Abstract
Objective
We sought to examine psychological mechanisms of treatment outcomes of a mindfulness meditation intervention for Generalized Anxiety Disorder (GAD).
Methods
We examined mindfulness and decentering as two potential therapeutic mechanisms of action of generalized anxiety disorder (GAD) symptom reduction in patients randomized to receive either mindfulness-based stress reduction (MBSR) or an attention control class (N=38). Multiple mediation analyses were conducted using a non-parametric cross product of the coefficients approach that employs bootstrapping.
Results
Analyses revealed that change in decentering and change in mindfulness significantly mediated the effect of MBSR on anxiety. When both mediators were included in the model, the multiple mediation analysis revealed a significant indirect effect through increases in decentering, but not mindfulness. Furthermore, the direct effect of MBSR on decrease in anxiety was not significant, suggesting that decentering fully mediated the relationship. Results also suggested that MBSR reduces worry through an increase in mindfulness, specifically by increases in awareness and nonreactivity.
Conclusions
Improvements in GAD symptoms resulting from MBSR are in part explained by increased levels of decentering.
Keywords: Mindfulness-Based Stress Reduction, Mindfulness Meditation, Generalized Anxiety Disorder, Decentering
I. Introduction
Mindfulness training, adapted from Buddhist meditation practices, teaches participants to increase awareness of present-moment experiences, including thoughts, emotions, and physical sensations, with a gentle and accepting attitude (Bishop et al., 2004). Mindfulness-based interventions have increased in popularity in the last several years and some of their core components have been integrated into a variety of behavioral interventions, including acceptance and commitment therapy (ACT; S. C. Hayes, Strosahl, & Wilson, 1999), dialectical behavior therapy (Linehan, 1993), and mindfulness-based stress reduction (MBSR; Kabat-Zinn, 1982; Kabat-Zinn, 1990). Results from both controlled and uncontrolled studies have demonstrated the efficacy of mindfulness-based interventions for stress and anxiety in a variety of patient populations (e.g., Hofmann, Sawyer, Witt, & Oh, 2010).
More recently, researchers have begun to examine the mechanisms, or therapeutic processes, by which these interventions exert their beneficial health effects. One candidate mechanism, or process, is dispositional mindfulness (i.e., the tendency to be aware of one's present-moment experiences with a non-judgmental attitude; Bishop et al., 2004). Although mechanisms of therapeutic action are most rigorously examined using formal mediation techniques or tests of indirect effects (e.g., causal steps approach using Baron and Kenny method), it is not uncommon to study simultaneous changes in process variables and outcome variables as a crude test of mediation. For instance, increases in mindfulness have been found to be associated with increases in well-being (Splevins, Smith, & Simpson, 2009) and decreases in depressed mood, stress, medical symptoms, and anxiety symptoms (Dobkin & Zhao, 2011; Goldin, Ziv, Jazaieri, & Gross, 2012). Additionally, although they were not able to test for true mediation, researchers found that increases in dispositional mindfulness accounted for reductions in anxiety and stress following a mindfulness-based intervention among patients with anxiety disorders (Vollestad, Sivertsen, & Nielsen, 2011). A second study found that changes in mindfulness preceded changes in mental health outcomes, raising the possibility that reductions in distress occurred as a result of earlier increases in mindfulness (Baer, Carmody, & Hunsinger, 2012). More compelling are results from a randomized, wait-list controlled study of MBSR for adults with general psychological distress in which mindfulness partially mediated improvements in quality of life and reductions in stress (Baer et al., 2012; Nyklicek & Kuijpers, 2008).
Another putative therapeutic mechanism in mindfulness-based treatments is decentering. Decentering is a metacognitive capacity of individuals to observe items that arise in the mind (e.g., thoughts, feelings, memories, etc.) as mere psychological events (Fresco, Moore, et al., 2007; Fresco, Segal, Buis, & Kennedy, 2007; Teasdale et al., 2002). Decentering promotes disengagement from internal experiences (i.e., an intense emotion, its corresponding motivational impetus, and associated maladaptive self-referential processing) in favor of adopting a more distanced perspective. This ability also involves recognizing that one’s thoughts, feelings, and urges are transient internal events rather than inherent, permanent aspects of the self or accurate representations of reality (Fresco, Moore, et al., 2007; Segal, Williams, & Teasdale, 2002). Some have noted that decentering and mindfulness are theoretically similar constructs (Carmody, Baer, E, & Olendzki, 2009); however, mindfulness involves bringing enhanced awareness coupled with an attitude of nonjudgment, whereas decentering more specifically refers to the ability to adopt a psychologically distanced stance. Studies report psychological benefits from promoting distance from the self in time (e.g., viewing inner experiences as temporary; Watkins, Teasdale, & Williams, 2000) and distance from the self in space (e.g., viewing inner experiences as physical objects that are separate from oneself; Kalisch et al., 2005). A series of studies utilizing a self-report measure of decentering (Fresco, Moore, et al., 2007) reveal that, as compared to healthy control participants, patients with major depressive disorder evidence lower levels of decentering (Fresco, Moore, et al., 2007) and demonstrate gains in decentering following treatment with cognitive behavioral therapy (CBT) but not antidepressant medication (ADM) (Fresco, Segal, et al., 2007). Further, gains in decentering during acute treatment with CBT (Fresco, Segal, et al., 2007) or prophylactic treatment with mindfulness-based cognitive therapy (MBCT) (Bieling et al., 2012) are predictive of a more durable treatment response. Although these studies provide preliminary evidence that decentering might at least partially mediate treatment outcomes, to our knowledge, this mediation hypothesis has not yet been tested nor have decentering and mindfulness been jointly examined as mediators of outcome in a study utilizing mindfulness-based treatment.
In sum, mindfulness-based interventions are effective in decreasing symptoms in a range of disorders including anxiety disorders, but the psychological mechanisms of mindfulness-based interventions and MBSR specifically are not fully understood. Although improvements in mindfulness are thought to mediate symptom improvements, other mechanisms of action such as decentering may mediate symptom reduction.
In the current study, we examined both mindfulness and decentering as mediators of outcome for patients receiving either MBSR or an attention control class as part of a randomized controlled trial evaluating the efficacy of MBSR for adults with generalized anxiety disorder (GAD; Hoge et al., 2013). GAD is a pervasive anxiety disorder characterized by chronic worry about several topics, along with physiological arousal symptoms such as difficulty concentrating, restlessness, and sleep disruption. MBSR was proposed as a treatment for GAD because of the intervention’s focus on the present moment, rather than the past-oriented ruminations and future-oriented worries that tend to be the attentional focus of individuals with GAD. Furthermore, individuals with GAD have lower levels of mindfulness compared to healthy controls (Roemer et al., 2009). Thus, increasing mindfulness may help decrease GAD anxiety symptoms. Given the ruminative nature of worry in GAD and the difficulty in separating from those thoughts (Marino, Lunt, & Negy, 2008), increases in decentering could also play a role in symptom improvement. Accordingly, we hypothesized that both mindfulness and decentering would be significant mediators of symptom reduction associated with MBSR.
II. Method
A. Procedures and Participants
The procedures of the parent randomized controlled trial have been extensively described previously (Hoge et al., 2013). Briefly, individuals age 18 and older with GAD, as determined by the Structured Clinical Interview for the DSM-IV (SCID) (First, Spitzer, & Williams, 2002), were randomized to either a slightly modified Mindfulness-Based Stress Reduction (MBSR) or Stress Management Education (SME). Participants were recruited by clinical referral and media advertisements. All study procedures were approved by the MGH/Partners Health Care institutional review board.
Exclusion criteria included lifetime history of psychotic disorder, intellectual disability, organic medical disorders, bipolar disorder, post-traumatic stress disorder or obsessive compulsive disorder; current alcohol or substance abuse or dependence; significant suicidal ideation or behaviors; and concurrent psychotherapy for GAD.
Participants to the present study were a subgroup (n=38) of the parent RCT sample that also had completed measures of decentering and mindfulness. (This scale was added to the study while already underway, resulting in a smaller sample for this mediation analysis than the full RCT sample.) Of this subgroup, 21 (55%) were women, 29 (76%) were White, and the mean (SD) age was 37.6 (11.7). There were no differences between this subsample and the full RCT sample in demographic variables (all p’s >0.29, all Chi2 < 0.59, and t-values < 1.3, which are comparable to Cohen’s d <0.24).
Mindfulness-Based Stress Reduction (MBSR)
The MBSR is an 8-week group-based intervention with a single weekend “retreat” day and daily home practice guided by audio recordings. In-class practices (breath-awareness, a body-scan, and gentle Hatha yoga) are used to cultivate awareness of internal present-moment experiences with an accepting, non-judgmental stance. The MBSR course was modified for this clinical population with the shortening of the “retreat” day to 4 hours, and the shortening of home exercises from 40 minutes to 20 minutes (for details, see Hoge et al., 2013). The SME was designed as an active control intervention for MBSR to control for the non-specific effects of treatment, such as group support, attention from the instructor, and participants’ expectations. The course focuses on improving overall health and wellness through education about diet, exercise, sleep, time management, and resilience, but it does not contain any meditation or other mind-body intervention. SME also included a ‘half-day of stress reduction’ with additional components, such as a stability ball exercise class and a dietician’s lecture.
B. Measures
1. Outcome Measures
Results from our previously published RCT revealed that MBSR was efficacious in reducing self-reported anxiety symptoms (Hoge et al., 2013). To parallel these findings, we chose self-reported anxiety symptoms and worry as the primary outcomes of interest for the present study. The 21-item self-report Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988) was used to assess anxiety at baseline and week 8 (endpoint). Items on the BAI are scored on a 4-point Likert type scale. Total scores range from 0 to 63, with higher scores indicating increased anxiety. The 15-item self-report Penn State Worry Questionnaire- Past Week (PSWQ-PW; Stober & Bittencourt, 1998) was used to assess worry at baseline and endpoint. Items on the PSWQ-PW are scored on a 7-point Likert-type scale. Total scores range from 0 to 90, with higher scores indicating more severe worry.
2. Potential mediators
Mindfulness
The 39-item Five Facet Mindfulness Questionnaire (FFMQ; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) was used to assess change in mindfulness. Participants rate items on a 5-point Likert-type scale (1 = never or very rarely true, 5 = very often or always true) and total scores range from 39 to 195, with higher scores indicating greater mindfulness. Prior factor analyses have yielded five facets of mindfulness: observing (attending to or noticing internal and external stimuli such as sensations, emotions, cognitions, sights, sounds, and smells); describing (mentally labeling these stimuli with words); acting with awareness (attending to one’s current actions, as opposed to behaving automatically or absent-mindedly); non-judging of inner experience (refraining from evaluation of one’s sensations, cognitions, and emotions); and non-reactivity to inner experience (allowing thoughts and feelings to come and go, without getting caught in them or reacting to them). Internal consistency was good at baseline (Cronbach’s alpha = 0.86) and follow-up (Cronbach’s alpha = 0.92).
Decentering
Decentering was assessed using the 11-item decentering subscale of the Experiences Questionnaire (also called “Experiences Questionnaire, Wider Experiences”) (Fresco, Moore, et al., 2007). This subscale comprises 11 items that are scored on 5-point Likert-type scales, yielding a total score ranging from 11 to 55. Higher scores reflect greater decentering. Internal consistency for the decentering subscale was good (Cronbach’s alpha = 0.83).
C. Statistical Analysis
Data analysis was performed using STATA version 12.1 (College Station, Texas). A mean imputation method with 15% or less missing items for each instrument was employed (Brannan, Heflinger, & Bickman, 1997) (9 subjects had missing questionnaire items). Pearson’s correlations and paired samples t-tests were conducted to characterize the overall relationship between variables. To assess the possibility of a meditational effect of pretreatment to posttreatment differences in mindfulness and decentering on differences in anxiety, we employed a multiple mediation model. Multiple mediation is analogous to a regression that examines the impact of multiple predictors. The primary advantage of multiple mediation is that one can examine the degree to which specific variables mediate the relationship between an independent and dependent variable, while controlling for the presence of other mediators. As has been recommended (see MacKinnon, Krull, & Lockwood, 2000; Preacher & Hayes, 2008), the multiple mediation analysis was accompanied by simple mediation analyses to bypass the issues that suppression effects can obscure possible indirect effects of individual mediators.
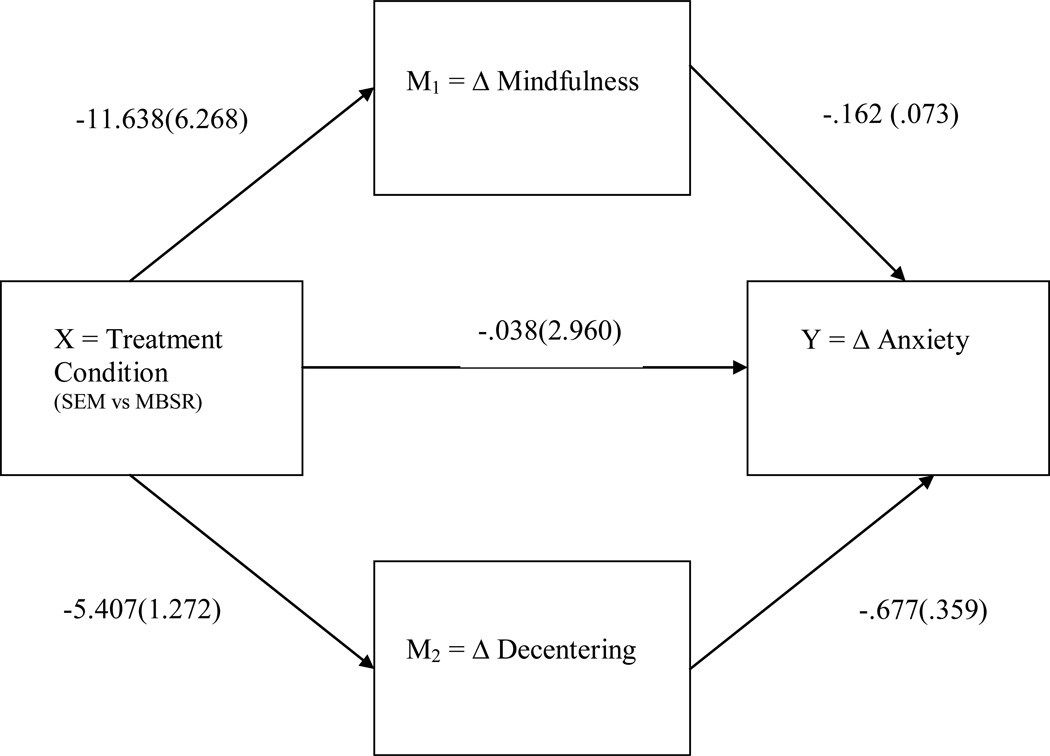
To compute an estimate of the indirect effects, we employed a bootstrapping method developed by Preacher and Hayes (2004, 2008) (see Figure 1). Bootstrapping is a nonparametric resampling method that bypasses assumptions of normality common to traditional tests of mediation and is thus more powerful, particularly with smaller samples (Preacher & Hayes, 2004, 2008). A causal step approach would have severely limited our power (A. F. Hayes, 2009) Specifically, 4,000 samples of the original size were taken from the obtained data (with replacement after each specific number was selected) and indirect effects were calculated in each sample. The mean indirect effect computed over each of these 4,000 samples was used to compute the point estimate. The bias corrected and accelerated 95% confidence intervals (i.e., with z score-based corrections for bias due to the underlying distribution) were then examined, and if these intervals did not contain zero, the point estimate of the indirect effect was considered significant. For all other analyses, the level of statistical significance was set to 0.05 (two-tailed, except for between group differences on anxiety and worry that was one-tailed, as we were replicating in a smaller subsample results reported in the overall sample).
Figure 1.
Illustration of multiple mediation model. Coefficients indicate regression weights B(SE)
III. Results
Relationship between MBSR, Potential Mediators, and Treatment Outcomes
The mean (SD) BAI, decentering and mindfulness baseline, endpoint, and change scores are reported in Table 1. Preliminary correlation analyses found that change in GAD symptom severity was strongly and inversely associated with change in mindfulness (r = −0.54, p<0.001) and change in decentering (r = −0.53, p<0.001). Change in mindfulness and in decentering were also correlated (r=0.56, p<0.001). Although the baseline BAI scores were higher in the MBSR group compared to SME (d=0.49), there were no significant differences between individuals randomized to MBSR compared to those assigned to SME on any of the variables at baseline. Individuals in the MBSR group exhibited a significantly greater change in decentering levels (t(36) = 4.13, p<0.001) and greater change in mindfulness levels (t(36)= 1.81, p=0.079) than individuals in the SME group (see Table 1). Effect sizes for change in BAI and PSWQ were similar to those found in the parent RCT (BAI: d = 0.71 vs. d = 0.74 in parent; PSWQ: d = 0.79 vs. 0.63 in parent) for MBSR. Between group differences on BAI change (t= −1.83, p=0.038) were significant, however, this was not the case for change in PSWQ (t=−0.64, p=0.26).
Table 1.
Group Means for MBSR and SME Treatments
| Overall sample [n=38] |
MBSR [n=19] |
SME [n=19] |
t | p | |||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||||
| BAI | pre | 15.9 | 8.9 | 18.1 | 9.7 | 13.8 | 7.6 | −1.51 | 0.140 |
| post | 11.2 | 7.0 | 10.6 | 8.1 | 11.8 | 5.8 | 0.53 | 0.602 | |
| change | −4.7 | 9.6 | −7.5 | 10.5 | −2.0 | 7.8 | −1.83 | 0.037 | |
| Worry | pre | 67.2 | 8.9 | 66.6 | 10.2 | 67.9 | 7.7 | 0.44 | 0.662 |
| post | 59.5 | 11.6 | 57.8 | 11.9 | 61.2 | 11.3 | 0.89 | 0.380 | |
| change | 7.74 | 9.8 | 8.8 | 10.3 | 6.7 | 9.4 | −0.64 | 0.262 | |
| Decentering | pre | 28.9 | 6.8 | 29.1 | 8.2 | 28.8 | 5.4 | −0.11 | 0.912 |
| post | 34.3 | 6.7 | 37.1 | 7.6 | 31.4 | 4.1 | −2.85 | <0.01 | |
| change | 5.3 | 4.8 | 8.0 | 4.8 | 2.6 | 3.1 | 4.14 | <0.001 | |
| Mindfulness | pre | 109.1 | 17.4 | 109.8 | 19.1 | 108.2 | 15.9 | −0.28 | 0.777 |
| post | 120.4 | 19.5 | 127.1 | 21.0 | 113.8 | 15.6 | −2.21 | 0.034 | |
| change | 11.4 | 20.4 | 17.2 | 25.8 | 5.53 | 11.0 | 1.81 | 0.079 | |
Mediation Analyses
Anxiety Symptoms
Separated bootstrapping analyses of the individual mediators indicated that there was a significant indirect effect of MBSR on reductions in BAI score through change in decentering and change in mindfulness (See Table 2).
Table 2.
Bootstrapped Point Estimates and Confidence Intervals for Total and Specific Indirect Effects of Change in Decentering and Mindfulness at Post-Treatment as Mediators of Change in Anxiety at Post-Treatment
| Product of coefficients | Bootstrapping Bias-Corrected and accelerated 95% Confidence Interval |
||||||
|---|---|---|---|---|---|---|---|
| Outcome: BAI | Point estimate | SE | Z | p* | Lower | Upper | |
| Single Mediator Analyses | |||||||
| Change in Mindfulness | 2.69 | 2.16 | 1.25 | 0.213 | .013 | 8.973 | |
| Change in Decentering | 5.84 | 2.68 | 2.18 | 0.029 | 2.037 | 13.443 | |
| Multiple Mediator Analysis | |||||||
| Change in Mindfulness | 1.89 | 1.74 | 1.09 | 0.277 | −.057 | 7.171 | |
| Change in Decentering | 3.66 | 1.88 | 1.95 | 0.051 | .682 | 8.377 | |
| Total Indirect | 5.549 | 2.64 | 2.10 | 0.035 | 1.555 | 12.306 | |
| Multiple Mediator Analysis | |||||||
| Change in Observing | −.46 | 2.95 | −.16 | .88 | −5.86 | 5.49 | |
| Change in Describing | .38 | 1.48 | .26 | .80 | −1.26 | 4.40 | |
| Change in Awareness | −.20 | 1.20 | −.17 | .87 | −3.22 | 1.59 | |
| Change in Non-judging | 1.00 | 1.89 | .53 | .60 | −2.26 | 5.54 | |
| Change in Non-reactivity | −1.1 | 1.75 | −.64 | .52 | −7.27 | 1.02 | |
| Change in Decentering | 4.17 | 2.49 | 1.68 | .09 | .50 | 10.74 | |
| Outcome: PSWQ | Point estimate | SE | Z | p* | Lower | Upper | |
| Single Mediator Analyses | |||||||
| Change in Mindfulness | 2.66 | 1.66 | 1.60 | 0.109 | 0.225 | 6.06 | |
| Change in Decentering | 3.66 | 2.24 | 1.63 | 0.103 | −.537 | 8.756 | |
| Multiple Mediator Analysis | |||||||
| Change in Observing | .41 | .60 | .69 | .491 | −.54 | 1.97 | |
| Change in Describing | .38 | .53 | .71 | .477 | −.32 | 1.92 | |
| Change in Awareness | .76 | .59 | 1.27 | .20 | .01 | 2.59 | |
| Change in Non-judging | .03 | .28 | .12 | .90 | −.33 | .83 | |
| Change in Non-reactivity | .96 | .66 | 1.46 | .15 | .06 | 2.92 | |
Notes:
BAI: Beck Anxiety Inventory
PSWQ: Penn State Worry Questionnaire
p values are included for completeness, but statistical significance was determined by examining bias-corrected and accelerated 95% Confidence Intervals
When both mediators were examined simultaneously, results from our multiple mediator mediation analysis revealed that the indirect effect through increases in decentering remained significant; however, the indirect effect through change in mindfulness was no longer significant suggesting that decentering may be a unique independent mediator of the effect of MBSR (see Table 2 and Figure 1). Conducting a similar analysis using the FFMQ subscales instead of the FFMQ total score did not change the pattern of result (i.e., change in decentering was the sole significant mediator).
Worry
Separated bootstrapping analyses of the individual mediators indicated that there was a significant indirect effect of MBSR on reductions in PSWQ score through change in mindfulness (See Table 2). Next, in order to examine whether change in certain dimensions of the FFMQ specifically mediated change in PSWQ score, we conducted a multiple mediation analysis with the five subscales of the FFMQ and found that only non-reactivity to inner experience (B = .96, SE = .66; BCa 95% CI = .066; 2.92) and acting with awareness were significant mediators (B = .76, SE = .59; BCa 95% CI = .01; 2.59), while observing (B = .41, SE = .60; BCa 95% CI = −.54; 1.97), describing (B = .38, SE = .53; BCa 95% CI = −.32; 1.92), and non-judging of inner experience (B = .03., SE = .28; BCa 95% CI = −.33; .83) were not.
IV. Discussion
In this sample of patients with GAD who were trained in MBSR or received an attention control, we found evidence that changes in both decentering and mindfulness may mediate the effect of MBSR on symptoms of GAD. In particular, results from our study suggest that MBSR promotes reductions in anxiety (i.e., BAI score) through increases in decentering, but reduces worry (i.e., PSWQ score) through increases in mindfulness, specifically via increases in awareness and nonreactivity. These results lead us to draw three important conclusions. First, these results provide evidence that mindfulness and decentering are indeed distinct constructs. Second, MBSR promotes reductions in GAD symptoms through different mechansims, namely mindfulness and decentering, suggesting that both skills are crucial components of successful GAD treatment. Finally, decentering and mindfulness appear to differentially influence symptoms of GAD. Specifically, decentering appears to be a process by which MBSR reduces anxiety, especially physiological anxiety (which is the primary construct measured by BAI), while mindfulness (awareness and nonreactivity) appears to be a key process by which MBSR reduces worry. Concerning the role of decentering in mediating outcomes in MBSR, these findings extend previous findings suggesting that decentering predicts improvements (or lack of relapse) in psychological symptoms after MBSR and MBCT (Bieling et al., 2012; Carmody et al., 2009). It could be that having a psychologically distanced stance buffers individuals from the distress associated with physical signs of anxiety. Although they were not examining individuals with anxiety conditions per se, a recent study found that decentering was beneficial among individuals with chronic pain (McCracken, Gutierrez-Martinez, & Smyth, 2013). Taken together, these findings suggest that decentering may be a crucial process by which psychotherapies target and alleviate distressing physical sensations. Decentering in response to anxiety may make one less prone to the detrimental consequences that can result from focusing attention on anxiety symptoms, which has been known to exacerbate negative affect (Mor & Winquist, 2002). The current study also found that mindfulness mediated reductions in worry. Specifically, awareness and nonreactivity, emerged as two key mechanisms by which MBSR reduces worry. These findings are in concert with results of a recent study which found that nonreactivity, nonjudging, and acting with awareness, were significantly and negatively associated with worry (Fisak & von Lehe, 2012). Similar to what they concluded, it could be that individuals who have a more mindful response to worries are less likely to experience the associated emotional distress that accompanies worry. For example, by not reacting to the worries, individuals may be less likely to attempt to control or suppress the worry, which can paradoxically increase distress (Abramowitz, Tolin, & Street, 2001). Lastly, these results provide evidence that mindfulness and decentering are indeed distinct constructs.
Given these findings showing that MBSR is associated with gains in decentering and improvements in mindfulness (nonreactivity and acting with awareness), an important future direction is to develop treatments that deliberately and focally promote decentering and mindfulness for anxiety and depressive disorders characterized by lack of this type of capacity. One example is Emotion regulation therapy (ERT; Fresco, Mennin, Heimberg, & Ritter, 2013; Mennin, Fresco, Heimberg, & Ritter, Under Review), which integrates CBT with emotion-focused interventions, and develops regulatory capacities including attending, allowing, decentering, and reframing. Recent open trial findings demonstrate that GAD patients treated with ERT show significant decreases in symptom severity, worry and impairment, but increases in decentering, quality of life and emotion regulation abilities (Mennin et al., Under Review). Another cognitive-behavioral psychotherapy is Acceptance-Based Behavior Therapy (ABBT), which encourages use of mindfulness exercises, teaching distancing from thoughts, and engagement in important, values-consistent activities; this treatment has demonstrated efficacy in treating GAD and in increasing decentering (Hayes-Skelton, Roemer, & Orsillo, 2012; Roemer, Orsillo, & Salters-Pedneault, 2008; Roemer, Williston, Eustis, & Orsillo, 2013).
Several limitations should be mentioned. First, findings are limited by small sample size, so they should be interpreted with caution. Second, there was only a small relative greater treatment effect of our active arm, MBSR, compared to the attention control treatment, SME. We believe that this was largely due to non-specific effects of treatment in the attention control (expectation bias, attention, group support). However, while the use of an attention control yields a smaller difference between groups, a strength of this design is that we can feel more confident that treatment differences are actually due to mindfulness meditation, rather than non-specific effects of treatment. A third limitation is that the nature of the assessments (pre- and post-treatment only) precludes us from establishing that change in decentering and mindfulness preceded change in anxiety. In addition, our anxiety symptom outcome measure, the BAI, has an emphasis on physiological arousal symptoms rather than a focus on the core symptoms of GAD. Therefore, it is possible that the BAI did not capture precisely the distress associated with GAD. Lastly, we studied a sample with GAD and therefore our findings are not necessarily generalizable to other conditions. Future studies could extend this research by examining these constructs in different populations. Such research would be particularly useful as contemporary paradigms seek to identify underlying dimensions of psychological functioning.
To our knowledge, this is the first study that jointly examined mindfulness and decentering as mechansims of action in MBSR for GAD. In conclusion, we found that decentering mediated anxiety symptom reduction, and that mindfulness mediated reductions in worry, in a group of patients with GAD. This study suggests that these constructs are empirically distinct and are key processes by which individuals with GAD experience reductions in symptoms. Identifying mechanisms of action in psychosocial treatments is important not only because it provides information about how existing treatments work, but also because it informs the development of new interventions, which is particularly important in the case of chronic, difficult-to-treat disorders.
Table 3.
Correlation Matrix for Change Scores of All Measures
| BAI | PSWQ | Decentering | |
|---|---|---|---|
| BAI | - | ||
| PSWQ | 0.36* | - | |
| Decentering | −0.53* | −0.29 | - |
| FFMQ | −0.54*** | −0.47** | 0.56*** |
| Observing | −0.48** | −0.41* | 0.63*** |
| Describing | −0.41* | −0.38* | 0.41* |
| Awareness | −0.31 | −0.38* | 0.32 |
| Non-Judging | −0.57*** | −0.35* | 0.41* |
| Non-reactivity | −0.45** | −0.44** | 0.59*** |
p<0.05;
p<0.01;
p<0.001
Acknowledgments
Funding/support: This study was primarily supported by grant K23AT4432 from the National Center on Complementary and Alternative Medicine, National Institutes of Health (Hoge, P.I.). The Highland Street Foundation provided additional support to Drs. Simon and Bui.
Author N. Simon lists the following financial relationships: Consulting: MGH Psychiatry Academy. Research Grants: American Cancer Society, American Foundation for Suicide Prevention, Department of Defense, Highland Street Foundation. Equity (Spouse only): Elan, Dandreon, G Zero, Gatekeeper.
Footnotes
Disclosure Statement: Authors E. Hoge, E. Bui, E. Goetter, D. Robinaugh, R. Ojserkis, and D. Fresco state that they have no financial or other relationships which would create a conflict of interest with regard to this manuscript.
Protection of Research Subjects: Consent was obtained by study staff before the beginning of study procedures, and the Partners Human Research Committee approved the study before initiation. No animals were involved in this study.
References
- Abramowitz JS, Tolin DF, Street GP. Paradoxical effects of thought suppression: a meta-analysis of controlled studies. Clin Psychol Rev. 2001;21(5):683–703. doi: 10.1016/s0272-7358(00)00057-x. [DOI] [PubMed] [Google Scholar]
- Baer RA, Carmody J, Hunsinger M. Weekly Change in Mindfulness and Perceived Stress in a Mindfulness-Based Stress Reduction Program. J Clin Psychol. 2012 doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Bieling PJ, Hawley LL, Bloch RT, Corcoran KM, Levitan RD, Young LT, Segal ZV. Treatment-specific changes in decentering following mindfulness-based cognitive therapy versus antidepressant medication or placebo for prevention of depressive relapse. J Consult Clin Psychol. 2012;80(3):365–372. doi: 10.1037/a0027483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SRB, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A Proposed Operational Definition. Clin Psychol Sci Prac. 2004;11(3):230–241. [Google Scholar]
- Brannan AM, Heflinger CA, Bickman L. The Caregiver Strain Questionnaire: Measuring the Impact on the Family of Living with a Child with Serious Emotional Disturbance. Journal of Emotional and Behavioral Disorders. 1997;5(4):212–222. [Google Scholar]
- Carmody J, Baer RA, E LBL, Olendzki N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. J Clin Psychol. 2009;65(6):613–626. doi: 10.1002/jclp.20579. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Zhao Q. Increased mindfulness--the active component of the mindfulness-based stress reduction program? Complement Ther Clin Pract. 2011;17(1):22–27. doi: 10.1016/j.ctcp.2010.03.002. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, G M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders-Patient Edition (SCID-I/P, 11/2002 revision) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 2002. [Google Scholar]
- Fisak B, von Lehe AC. The Relation Between the Five Facets of Mindfulness and Worry in a Non-clinical Sample. Mindfulness. 2012;3(1):15–21. [Google Scholar]
- Fresco DM, Mennin DS, Heimberg RG, Ritter M. Emotion Regulation Therapy for Generalized Anxiety Disorder. Cognitive and Behavioral Practice. 2013;20(3):282–300. doi: 10.1016/j.cbpra.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Moore MT, van Dulmen MH, Segal ZV, Ma SH, Teasdale JD, Williams JM. Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behav Ther. 2007;38(3):234–246. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. J Consult Clin Psychol. 2007;75(3):447–455. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- Goldin P, Ziv M, Jazaieri H, Gross JJ. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: effects on the self-referential brain network in social anxiety disorder. Front Hum Neurosci. 2012;6:295. doi: 10.3389/fnhum.2012.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton SA, Roemer L, Orsillo SM. Decentering as a common mechanism across two behavioral treatments for generalized anxiety disorder. In: SA Hayes-Skelton (Chair), Processes and mechanisms of action in a randomized controlled trial of two behavioral therapies for generalized anxiety disorder; Paper presented at the Presented as the annual meeting of the Society for Psychotherapy Research; Virginia Beach, VA. 2012. [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. New York: Guilford Press; 1999. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, Simon NM. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry. 2013;74(8):786–792. doi: 10.4088/JCP.12m08083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Bantam Dell; 1990. [Google Scholar]
- Kalisch R, Wiech K, Critchley HD, Seymour B, O'Doherty JP, Oakley DA, Dolan RJ. Anxiety reduction through detachment: subjective, physiological, and neural effects. J Cogn Neurosci. 2005;17(6):874–883. doi: 10.1162/0898929054021184. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Skills for Training Manual for Treating Borderline Personality Disorder. New York: Guilford Press; 1993. [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1(4):173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino TL, Lunt RA, Negy C. Thought-action fusion: a comprehensive analysis using structural equation modeling. Behav Res Ther. 2008;46(7):845–853. doi: 10.1016/j.brat.2008.03.005. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Gutierrez-Martinez O, Smyth C. "Decentering" reflects psychological flexibility in people with chronic pain and correlates with their quality of functioning. Health Psychol. 2013;32(7):820–823. doi: 10.1037/a0028093. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM, Heimberg RG, Ritter M. An Open Trial of Emotion Regulation Therapy For Generalized Anxiety Disorder and Comorbid Depression. doi: 10.1002/da.22377. (Under Review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor N, Winquist J. Self-focused attention and negative affect: a meta-analysis. Psychol Bull. 2002;128(4):638–662. doi: 10.1037/0033-2909.128.4.638. [DOI] [PubMed] [Google Scholar]
- Nyklicek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Ann Behav Med. 2008;35(3):331–340. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Roemer L, Lee JK, Salters-Pedneault K, Erisman SM, Orsillo SM, Mennin DS. Mindfulness and emotion regulation difficulties in generalized anxiety disorder: preliminary evidence for independent and overlapping contributions. Behav Ther. 2009;40(2):142–154. doi: 10.1016/j.beth.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: evaluation in a randomized controlled trial. J Consult Clin Psychol. 2008;76(6):1083–1089. doi: 10.1037/a0012720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Williston SK, Eustis EH, Orsillo SM. Mindfulness and acceptance-based behavioral therapies for anxiety disorders. Curr Psychiatry Rep. 2013;15(11):410. doi: 10.1007/s11920-013-0410-3. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- Splevins K, Smith A, Simpson J. Do improvements in emotional distress correlate with becoming more mindful? A study of older adults. Aging Ment Health. 2009;13(3):328–335. doi: 10.1080/13607860802459807. [DOI] [PubMed] [Google Scholar]
- Stober J, Bittencourt J. Weekly assessment of worry: an adaptation of the Penn State Worry Questionnaire for monitoring changes during treatment. Behav Res Ther. 1998;36(6):645–656. doi: 10.1016/s0005-7967(98)00031-x. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. J Consult Clin Psychol. 2002;70(2):275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Vollestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behav Res Ther. 2011;49(4):281–288. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Watkins E, Teasdale JD, Williams RM. Decentring and distraction reduce overgeneral autobiographical memory in depression. Psychol Med. 2000;30(4):911–920. doi: 10.1017/s0033291799002263. [DOI] [PubMed] [Google Scholar]