Abstract
Objective To evaluate an occupational therapy intervention to improve outdoor mobility after stroke.
Design Randomised controlled trial.
Setting General practice registers, social services departments, a primary care rehabilitation service, and a geriatric day hospital.
Participants 168 community dwelling people with a clinical diagnosis of stroke in previous 36 months: 86 were allocated to the intervention group and 82 to the control group.
Interventions Leaflets describing local transport services for disabled people (control group) and leaflets with assessment and up to seven intervention sessions by an occupational therapist (intervention group).
Main outcome measures Responses to postal questionnaires at four and 10 months: primary outcome measure was response to whether participant got out of the house as much as he or she would like, and secondary outcome measures were response to how many journeys outdoors had been made in the past month and scores on the Nottingham extended activities of daily living scale, Nottingham leisure questionnaire, and general health questionnaire.
Results Participants in the treatment group were more likely to get out of the house as often as they wanted at both four months (relative risk 1.72, 95% confidence interval 1.25 to 2.37) and 10 months (1.74, 1.24 to 2.44). The treatment group reported more journeys outdoors in the month before assessment at both four months (median 37 in intervention group, 14 in control group: P < 0.01) and 10 months (median 42 in intervention group, 14 in control group: P < 0.01). At four months the mobility scores on the Nottingham extended activities of daily living scale were significantly higher in the intervention group, but there were no significant differences in the other secondary outcomes. No significant differences were observed in these measures at 10 months.
Conclusion A targeted occupational therapy intervention at home increases outdoor mobility in people after stroke.
Introduction
Many people after stroke do not get out of the house as much as they would like, and this has deleterious effects on quality of life.1,2 Some reasons for poor outdoor mobility are potentially remediable, including lack of confidence and inadequate information on transport options, aids, appliances, or adaptations to the home.3 On the basis of findings of a qualitative interview study, we developed an occupational therapy intervention programme to overcome these barriers.3
Our primary objective was to establish whether people who received the intervention were more likely to get out of the house as much as they wanted. Our secondary objectives were to examine whether the intervention increased the number of journeys taken outdoors, affected the performance of activities of daily living, leisure activity, or psychological wellbeing, and affected the psychological wellbeing of partners or carers.
Methods
We identified patients with a clinical diagnosis of stroke in the previous 36 months from general practice registers and other sources in the community. We included people in care homes. A research occupational therapist (PAL) visited those who had shown interest in invitations by post and asked for their written consent.
PAL collected baseline data, which included personal details, mobility status, personal activities of daily living ability (Barthel activities of daily living index),4 instrumental activities of daily living ability (Nottingham extended activities of daily living),5 and psychological wellbeing (12 item version of the general health questionnaire).6 At this visit PAL provided one session of occupational therapy. This included advice, encouragement, and the provision of leaflets describing local mobility services. This session reflected a routine occupational therapy session and also served as the intervention for those who were later allocated to the control group.
Using the Trent Institute for Health Services Research telephone randomisation service, participants were then randomly allocated to either the control intervention or the outdoor mobility intervention. A computer generated random sequence was used, stratified by age (≤ 65, > 65) and baseline self reported dependency on travel (housebound, accompanied travel, travel alone).
PAL made a clinical assessment of the barriers to outdoor mobility in the participants allocated to the occupational therapy intervention, negotiated mobility goals with them, and then delivered interventions to achieve those goals, using up to seven treatment sessions at home for up to three months. The treatment programme included the provision of information (for example, resuming driving, alternatives to cars and buses); the use of minor aids or adaptations, such as walking aids; and overcoming fear and apprehension by, for example, accompanying participants until confidence was restored. Aids and appliances were obtained from usual sources.
Outcome measures
We measured outcomes by post at four and 10 months after randomisation. Independent, blinded, assessors clarified missing or ambiguous data by telephone or a home visit. Our main outcome measure was the response to the query “do you get out of the house as much as you would like?” This measure has test-retest reliability (unpublished data). Our secondary measures were response to the query “how many journeys outdoors have you taken in the last month?” and scores on the Nottingham extended activities of daily living scale,5 Nottingham leisure questionnaire,7 and the 12 item version of the general health questionnaire.6
Statistical analysis
In the absence of pilot data for our principal outcome measure, we estimated that we needed a sample size of 200 to detect a three point difference in the scores on the Nottingham activities of daily living scale (α = 0.05, power 80%, and standard deviation 58,9).
We used contingency table analysis for our main outcome measure. The distribution of the numbers of outdoor journeys was skewed and analysed using Mann-Whitney U tests. We used multivariate linear regression analysis to analyse the secondary outcome measures. This analysis was adjusted for baseline variables (sex, ethnic origin, age, prior use of transport).
We undertook intention to treat analyses. For our main outcome measure we allocated the worst outcome for participants who were dead at the point of assessment. For others who were lost to follow up, we used their baseline or last recorded responses. We used baseline values to impute missing values for the other analyses.
Results
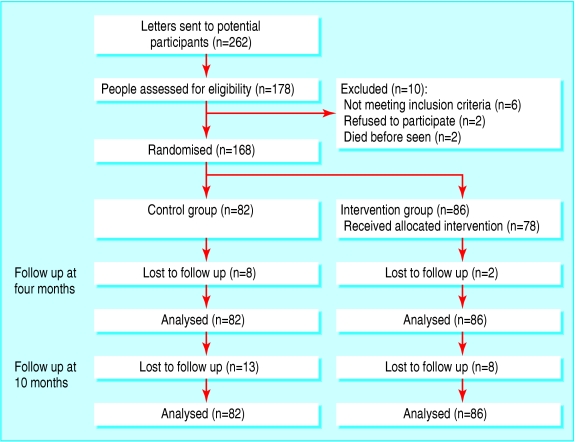
Between June 2001 and December 2002, we invited 262 people to take part in our study (fig 1). We identified eligible participants with a clinical diagnosis of stroke in the previous 36 months from social services departments, a primary care rehabilitation service, a geriatric day hospital, and general practice registers. Overall, 178 of the 262 people responded of whom 10 were excluded, leaving 168 participants. Table 1 shows the characteristics of the groups at baseline.
Fig 1.
Flow of participants through trial
Table 1.
Baseline characteristics of people with clinical diagnosis of stroke allocated to outdoor mobility intervention of leaflet describing local transport services for disabled people (control group). Values are numbers (percentages) of participants unless stated otherwise
| Characteristic | Intervention group (n=86) | Control group (n=82) |
|---|---|---|
| Mean (SD) age (years) | 74 (8.4) | 74 (8.6) |
| Men | 40 (46) | 51 (62) |
| Residential status: | ||
| Lives alone | 36 (42) | 31 (39) |
| Lives with others | 46 (54) | 47 (57) |
| Lives in care home | 4 (5) | 4 (5) |
| Mean (SD) time (months) from stroke | 11 (8.4) | 10 (9.0) |
| Self reported mobility: | ||
| Housebound | 32 (37) | 30 (37) |
| Is accompanied when travelling | 25 (29) | 20 (24) |
| Travels alone | 29 (34) | 32 (39) |
| Gets out of house as much as wants | 24 (28) | 32 (39) |
| Median (interquartile range) scores: | ||
| Barthel activities of daily living index | 18 (16-20) | 17 (13-20) |
| Nottingham activities of daily living | 23 (12-31) | 21 (9-35) |
| General health questionnaire | 10 (7-13) | 11 (8-13) |
Intervention and outcomes
Participants in the intervention group had a mean number of 4.7 visits (median 6, interquartile range 4-6), giving a mean (SD) total of contact time of 230 (113) minutes.
Seven participants in the control group and nine participants in the intervention group required visits at four months to obtain outcome data. At 10 months this applied to eight participants in the control group and 10 participants in the intervention group.
At both four and 10 months, participants in the intervention group were more likely to get out of the house as often as wanted and to undertake more journeys in the month before assessment (table 2).
Table 2.
Outcomes at four and 10 months for people receiving outdoor mobility intervention or leaflets describing local transport services for disabled people. Values are medians (interquartile ranges) unless stated otherwise
| Outcomes | Intervention group (n=86) | Control group (n=82) | Relative risk (95% CI) | P value (Mann-Whitney U test) |
|---|---|---|---|---|
| Four months: | ||||
| No (%) who got out of house as much as wanted | 56 (65) | 30 (35) | 1.72 (1.25 to 2.37)*; number needed to treat 3.3 | — |
| Outdoor journeys in past month | 37 (18-62) | 14 (5-34) | — | P<0.01* |
| 10 months: | ||||
| No (%) who got out of house as much as wanted | 53 (62) | 33 (38) | 1.74 (1.24 to 2.44)†; number needed to treat 4.0 | — |
| Outdoor journeys in past month | 42 (13-69) | 14 (7-32) | — | P<0.01† |
Number needed to treat is number of participants needed to be treated to produce one additional person who could get out of house as much as he or she wanted.
Responders only (n=158): relative risk 1.64 (1.20 to 2.25); intervention, median 39, control, median 15.
Responders only (n=147): relative risk 1.67 (1.21 to 2.31); intervention, median 46, control, median 15.
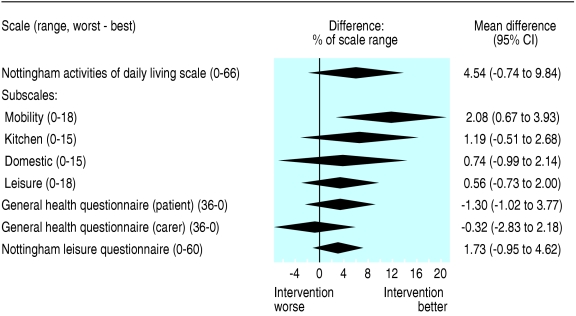
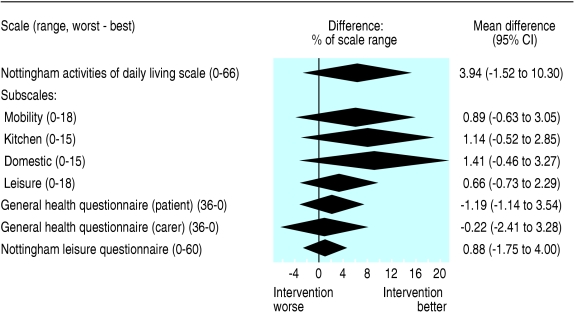
At four months, mobility scores on the Nottingham extended activities of daily living scale were significantly higher in the intervention group than in the control group, but the differences in the scores on the total and other subscores of the Nottingham extended activities of daily living scale, Nottingham leisure questionnaire, and general health questionnaire (for participants or carers) did not reach significance (fig 2). By 10 months we found no significant differences in the scores (fig 3).
Fig 2.
Multivariate linear regression analysis of self reported mobility scores at four months, adjusted for sex, ethnic origin, age, and prior use of transport at baseline. Centre of diamonds represent estimated treatment effect when expressed as percentage of scale range for each scale, and ends of diamonds are 95% confidence intervals for effects
Fig 3.
Multivariate linear regression analysis of self reported mobility scores at 10 months, adjusted for sex, ethnic origin, age, and prior use of transport at baseline. Centre of diamonds represent estimated treatment effect when expressed as percentage of scale range for each scale, and ends of diamonds are 95% confidence intervals for effects
Ancillary analyses
The effect of the intervention at four months was non-significantly greater in those (112 participants) who did not get out of the house as much as they wanted at baseline (relative risk 2.1, 95% confidence interval 1.32 to 3.34) compared with those (56 participants) who got out of the house as much as they wanted at baseline (1.42, 0.92 to 2.18); test for interaction, P = 0.21. Twenty three of the participants (41%) who got out of the house as much as they wanted at baseline did not get out of the house as much as they wanted at four months (seven in intervention group, 16 in control group).
Twenty seven participants who got out of the house as much as they wanted at four months reported that they did not do so at 10 months (17 in intervention group, 10 in control group). Twenty two participants who did not get out of the house as much as they wanted at four months reported that they did at 10 months (14 in intervention group, eight in control group). These differences were not statistically significant (P > 0.1).
The intervention group made a median of 16 more outside journeys at four months than at baseline, compared with a median change of 0 in the control group (P < 0.01). Both groups had a median 0 change in the number of journeys between four and 10 months (P < 0.01).
Discussion
A simple and feasible occupational therapy intervention in people after stroke was successful in increasing outdoor mobility in both the short and the longer term. The benefits of occupational therapy were greatest in those with the worse self reported outdoor mobility at the start of treatment, presumably because they had the most to gain, but we also observed a trend towards a reduction in deterioration in perceived mobility. The benefits of treatment were not lost over time.
This targeted intervention was specially prepared for this study and was expected to overcome many of the barriers to outdoor mobility in patients after stroke. We measured the number of outdoor journeys, expecting it to be affected by the intervention, but chose a person centred principal outcome assessment, measuring at the level of participation rather than of activity. We propose that a cause and effect relation exists between our intervention and the improvement in outcome, and also that our findings are clinically meaningful.
We assessed outcomes by post to reduce the likelihood of inducing bias through face to face assessment, and we think it unlikely that the magnitude, consistency, and persistence of the effect on our principal outcome measure could be explained by response bias. We did not see significant or persistent effects with our secondary measures of instrumental activities of daily living ability, leisure activity, or psychological wellbeing, but due to our sample size we could not exclude moderate treatment benefits in activities of daily living ability. Observer bias in clinical trials has been shown to be unlikely when assessing outcomes by post.10
Our recruitment rate indicates that there is likely to be a sufficient number of people in other health districts to make it worthwhile setting up services to deliver the intervention elsewhere. The high adherence to the trial protocol and the relatively small number of visits for occupational therapy suggests that the intervention is feasible within a NHS or similar healthcare setting (for example, community rehabilitation teams).
Our findings are likely to apply to the delivery of the intervention by other motivated occupational therapists who have been trained to provide the sorts of interventions used in this study. Our findings may not, however, apply to services delivered by untrained staff, to treatments that are considerably shorter than in our study, or to where one or more elements of the intervention cannot be provided, such as access to aids and equipment.
Our findings that occupational therapy can improve outdoor mobility are novel, but they are compatible with existing evidence that supports the use of community rehabilitation services after stroke11 and targeted interventions from an occupational therapist.12
What is already known on this topic
The quality of life of many people after stroke is poor because they are housebound
What this study adds
A brief intervention by an occupational therapist improves outdoor mobility in community dwelling people after stroke
The intervention includes the provision of information, aids, and appliances, and approaches to overcoming fear
The intervention is likely to be feasible in many healthcare settings
We thank the participants, the primary care services who searched their records for people with stroke and sent letters on our behalf, Carol Coupland (lecturer in statistics) who provided statistical assistance, and Trent Focus, Primary Care Research network for promoting the research in the primary care setting.
Contributors: PAL had the idea for the study, secured funding, obtained ethical approval, conducted and analysed the study, and contributed to writing the manuscript. JRFG advised over study design, supervised PAL, helped with analysis, and drafted the manuscript; he is guarantor. AA advised over study design, supervised PAL, advised over analysis, and contributed to the preparation of the manuscript. MFW advised over study design and analysis and contributed to the preparation of the manuscript. JD advised over study design, access to patients and recruitment, interpretation of findings, and preparation of the manuscript. LG advised over study design, analysis, interpretation, and preparation of the manuscript.
Funding: The NHS research and development department funded the study through a National Primary Care Researcher Development Award to PAL.
Competing interests: None declared.
Ethical approval: Ethical approval was obtained from the Nottingham Queen's Medical Centre ethics committee (HC060001).
References
- 1.Logan PA, Gladman JRF, Radford KA. The use of transport by stroke patients. Br J Occup Ther 2001;64: 261-4. [Google Scholar]
- 2.Pound P, Gompertz P, Ebrahim S. A patient-centred study of the consequences of stroke. Clin Rehabil 1998;12: 338-47. [DOI] [PubMed] [Google Scholar]
- 3.Logan PA, Gladman JRF, Dyas J. An interview study of the use of transport by people who have had a stroke. Clin Rehabil 2004;18: 703-8. [DOI] [PubMed] [Google Scholar]
- 4.Collin C, Wade DT, Davies S, Horne V. The Barthel ADL index: a reliability study. Int Disability Stud 1988;10: 61-3. [DOI] [PubMed] [Google Scholar]
- 5.Nouri FM, Lincoln NB. An extended activities of daily living scale for stroke patients. Clin Rehabil 1987;1: 301-5. [Google Scholar]
- 6.Goldberg D. General health questionnaire (GHQ-12). Windsor: Nfer-Nelson, 1992.
- 7.Drummond AER, Parker CJ, Gladman JRF, Logan PA on behalf of the TOTAL study group. Development and validation of the Nottingham leisure questionnaire. Clin Rehabil 2001;15: 647-56. [DOI] [PubMed] [Google Scholar]
- 8.Walker MF, Gladman JRF, Lincoln NB, Siemonsma P, Whiteley T. A randomised controlled trial of occupational therapy for stroke patients not admitted to hospital. Lancet 1999;354: 278-80. [DOI] [PubMed] [Google Scholar]
- 9.Parker CJ, Gladman JRF, Drummond AER, Dewey ME, Lincoln NB, Barer BH, et al. A multi-centre randomised controlled trial of leisure therapy and conventional occupational therapy after stroke. Clin Rehabil 2001;15: 42-52. [DOI] [PubMed] [Google Scholar]
- 10.Parker CJ, Dewey ME on behalf of the TOTAL study group. Assessing research outcomes by postal questionnaire with telephone follow up. Int J Epidemiol 2000;29: 1065-9. [DOI] [PubMed] [Google Scholar]
- 11.Outpatient Therapy Trialists. Rehabilitation therapy services for stroke patients living at home: a systematic review of the randomised trials. Lancet 2004;363: 352-6. [DOI] [PubMed] [Google Scholar]
- 12.Steultjens EMJ, Dekker J, Bouter LM, van de Nes JCM, Cup EHC, van den Ende CHM. Occupational therapy for stroke patients. A systematic review. Stroke 2002;34: 676-87. [DOI] [PubMed] [Google Scholar]