Abstract
Background
Apolipoprotein D (ApoD) has been proposed as a predictor of breast cancer recurrence among estrogen receptor-positive (ER+), tamoxifen-treated patients.
Methods
We conducted a population-based case-control study nested in a population of 11,251 women aged 35–69 years at diagnosis with Stage I–III breast cancer between 1985 and 2001 on Denmark’s Jutland Peninsula and registered with the Danish Breast Cancer Cooperative Group. We identified 541 recurrent or contralateral breast cancers cases among women with ER+ disease treated with tamoxifen for at least 1 year and 300 cases in women with ER– disease never treated with tamoxifen. We matched one control subject per case and assessed ApoD expression in the tumor cell nucleus and cytoplasm using tissue microarray immunohistochemistry. We computed the odds ratio (OR) associating ApoD expression with recurrence and adjusted for potential confounding using logistic regression.
Results
Cytoplasmic ApoD expression was seen in 68% of ER+ tumors, in 66% of ER– tumors, and in 66% of controls across both groups. In women with ER+ tumors, the associations of cytoplasmic ApoD expression with recurrence (OR = 1.0; 95% CI = 0.7 to 1.4) and increasing cytoplasmic expression with recurrence (OR = 1.0; 95% CI = 0.996 to 1.003) were null, as were those for women with ER– tumors. Associations for nuclear ApoD expression and combined nuclear and cytoplasmic expression were similarly near-null.
Conclusion
ApoD expression is likely not a predictor of recurrence in tamoxifen-treated patients.
Impact
This study eliminates the previously suggested marker ApoD as a predictor of recurrence among tamoxifen-treated women.
Introduction
Breast cancer accounts for the highest number of cancer cases among women worldwide, and is the second leading cause of cancer death.[1, 2] Between two-thirds and three-quarters of breast tumors express the estrogen-receptor-alpha (ERα) protein.[3, 4] Patients with ER+ breast cancers usually receive adjuvant anti-estrogen therapy, typically tamoxifen—a selective ER modulator—or an aromatase inhibitor. [5–11] Tamoxifen selectively binds to the ligand-binding domain of the ER, blocking estrogen’s ability to bind and induce proliferation of the cancer cells.[12–14]
In spite of tamoxifen’s measurable positive effect on breast cancer prognosis, only about 70% of all ER+ breast cancers respond to anti-estrogen therapies.[12, 15] In addition, many breast cancers that initially respond eventually develop resistance to these therapies.[16] Effective use of anti-estrogen therapy may depend on the ability to subtype receptor-positive breast cancers based on their biomarker profiles.[15, 17–19] Despite a number of studies on the subject, to date, no biomarker has been translated into clinical practice to predict which tamoxifen-treated patients are at high risk for recurrence.[20]
Apolipoprotein D (ApoD) expression may be predictive of recurrence among tamoxifen-treated patients.[21–24] ApoD is a 29-kDa glycoprotein involved in transport of hydrophobic ligands and is ubiquitous in human tissue.[25–27] Molecular studies have demonstrated an inhibitory effect of the ER on ApoD, with up-regulation following tamoxifen treatment, likely through blockage of ER activity.[28] As a result, combined ER positivity and ApoD positivity could reflect a malfunctioning hormone receptor pathway, resulting in ineffective tamoxifen treatment and a higher risk for relapse.[27–31] Only two studies have explored the direct relation between ApoD expression and recurrence among tamoxifen-treated patients.[26, 32] We sought to examine precisely this association in a larger, well-characterized population.
Materials and methods
Patients
Using the Danish Breast Cancer Cooperative Group (DBCG) database, we collected information on 11,251 female residents of the Jutland Peninsula between the ages of 35 and 69 who were diagnosed with Stage I–III invasive breast cancer between 1985 and 2001.[33, 34] The DBCG ends routine follow-up of breast cancer patients at ten years. For the purposes of this study, data were collected beginning at one year after the date of diagnosis, and ending on the date of a first breast cancer recurrence, death from any cause, loss to follow-up due to emigration, after ten years, or September 1, 2006 (the end of the study’s follow-up period) by linkage to the Civil Registration System.[35, 36] All data were linked using Danish Personal Registration Numbers.
Patients were divided into two subgroups—those whose tumors showed expression of ER and who had been on tamoxifen therapy for at least one year, and those whose tumors did not show expression of ER, were not treated with tamoxifen, and who had survived for at least one year. All other patients were excluded, including patients who received neoadjuvant treatment, though this was highly uncommon during the study period in Denmark.[37] Tumors were considered ER+ if ≥10% of cells expressed the ER.
The DBCG data provided recurrence information, defined as breast cancer—including contralateral cancer—or distant metastases diagnosed after receipt of initial treatment. Because tamoxifen reduces the rate of local, distant, and contralateral recurrences, these were grouped under a global heading of”recurrence” for assessing the direct predictive effect of ApoD on recurrence via the tamoxifen pathway. For the purposes of this study, a “case” was defined as a recurrence that occurred within ten years of the initial diagnosis. Controls were free of recurrence at the time of matching, and were matched to cases on ER status, menopausal status, stage, calendar time of diagnosis, and county.
Patients were also excluded if they had insufficient or invalid tissue material that could not be scored on the tissue microarrays (TMAs). Invalid tissue included tumors that were non-invasive, such as cores with only ductal carcinoma in situ, cores that were excessively over stained, cores that were damaged or cores that were missing from the stained sections. In total, 371 patients were excluded because there was insufficient valid tissue for ApoD determination. After these exclusions for quality control, 1,267 women remained in the study, each tumor being represented by between one and four evaluable TMA cores.
Immunohistochemistry
Tissues were processed from formalin-fixed paraffin-embedded tissue blocks obtained from pathology department archives using sterile protocols designed to avoid cross-contamination. Cylindrical cores were sampled from each donor tumor and re-embedded into recipient TMA paraffin blocks using standard procedures. TMAs were constructed using a TMA Master (3DHistech Ltd., Budapest, Hungary) using 1 mm diameter cores. An asymmetrical design was employed, using liver and placental tissue tissue cores as TMA orientation markers and as controls. When possible, up to a maximum of three representative tumor cores and one marginal tissue core were sampled from each donor block (one block per patient), including a core with normal tissue for quality control.
We used immunohistochemistry to determine the subcellular expression intensity and location of ApoD. ApoD expression was detected using a rabbit monoclonal primary antibody at a 1:250 dilution, with thirty minutes of incubation time at room temperature (clone EPR2916, Abcam, Cambridge, UK). We performed heat induced epitope retrieval using a target retrieval solution with pH of 9. The visualization system used was Envision Flex, which uses 3,3’-diaminobenzidine as a chromogen and horseradish peroxidase as a labeled polymer. The stained TMA sections were scanned at 40x magnification with the Hamamatsu Nanozoomer 2.0HT in .ndpi format. Slides were converted with a beta version converter to conform to the 3DHistech software and uploaded to Panoramic Viewer TMA Module software.
Scoring of TMA cores
Laboratory personnel, including scorers, were blinded to all clinical information, including case or control status, ER status, and receipt of therapeutic agents. The stained TMA breast carcinoma sections were read and scored for Apo-D expression by three observers (one experienced pathologist (YH), and two trained students (DK and TJ)). Initially, 62 cores were independently scored by the three raters, and agreement was compared for each rater pair. For ascertainment of positive cytoplasmic staining, agreement was generally good, with an average concordance of 89%. Concordance of positive nuclear staining was lower, with 79% agreement on average, although the total number of positively stained nuclei in the test sample was low, leading to less precise measures of agreement. The pathologist reviewed all the TMA cores after they were initially scored by the two other raters, to maximize scoring consistency. Discordantly scored cores were discussed by all three raters and a consensus score was agreed. Cores were excluded if they were excessively torn, over-stained, or consisted exclusively of carcinoma in situ or normal tissue. If a combination of normal tissue and tumor was present, only the portion with tumor was scored for ApoD.
Definitions of analytical variables
ApoD cytoplasmic staining
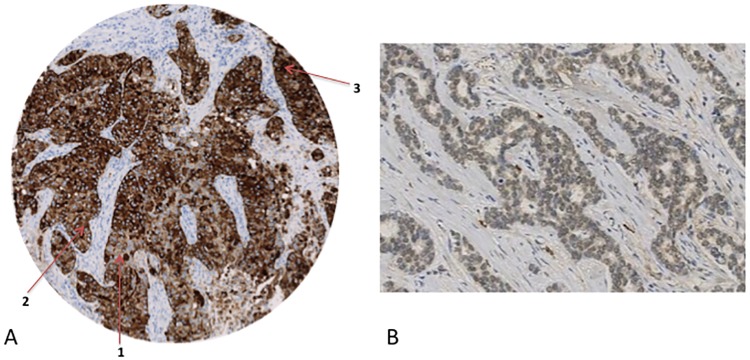
A semi-quantitative scoring system employing a histological score, or “H-score,” was used for all analyses, as described by Soiland et al.[38] Briefly, the H-score weights the proportion of tumor cells in each TMA core by the intensity of their staining according to a four-level ordinal scale (0/negative, 1/weak, 2/moderate, or 3/strong). Soiland et al. identified a threshold H-score of 0 as a significant cutoff for patients over seventy years of age. Thus, patients with an H-score of zero were considered to have no ApoD expression, while patients with an H-score >0 were considered to have ApoD present. Two variables were used separately in the analysis—one dichotomous variable specifying staining as negative versus positive, and one continuous variable with the H-score itself (1–300) to assess dose-response (Fig 1a).
Fig 1. ApoD staining determinationζ §.
§The source population consisted of 11,251 female residents of the Jutland Peninsula in Denmark aged 35–69 years who were diagnosed with Stage I, II, or III breast cancer between 1985 and 2001. ζ Brown signifies positive ApoD staining. A.Image depicts an immunohistochemically stained TMA core that was scored for cytoplasmic ApoD by the three raters as follows: 45% tumor cells weakly positive (1), 50% tumor cells moderately positive (2), and 5% tumor cells strongly positive (3). B. Image depicts a TMA core with widespread, weak nuclear staining.
ApoD nuclear staining
Nuclear staining was quantified using a simplified nuclear N-score, defined as the product between intensity of staining (1/light, 2/dark) and frequency of staining (0/negative, 1/<25% positive nuclei, 2/25+ positive nuclei). Two variables were used for this analysis as with cytoplasmic staining—one dichotomous (negative versus positive, cutoff of 0), and one continuous (1–4) using the nuclear H-score (Fig 1b).
Statistical analysis
All statistical analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC). All analyses were performed within strata of ER+/TAM+ and ER–/TAM– to isolate the association between ApoD and recurrence. The ER–/TAM– group was included to examine any direct prognostic effect of ApoD expression on recurrence. Crude frequencies were calculated within the two strata showing the proportion of cases and controls in various categories of ApoD staining, separated into nuclear and cytoplasmic staining. Conditional logistic regression was used to calculate measures of association, with recurrence as the outcome and ApoD staining status as the exposure variable. Odds ratios estimating the association of ApoD positivity in the nucleus or cytoplasm with recurrence were computed, controlling for covariates. Matched odds ratios (OR) were compared with those computed with additional adjustment for receipt of chemotherapy, receipt of radiation therapy, and type of surgery. Within continuous categorization of ApoD staining status, the OR was computed excluding the negative referent group to assess the presence of a dose-response. We replicated analyses within strata of stage to further assess the predictive value of ApoD. A probabilistic bias analysis was performed to account for potential misclassification of ApoD staining, the results and methods of which are presented in S1 File and S1 Table.
This study was approved by the Danish Data Protection Agency (journal number 2012-41-1170) and the Ethical Committee (record number 1-10-72-16-15).
Results
Descriptive statistics
The majority of women were either Stage II (45%) or III (53%) at diagnosis, with only 2% designated as Stage I according to standards set by the Union for International Cancer Control.[34] Approximately half of the women were between the ages of 55–64, with 24% in the 65–69 category, 22% in the 45–54 category, and only 3% of women between the ages of 35 and 44 years. Given the age distribution, only 6% of women were premenopausal (Table 1).
Table 1. Frequency and proportion of breast cancer recurrence case patients and matched control subjects within group strata*.
| Patient Characteristic | ER+/TAM+, No.(%) | ER-/TAM-, No.(%) | ||
|---|---|---|---|---|
| Recurrent Cases | Controls | Recurrent Cases | Controls | |
| Cytoplasmic ApoD Expression (H-Score) | ||||
| = 0 | 135 (32) | 144 (34) | 80 (34) | 77 (35) |
| >0 | 292 (68) | 280 (66) | 157 (66) | 146 (66) |
| Missing † | 114 | 117 | 63 | 77 |
| Nuclear ApoD Expression (H-Score) | ||||
| = 0 | 260 (61) | 258 (61) | 169 (71) | 165 (74) |
| >0 | 167 (39) | 166 (39) | 68 (29) | 58 (26) |
| Missing † | 114 | 117 | 63 | 77 |
| Joint ApoD Expressionζ | ||||
| = 0 | 115 (44) | 131 (46) | 76 (54) | 71 (58) |
| >0 | 147 (56) | 153 (54 | 64 (46) | 52 (42) |
| Missing † | 279 | 257 | 160 | 177 |
| Diagnosis Year§ | ||||
| 1985–1993 | 235 (43) | 234 (43.3) | 107 (36) | 100 (33) |
| 1994–1996 | 113 (21) | 112 (20.7) | 81 (27) | 83 (28) |
| 1997–2001 | 193 (36) | 195 (36) | 112 (37) | 117 (39) |
| Age category at diagnosis, yrs | ||||
| 35–44 | 13 (3) | 12 (2.8) | 52 (22) | 41 (18) |
| 45–54 | 92 (22) | 86 (20) | 94 (40) | 84 (38) |
| 55–64 | 221 (52) | 222 (52) | 67 (28) | 68 (31) |
| 65–69 | 101 (24) | 104 (25) | 24 (10) | 30 (13) |
| Menopausal Status at diagnosis§ | ||||
| Premenopausal | 34 (6.3) | 34 (6.3) | 121 (40) | 121 (40) |
| Postmenopausal | 507 (94) | 507 (94) | 179 (60) | 179 (60) |
| UICC tumor stage at diagnosis§ | ||||
| I | 8 (1.9) | 6 (1.4) | 14 (5.9) | 15 (6.7) |
| II | 194 (45) | 193 (46) | 128 (54) | 115 (52) |
| III | 225 (53) | 225 (53) | 95 (40) | 93 (42) |
| Nodal involvement at diagnosis | ||||
| 0 | 33 (6.1) | 39 (7.2) | 82 (27) | 110 (37) |
| 1–3 | 240 (44) | 251 (46) | 101 (34) | 76 (25) |
| 4–9 | 177 (33) | 196 (36) | 76 (25) | 84 (28) |
| 10+ | 91 (17) | 55 (10) | 41 (14) | 30 (10) |
| Histological grade | ||||
| I | 108 (20) | 144 (27) | 27 (9.0) | 23 (7.7) |
| II | 234 (43) | 215 (40) | 125 (42) | 98 (33) |
| III | 92 (17) | 57 (11) | 103 (34) | 106 (35) |
| IV | 107 (20) | 125 (23) | 45 (15) | 73 (24) |
| Missing | ||||
| Surgery type | ||||
| Breast-conserving surgery | 383 (90) | 368 (87) | 199 (84) | 181 (81) |
| Mastectomy | 44 (10) | 56 (13) | 37 (16) | 42 (19) |
| Missing | 0 | 0 | 1 | 0 |
| Radiation therapy | ||||
| Yes | 149 (35) | 150 (35) | 103 (44) | 90 (47) |
| No | 278 (65) | 274 (65) | 130 (56) | 102 (53) |
| Missing | 0 | 0 | 6 | 40 |
| Tamoxifen protocol, yrs | ||||
| 1 | 257 (48) | 261 (48) | ||
| 2 | 98 (18) | 92 (17) | ||
| 5 | 186 (34) | 188 (35) | ||
| Systemic adjuvant chemotherapy | ||||
| Yes | 53 (12) | 42 (9.9) | 203 (86) | 139 (62) |
| No | 374 (88) | 382 (90) | 34 (14) | 84 (38) |
| Current ER expression | ||||
| Positive | 397 (93) | 411 (97) | 59 (25) | 56 (25) |
| Negative | 30 (7.0) | 12 (2.8) | 177 (75) | 165 (74) |
| Not available† | 0.0 | 1 (0.2) | 1 (0.4) | 2 (0.9) |
*The source population consisted of 11,251 female residents of the Jutland Peninsula in Denmark aged 35–69 years who were diagnosed with Stage I, II, or III breast cancer between 1985 and 2001. Subjects were estrogen receptor positive and received at least 1 year of tamoxifen therapy (ER+/TAM+) or ER negative and never received tamoxifen therapy and survived at least 1 year after diagnosis (ER-/TAM-). ApoD = Apolipoprotein D; UICC = Union for International Cancer Control.
†No tissue available for assay or assay results indeterminate
§Variable included in risk set sampling to match control subjects to case patients.
ζJoint effect indicates combined nuclear and cytoplasmic dichotomous staining
Approximately half of the ER+ tumor patients were initially assigned to two-year tamoxifen treatment protocols according to the DBCG guidelines, with the remaining half split between one- and five-year protocols. Medical records often indicated a longer tamoxifen protocol compared to the registry, as patients likely were switched to the five-year protocol as evidence emerged supporting longer adjuvant treatment.[37] As expected, a much greater percentage of the ER– group was assigned to systemic chemotherapy treatment, as the overall prognosis for this subset of breast cancer patients was lower, and fewer adjuvant treatment options existed.
In both the ER+ and ER– strata, the percentage of women with some positive cytoplasmic ApoD expression was between 65% and 70%. Nuclear staining patterns differed somewhat between ER strata, with approximately 39% of ER+ tumors exhibiting positive nuclear staining, compared with 25–30% of ER– tumors (Table 1).
Model results
In both the ER+/TAM+ and ER–/TAM– strata, all matched associations between ApoD and breast cancer recurrence were near null in both the ER+/TAM+ and ER–/TAM– strata (Table 2). For cytoplasmic staining, both dichotomous coding of ApoD staining (matched OR = 1.0, 95% CI = 0.72, 1.39), as well as continuous coding assessing dose response (matched OR = 1.0, 95% CI = 0.998, 1.002) resulted in null associations. Similarly, nuclear staining also yielded near-null results both using dichotomous coding of ApoD staining (matched OR = 1.0, 95% CI = 0.75, 1.38) and continuous coding (matched OR = 0.99, 95% CI = 0.83, 1.18). The ER–/TAM– group also yielded near null associations that were almost identical to those in the ER+/TAM+ group. The associations estimating the effect of joint nuclear and cytoplasmic expression on recurrence were also near-null in both the ER+ stratum (matched OR = 0.87, 95% CI = 0.55, 1.38) and the ER– stratum (matched OR = 1.06, 95% CI = 0.54, 2.1). Associations were similarly null among women of all stages when examined separately (S2 Table)
Table 2. Associations between ApoD expression and breast cancer recurrence within strata*.
| ApoD Expression | ER+/TAM+ | ER-/TAM- | ||||
|---|---|---|---|---|---|---|
| Recurrent cases/controls or mean§ | Matched OR (95% CI)† | Adjusted OR (95% CI)‡ | Recurrent cases/controls or mean§ | Matched OR (95% CI)† | Adjusted OR (95% CI)‡ | |
| Joint Expression | ||||||
| = 0 | 115/131 | 76/71 | ||||
| >0 | 147/153 | 0.87(0.55, 1.38) | 1.14 (0.79, 1.65) | 65/52 | 1.06 (0.54, 2.10) | 1.29 (0.72, 2.32) |
| Cytoplasmic H-score | ||||||
| = 0 | 135/144 | 80/77 | ||||
| >0 | 292/280 | 1.00 (0.72,1.39) | 1.19 (0.83,1.50) | 157/146 | 0.98 (0.64,1.49) | 1.14 (0.74, 1.75) |
| Continuous | Mean: 85.77/87.29 | 1.00 (0.996, 1.003) | 1.00 (0.998,1.002) | Mean: 90.9/108.4 | 1.00 (0.995,1.003) | 1.00 (0.996, 1.001) |
| Nuclear H-score | ||||||
| = 0 | 260/258 | 169/165 | ||||
| >0 | 167/166 | 1.01 (0.74,1.38) | 1.05 (0.78,1.40) | 68/58 | 1.17 (0.71,1.92) | 1.25 (0.79, 2.00) |
| Continuous | Mean: 1.390/1.396 | 1.00 (0.65,1.55) | 1.03 (0.88,1.21) | Mean: 1.47/1.70 | 0.72 (0.38,1.37) | 1.01 (0.80, 1.26) |
*The source population consisted of 11,251 female residents of the Jutland Peninsula in Denmark aged 35–69 years who were diagnosed with Stage I, II, or III breast cancer between 1985 and 2001. Subjects were estrogen receptor positive and received at least 1 year of tamoxifen therapy (ER+/TAM+) or ER negative and never received tamoxifen therapy and survived at least 1 year after diagnosis (ER-/TAM-). ApoD = Apolipoprotein D; UICC = Union for International Cancer Control.
†Estimated using logistic regression; case patients were matched to controls on ER status, menopausal status, stage, calendar time of diagnosis, and county
‡Estimated using logistic regression with adjustment for time to recurrence or control selection, menopausal status, stage, receipt of chemotherapy, receipt of radiation therapy, and type of surgery.
§Mean for cases/controls provided for continuous variable, whereas frequency is provided for cases/controls for dichotomous exposure variable
Discussion
In spite of plausible biological hypotheses and the results of earlier studies, we did not observe an association between tumor ApoD expression and recurrence among ER+, tamoxifen-treated patients. The effect was near null in all categories of ApoD localization—nuclear, cytoplasmic or both—and in both dichotomous and continuous categorizations of staining. Associations were near null among ER+ tumor patients and ER– tumor patients, with indiscernible differences in estimates between the two groups. This further suggests that ApoD positivity in ER+ patients is not reflective of a malfunctioning tamoxifen pathway, as any effect dependent upon the estrogen-tamoxifen pathway would be confined to the ER+ group.
This study is the largest yet investigating the association between ApoD expression and recurrence (80% power to detect a 1.5-fold change in recurrence), and resulted in precise and null estimates. Selection bias was likely avoided in the design phase, as all cases and controls were selected from the DBCG registry, which contains nearly all Danish breast cancer cases under the age of 70 at diagnosis.[33]
Tamoxifen therapy duration was often inconsistent between the DBCG registry and the patients’ medical records, with the registry indicating that the patient was assigned a shorter duration of therapy. These patients were likely initially assigned the one- or two-year protocol, and then switched to longer protocols as evidence in favor of the five-year protocol became more widespread.[37] Since patients were likely to be on tamoxifen for longer periods of time than the registry indicated, their recurrences were less likely to result from short duration therapy.
There was good concordance between ER+ status at diagnosis and upon re-assay.[39] A previous validation study using medical record review confirmed all recurrences, eliminating the potential for outcome misclassification, and showed perfect agreement for all covariates except one patient’s menopausal status.[40] Staining guidelines were designed to be clinically applicable to ensure that ApoD could be a practical predictive or prognostic indicator if an association was found.
In certain strata, such as for assessing the joint effect of nuclear and cytoplasmic staining, the sample size was fairly small. However, given the consistency of precise null results in nearly all categories of staining, it is unlikely that these estimates would change meaningfully with an increased sample size.
As with many other predictive immunohistochemical biomarkers, the threshhold expression levels to be used to discriminate between ApoD positive and negative cases remain to be established. There is insufficient information to designate such a cutoff for ApoD, but results were null when assessed using dichotomous categorization, as well as dose-response continuous coding among non-zero cores.
Earlier studies that demonstrated an association between ApoD and recurrence did so only within age-specific strata, and had smaller sample sizes.[26, 32] In order for ApoD to be prognostically relevant, it must be meaningfully associated with recurrence in largely nonspecific groups, or its stratum-specific associations must be meaningfully different. A key earlier study in particular found a potential association between ApoD and disease-specific survival in elderly, comorbid patients not receiving chemotherapy.[38] Our results are near null and similar across biologically relevant groups, suggesting that the true association between ApoD expression and recurrence is likely null. As such, the need remains for predictors of response to tamoxifen, as well as recurrence following completion of adjuvant treatment, in order to assess the need for longer duration of therapy or alternate treatments.
Supporting information
*Adjusted estimates were calculated using summary-level 2x2 tables containing exposure and outcome data using an excel spreadsheet created by Lash, Fox, and Fink3 †Value calculated from external validation study conducted by Soiland et al1 ‡Sensitivity analysis resulted in negative bias-adjusted cell values.
(PDF)
*The source population consisted of 11,251 female residents of the Jutland Peninsula in Denmark aged 35–69 years who were diagnosed with Stage I, II, or III breast cancer between 1985 and 2001. Subjects were estrogen receptor positive and received at least 1 year of tamoxifen therapy (ER+/TAM+) or ER negative and never received tamoxifen therapy and survived at least 1 year after diagnosis (ER-/TAM-). ApoD = Apolipoprotein D; UICC = Union for International Cancer Control. †Estimated using logistic regression; case patients were matched to controls on ER status, menopausal status, stage, calendar time of diagnosis, and county NC = Model convergence not satisfied due to sample size limitations within certain strata §Over-inflated variance due to sample size limitations within certain strata.
(PDF)
(PDF)
Data Availability
The data derive from Danish health registries and are augmented by bioassay data generated by the research group. Biomarker data are linked with the Danish Breast Cancer Cooperative Group clinical data at the Danish Breast Cancer Cooperative Group. The research group does not have authority to release the data. All of the data are, however, available to outside researchers by application to the Danish authorities who have oversight of registry-based research. The procedures for application can be obtained by contacting Statistics Denmark (http://www.dst.dk/en/TilSalg/Forskningsservice). Access can also be arranged by contacting dbcg@dbcg.dk.
Funding Statement
This study was supported by the Danish Medical Research Council [DOK 1158859 (T. L. Lash)], U.S. National Cancer Institute at the U.S. National Institutes of Health [R01 CA118708 and R01 CA166825 (T. L. Lash)]; Danish Cancer Society [DP06117 (S. Hamilton-Dutoit)]; Karen Elise Jensen Foundation (H. T. Sørensen); Henrik Toft Sørensen is supported by the Program for Clinical Research Infrastructure established by the Lundbeck and the Novo Nordisk Foundations; Susan G. Komen for the Cure [CCR13264024 (T. Ahern)]; The Mary Kay Foundation [003-14 (T. Ahern)]; and the Lundbeck Foundation [R167-2013-15861 (D.P. Cronin-Fenton)]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Surveillance, Epidemiology, and End Results (SEER) Program, 2009–2011. SEER Stat Fact Sheets: Breast Cancer http://seercancergov/statfacts/html/breasthtml.
- 2.Tao Z, Shi A, Lu C, Song T, Zhang Z, Zhao J. Breast Cancer: Epidemiology and Etiology. Cell biochemistry and biophysics. 2014. [DOI] [PubMed] [Google Scholar]
- 3.Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. The New England journal of medicine. 2006;354(3):270–82. 10.1056/NEJMra050776 [DOI] [PubMed] [Google Scholar]
- 4.Ali S, Coombes RC. Estrogen receptor alpha in human breast cancer: occurrence and significance. Journal of mammary gland biology and neoplasia. 2000;5(3):271–81. [DOI] [PubMed] [Google Scholar]
- 5.National Comprehensive Cancer Network. Stages I and II Breast Cancer. (Version I2014).
- 6.National Comprehensive Cancer Network. Stage III Breast Cancer. (Version I 2014).
- 7.Chlebowski RT. Changing concepts of hormone receptor-positive advanced breast cancer therapy. Clinical breast cancer. 2013;13(3):159–66. 10.1016/j.clbc.2012.11.002 [DOI] [PubMed] [Google Scholar]
- 8.Kelly E, Lu CY, Albertini S, Vitry A. Longitudinal trends in utilization of endocrine therapies for breast cancer: an international comparison. Journal of clinical pharmacy and therapeutics. 2015;40(1):76–82. 10.1111/jcpt.12227 [DOI] [PubMed] [Google Scholar]
- 9.Early Breast Cancer Trialists' Collaborative G, Davies C, Godwin J, Gray R, Clarke M, Cutter D, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378(9793):771–84. 10.1016/S0140-6736(11)60993-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Early Breast Cancer Trialists' Collaborative G. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365(9472):1687–717. 10.1016/S0140-6736(05)66544-0 [DOI] [PubMed] [Google Scholar]
- 11.Burstein HJ, Griggs JJ. Deep time: the long and the short of adjuvant endocrine therapy for breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2012;30(7):684–6. [DOI] [PubMed] [Google Scholar]
- 12.Riggins RB, Schrecengost RS, Guerrero MS, Bouton AH. Pathways to tamoxifen resistance. Cancer letters. 2007;256(1):1–24. 10.1016/j.canlet.2007.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonnell DP, Wardell SE. The molecular mechanisms underlying the pharmacological actions of ER modulators: implications for new drug discovery in breast cancer. Current opinion in pharmacology. 2010;10(6):620–8. 10.1016/j.coph.2010.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cuzick J, Sestak I, Baum M, Buzdar A, Howell A, Dowsett M, et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. The Lancet Oncology. 2010;11(12):1135–41. 10.1016/S1470-2045(10)70257-6 [DOI] [PubMed] [Google Scholar]
- 15.Rastelli F, Crispino S. Factors predictive of response to hormone therapy in breast cancer. Tumori. 2008;94(3):370–83. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez-Angulo AM, Morales-Vasquez F, Hortobagyi GN. Overview of resistance to systemic therapy in patients with breast cancer. Advances in experimental medicine and biology. 2007;608:1–22. [DOI] [PubMed] [Google Scholar]
- 17.Viedma-Rodriguez R, Baiza-Gutman L, Salamanca-Gomez F, Diaz-Zaragoza M, Martinez-Hernandez G, Ruiz Esparza-Garrido R, et al. Mechanisms associated with resistance to tamoxifen in estrogen receptor-positive breast cancer (review). Oncology reports. 2014;32(1):3–15. 10.3892/or.2014.3190 [DOI] [PubMed] [Google Scholar]
- 18.Milani A, Geuna E, Mittica G, Valabrega G. Overcoming endocrine resistance in metastatic breast cancer: Current evidence and future directions. World journal of clinical oncology. 2014;5(5):990–1001. 10.5306/wjco.v5.i5.990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ellis MJ, Tao Y, Luo J, A'Hern R, Evans DB, Bhatnagar AS, et al. Outcome prediction for estrogen receptor-positive breast cancer based on postneoadjuvant endocrine therapy tumor characteristics. Journal of the National Cancer Institute. 2008;100(19):1380–8. 10.1093/jnci/djn309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harris L, Fritsche H, Mennel R, Norton L, Ravdin P, Taube S, et al. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2007;25(33):5287–312. [DOI] [PubMed] [Google Scholar]
- 21.Lamelas ML, Vazquez J, Enguita MI, Rodriguez JC, Gonzalez LO, Merino AM, et al. Apolipoprotein D expression in metastasic lymph nodes of breast cancer. International journal of surgical investigation. 2000;2(4):285–93. [PubMed] [Google Scholar]
- 22.Carreno G, Del Casar JM, Corte MD, Gonzalez LO, Bongera M, Merino AM, et al. Local recurrence after mastectomy for breast cancer: analysis of clinicopathological, biological and prognostic characteristics. Breast cancer research and treatment. 2007;102(1):61–73. 10.1007/s10549-006-9310-0 [DOI] [PubMed] [Google Scholar]
- 23.Diez-Itza I, Vizoso F, Merino AM, Sanchez LM, Tolivia J, Fernandez J, et al. Expression and prognostic significance of apolipoprotein D in breast cancer. The American journal of pathology. 1994;144(2):310–20. [PMC free article] [PubMed] [Google Scholar]
- 24.Do Carmo S, Levros LC Jr., Rassart E. Modulation of apolipoprotein D expression and translocation under specific stress conditions. Biochimica et biophysica acta. 2007;1773(6):954–69. 10.1016/j.bbamcr.2007.03.007 [DOI] [PubMed] [Google Scholar]
- 25.Rassart E, Bedirian A, Do Carmo S, Guinard O, Sirois J, Terrisse L, et al. Apolipoprotein D. Biochimica et biophysica acta. 2000;1482(1–2):185–98. [DOI] [PubMed] [Google Scholar]
- 26.Soiland H, Skaland I, Varhaug JE, Korner H, Janssen EA, Gudlaugsson E, et al. Co-expression of estrogen receptor alpha and Apolipoprotein D in node positive operable breast cancer—possible relevance for survival and effects of adjuvant tamoxifen in postmenopausal patients. Acta oncologica. 2009;48(4):514–21. 10.1080/02841860802620613 [DOI] [PubMed] [Google Scholar]
- 27.Soiland H, Soreide K, Janssen EA, Korner H, Baak JP, Soreide JA. Emerging concepts of apolipoprotein D with possible implications for breast cancer. Cellular oncology: the official journal of the International Society for Cellular Oncology. 2007;29(3):195–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harding C, Osundeko O, Tetlow L, Faragher EB, Howell A, Bundred NJ. Hormonally-regulated proteins in breast secretions are markers of target organ sensitivity. British journal of cancer. 2000;82(2):354–60. 10.1054/bjoc.1999.0926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simard J, Dauvois S, Haagensen DE, Levesque C, Merand Y, Labrie F. Regulation of progesterone-binding breast cyst protein GCDFP-24 secretion by estrogens and androgens in human breast cancer cells: a new marker of steroid action in breast cancer. Endocrinology. 1990;126(6):3223–31. 10.1210/endo-126-6-3223 [DOI] [PubMed] [Google Scholar]
- 30.Beelen K, Zwart W, Linn SC. Can predictive biomarkers in breast cancer guide adjuvant endocrine therapy? Nature reviews Clinical oncology. 2012;9(9):529–41. 10.1038/nrclinonc.2012.121 [DOI] [PubMed] [Google Scholar]
- 31.Soreide JA, Lea OA, Anda O, Skarstein A, Varhaug JE, Kvinnsland S. Progesterone-binding cyst protein (PBCP) in operable breast cancer: correlations with prognostic factors and predictive value for effect of adjuvant tamoxifen treatment. Anticancer research. 1991;11(2):601–5. [PubMed] [Google Scholar]
- 32.Soreide JA, Kolnes J, Skarstein A, Aas T, Kvinnsland S. Progesterone binding cyst protein in hormone receptor positive breast cancer; a predictive factor for effect of adjuvant tamoxifen treatment. Anticancer research. 1994;14(5B):2105–8. [PubMed] [Google Scholar]
- 33.Moller S, Jensen MB, Ejlertsen B, Bjerre KD, Larsen M, Hansen HB, et al. The clinical database and the treatment guidelines of the Danish Breast Cancer Cooperative Group (DBCG); its 30-years experience and future promise. Acta oncologica. 2008;47(4):506–24. 10.1080/02841860802059259 [DOI] [PubMed] [Google Scholar]
- 34.Union for International Cancer Control. TNM Classification of Malignant Tumors. Geneva, Switzerland: Springer, 1997. [Google Scholar]
- 35.Christiansen P, Al-Suliman N, Bjerre K, Moller S, Danish Breast Cancer Cooperative G. Recurrence pattern and prognosis in low-risk breast cancer patients—data from the DBCG 89-A programme. Acta oncologica. 2008;47(4):691–703. 10.1080/02841860802056594 [DOI] [PubMed] [Google Scholar]
- 36.Schmidt M P L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. European Journal of Epidemiology. 2014;29(8):541–9. 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 37.Lash TL, Cronin-Fenton D, Ahern TP, Rosenberg CL, Lunetta KL, Silliman RA, et al. CYP2D6 inhibition and breast cancer recurrence in a population-based study in Denmark. Journal of the National Cancer Institute. 2011;103(6):489–500. 10.1093/jnci/djr010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soiland H, Janssen EA, Korner H, Varhaug JE, Skaland I, Gudlaugsson E, et al. Apolipoprotein D predicts adverse outcome in women >or = 70 years with operable breast cancer. Breast cancer research and treatment. 2009;113(3):519–28. 10.1007/s10549-008-9955-y [DOI] [PubMed] [Google Scholar]
- 39.Cronin-Fenton DP, Hellberg Y, Lauridsen KL, Ahern TP, Garne JP, Rosenberg C, et al. Factors associated with concordant estrogen receptor expression at diagnosis and centralized re-assay in a Danish population-based breast cancer study. Acta oncologica. 2012;51(2):254–61. 10.3109/0284186X.2011.633556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jensena AR E M, Cold S, Storm HH, Overgaard J. Time trends and regional differences in registration, stage distribution, surgical management, and survival of breast cancer in Denmark. Eur J Cancer. 2003;39(12):1783–93. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
*Adjusted estimates were calculated using summary-level 2x2 tables containing exposure and outcome data using an excel spreadsheet created by Lash, Fox, and Fink3 †Value calculated from external validation study conducted by Soiland et al1 ‡Sensitivity analysis resulted in negative bias-adjusted cell values.
(PDF)
*The source population consisted of 11,251 female residents of the Jutland Peninsula in Denmark aged 35–69 years who were diagnosed with Stage I, II, or III breast cancer between 1985 and 2001. Subjects were estrogen receptor positive and received at least 1 year of tamoxifen therapy (ER+/TAM+) or ER negative and never received tamoxifen therapy and survived at least 1 year after diagnosis (ER-/TAM-). ApoD = Apolipoprotein D; UICC = Union for International Cancer Control. †Estimated using logistic regression; case patients were matched to controls on ER status, menopausal status, stage, calendar time of diagnosis, and county NC = Model convergence not satisfied due to sample size limitations within certain strata §Over-inflated variance due to sample size limitations within certain strata.
(PDF)
(PDF)
Data Availability Statement
The data derive from Danish health registries and are augmented by bioassay data generated by the research group. Biomarker data are linked with the Danish Breast Cancer Cooperative Group clinical data at the Danish Breast Cancer Cooperative Group. The research group does not have authority to release the data. All of the data are, however, available to outside researchers by application to the Danish authorities who have oversight of registry-based research. The procedures for application can be obtained by contacting Statistics Denmark (http://www.dst.dk/en/TilSalg/Forskningsservice). Access can also be arranged by contacting dbcg@dbcg.dk.