy weight at the initial prenatal visit. Among 343 women who had weight recorded in the medical record in the 3 months before their last menstrual period, the association between self-reported and clinically measured weight was linear (r=0.997).15 We extracted serial prenatal weights from medical records. We obtained a median of 13 (range 5 to 27) clinical weights recorded per woman over the course of the index pregnancy. We calculated total GWG rate as the difference between the last prenatal weight recorded (within 4 weeks of delivery) minus the pre-pregnancy weight, divided by number of gestational weeks at delivery. We defined 1st trimester as the date of last menstrual period to day 91, 2nd trimester as days 91–182, and 3rd trimester as day 182 to the time of the last prenatal weight recorded (within 4 weeks of delivery).
As previously reported,6,16,17 we performed linear interpolation between the 2 closest weight measures to estimate weights at day 91 and day 182 and calculated GWG rates (kg/wk) for each trimester. We also categorized total gestational weight gain as inadequate, adequate, or excessive according to the 2009 Institute of Medicine (IOM) guidelines, which advise less weight gain for women with higher pre-pregnancy BMI. For an underweight woman (BMI <18.5 kg/m2), the IOM guidelines recommend a total weight gain during pregnancy of 28–40 pounds, for a normal weight woman (BMI 18.5-<25.0 kg/m2) the recommended gain is 25–35 pounds, for an overweight woman (BMI 25.0-<30.0 kg/m2) the recommended gain is 15–25 pounds, and for an obese woman (BMI ≥30.0 kg/m2) the recommended gain is 11–20 pounds.1
Outcomes – umbilical cord hormone levels
We included as outcomes umbilical cord plasma concentrations of IGF-1, IGF-2, IGFBP-3, insulin, C-peptide, leptin, and adiponectin. We collected cord blood samples from the umbilical vein after delivery of the infant, refrigerated whole blood for <24 hours, then spun and aliquotted plasma samples for storage in liquid nitrogen.18 We measured hormones using the following commercial assays: adiponectin and leptin (radioimmunoassay, Linco Research Inc., St. Charles, MO);19 C-peptide and insulin (competitive electrochemiluminescence immunoassay, Roche Diagnostics, Indianapolis, IN), insulin-like growth factor-1 (IGF-1) and insulin-like growth factor binding protein 3 (IGF-BP3; ELISA, R&D Systems, Minneapolis, MN); and insulin-like growth factor-2 (IGF-2; ELISA, Alpco Diagnostics, Salem, NH). Day to day variabilities for each of these assays were below 10%.
Other variables
At the initial prenatal visit (median 9.9 weeks gestation), we collected self-reported maternal pre-pregnancy weight, height, education, smoking history, race/ethnicity, and parity.14 All data collection instruments used in Project Viva are publicly available at https://www.hms.harvard.edu/viva/. We calculated pre-pregnancy body mass index (BMI) in kg/m2. We obtained infant birth date, weight, and sex from the hospital medical record. We calculated gestational age at birth using the date of the last menstrual period, or from a mid-pregnancy ultrasound if the two estimates differed by >10 days. We determined sex-specific birth weight for-gestational-age z scores using US reference data.20
Statistical analysis
We conducted linear regression analyses modeling weekly rate of GWG – per 0.2 kg/week – for the total period of pregnancy and for each trimester, to examine their associations with cord blood hormone levels. We selected 0.2 kg/week as the effect size since this was the approximate standard deviation of GWG rate at each trimester in our cohort. We adjusted models for maternal race/ethnicity, pre-pregnancy BMI, parity, education, and pregnancy smoking status. Since weight gain may track across time, to evaluate the independent contributions of each trimester, we additionally adjusted 2nd trimester models for GWG during the 1st trimester, and 3rd trimester models for 1st and 2nd trimester GWGs. Additional adjustment for maternal lifestyle factors during pregnancy (physical activity, television viewing, and intake of sugar-sweetened beverages and fast food) did not appreciably alter findings, so we did not include these measures in our final models. We did not adjust for birth weight, fetal growth, or gestation length because these factors might be on the causal pathway, and conditioning on factors present at birth is likely to introduce collider bias.21,22 All models met standard assumptions for linear regression. Distributions of insulin and C-peptide were somewhat right-skewed, but when we re-ran our analyses using log-transformed results, the directions and significance of estimates were very similar, and therefore we present the untransformed values for ease of interpretation and for comparability across outcomes. We additionally adjusted models with IGF-1 or IGF-2 as the outcome for levels of IGFBP-3, to get an estimate of the effect on IGF-1 or IGF-2 independent of the level of the binding protein. We also conducted linear regression analyses modeling GWG as a categorical variable – inadequate, adequate, or excessive weight according to the 2009 IOM guidelines.1
As a secondary analysis, we stratified models by child sex and also examined interaction p-values. As a sensitivity analysis, we repeated our final models after excluding 59 participants with GDM because management of GDM can influence subsequent weight gain, as well as 36 with pre-pregnancy BMI <18.5 kg/m2and 12 with gestation length <34 weeks, given small numbers and likely different weight gain patterns in these categories. We performed all analyses using SAS version 9.3 (SAS Institute, Cary NC).
Results
Of the 978 women included in this analysis, mean ± SD age at enrollment was 31.8 ± 5.2 years and pre-pregnancy BMI was 24.9 ± 5.5 kg/m2. At enrollment,30% were non-white, 63% were college graduates, 45% were nulliparous, 92% were married or cohabitating, and 60% reported a household income of >$70,000 per year (Table 1). Mean ± SD 1st, 2nd and 3rd trimester GWG rates were 0.22 ± 0.22, 0.49 ± 0.19 and 0.46 ± 0.22 kg/wk. Rate of GWG for the whole pregnancy was strongly correlated with rate of GWG in the 1st trimester (Pearson r=0.58), 2nd trimester (r=0.75), and 3rd trimester (r=0.70). The correlation coefficient for 2nd and 3rd trimester GWG was 0.43, 1st and 2nd trimester GWG was 0.15, and 1st and 3rd trimester GWG was −0.01.
Table 1.
Characteristics of 978 pregnant women and their infants in Project Viva, overall and according to total GWG per 2009 Institute of Medicine (IOM) guidelines1
| Total GWG per IOM guidelines* | ||||
|---|---|---|---|---|
| Overall | Inadequate | Adequate | Excessive | |
| n=978 | n=122 | n=289 | n=554 | |
| N (%) or Mean (SD) | ||||
| Maternal Characteristics | ||||
| Age, years | 31.8 (5.2) | 31.4 (5.9) | 32.1 (4.9) | 31.9 (5.1) |
| Pre-pregnancy BMI, kg/m2 | 24.9 (5.5) | 24.8 (5.9) | 23.8 (5.5) | 25.6 (5.3) |
| Pre-pregnancy BMI category | ||||
| 18.5 – <25.0 kg/m2 | 616 (63.0) | 87 (71.3) | 225 (77.9) | 295 (53.2) |
| 25.0 – <30.0 kg/m2 | 207 (21.2) | 14 (11.5) | 37 (12.8) | 154 (27.8) |
| >=30.0 kg/m2 | 155 (15.8) | 21 (17.2) | 27 (9.3) | 105 (19.0) |
| Race/ethnicity, % | ||||
| Black | 142 (14.6) | 19 (15.6) | 47 (16.3) | 74 (13.4) |
| Hispanic | 65 (6.7) | 17 (13.9) | 22 (7.6) | 26 (4.7) |
| White | 683 (70.1) | 75 (61.5) | 191 (66.3) | 412 (74.5) |
| Other | 85 (8.7) | 11 (9.0) | 28 (9.7) | 41 (7.4) |
| College graduate, % | ||||
| No | 358 (36.7) | 51 (41.8) | 101 (35.1) | 201 (36.3) |
| Yes | 617 (63.3) | 71 (58.2) | 187 (64.9) | 352 (63.7) |
| Nulliparous, % | ||||
| No | 533 (54.5) | 79 (64.8) | 164 (56.7) | 282 (50.9) |
| Yes | 445 (45.5) | 43 (35.2) | 125 (43.3) | 272 (49.1) |
| Married or cohabitating, % | ||||
| No | 82 (8.4) | 12 (9.8) | 23 (8.0) | 47 (8.5) |
| Yes | 892 (91.6) | 110 (90.2) | 264 (92.0) | 506 (91.5) |
| Household income % | ||||
| <=$70,000/yr | 349 (39.9) | 50 (46.7) | 107 (40.5) | 188 (37.8) |
| >$70,000/yr | 526 (60.1) | 57 (53.3) | 157 (59.5) | 309 (62.2) |
| Smoking status | ||||
| Never | 654 (67.6) | 90 (73.8) | 206 (71.5) | 351 (63.9) |
| Former | 191 (19.7) | 22 (18.0) | 49 (17.0) | 119 (21.7) |
| During pregnancy | 123 (12.7) | 10 (8.2) | 33 (11.5) | 79 (14.4) |
| Prenatal glycemic status, % | ||||
| Normal glycemia | 792 (82.0) | 94 (77.7) | 242 (83.7) | 453 (81.9) |
| IH | 85 (8.8) | 11 (9.1) | 22 (7.6) | 52 (9.4) |
| IGT | 30 (3.1) | 2 (1.7) | 8 (2.8) | 20 (3.6) |
| Gestational diabetes mellitus | 59 (6.1) | 14 (11.6) | 17 (5.9) | 28 (5.1) |
| Total GWG, kg | 15.5 (5.8) | 7.5 (4.2) | 12.8 (2.7) | 18.8 (4.6) |
| 1st trimester GWG, kg/wk | 0.22 (0.22) | 0.02 (0.20) | 0.17 (0.16) | 0.30 (0.22) |
| 2nd trimester GWG, kg/wk | 0.49 (0.19) | 0.29 (0.19) | 0.43 (0.15) | 0.55 (0.18) |
| 3rd trimester GWG, kg/wk | 0.46 (0.22) | 0.27 (0.20) | 0.37 (0.15) | 0.56 (0.20) |
| Child Characteristics | ||||
| Sex, % | ||||
| Male | 510 (52.1) | 58 (47.5) | 142 (49.1) | 304 (54.9) |
| Female | 468 (47.9) | 64 (52.5) | 147 (50.9) | 250 (45.1) |
| Birth weight, g | 3523 (534) | 3296 (595) | 3436 (510) | 3617 (514) |
| Gestation length, wk | 39.6 (1.6) | 39.1 (2.2) | 39.5 (1.6) | 39.8 (1.5) |
| Birth weight for gestational age, z-score | 0.24 (0.95) | −0.07 (0.96) | 0.07 (0.94) | 0.40 (0.93) |
| Cesarean delivery, % | ||||
| No | 797 (82.3) | 100 (82.0) | 244 (84.4) | 450 (81.2) |
| Yes | 171 (17.7) | 22 (18.0) | 45 (15.6) | 104 (18.8) |
| Cord blood hormones | ||||
| IGF-1, ng/mL | 56.4 (24.3) | 57.6 (25.5) | 55.7 (22.7) | 56.5 (24.7) |
| IGF-2, ng/mL | 409 (93) | 391 (82) | 403 (92) | 416 (95) |
| IGFBP-3, ng/mL | 1084 (318) | 1032 (289) | 1070 (305) | 1100 (328) |
| Insulin, uU/mL | 6.5 (7.2) | 5.6 (5.2) | 5.9 (5.1) | 7.1 (8.4) |
| C-peptide, ng/mL | 1.0 (0.6) | 0.9 (0.5) | 1.0 (0.5) | 1.1 (0.7) |
| Leptin, ng/mL | 9.0 (6.6) | 7.9 (6.0) | 8.5 (6.6) | 9.5 (6.7) |
| Adiponectin, μg/mL | 28.7 (6.8) | 27.7 (7.1) | 29.0 (6.7) | 28.7 (6.8) |
We categorized total gestational weight gain as inadequate, adequate, or excessive according to the 2009 Institute of Medicine (IOM) guidelines. For an underweight woman (BMI <18.5 kg/m2), the IOM guidelines recommend a total weight gain during pregnancy of 28–40 pounds, for a normal weight woman (BMI 18.5-<25.0 kg/m2) the recommended gain is 25–35 pounds, for an overweight woman (BMI 25.0-<30.0 kg/m2) the recommended gain is 15–25 pounds, and for an obese woman (BMI ≥30.0 kg/m2) the recommended gain is 11–20 pounds.
According to the 2009 IOM guidelines for total pregnancy weight gain, 57% of women gained excessive weight, 30% gained adequate weight, and 13% gained adequate weight. Proportions were similar for categorical weight gain within 2nd and 3rd trimesters (data not shown).
Mean ± SD cord blood hormone levels were: insulin-like growth factor [IGF]-1 (56.4 ± 24.3 ng/mL), IGF-2 (408.5 ± 92.7 ng/mL), IGFBP-3 (1084 ± 318 ng/mL), insulin (6.5 ± 7.2 uU/mL), C-peptide (1.0 ± 0.6 ng/mL), leptin (9.0 ± 6.6 ng/mL) and adiponectin (28.7 ± 6.8 μg/mL). Cord blood hormone concentrations differed substantially by infant sex, with lower levels of all hormones among boys (data not shown).23
Umbilical cord blood hormone concentrations were correlated with each other to varying degrees, with the strongest correlations between C-peptide and insulin (Spearman r=0.80), IGFBP-3 and IGF-1 (r=0.65), and IGFBP-3 and IGF-2 (r=0.65). IGF-1 was modestly correlated with IGF-2 (r=0.26) and also with insulin (r=0.38), C-peptide (r=0.33), and leptin (r=0.24).23
Estimates of association were only minimally different unadjusted v. adjusted for maternal race/ethnicity, pre-pregnancy BMI, parity, education, pregnancy smoking status and child sex, and so we report only the adjusted estimates (Table 2). Greater 1st trimester GWG (per each 0.2 kg/wk) was associated with higher insulin (0.5 uU/mL; 95% CI 0.1, 0.9) and c-peptide (0.06 ng/mL; 95% CI 0.02, 0.09) and lower adiponectin (−0.4 μg/mL; 95% CI −0.9, 0.0). 2nd trimester gain was more weakly associated with insulin (0.4; 95% CI: −0.1, 0.9) and c-peptide (0.04; 95% CI: −0.01, 0.08). Additionally, greater 2nd trimester GWG (0.2 kg/wk) was associated with higher IGF-1 (2.3 ng/mL; 95% CI 0.6, 4.0), IGF-2 (7.9 ng/mL; 95% CI 1.2, 14.6), IGFBP-3 (41.6 ng/mL; 95% CI 19.4, 63.7) and leptin (0.9 ng/mL; 0.4, 1.4). 3rd trimester GWG was not associated with cord blood hormones. When we additionally adjusted for IGFBP-3, 2nd trimester GWG was no longer associated IGF-1 (0.2 ng/mL; 95% CI −1.0, 1.5) or IGF-2 (−0.8 ng/mL; 95% CI −5.7, 4.1). Total GWG was directly associated with almost all outcomes (Table 2) with the exception of adiponectin, and was not associated with IGF-1 or IGF-2 after adjustment for IGFBP-3. We observed similar results when we compared excessive v. inadequate total GWG per IOM guidelines.1 (Table 3)
Table 2.
Multivariable associations of trimester-specific GWG with cord blood hormone concentrations at delivery (N=978)
| Exposure - GWG (per 0.2 kg/wk) | ||||
|---|---|---|---|---|
| 1st trim | 2nd trim | 3rd trim | Total pregnancy | |
| Umbilical cord blood hormone | β (95% CI) | |||
| IGF-1 ng/mL | −0.4 (−1.7, 0.9) | 2.3 (0.6, 4.0) | 0.5 (−1.0, 2.0) | 1.9 (−0.3, 4.0) |
| IGF-2, ng/mL | 1.1 (−4.2, 6.4) | 7.9 (1.2, 14.6) | 3.6 (−2.4, 9.7) | 10.7 (2.0, 19.4) |
| IGFBP-3 ng/mL | 3.6 (−14.0, 21.1) | 41.6 (19.4, 63.7) | 13.9 (−6.1, 33.9) | 47.6 (19.0, 76.2) |
| IGF-1 ng/mL* | −0.6 (−1.5, 0.4) | 0.2 (−1.0, 1.5) | −0.2 (−1.3, 0.9) | −0.5 (−2.1, 1.1) |
| IGF-2, ng/mL* | 0.3 (−3.5, 4.2) | −0.8 (−5.7, 4.1) | 0.8 (−3.7, 5.2) | 0.8 (−5.5, 7.2) |
| Insulin uU/mL | 0.5 (0.1, 0.9) | 0.4 (−0.1, 0.9) | −0.1 (−0.5, 0.4) | 0.8 (0.1, 1.4) |
| C-peptide ng/mL | 0.06 (0.02, 0.09) | 0.04 (−0.01, 0.08) | −0.01 (−0.05, 0.03) | 0.08 (0.02, 0.14) |
| Leptin, ng/mL | 0.0 (−0.4, 0.4) | 0.9 (0.4, 1.4) | 0.1 (−0.4, 0.5) | 0.8 (0.2, 1.5) |
| Adiponectin, μg/mL | −0.4 (−0.9, 0.0) | 0.4 (−0.1, 1.0) | −0.3 (−0.8, 0.2) | −0.2 (−0.9, 0.5) |
Adjusted for maternal race/ethnicity, pre-pregnancy BMI, parity, education, pregnancy smoking status and child sex.
2nd and 3rd trimester models additionally adjusted for GWG in prior trimesters.
Additionally adjusted for IGFBP-3.
Table 3.
Multivariable associations of total GWG categories per 2009 Institute of Medicine (IOM) guidelines1 with cord blood hormone concentrations at delivery (N=978)
| Total GWG categories per IOM guidelines | |||
|---|---|---|---|
| Inadequate | Adequate | Excessive | |
| Umbilical cord blood hormone | β (95% CI) | ||
| IGF-1 ng/mL | 0.0 (ref) | −0.4 (−5.3, 4.5) | 1.9 (−2.7, 6.5) |
| IGF-2, ng/mL | 0.0 (ref) | 13.0 (−6.8, 32.8) | 25.2 (6.6, 43.7) |
| IGFBP-3 ng/mL | 0.0 (ref) | 46.4 (−19.0,111.8) | 84.4 (23.0,145.7) |
| IGF-1 ng/mL* | 0.0 (ref) | −2.7 (−6.4, 1.0) | −2.3 (−5.8, 1.1) |
| IGF-2, ng/mL* | 0.0 (ref) | 3.4 (−11.0, 17.9) | 7.6 (−5.9, 21.2) |
| Insulin uU/mL | 0.0 (ref) | 0.5 (−1.0, 2.0) | 1.5 (0.0, 2.9) |
| C-peptide ng/mL | 0.0 (ref) | 0.07 (−0.07, 0.20) | 0.15 (0.02, 0.28) |
| Leptin, ng/mL | 0.0 (ref) | 0.6 (−0.9, 2.1) | 1.8 (0.4, 3.2) |
| Adiponectin, μg/mL | 0.0 (ref) | 1.4 (−0.2, 2.9) | 1.2 (−0.2, 2.7) |
Adjusted for maternal race/ethnicity, pre-pregnancy BMI, parity, education, pregnancy smoking status and child sex.
Additionally adjusted for IGFBP-3.
The association of 1st trimester GWG with IGF-1 differed by infant sex (interaction p-value = 0.01). Among girls, greater 1st trimester GWG (0.2 kg/wk) was associated with lower IGF-1 (−2.3 ng/mL; 95% CI −4.3, −0.2) but not among boys (−1.2 ng/mL; 95% CI −0.5, 2.9). The rest of the associations did not differ by infant sex.
In our sensitivity analysis, excluding 107 participants with GDM, BMI <18.5 kg/m2, or gestation length <34 weeks, estimates of association were only minimally different. For example, greater 2nd trimester GWG (per 0.2 kg/wk) was associated with higher IGF-1 (2.5 ng/mL; 95% CI 0.8, 4.4), IGF-2 (8.5 ng/mL; 95% CI 1.5, 16.6), IGFBP-3 (45.5 ng/mL; 95% CI 22.6, 68.3) and leptin (1.0 ng/mL; 0.5, 1.4).
Discussion
In this prospective study of almost 1000 mother-infant pairs, we found that greater 1st trimester GWG was associated with higher insulin and c-peptide and lower adiponectin, whereas greater 2nd trimester GWG was associated with higher IGF-1, IGF-2, IGFBP-3, and leptin. 3rd trimester GWG was not associated with cord blood hormones. This pattern suggest that 1st trimester weight gain may impact glucose and insulin regulation, whereas 2nd trimester gain may impact fetal and postnatal growth.
Our results are consistent with the existing, limited literature on weight gain during pregnancy and cord blood hormone concentrations. Higher weight gain over the entire pregnancy has been associated with higher cord blood leptin24,25 and insulin24 in population-based birth cohorts. Also in line with our findings, the “Rhea” cohort in Crete further subdivided the timing of GWG and demonstrated associations of cord blood leptin with mid-late (2nd/3rd trimester) but not early (1st trimester) weight gain.8 However, that approach could not distinguish between 2nd and 3rd trimester-specific effects. Our study adds to the existing literature by examining additional cord blood hormones related to growth and adiposity and by examining pregnancy weight gain separately during each trimester.
Disentangling the influence of GWG during each trimester on the metabolic profile of the fetus provides insight into potential biological pathways through which trimester-specific GWG differentially impacts fetal and child adiposity. For example, in our cohort6 and others,7,8,11 early but not late GWG was associated with greater adiposity in offspring during childhood. Here, we found greater GWG during the 1st but not later trimesters to be associated with lower adiponectin and higher c-peptide and insulin in cord blood.
Early GWG represents primarily maternal rather than fetal fat gain, and a resultant metabolically dysregulated intrauterine environment (i.e., lower adiponectin and higher insulin) could predispose offspring to adiposity and insulin resistance. Adiponectin acts on the central nervous system to increase energy expenditure and decrease body weight,26 and low adiponectin has been specifically associated with central adiposity.27,28 Thus, low adiponectin in utero may be a pathway through which 1st trimester GWG could program increased adiposity, especially central adiposity6,8,11 in mid-childhood. Adiponectin also acts directly on adipose tissue to increase insulin sensitivity.29 Our finding of an association between 1st trimester GWG and higher cord blood insulin and c-peptide may reflect low adiponectin leading to impaired insulin action in adipose and other peripheral tissues. Cord blood insulin tracks with insulin levels later in life, suggesting that it may be a marker of later insulin resistance.30 However, studies have not shown a consistent association between GWG and insulin resistance into adolescence.11,31,32
Higher GWG has been consistently reported to be associated with higher birth size, with the strongest associations between mid-late pregnancy GWG and birth size.6–10 This is in line with the fact that mid-late pregnancy GWG primarily reflects fetal and placental growth rather than maternal fat gain. In Project Viva, we previously found that higher rates of GWG during each trimester were associated with higher birth weight for gestational age z-scores, with the largest effect size for 2nd trimester weight gain.6 Similarly, in the present study, we found greater GWG specifically during the 2nd trimester to be associated with higher levels of growth-promoting factors IGF-1, IGF-2, IGFBP-3, and leptin in cord blood. This raises the possibility that mid-pregnancy GWG leads to an intrauterine growth-promoting hormonal milieu and thereby increased size at birth.
The 2nd trimester is the most important period for development of adipose tissue and fetal organs, including muscle, heart, liver, and bone.33 IGF-2 plays a role in organogenesis,34 and IGF-1 promotes fetal growth in mid-late pregnancy.35 Cord blood IGF-136 and leptin25,37,38 correlate strongly with size at birth, with weaker associations between IGF-2 and birth size.39 IGFBP-3 is a major IGF binding protein, with approximately 80% of IGF-I and IGF-2 bound to IGFBP-3 and 1% free.40 We found that 2nd trimester GWG was no longer associated with IGF-1 and IGF-2 when we additionally adjusted for IGFBP-3. GWG may impact this binding protein rather than directly altering IGF-1 or IGF-2 levels, although these results require replication.
Strengths of this study are its large sample size, inclusion of important covariates including maternal BMI, evaluation of a large array of cord blood hormones, and prospective assessment of trimester-specific GWG. However, generalizability may be limited because women were generally well-educated and all recruited from a single health system. Another limitation was that we were able to evaluate only subset of the Project Viva cohort because we did not collect cord blood on all participants. However, we believe our results are unlikely to be influenced by selection bias, as included versus excluded participants were similar in pre-pregnancy BMI, GWG, and other characteristics.
In summary, we found that 1st trimester weight gain appears to matter more for cord blood hormones related to glucose and insulin regulation, whereas 2nd trimester gain matters more for those related to fetal and postnatal growth. 3rd trimester GWG was not associated with the cord blood hormonal milieu. These findings suggest that the intrauterine metabolic environment may be programmed by GWG during early to mid- rather than late pregnancy. Thus, interventions to limit excessive GWG may benefit by starting in very early pregnancy.
Acknowledgments
Funding: Project Viva is supported by the National Institutes of Health (R01HD034568). Dr. Oken is additionally supported by K24 HD069408 and P30 DK092924. Dr. Fleisch is additionally supported by K23ES024803.
Abbreviations
- BMI
body mass index
- CI
confidence interval
- GWG
gestational weight gain
- IGF
insulin-like growth factor
- SD
standard deviation
Footnotes
The views expressed in this article do not necessarily represent the views of the US Government, the Department of Health and Human Services or the National Institutes of Health.
Conflicts of interest: None
Authors’ contributions: SRS, EO, and MWG contributed to the conception and design of the study; SRS, CM, MWG, and EO contributed to the acquisition of the data; SRS, AF, MFH, CM, MWG, and EO and contributed to the interpretation of the data; SRS performed statistical analyses; SRS drafted the manuscript; SRS has primary responsibility for the final content. All authors have read, critically revised, and approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Institute of Medicine National Research Council Committee to Reexamine I. O. M. Pregnancy Weight Guidelines. The National Academies Collection: Reports funded by National Institutes of Health. In: Rasmussen KM, Yaktine AL, editors. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academies Press (US) National Academy of Sciences; 2009. [Google Scholar]
- 2.Luke B, Hediger ML, Scholl TO. Point of diminishing returns: When does gestational weight gain cease benefiting birthweight and begin adding to maternal obesity? J Matern Fetal Med. 1996;5:168–73. doi: 10.1002/(SICI)1520-6661(199607/08)5:4<168::AID-MFM2>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 3.Whitaker RC, Dietz WH. Role of the prenatal environment in the development of obesity. J Pediatr. 1998;132:768–76. doi: 10.1016/s0022-3476(98)70302-6. [DOI] [PubMed] [Google Scholar]
- 4.Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003;11:496–506. doi: 10.1038/oby.2003.69. [DOI] [PubMed] [Google Scholar]
- 5.Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196:322, e321–e328. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hivert MF, Rifas-Shiman SL, Gillman MW, Oken E. Greater early and mid-pregnancy gestational weight gains are associated with excess adiposity in mid-childhood. Obesity (Silver Spring) 2016 Jul;24(7):1546–53. doi: 10.1002/oby.21511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Margerison-Zilko CE, Shrimali BP, Eskenazi B, Lahiff M, Lindquist AR, Abrams BF. Trimester of maternal gestational weight gain and offspring body weight at birth and age five. Matern Child Health J. 2012;16(6):1215–23. doi: 10.1007/s10995-011-0846-1. [DOI] [PubMed] [Google Scholar]
- 8.Karachaliou M, Georgiou V, Roumeliotaki T, Chalkiadaki G, Daraki V, Koinaki S, Dermitzaki E, Sarri K, Vassilaki M, Kogevinas M, Oken E, Chatzi L. Association of trimester-specific gestational weight gain with fetal growth, offspring obesity, and cardiometabolic traits in early childhood. American Journal of Obstetrics & Gynecology. 212(4):502.e1–502.e14. doi: 10.1016/j.ajog.2014.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruchat S, Allard C, Doyon M, et al. Timing of excessive weight gain during pregnancy modulates newborn anthropometry. J Obstet Gynaecol Can. 2016;38:108–117. doi: 10.1016/j.jogc.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Sridhar SB, Xu F, Hedderson MM. Trimester-Specific Gestational Weight Gain and Infant Size for Gestational Age. PLoS One. 2016;11:e0159500. doi: 10.1371/journal.pone.0159500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gaillard R, Welten M, Oddy WH, Beilin LJ, Mori TA, Jaddoe VW, et al. Associations of maternal prepregnancy body mass index and gestational weight gain with cardio-metabolic risk factors in adolescent offspring: a prospective cohort study. BJOG. 2016;123:207–16. doi: 10.1111/1471-0528.13700. [DOI] [PubMed] [Google Scholar]
- 12.Oken E, Huh SY, Taveras EM, Rich-Edwards JW, Gillman MW. Associations of maternal prenatal smoking with child adiposity and blood pressure. Obes Res. 2005;13:2021–8. doi: 10.1038/oby.2005.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dabelea D, Hanson RL, Lindsay RS, et al. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships. Diabetes. 2000;49:2208–11. doi: 10.2337/diabetes.49.12.2208. [DOI] [PubMed] [Google Scholar]
- 14.Oken E, Baccarelli AA, Gold DR, et al. Cohort profile: Project Viva. Int J Epidemiol. 2015 Feb;44(1):37–48. doi: 10.1093/ije/dyu008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Provenzano AM, Rifas-Shiman SL, Herring SJ, Rich-Edwards JW, Oken E. Associations of maternal material hardships during childhood and adulthood with prepregnancy weight, gestational weight gain, and postpartum weight retention. J Womens Health(Larchmt) 2015;24(7):563–71. doi: 10.1089/jwh.2014.5016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kleinman KP, Oken E, Radesky JS, Rich-Edwards JW, Peterson KE, Gillman MW. How should gestational weight gain be assessed? A comparison of existing methods and a novel method, area under the weight gain curve. Int J Epidemiol. 2007 Dec;36(6):1275–1282. doi: 10.1093/ije/dym156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walter JR, Perng W, Kleinman KP, Rifas-Shiman SL, Rich-Edwards JW, Oken E. Associations of trimester-specific gestational weight gain with maternal adiposity and systolic blood pressure at 3 and 7 years postpartum. Am J Obstet Gynecol. 2014 Nov 13; doi: 10.1016/j.ajog.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parker M, Rifas-Shiman SL, Belfort MB, et al. Gestational glucose tolerance and cord blood leptin levels predict slower weight gain in early infancy. J Pediatr. 2011;158(2):227–233. doi: 10.1016/j.jpeds.2010.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mantzoros CS, Rifas-Shiman SL, Williams CJ, Fargnoli JL, Kelesidis T, Gillman MW. Cord blood leptin and adiponectin as predictors of adiposity in children at 3 years of age: a prospective cohort study. Pediatrics. 2009;123(2):682–689. doi: 10.1542/peds.2008-0343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3(1):6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.VanderWeele TJ, Mumford SL, Schisterman EF. Conditioning on intermediates in perinatal epidemiology. Epidemiology. 2012 Jan;23(1):1–9. doi: 10.1097/EDE.0b013e31823aca5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tu YK, West R, Ellison GT, Gilthorpe MS. Why evidence for the fetal origins of adult disease might be a statistical artifact: the "reversal paradox" for the relation between birth weight and blood pressure in later life. Am J Epidemiol. 2005 Jan 1;161(1):27–32. doi: 10.1093/aje/kwi002. [DOI] [PubMed] [Google Scholar]
- 23.Oken E, Eggleston EM, Rifas-Shiman SL, Switkowski K, Hivert M-F, Mantzoros C, Gillman MW. Sex-specific associations of maternal gestational glycemia with hormones in umbilical cord blood at delivery. American Journal of Perinatology. 2016 doi: 10.1055/s-0036-1586509. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lemas DJ, Brinton JT, Shapiro AL, Glueck DH, Friedman JE, Dabelea D. Associations of maternal weight status prior and during pregnancy with neonatal cardiometabolic markers at birth: the Healthy Start study. Int J Obes (Lond) 2015;39:1437–42. doi: 10.1038/ijo.2015.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karakosta P, Georgiou V, Fthenou E, Papadopoulou E, Roumeliotaki T, Margioris A, et al. Maternal weight status, cord blood leptin and fetal growth: a prospective mother-child cohort study (Rhea study) Paediatr Perinat Epidemiol. 2013;27:461–71. doi: 10.1111/ppe.12074. [DOI] [PubMed] [Google Scholar]
- 26.Qi Y, Takahashi N, Hileman SM, et al. Adiponectin acts in the brain to decrease body weight. Nature medicine. 2004;10:524–9. doi: 10.1038/nm1029. [DOI] [PubMed] [Google Scholar]
- 27.Rasmussen-Torvik LJ, Pankow JS, Jacobs DR, Jr, Steinberger J, Moran A, Sinaiko AR. Development of associations among central adiposity, adiponectin and insulin sensitivity from adolescence to young adulthood. Diabet Med. 2012;29:1153–8. doi: 10.1111/j.1464-5491.2012.03726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steffes MW, Gross MD, Schreiner PJ, Yu X, Hilner JE, Gingerich R, et al. Serum adiponectin in young adults--interactions with central adiposity, circulating levels of glucose, and insulin resistance: the CARDIA study. Ann Epidemiol. 2004;14:492–8. doi: 10.1016/j.annepidem.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 29.Turer AT, Scherer PE. Adiponectin: mechanistic insights and clinical implications. Diabetologia. 2012;55:2319–26. doi: 10.1007/s00125-012-2598-x. [DOI] [PubMed] [Google Scholar]
- 30.Wang G, Divall S, Radovick S, Paige D, Ning Y, Chen Z, et al. Preterm birth and random plasma insulin levels at birth and in early childhood. JAMA. 2014;311:587–96. doi: 10.1001/jama.2014.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hrolfsdottir L, Rytter D, Olsen SF, Bech BH, Maslova E, Henriksen TB, et al. Gestational weight gain in normal weight women and offspring cardio-metabolic risk factors at 20 years of age. Int J Obes (Lond) 2015;39:671–6. doi: 10.1038/ijo.2014.179. [DOI] [PubMed] [Google Scholar]
- 32.Perng W, Gillman MW, Mantzoros CS, Oken E. A prospective study of maternal prenatal weight and offspring cardiometabolic health in mid-childhood. Ann Epidemiol. 2014 Nov;24(11):793–800.e1. doi: 10.1016/j.annepidem.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poissonnet CM, Burdi AR, Bookstein FL. Growth and development of human adipose tissue during early gestation. Early Hum Dev. 1983;8(1):1–11. doi: 10.1016/0378-3782(83)90028-2. [DOI] [PubMed] [Google Scholar]
- 34.Chao W, D'Amore PA. IGF2: epigenetic regulation and role in development and disease. Cytokine & growth factor reviews. 2008 Apr;19(2):111–120. doi: 10.1016/j.cytogfr.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bloomfield FH, Spiroski AM, Harding JE. Fetal growth factors and fetal nutrition. Seminars in fetal & neonatal medicine. 2013 Apr 30; doi: 10.1016/j.siny.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 36.Wiley AS, Lubree HG, Joshi SM, Bhat DS, Ramdas LV, Rao AS, et al. Cord IGF-I concentrations in Indian newborns: associations with neonatal body composition and maternal determinants. Pediatr Obes. 2016;11:151–7. doi: 10.1111/ijpo.12038. [DOI] [PubMed] [Google Scholar]
- 37.Donnelly JM, Lindsay KL, Walsh JM, Horan M, Molloy EJ, McAuliffe FM. Fetal metabolic influences of neonatal anthropometry and adiposity. BMC Pediatr. 2015;15:175. doi: 10.1186/s12887-015-0499-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Inoue M, Itabashi K, Nakano Y, Tobe T. High-molecular-weight adiponectin and leptin levels in cord blood are associated with anthropometric measurements at birth. Horm Res. 2008;70:268–72. doi: 10.1159/000157872. [DOI] [PubMed] [Google Scholar]
- 39.Ong K, Kratzsch J, Kiess W, Costello M, Scott C, Dunger D. Size at birth and cord blood levels of insulin, insulin-like growth factor I (IGF-I), IGF-II, IGF-binding protein-1 (IGFBP-1), IGFBP-3, and the soluble IGF-II/mannose-6-phosphate receptor in term human infants. The ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. J Clin Endocrinol Metab. 2000 Nov;85(11):4266–4269. doi: 10.1210/jcem.85.11.6998. [DOI] [PubMed] [Google Scholar]
- 40.Rutanen EM. Insulin-like growth factors in obstetrics. Curr Opin Obstet Gynecol. 2000 Jun;12(3):163–168. doi: 10.1097/00001703-200006000-00001. [DOI] [PubMed] [Google Scholar]